Abstract
Objectives
This study aims to (1) examine the direct and indirect effects internalized heterosexism, concealment of gender identity, and perceived general stress in association with depression among transgender older adults; and (2) to assess the relative contribution of each relationship.
Methods
Secondary analyses of data from a large community-based study of older sexual and gender minorities were conducted utilizing structural equation modeling with a subsample (n = 174) of transgender adults aged 50 to 86-years old.
Results
Disclosure of gender identity had no significant direct or indirect effects on either perceived general stress or depression. Internalized heterosexism did not have a direct effect on depression, but did have a significant indirect effect through perceived general stress. Finally, perceived general stress had an additional significant direct effect on depression, over and above internalized heterosexism. Total effect sizes appear to be considerable with standardized betas greater than 5.0.
Conclusion
Perceived general stress and internalized heterosexism independently and cumulatively have significant direct and indirect effects on depression among transgender older adults. Implications for depression among transgender older adults and the role of community psychology are discussed.
Keywords: gender identity, mental health, stigma, older adults, social stress, LGBT
Introduction
Depression is the most prevalent chronic mental health condition affecting older Americans (Centers for Disease Control and Prevention, 2013), and with the rapidly expanding older adult population is projected to become the second major cause of disease burden worldwide within a few short years (World Health Organization, 2012). Large community-based research suggests that transgender older adults may be at greater risk for depression than lesbian, gay, and bisexual (LGB) older adults (Fredriksen-Goldsen, Cook-Daniels, et al., 2013), who are themselves at heightened risk for depression in later life compared to heterosexual older adults (Fredriksen-Goldsen, Kim, Barkan, Muraco, & Hoy-Ellis, 2013; Valanis et al., 2000; Wallace, Cochran, Durazo, & Ford, 2011). Although increasing, research with transgender older adults is somewhat sparse and there is limited empirical evidence elucidating underlying mechanisms linking risk and protective factors to depression (Institute of Medicine, 2011). Reducing the prevalence of major depression among transgender and older adults is a primary objective of Healthy People 2020 (U.S. Department of Health and Human Services, 2013,U.S. Department of Health and Human Services, 2016). Individual and group level clinical interventions are prototypical responses to stigma-related depression among transgender people (Hendricks & Testa, 2012). Community psychology is uniquely positioned to take a leadership role in addressing stigma as a primary social determinant of mental health disparities, including depression among gender and sexual minorities. Understanding pathways by which upstream, social forces manifest as downstream, individual risk factors contributing to poor mental health outcomes will be a key component of this opportunity.
Estimates of the prevalence of depression among older adults in the general population range from 1% – 5% (Centers for Disease Control and Prevention, 2015) to 6% – 8% (Centers for Disease Control and Prevention and National Association of Chronic Disease Directors, 2009; Substance Abuse and Mental Health Services Administration, 2013). Subsyndromal depression among older Americans may range as high as 15% (Fiske, Wetherell, & Gatz, 2009). Large community and national internet surveys using tools that screen for clinically significant depressive symptomatology have found rates among transgender adults that range from 44% (Bockting, Miner, Swinburne Romine, Hamilton, & Coleman, 2013), to 48% (Fredriksen-Goldsen, Cook-Daniels, et al., 2013), and potentially as high as 55% to 62% (Clements-Nolle, Marx, Guzman, & Katz, 2001; Clements-Nolle, Marx, & Katz, 2006), although these rates may be influenced by bias inherent in community sampling (Rosser, Oakes, Bockting, & Miner, 2007). Gender and gender identity have been identified as independent risk factors for negative mental health outcomes (Hankivsky, 2012; Persson, 2009; Springer, Hankivsky, & Bates, 2012). Related factors such as internalized stigma (Hendricks & Testa, 2012; Meyer, 2003) contribute to transgender older adults’ heightened risk for depression (Fredriksen-Goldsen, Cook-Daniels, et al., 2013; Persson, 2009).
Conceptual framework
Social stressors, such as low socioeconomic status (SES) (Blazer & Hybels, 2005) and marginalized social position (Cairney & Krause, 2005) are associated with greater risk for depression among older adults. Part of this greater risk results from stress proliferation; exposure to stressors multiplies and leads to exposure to still more stressors (Aneshensel, 2009; Pearlin, Aneshensel, & LeBlanc, 1997). Stigma, its constituent components and its correlates is a “fundamental cause” of health disparities (including depression) among minority groups around the world (Hatzenbuehler, Phelan, & Link, 2013). It is a veritable breeding ground for stress proliferation. The minority stress model describes pathways by which external and internal minority stress processes (i.e., stigma) operate relative to other minority statuses (e.g., race/ethnicity, gender) to impact mental health outcomes among sexual (Meyer, 2003) and gender minorities (Hendricks & Testa, 2012). While external minority stressors (i.e., discrimination, victimization) may be experienced by anyone who is ‘perceived” to hold a minority status; only those who actually self-identify with a particular minority status are subject to internal minority stress processes. The most internal of minority stressors are the long-term concealment of minority identity (Meyer, 2003), including gender identity (S.Cole, Denny, Eyler, & Samons, 2000), and the internalization of stigma attached to a given minority status, including transgender (Hendricks & Testa, 2012).
Heterosexism, as it relates to sex and gender privileges traditional female/male sex and woman/man gender binaries, assuming that the gender assigned at birth based on ascribed sex should be the gender with which one identifies. This stance stigmatizes any manifestation of gender nonconformity and transgender identity as unnatural and abnormal (Gordon & Meyer, 2007). When internalized, negative attitudes, beliefs, and stereotypes associated non-normative gender identities and expressions (i.e., internalized heterosexism) can diminish transgender people’s feelings of self-worth, making it more difficult to deal with stressful events and conditions in the larger environment, thereby becoming a source of chronic stress (Hendricks & Testa, 2012). One avenue by which transgender individuals may attempt to respond to stressful environmental conditions, such as potential and actual discrimination and victimization is attempted concealment, a strategy wherein coping with social stigma is achieved by hiding a non-heteronormative gender identity (Bockting et al., 2013). While such a strategy may be protective initially through reducing one’s visibility as a target, it can also have detrimental consequences over time (Meyer, 2003). For example, it can negatively impact psychoneuroimmunological functioning (S. W.Cole, Kemeny, Taylor, Visscher, & Fahey, 1996), and diminish opportunities to develop individual, social, and community resources that foster coping capacities (Meyer, 2003). Conversely, disclosure of a stigmatized identity may provide access to these important coping resources and consequently ameliorate internalized heterosexism (Hendricks & Testa, 2012; Meyer, 2003). Disclosure of sexual orientation has been linked to lower levels of internalized heterosexism among LGB older adults (Hoy-Ellis & Fredriksen-Goldsen, 2016). Concealment of gender identity or sexual orientation from family members and friends has been associated with internalized heterosexism and increased risk for depression among transgender older adults (Fredriksen-Goldsen, Cook-Daniels, et al., 2013). These minority stress processes are theorized to be cumulative and in addition to general life stressors common to everyone (Meyer, 2003).
