Abstract
AIDS stigmas delay HIV diagnosis, interfere with health care, and contribute to mental health problems among people living with HIV. While there are few studies of the geographical distribution of AIDS stigma, research suggests that AIDS stigmas are differentially experienced in rural and urban areas. We conducted computerized interviews with 696 men and women living with HIV in 113 different zip code areas that were classified as large-urban, small-urban, and rural areas in a southeast US state with high-HIV prevalence. Analyses conducted at the individual level (N = 696) accounting for clustering at the zip code level showed that internalized AIDS-related stigma (e.g., the sense of being inferior to others because of HIV) was experienced with greater magnitude in less densely populated communities. Multilevel models indicated that after adjusting for potential confounding factors, rural communities reported greater internalized AIDS-related stigma compared to large-urban areas, and that small-urban areas indicated greater experiences of enacted stigma (e.g., discrimination) than large-urban areas. The associations between anticipated AIDS-related stigma (e.g., expecting discrimination) and population density at the community-level were not significant. Results suggest that people living in rural and small-urban settings experience greater AIDS-related internalized and enacted stigma than their counterparts living in large-urban centers. Research is needed to determine whether low-density population areas contribute to or are sought out by people who experienced greater AIDS-related stigma. Regardless of causal directions, interventions are needed to address AIDS-related stigma, especially among people in sparsely populated areas with limited resources.
Keywords: Stigma, HIV/AIDS, Urban Health, Rural Health
Introduction
The stigmatization of AIDS is manifested in social distancing, avoidance, prejudice, discrimination, and self-devaluation. Negative attitudes toward and discrimination against people living with HIV remain entrenched across cultures (Kalichman et al., 2009; Lieber, Li, Wu, Rotheram-Borus, & Guan, 2006; Tsai et al., 2013b) and are not simply the result of misinformation (Wong, 2013). People living with HIV who experience greater AIDS-related stigma have poorer mental health and poorer medical outcomes (Rao et al., 2011; Tsai et al., 2013a; Vanable, Carey, Blair, & Littlewood, 2006). AIDS stigmas have been studied in relation to medication adherence, where the relationship between experiencing greater stigma and suboptimal antiretroviral therapy (ART) adherence is clearly established (Katz et al., 2013; Sweeney & Vanable, 2015). There are multiple dimensions to stigma and each has potential adverse health implications for people living with HIV. Earnshaw et al. (2013) proposed a model consisting of three distinct stigma mechanisms, specifically internalized, anticipated, and enacted stigma, each linked to different health outcomes. Internalized stigma reflects a sense of being less worthy or inferior to others due to having HIV and is directly associated with mental health outcomes including a sense of helplessness and denial of one’s diagnosis. Anticipated stigma, on the other hand, reflects how a person with HIV may expect to be mistreated and discriminated against in the future because they are HIV positive. Anticipated stigma may have its greatest impacts on medication adherence and attending health care appointments. Finally, enacted stigma represents past experiences of prejudice and discrimination, which are theorized to manifest in physical debilitation.
While widely observed, the geographical distribution of AIDS stigma is not uniform. For instance, studies suggest that stigma may be more prevalent and experienced with greater magnitude in rural settings compared to urban areas. For example, Gonzalez, Miller, Solomon, Bunn, and Cassidy (2009) found that people in rural areas perceived greater concerns with disclosure, public attitudes toward AIDS, personal negative self-image, and enacted stigma. For people in rural areas of the United States, experiences with AIDS-related discrimination occur with impacts on mental health including poorer life satisfaction and a lack of social support (Heckman, Somlai, Kalichman, Franzoi, & Kelly, 1998), and perceived community stigma and internalized stigma are related to depression (Vyavaharkar et al., 2010). In rural communities AIDS stigmas also interfere with access to transportation, raise concerns about confidentiality, and inhibit talking openly with care providers (for a review see Pellowski, 2013). People living in rural areas of the southeastern United States are more likely to avoid HIV testing and are more likely diagnosed with later stage HIV infection, risking increased morbidity, mortality, and forward HIV transmission (Reif, Golin, & Smith, 2005; Trepka et al., 2014; Weis, Liese, Hussey, Gibson, & Duffus, 2010). AIDS-related enacted stigma experiences create significant barriers to accessing care among people living with HIV in rural areas (Whetten-Goldstein, Nguyen, & Heald, 2001).