Studies that examine depression among minority populations do not generally account for general and minority stressors simultaneously, even though they typically co-occur (Hatzenbuehler, 2009; Williams, Neighbors, & Jackson, 2003). Exposures to general and minority stressors are inherently determined by conditions in the larger environment and are interactive by nature (Meyer, 2003), although the relative influence of each respective type of stressor on mental health outcomes (e.g., depression) may be unclear. For example, a transgender older adult who experiences employment discrimination because of their gender identity may experience both poverty (general stressor) and activation of internalized negative heterosexist attitudes and beliefs about themselves (minority stressor). Further complicating the comparative contributions of each is the subjective perception of objective experience.
High levels of perceived stress are associated with depression (Bergdahl & Bergdahl, 2002); especially when the stress is ongoing (Nurius & Hoy-Ellis, 2013); and is a stronger predictor of depression than acute stressful life events (Cohen, Kamarck, & Mermelstein, 1983). The brain plays a key role in determining whether events and conditions in the social environment are experienced as stressful. Primary appraisals determine the actuality of perceived threat (i.e., is the threat “real”), while secondary appraisals gauge whether the individual can marshal resources sufficient to cope with identified threats (Lazarus & Folkman, 1984). Thus, it is the perception of events or conditions as threatening, coupled with the perception of available coping resources that are predictive of stress, rather than any objective determinations of actual threat or accessible resources. Internalized heterosexism related to gender identity can be considered a chronic stressor that limits transgender people’s ability to deal with general stressors (Hendricks & Testa, 2012) by wearing down coping capacities (McEwen, 1998). Internalized heterosexism and concealment of gender identity are also each independently predictive of perceived stress among transgender older adults (Fredriksen-Goldsen, Cook-Daniels, et al., 2013).
This study seeks to identify specific linkages between, and relative differential effects of internalized heterosexism, disclosure of gender identity, perceived general stress, and depression among transgender older adults. Specifically, we hypothesize that (1) internalized heterosexism will have positive direct and indirect (via perceived general stress) associations with depression; (2) disclosure of identity will have inverse direct and indirect (via [a] internalized heterosexism, and [b] perceived general stress) associations with depression; and (3) perceived general stress will have an additional positive direct association with depression, over and above the effects of internalized heterosexism and identity disclosure (see Figure 1). Understanding the relative contributions of minority and general stress will help further our knowledge of depression among this at-risk population, and potentially identify key points for intervention.
Figure 1.
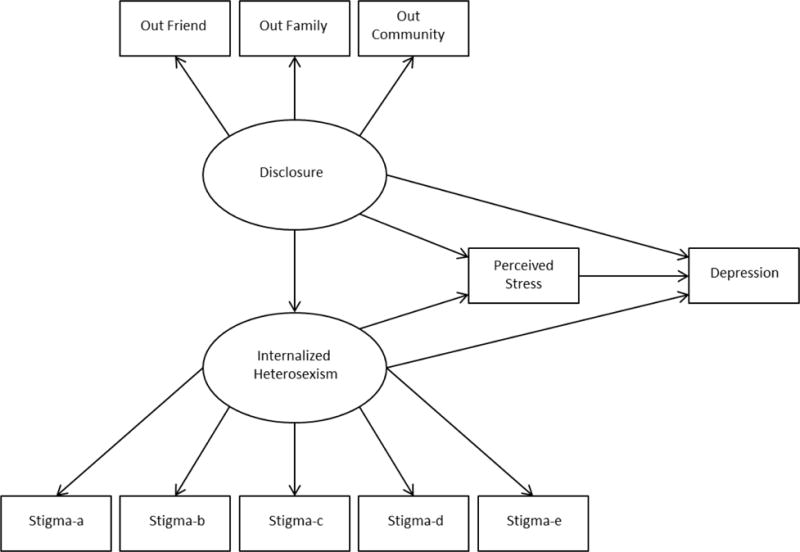
Hypothesized Structural Equation Model
Methods
In order to test these hypotheses, we conducted secondary analyses of cross-sectional data from the Caring & Aging with Pride Over Time: National Health, Aging, Sexuality/Gender Study (NHAS), a collaboration between the Institute for Multigenerational Health and 11 agencies in the U.S. that serve the needs of older LGBT adults. In addition to full review and approval by the sponsoring university’s IRB, several agencies also conducted their own internal reviews. Study materials, including informed consent and study surveys were distributed via the agency mailing lists to potential participants. In order to be eligible for the study, respondents were required to be (1) 50 years-old or older at the time of data collection; and (2) self-identify as lesbian, gay, bisexual, or transgender. In addition to standard sociodemographic questions such as age, income, and education, surveys included measures that assessed mental health, perceived global stress, and specific minority stressors, such as internalized heterosexism and disclosure of sexual and/or gender identity. A response rate of 63% yielded 2,560 surveys completed by LGBT adults aged 50 to 95 years old. This study focuses specifically on the 174 participants who self-identified as transgender. For a fuller description of the original study see Fredriksen-Goldsen, Cook-Daniels, and colleagues (2013).
Measurement
Disclosure of identity was assessed via the 12-item Outness Inventory (Mohr & Fassinger, 2000), which asks participants to indicate the degree to which others “know or have known that [they] are gay, lesbian, bisexual, or transgender” on a 4-point Likert scale (1 = definitely do not know, through 4 = definitely do know) in three primary social domains: best friend, family (e.g., parents, siblings), and community (e.g., neighbors, faith community). Higher scores indicate lower levels of concealment and higher levels of disclosure; Cronbach’s α = 0.82.
Internalized heterosexism was measured with an adapted version of the Homosexual Stigma Scale (Liu, Feng, & Rhodes, 2009) that asks the level of agreement on a 4-point Likert scale (1 = strongly disagree, through 4 = strongly agree) to five statements, such as “I wish I weren’t lesbian, gay, bisexual or transgender.” Higher scores indicate higher levels of internalized heterosexism; Cronbach’s α = 0.79.
General stress was evaluated via the 4-item Perceived Stress Scale (PSS) (Cohen et al., 1983). Utilizing a 5-point Likert scale (0 = never, through 4 = very often), participants indicated their subjective perception of general stress in their lives during the preceding month. An example question was “in the last month, how often have you felt that you were unable to control the important things in your life?” Higher scores indicate higher levels of perceived general stress; Cronbach’s α = 0.84.
Depression was gauged with the short 10-item form of the Center for Epidemiological Studies Depression Scale (CESD-10) (Radloff, 1977). This scale asks respondents to indicate how often during the past week (0 = < less than 1 day, through 3 = 5 – 7 days) they had “felt or behaved” in particular ways, such as “I felt that everything I did was an effort.” The CESD-10 has good psychometric properties (Zhang et al., 2012); Cronbach’s α = 0.88. On a range of 0 – 30, scores ≥ 10 indicate clinically significant depressive symptomatology.
Because of their known relationship to both stress and depression (Marmot et al., 1991; Marmot & Wilkinson, 2006), the following variables were controlled for. Age was calculated from year of birth. Gross annual household income was assessed across six intervals: < $20,000; $20,000 – $24,999; $25,000 – $34,999; $35,000 – $49,999; $50,000 – $74,999; and $75,000 or more. Educational attainment was categorized as: kindergarten or none; grade 9 – 11; grade 12 or GED; college 1 – 3 years of college; and college 4 years or more.
Analytic plan
Because of its utility in testing a priori theorized models (Bollen, 1989), in this case the hypothesized structural relationships between disclosure/concealment of gender identity, internalized heterosexism, perceived stress, and depression, structural equation modeling (SEM) was used. SEM accounts for measurement error and provides more precise standard errors (Iacobucci, Saldhana, & Deng, 2007) that are closer to the true population. SEM is also sensitive to mediation effects when they exist, even with sample sizes as small as n = 30 (Iacobucci et al., 2007). A sample size of at least 200 has been considered the minimum for SEM analyses, a requirement that is often not met in published, peer-reviewed studies (Hoyle & Gottfredson, 2014; Matsueda, 2012). According to Hoyle and Gottfredson (2014) it is not the sample size per se, but the ratio of observations to free parameters that determines stability of estimates. Following guidelines for lower bounds for sample size in SEM established by Westland (2010)), the minimum sample size required for a small effect size of 0.1; power level of 0.8; two latent variables and eight observed variables (both measurement and indicator); p – value ≤ .05 is 152. To increase stability of parameter estimates through maximization of small sample size (Hopkin, Hoyle, & Gottfredson, 2015), the maximum likelihood with missing values (MLMV) estimator was used along with bootstrapping (500 replications) for more precise standard errors (Hoyle & Gottfredson, 2014).
Stata version 12 was used for all analyses, including descriptive and summary statistics. Additionally, standardized coefficients in the final structural equation model were obtained in order to compare the relative contributions of latent and measured variables on depression. Multiple post-estimation goodness-of-fit (GOF) statistics offer a variety of indices that individually and collectively determine how close the data fit the theorized model (Hooper, Coughlan, & Mullen, 2008). A Root Mean Square Error of Approximation (RMSEA) < .06; Comparative Fit Index (CFI) > .90; p of Close Fit (pCLOSE) > .05; and Confidence Interval (CI) close to 0.0 separately and together indicate a good fit of the model to the data. The coefficient of determination (CD) provides model R2.
Results
The age range of sample participants (n = 174) was 50 to 86-years old (M = 60.97; SD = 7.96), nearly two-thirds (64%) identified as female, and the majority (82%) as non-Hispanic white. In terms of sexual orientation, nearly a third (32%) identified as lesbian or gay, slightly fewer (27%) as bisexual, the fewest (19%) as heterosexual, and just over a fifth (22%) as something else. Although close to two-thirds (62%) had four or more years of college, more than half (53%) had yearly household incomes less than $35,000 (see Table 1 for more complete sociodemographics).
Table 1.
Sample Sociodemographic Characteristics of Transgender-Identified Participants
| Variable | (%) | (n) |
|---|---|---|
| Age M (SD) | 60.97 (7.96) | 174 |
| Gender | ||
| Women | 64.03 | 89 |
| Men | 35.97 | 50 |
| Sexual orientation | ||
| Lesbian/Gay | 31.58 | 54 |
| Bisexual | 27.49 | 47 |
| Heterosexual | 18.71 | 32 |
| Other | 22.22 | 38 |
| Race/Ethnicity | ||
| Hispanic | 3.64 | 6 |
| Black | 4.85 | 8 |
| American Indian/Alaska Native | 7.27 | 12 |
| Asian/Hawaiian/Pacific Islander | 1.82 | 3 |
| Non-Hispanic white | 82.42 | 136 |
| Education | ||
| Grade 1 − 8 | 1.74 | 3 |
| Grade 9 – 11 | 1.74 | 3 |
| Grade 12 or GED | 8.14 | 14 |
| College 1 – 3 years | 26.16 | 45 |
| College 4 years or more | 62.21 | 107 |
| Annual household income | ||
| < $20,000 | 29.24 | 50 |
| $20,000 – $24,999 | 10.53 | 18 |
| $25,000 – $34,999 | 12.87 | 22 |
| $35,000 – $49,999 | 14.62 | 25 |
| $50,000 – $74,999 | 14.04 | 24 |
| $75,000 or more | 18.71 | 32 |
Participants evidence relatively high levels of disclosure overall (M = 3.29, SD = .82, range = 1 – 4); low to moderate levels of internalized heterosexism (M = 1.78, SD = .65, range = 1 – 4); and perceived general stress (M = 1.56, SD = .88, range = 1 – 4). The mean depression score of participants (M = 10.34, SD = 7.29, range = 0 – 30) exceeds the established threshold ≥ 10 on the CESD-10, indicating clinically significant depressive symptomatology (Radloff, 1977; Zhang et al., 2012). Detailed sample summary statistics are shown in Table 2.
Table 2.
Sample Summary Statistics
| Variable | range | M (SD) |
|---|---|---|
| Out to friend | 3.65 (.91) | |
| Out to family | 1 – 4 | 3.25 (.97) |
| Out to community | 3.25 (.94) | |
| Internalized heterosexism | 1 – 4 | 1.78 (.65) |
| Perceived general stress | 0 – 4 | 1.56 (.88) |
| Depression (CESD) | 0 – 30 | 10.34 (7.29) |
| CESD ≥ 10 | 47.9% (n = 81) | --- |
The fitted structural equation model is displayed in Figure 2; factor loadings and regression coefficients are standardized. A variance inflation factor (VIF) of 1.60 is significantly lower than the upper limit threshold of 5.0 (StataCorp, 2011), indicating that multicollinearity was not an issue. Separately and collectively, the GOF statistics suggested by Hooper and colleagues (2008) suggest that the model is a close fit to the data (see Table 3). Post-estimation decomposition of effects in the fitted model indicates that internalized heterosexism has significant positive indirect (p = .005) and total effects (p = .003), and a non-significant direct effect (p = .066) on depression, implying that perceived stress mediates the relationship between internalized heterosexism and depression. Concealment of gender identity is not significantly associated with depression, either directly (p = .486) or indirectly through perceived general stress (p = .286), and the total effect is also non-significant (p = .681). There is a significant inverse relationship between concealment of gender identity and internalized heterosexism (p = .020), but this effect does not appear extend to either perceived general stress or depression. The direct/total effect of perceived general stress on depression is significant (p < .001). The coefficient of determination is 0.74, indicating that the predictor variables account for 74% of the variance in depression. Standardized direct, indirect, and total effects of predictor variables on depression and bootstrapped standard errors are shown in Table 4. The total effect of perceived general stress on depression (b* = 5.93) is nearly one standard deviation greater than the effect of internalized heterosexism (b* = 5.01).
Figure 2.
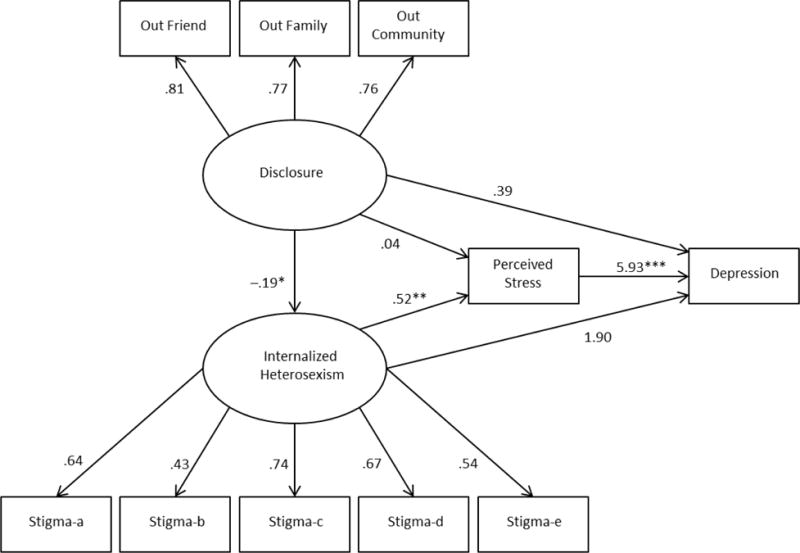
Fitted Structural Equation Model.
Note: Factor loadings and path coefficients are standardized.
Table 3.
Model Goodness-of-fit Statistics
| Statistical test | Statistical value |
|---|---|
| Χ2 (df) | 62.13 (47), p = .069 |
| Root Mean Square Error of Approximation | 0.04 |
| p of Close Fit | .62 |
| Confidence Interval (90%) | [.00, .07] |
| Comparative Fit Index | 0.97 |
| Coefficient of Determination (Model R2) | 0.74 |
Table 4.
Decomposition of Effects of Predictor Variables on Depression
| Depression
|
||||||
|---|---|---|---|---|---|---|
| Direct b* | p | Indirect b* | p | Total b* | p | |
| Concealment | 0.39 | .486 | − 0.72 | .269 | − .33 | .681 |
| Internalized heterosexism | 1.90 | .066 | 3.11 | .005 | 5.01 | .003 |
| Perceived stress | 5.93 | <.001 | – | – | 5.93 | <.001 |
Note: Coefficients are standardized
Discussion
This is one of the few empirical studies that have examined the mental health needs of transgender older adults as a distinct group. It is one of the first to test the applicability of the minority stress model to a transgender sample, and to explore the relative contribution of both general stress and select minority stressors on the mental health of transgender older adults. In this study, nearly half (48%) of the transgender older adults were experiencing clinically significant depressive symptomatology. Results suggest an array of direct and indirect pathways between minority and general stress and depression. The sum of these effects suggest that general stress may exert at least as strong an influence as minority stress on mental health that may shed light on our understanding of depression in this highly marginalized population.
The first hypothesis was partially supported. Among transgender older adults in this sample, internalized heterosexism had a non-significant direct effect on depression, but did have a significant indirect effect, suggesting that perceived general stress mediates the relationship. This is consistent with the minority stress perspective in that general stress and minority stress appear to operate in tandem in affecting depression (Meyer, 2003). That internalized heterosexism did not influence depression directly or independently of perceived general stress is both consistent and inconsistent with other research. Fredriksen-Goldsen, Cook-Daniels and colleagues (2013) reported that internalized heterosexism mediated the relationship between gender identity and depression, and gender identity and perceived stress in a comparison of transgender versus non-transgender LGB older adults. In the model they tested, both perceived general stress and depression were treated as outcome variables, while the current study examined a model wherein perceived general stress was a predictor of depression. More recent findings suggest that prior military service may attenuate the relationship between internalized heterosexism and depression among transgender older adults (Hoy-Ellis et al., 2017). There may be differences between older transgender women and men, given the gendered construction of American society. The lack of a direct effect may also be the result of a Type II error, as the p-value (.066) is fairly close to the .05 level of significance. Other factors may influence the link between internalized heterosexism and depression among this specific population. For example, transgender individuals who have successfully transitioned may experience less of the negative consequences of internalized heterosexism and consequent depression (Hendricks & Testa, 2012). As phenotypic expression becomes more congruent with gender identity, cognitive dissonance and accompanying psychological distress likely decrease, attenuating levels of internalized heterosexism. Gender transition processes may also affirm social identification of individual gender identity, potentially influencing the association between internalized heterosexism and concealment/disclosure of transgender identity related to hypothesis 2. Differentiating between those who have and haven’t completed transition, length of time since completion, and the degree to which individuals appraise their transitional processes and concurrent visible expressions of gender as being more or less affirming actual gender identities (regardless of time to/from transition) may also be important in understanding pathways of risk and resilience.
The second hypothesis was not supported; identity disclosure was neither directly related to depression, nor indirectly through internalized heterosexism nor perceived general stress. It is interesting that identity disclosure had a significant inverse relationship with internalized heterosexism, but that did not extend to either perceived general stress or depression. This may be a Type II error due to the small sample size. On the other hand, while gender identity itself is not outwardly visible, gender expression – the social signaling of gender through dress, mannerisms, behaviors, and grooming (among others) – is visible by design. According to minority stress theory, continued concealment of identity over time negatively impacts mental health, while disclosure of minority identity can eventually diminish the negative impact of internalized heterosexism on mental health outcomes through positive self-reappraisals of one’s identity, and group-level coping supports from similar others (Meyer, 2003). As one travels along the arc of gender transition, the avoidant coping style inherent to concealment of identity gradually is replaced by a more facilitative, problem-solving coping style as one learns to navigate the nuances of disclosure (Budge, Adelson, & Howard, 2013). A recent qualitative study of transgender older adults who transitioned after the age of 50 found that for most participants, accepting and disclosing their transgender identity as they transitioned was:
fraught with emotional anguish and anger, which took a toll on their mental health…. [but resulted in] the sheer peace of accepting oneself and feeling comfortable in one’s own skin. Emotions of shame and anger were balanced with great fortitude and a sense of joy and liberation for most participants (Fabbre, 2015, p. 149).
The sense of joy and liberation accompanying transition may ameliorate the toll of concealment on mental health. Gender transition and identity disclosure processes may also attenuate perceived general stress. Actual and anticipated reactions to disclosure may respectively moderate and mediate the impact of disclosure on mental health outcomes, and subsequent decisions as to whether to disclose or conceal (Pachankis, 2007; Quinn et al., 2014). The ‘threat’ of anticipated reactions is only a threat, and hence uncontrollable in its unpotentiated state. Once disclosure is made, the threat becomes a challenge with multiple potential responses to meet that challenge. Initial disclosure reactions may thus provide a type of stress inoculation to subsequent disclosures and increase a sense of self-efficacy. Actual and anticipated reactions to disclosure and data regarding gender transition were not available in this study, but will be important to account for in future research.
As predicted in hypothesis 3, perceived general stress has a significant direct effect on depression, independent of internalized heterosexism and concealment of gender identity. These findings indicate that both general and minority stress processes are influential in depression among older transgender adults, which is consistent with general social stress theory (Aneshensel, 1992) and the minority stress model (Meyer, 2003). Transgender older adults in this study evidenced alarmingly high rates of clinically significant depressive symptomatology, potentially the result of stress proliferation. Because of the transactional nature of social experience, stressors arising in one domain of life often expand into other domains of life (Pearlin et al., 1997). Such “chain reactions” go beyond simply increasing the number and types of stressors that an individual experiences; stress proliferation can also influence the subjective stress appraisal process, which can negatively impact mental health (LeBlanc, Frost, & Wight, 2015). For example, experiencing an act of discrimination or victimization (for instance employment-based) related to transgender identity may consequently activate internalized negative heterosexist stereotypes related to gender variance, which may lead to increased anticipation of further experiences of transgender identity-based discrimination. The subsequent secondary appraisal that ‘there is nothing one can do’ about such experiences, the hallmark of insufficient coping resources to respond to adaptation demands (Lazarus & Folkman, 1984) would thus increase the risk for depression.Meyer (2003) notes that environmental circumstances are associated with both general and minority stressors. However, the line demarcating general from minority stressors, and the overlap and interactions between these two primary categories of stressors, is far from clear.Meyer (2003) provides an example of how a gay man’s status as a sexual minority (i.e., minority stressor) and being low on the SES ladder (i.e., general stressor) would conjointly determine his level of stress exposure. But what if low SES is instead a direct result of minority status? For example, accumulating evidence from large community-based and internet studies indicate that in addition to the stress associated with internalized heterosexism, transgender adults in general (Bockting et al., 2013; Grant et al., 2011), and older transgender adults in particular (Fredriksen-Goldsen, Cook-Daniels, et al., 2013) also experience economic disadvantage due to their transgender status, despite high levels of education. Whether chronic or episodic, transgender individuals encounter high levels of unemployment and underemployment throughout their adult lives (Conron, Scott, Stowell, & Landers, 2012; Grant et al., 2011); this is attributable to gender identity-based discrimination that is so commonplace that transgender older adults consider it to be a “normal” part of their lived experience (Persson, 2009). Socioeconomic instability and low income are primary sources of stress proliferation (Thoits, 2010), and when they result from a marginalized status, such as being transgender, tend to increase exposure to other stressors (Meyer, 2003). Thus, what may be characterized on one hand as a general stressor may in fact be an effect of a minority stressor.
Implications
The results of this study have important implications for research and practice. One significant factor in transgender older adults being “understudied” is that although gender is a demographic routinely assessed in national and other probability surveys, such as the U.S. Census and state-level Behavioral Risk Factor Surveillance Surveys (BRFSS), questions regarding gender identity remain absent. In order to address population health disparities and improve quality of life among marginalized groups, primary objectives of Healthy People 2020 (U. S. Department of Health and Human Services, 2011) and other similar initiatives, we must have a clearer understanding of the nature and scope of said disparities and quality of life. To achieve these goals, we need to begin by assessing gender identity in major research projects, which will be instrumental in obtaining robust estimates of the prevalence of the transgender population. Such knowledge will be foundational to establishing and ascertaining risk and protective factors and their underlying relationships to health (Institute of Medicine, 2011). Such an undertaking is likely to be extremely complex as our understanding of gender as a binary construct evolves, and will be further complicated by who is included or excluded under the transgender umbrella. For example, cross-gender impersonators (e.g., drag queens and kings), and transvestites (i.e., cross-dressers) have been increasingly included under the rubric of transgender (Lombardi, 2009; Persson, 2009), even though such individuals do not typically identify as transgender. In addition to assessing gender identity in national and probability studies, longitudinal studies specific to the transgender population across the life course will also be needed. Such studies should include items pertaining to gender transition, transgender identity development, and minority stressors, such as transgender identity management strategies and internalized heterosexism specific to gender. Studies like these will also be complex and will need to clearly differentiate minority stressors related to gender identity from those associated with sexual orientation. Standardization and uniform application of measures assessing minority stressors and constructs unique to transgender experience will be invaluable in comparing results across studies.
Because general and minority stressors are situated in the larger environment, and minority stressors in particular are rooted in heterosexist structures and institutions, policies that shape these contexts, such as legal protection against gender identity-based discrimination are critical, and may ultimately have the greatest impact on the mental health of transgender older adults. As noted by Kenny and Hage (2009), “preventive interventions that reduce oppressive societal structures, change attitudes that contribute to oppression, and enhance individual, family, and community strengths that empower persons to resist oppression represent important vehicles for advancing social justice” (p. 1173). For example, even after achieving federal marriage equality, it is still legal in more states than not to discriminate on the basis of gender identity (Human Rights Campaign, 2015). Lack of legal recourse in the face of employment and housing discrimination is a significant factor in the ongoing socioeconomic marginalization that transgender older adults continue to experience; enacting federal antidiscrimination laws that address gender identity and expression and sexual orientation would provide one avenue of recourse (Transgender Law & Policy Institute, 2012). Passage of the LGBT Elder Americans Act would amend the 1965 Older Americans Act to make it more responsive to the unique challenges that transgender older adults face by designating them a most vulnerable population (Human Rights Campaign, 2013). Beyond their instrumental value, such policies would also serve as guides to reduce the heterosexism and sexism inherent in social structures and institutions.
Conclusion and limitations
While this study provides new insights into depression among transgender older adults, it is important to recognize its limitations. The data is cross-sectional and was collected via agency mailing lists — those connected with agencies that serve sexual and gender minority older adults may be dissimilar from those not connected with such agencies. Partner agencies are located in major metropolitan areas for the most part; therefore, rural-dwelling transgender older adults and those living in small towns and medium sized cities may be underrepresented. As a result, these findings may not generalize beyond the current sample. Sampling bias is a distinct possibility: transgender older adults who responded to the research announcement may differ from those who did not respond. Similarly, Just who identifies as transgender in survey research may also be an issue; for example, some transgender older adults who have completed gender transition may no longer consider themselves to be transgender (Witten & Eyler, 2012).
The intersectional nature of social identities are contextualized through multiple levels and layers of associated stigmas situated with life course and lifespan dynamics (Dannefer & Daub, 2009). On top of transgender issues are the issues of age and gender bias in general. Older adults often experience discrimination against in many areas of their life, including seeking employment based on age, and female adults (regardless of birth sex) are victims of discrimination in employment and other settings based on gender. This highlights the difficulty and importance working to untangle the relative contribution of internalized stigma based on age and other significant identities that intersect with transgender identitities.
Limitations notwithstanding, this study makes a significant contribution to the knowledge base of social gerontology and community psychology. While emerging evidence has begun to outline the scope of depression among transgender older adults, the findings presented here extend our understanding of the nature of depression among a marginalized and vulnerable subgroup of older Americans – transgender older adults. General and minority stressors interact to exert negative impacts on the mental health of transgender individuals and communities. We must identify and illuminate pathways and mechanisms by which risk becomes embodied to manifest in health disparities. As has been noted by many scholars, finding cures for proximal causes of disease and disorders is necessary but insufficient to address health disparities – we must engage with social stigma as a fundamental cause. This is the challenge for community psychology.
Highlights.
Tests minority stress model identifying relative contributions of general and minority stress on mental health
Discusses stigma associated with gender, gender identity, age and impact on mental health
Identifies potential pathways of risk that may inform innovative resilience frameworks
Acknowledgments
Some research reported in this publication was supported in part by grants from the National Institute on Aging of the National Institutes of Health under Award Number R01AG026526 (Fredriksen-Goldsen, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, National Institute of Aging, The University of Utah, or the University of Washington.
Footnotes
The authors hereby attest that they have no conflict of interest regarding the research presented in this manuscript.
Contributor Information
Charles P. Hoy-Ellis, College of Social Work, University of Utah., Salt Lake City, UT, USA.
Karen I. Fredriksen-Goldsen, School of Social Work, University of Washington. Seattle, WA, USA.
References
- Aneshensel CS. Social stress: Theory and research. Annual Review of Sociology. 1992;18:15–38. [Google Scholar]
- Aneshensel CS. Toward explaining mental health disparities. Journal of Health and Social Behavior. 2009;50(4):377–394. doi: 10.1177/002214650905000401. [DOI] [PubMed] [Google Scholar]
- Bergdahl J, Bergdahl M. Perceived stress in adults: Prevalence and association of depression, anxiety and medication in a Swedish population. Stress and Health. 2002;18(5):235–241. doi: 10.1002/smi.946. [DOI] [Google Scholar]
- Blazer DG, Hybels CF. Origins of depression in later life. Psychological Medicine. 2005;35(9):1241–1252. doi: 10.1017/S0033291705004411. [DOI] [PubMed] [Google Scholar]
- Bockting WO, Miner MH, Swinburne Romine RE, Hamilton A, Coleman E. Stigma, mental health, and resilience in an online sample of the U.S. transgender population. American Journal of Public Health. 2013;103(5):943–951. doi: 10.2105/AJPH.2013.301241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York: Wiley; 1989. [Google Scholar]
- Budge SL, Adelson JL, Howard KAS. Anxiety and depression in transgender individuals: The roles of transition status, loss, social support, and coping. Journal of Consulting and Clinical Psychology. 2013;81(3):545–557. doi: 10.1037/a0031774. [DOI] [PubMed] [Google Scholar]
- Cairney J, Krause N. The social distribution of psychological distress and depression in older adults. Journal of Aging and Health. 2005;17(6):807–835. doi: 10.1177/0898264305280985. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. The State of Aging and Health in America 2013. Atlanta, GA: 2013. Retrieved from. http://www.cdc.gov/features/agingandhealth/state_of_aging_and_health_in_america_2013.pdf. [Google Scholar]
- Centers for Disease Control and Prevention and National Association of Chronic Disease Directors. The state of mental health and aging in America - Issue brief 2: Addressing depression in older adults: Selected evidence-based programs. Atlanta, GA: 2009. Retrieved from. http://www.cdc.gov/aging/pdf/mental_health_brief_2.pdf. [Google Scholar]
- Clements-Nolle K, Marx R, Guzman R, Katz M. HIV prevalence, risk behaviors, health care use, and mental health status of transgender persons: Implications for public health intervention. American Journal of Public Health. 2001;91(6):915–921. doi: 10.2105/ajph.91.6.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clements-Nolle K, Marx R, Katz M. Attempted suicide among transgender persons: The influence of gender-based discrimination and victimization. Journal of Homosexuality. 2006;51(3):53–69. doi: 10.1300/J082v51n03_04. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health & Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Cole S, Denny D, Eyler A, Samons S. Issues of transgender. In: Szuchman L, Muscarella F, editors. Psychological perspectives on human sexuality. Hoboken, NJ: John Wiley and Sons; 2000. pp. 149–195. [Google Scholar]
- Cole SW, Kemeny ME, Taylor SE, Visscher BR, Fahey JL. Accelerated course of human immunodeficiency virus infection in gay men who conceal their homosexual identity. Psychosom Med. 1996;58(3):219–231. doi: 10.1097/00006842-199605000-00005. [DOI] [PubMed] [Google Scholar]
- Conron KJ, Scott G, Stowell GS, Landers SJ. Transgender health in Massachusetts: Results from a household probability sample of adults. American Journal of Public Health. 2012;102(1):118–122. doi: 10.2105/AJPH.2011.300315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dannefer D, Daub A. Extending the interrogation: Life span, life course, and the constitution of human aging. Advances in Life Course Research. 2009;14(1–2):15–27. doi: 10.1016/j.alcr.2009.05.001. [DOI] [Google Scholar]
- Fabbre VD. Gender transitions in later life: A queer perspective on successful aging. The Gerontologist. 2015;55(1):144–153. doi: 10.1093/geront/gnu079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annual Review of Clinical Psychology. 2009;5:363–389. doi: 10.1146/annurev.clinpsy.032408.153621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Cook-Daniels L, Kim HJ, Erosheva EA, Emlet CA, Hoy-Ellis CP, Muraco A. Physical and mental health of transgender older adults: An at-risk and underserved population. The Gerontologist. 2013;54(3):488–500. doi: 10.1093/geront/gnt021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Kim HJ, Barkan SE, Muraco A, Hoy-Ellis CP. Health disparities among lesbian, gay male and bisexual older adults: Results from a population-based study. American Journal of Public Health. 2013;103(10):1802–1809. doi: 10.2105/AJPH.2012.301110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon AR, Meyer IH. Gender nonconformity as a target of prejudice, discrimination, and violence against LGB individuals. Journal of LGBT Health Research. 2007;3(3):55–70. doi: 10.1080/15574090802093562. 10.1080.15574090802093562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant JM, Mottet LA, Tanis J, Harrison J, Herman JL, Keisling M. Injustice at every turn: A report of the National Transgender Discrimination Survey. Washington, DC: 2011. Retrieved from. http://www.thetaskforce.org/downloads/reports/reports/ntds_full.pdf. [Google Scholar]
- Hankivsky O. Women’s health, men’s health, and gender and health: Implications of intersectionality. Social Science & Medicine. 2012;74(11):1712–1720. doi: 10.1016/j.socscimed.2011.11.029. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML. How does sexual minority stigma “get under the skin?”: A psychological mediation framework. Psychological Bulletin. 2009;135(5):707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. American Journal of Public Health. 2013;103(5):813–821. doi: 10.2105/AJPH.2012.301069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender noncomforming clients: An adaptation of the minority stress model. Professional Psychology: Research and Practice. 2012;43(5):460–467. doi: 10.1037/a0029597. [DOI] [Google Scholar]
- Hooper D, Coughlan J, Mullen MR. Structural equation modeling: Guidelines for determining model fit. Electronic Journal of Business Research Methods. 2008;6(1):53–60. [Google Scholar]
- Hopkin CR, Hoyle RH, Gottfredson NC. Maximizing the yield of small samples in prevention research: A review of general strategies and best practices. Prevention Science, Advanced online access. 2015 doi: 10.1007/s11121-014-0542-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoy-Ellis CP, Fredriksen-Goldsen KI. Lesbian, gay, & bisexual older adults: Linking internal minority stressors, chronic health conditions, and depression. Aging and Mental Health, Advance online access. 2016:1–10. doi: 10.1080/13607863.2016.1168362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoy-Ellis CP, Shiu C, Sullivan KM, Kim HJ, Sturges AM, Fredriksen-Goldsen KI. Prior military service, identity stigma, and mental health among transgender older adults. The Gerontologist. 2017;57(suppl 1):S63–S71. doi: 10.1093/geront/gnw173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyle RH, Gottfredson NC. Sample size considerations in prevention research applications of multilevel modeling and structural equation modeling. Prevention Science, Advance online access. 2014 doi: 10.1007/s11121-014-0489-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Human Rights Campaign. LGBT Elder Americans Act. Issue: Federal Advocacy. 2013 Retrieved from http://www.hrc.org/laws-and-legislation/federal-legislation/lgbt-elder-americans-act.
- Human Rights Campaign. Why the Equality Act? Resource. 2015 Retrieved from http://www.hrc.org//resources/entry/why-the-equality-act.
- Iacobucci D, Saldhana N, Deng X. A meditation on mediation: Evidence that structural equations models perform better than regressions. Journal of Consumer Psychology. 2007;12(2):139–153. doi: 10.1016/S1057-7408(07)70020-7. [DOI] [Google Scholar]
- Institute of Medicine. The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- Kenny ME, Hage SM. The next frontier: Prevention as an instrument of social justice. Journal of Primary Prevention. 2009;30(1):1–10. doi: 10.1007/s10935-008-0163-7. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer Publishing Company; 1984. [Google Scholar]
- LeBlanc AJ, Frost DM, Wight RG. Minority stress and stress proliferation among same-sex and other marginalized couples. Journal of Marriage and Family. 2015;77(1):40–59. doi: 10.1111/jomf.12160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H, Feng T, Rhodes AG. Assessment of the Chinese version of HIV and homosexuality related stigma scales. Sexually Transmitted Infections. 2009;85(1):65–69. doi: 10.1136/sti.2008.032714. [DOI] [PubMed] [Google Scholar]
- Lombardi E. Varieties of transgender/transsexual lives and their relationship with transphobia. Journal of Homosexuality. 2009;56(8):977–992. doi: 10.1080/00918360903275393. [DOI] [PubMed] [Google Scholar]
- Marmot MG, Stansfeld S, Patel C, North F, Head J, White I, Smith GD. Health inequalities among British civil servants: The Whitehall II study. The Lancet. 1991;337(8754):1387–1393. doi: 10.1016/0140-6736(91)93068-K. [DOI] [PubMed] [Google Scholar]
- Marmot MG, Wilkinson RG. Social determinants of health. 2nd. New York: Oxford University Press; 2006. [Google Scholar]
- Matsueda RL. Key advances in the history of structural equation modeling. In: Hoyle RH, editor. Handbook of structural equation modeling. New York: The Guilford Press; 2012. pp. 17–42. [Google Scholar]
- McEwen BS. Stress, adaptation, and disease. Allostasis and allostatic load. Annals of the New York Academy of Sciences. 1998;840:33–44. doi: 10.1111/j.1749-6632.1998.tb09546.x. [DOI] [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr J, Fassinger R. Measuring dimensions of lesbian and gay male experience. Measurement and Evaluation in Counseling and Development. 2000;33(2):66–90. [Google Scholar]
- Nurius PS, Hoy-Ellis CP. Stress effects and health. In: Franklin C, editor. Encyclopedia of Social Work Online. New York: NASW & Oxford University Press; 2013. Retrieved from http://socialwork.oxfordre.com/view/10.1093/acrefore/9780199975839.001.0001/acrefore-9780199975839-e-1045?rskey=f3iOcW&result=10. [DOI] [Google Scholar]
- Pachankis JE. The psychological implications of concealing a stigma: A cognitive-affective-behavioral model. Psychological Bulletin. 2007;133(2):328–345. doi: 10.1037/0033-2909.133.2.328. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Aneshensel CS, LeBlanc AJ. The forms and mechanisms of stress proliferation: The case of AIDS caregivers. Journal of Health & Social Behavior. 1997;38(3):223–236. [PubMed] [Google Scholar]
- Persson DI. Unique challenges of transgender aging: Implications from the literature. Journal of Gerontological Social Work. 2009;52(6):633–646. doi: 10.1080/01634370802609056. [DOI] [PubMed] [Google Scholar]
- Quinn DM, Williams MK, Quintana F, Gaskins JL, Overstreet NM, Pishori A, Chaudoir SR. Examining effects of anticipated stigma, centrality, salience, internalization, and outness on psychological distress for people with concealable stigmatized identities. PLoS One. 2014;9(5):e96977. doi: 10.1371/journal.pone.0096977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rosser BR, Oakes JM, Bockting WO, Miner M. Capturing the social demographics of hidden sexual minorities: An internet study of the transgender population in the United States. Sexuality Research & Social Policy. 2007;4(2):50–64. [Google Scholar]
- Springer KW, Hankivsky O, Bates LM. Gender and health: Relational, intersectional, and biosocial approaches. Social Science & Medicine. 2012;74(11):1661–1666. doi: 10.1016/j.socscimed.2012.03.001. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata: Release 12 (Vol. Stata) College Station, TX: StataCorp LP; 2011. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Mental Health Findings. Rockville, MD: 2013. Retrieved from. http://www.samhsa.gov/data/sites/default/files/2k12MH_Findings/2k12MH_Findings/NSDUHmhfr2012.htm#sec2–3. [Google Scholar]
- Thoits PA. Stress and health: Major findings and policy implications. Journal of Health & Social Behavior. 2010;51(Suppl):S41–S53. doi: 10.1177/0022146510383499. [DOI] [PubMed] [Google Scholar]
- Transgender Law & Policy Institute. Non-discrimination laws that include gender identity and expression. 2012 Retrieved from http://www.transgenderlaw.org/ndlaws/index.htm.
- U. S. Department of Health and Human Services. Healthy People 2020 Objectives: Lesbian, Gay, Bisexual, and Transgender Health. 2011 Retrieved from http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=25.
- U. S. Department of Health and Human Services. Healthy People 2020 Topics & Objectives: Older Adults. 2013 Retrieved from http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=31.
- U. S. Department of Health and Human Services. Lesbian, Gay, Bisexual, and Transgender Health. 2020 Topics & Objectives. 2016 Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bisexual-and-transgender-health/objectives.
- Valanis BG, Bowen DJ, Bassford T, Whitlock E, Charney P, Carter RA. Sexual orientation and health: Comparisons in the Women’s Health Initiative sample. Archives of Family Medicine. 2000;9(9):843–853. doi: 10.1001/archfami.9.9.843. [DOI] [PubMed] [Google Scholar]
- Wallace SP, Cochran SD, Durazo EM, Ford CL. The health of aging lesbian, gay and bisexual adults in California. Los Angeles, CA: 2011. Retrieved from. [PMC free article] [PubMed] [Google Scholar]
- Westland JC. Lower bounds on sample size in structural equation modeling. Electronic Commerce Research and Applications. 2010;9(6):476–487. [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: Findings from community studies. American Journal of Public Health. 2003;93(2):200–208. doi: 10.2105/AJPH.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witten TM, Eyler EA. Gay, lesbian, bisexual, and transgender aging: Challenges in research, practice, and policy. Baltimore, MA: Johns Hopkins University Press; 2012. [Google Scholar]
- World Health Organization. Depression. Mental health. 2012 Retrieved from http://www.who.int/mediacentre/factsheets/fs369/en/
- Zhang W, O’Brien N, Forrest JI, Salters KA, Patterson TL, Montaner JS, Lima VD. Validating a shortened depression scale (10 Item CES-D) among HIV-Positive people in British Columbia, Canada. PLoS One. 2012;7(7):e40793. doi: 10.1371/journal.pone.0040793. [DOI] [PMC free article] [PubMed] [Google Scholar]