Previous research on the geographical distribution of HIV infection across urban and rural areas also finds reliable associations between socio-demographic characteristics and the distribution of AIDS-related health disparities (Kalichman et al., 2011). For example, Niyonsenga et al. (2013) found that poverty at the zip code level predicted AIDS cases in urban areas of Florida, but poverty was not related to AIDS in rural areas. Population density at the zip code level also differentiates life expectancies of Latinos differently for those living with HIV compared to the general Latino population (Sheehan et al., 2015). Specifically, greater population density offers advantages for longevity among Latinos possibly due to greater access to social resources. In a study conducted in the northeastern US, Gonzalez et al. (2009) found that women living with HIV in rural communities experience greater concerns about HIV disclosure than women in urban settings. In contrast, the opposite relationship was true for HIV positive men, with those living in urban settings experiencing greater HIV disclosure concerns than men in rural communities.
The current study examined variations in the three AIDS-related stigma mechanisms proposed by Earnshaw et al. (2013), namely internalized, anticipated and enacted stigma, in relation to residential population density. We examined AIDS-related stigma in a sample of men and women living with HIV in and around a large-urban, small-urban, and rural areas of a state in the southeastern US. This study extends previous research on stigma dimensions in relation to community size that was conducted in the northeastern US (Gonzalez et al., 2009). In addition, we controlled for potential confounding factors including depression, which overlaps with internalized stigma (Friedman, Terras, Zhu, & McCallum, 2004; Patton, 1991) and medical mistrust, which overlaps with anticipated and enacted stigma (Eaton et al., 2015). We therefore tested the hypothesis that population density would be associated with internalized, anticipated and enacted AIDS-related stigmas over and above relevant demographic characteristics, depression symptoms, and medical mistrust.
Methods
Participants and Setting
Participants were 473 men and 223 women living with HIV infection in the state of Georgia. While 28% of the US population lives in the nine states representing the south, 40% of AIDS diagnoses occur in this region. Georgia has the 5th highest number of people diagnosed with AIDS in the US and the 9th highest rate of AIDS cases per 100,000 persons. There were an estimated 51,510 persons living with HIV infection in Georgia in 2013, with one in three living outside of metropolitan Atlanta (Georgia Department of Public Health, 2013).
Measures
Participants completed measures of demographic, social and health characteristics, depression symptoms, medical mistrust, and AIDS-related stigma. Measures were collected anonymously with assistance provided to participants as requested.
Demographic and health characteristics
Participants were asked their gender, age, years of education, income, ethnicity, employment status, and the zip code for their current residence. Participants also reported the year they first tested HIV positive and whether they were currently taking ART. We also asked participants their current CD4 cell count and their most recent HIV RNA viral load, indicating whether the result of their most recent viral load test was either ‘detectable’ or ‘undetectable’. This format for collecting self-report CD4 cell counts and HIV viral load has been found valid when compared to medical record chart abstractions (Kalichman, Rompa, & Cage, 2000).
Depression symptoms
The Cognitive-Affective subscale of Center for Epidemiological Studies-Depression Scale (CES-D) was used to assess current depression symptomatology (Radloff, 1977). We used items reflecting cognitive and affective symptoms of depression to avoid confounding depression with the physical symptoms of advancing HIV disease. Participants rated the frequency with which they have experienced 12 depression symptoms over the course of one week (e.g., “I felt that I could not shake off the blues even with help from my family or friends”, “I thought my life had been a failure”). The 12 depression symptoms were rated on a scale from 0 (0 days) to 3 (5–7 days). Items were summed into a composite score, alpha =.87.
Medical mistrust
Participants completed 12 items from the Medical Mistrust Index (LaVeist, Isaac, & Williams, 2009). The items reflect a broad sense of mistrust in medical providers. Example items include “Patients have sometimes been deceived or misled by healthcare providers”, “When healthcare providers make mistakes they usually cover it up”, and “Healthcare providers have sometimes done harmful things to patients without their knowledge”. Items are responded to on a 5-point scale, 1 = Strongly agree, 5 = Strongly disagree, and scores were calculated taking the mean response, alpha = .83.
AIDS-related stigmas
We used a measure developed by Earnshaw et al. (Earnshaw & Chaudoir, 2009; Earnshaw et al., 2013) to assess three dimensions of AIDS-related stigma from the perspective of individuals living with HIV. First, we assessed internalized AIDS stigma using a five item composite. Internalized AIDS-related stigma reflects the sense of being less or inferior to others directly due to having HIV. Example items include “I feel I’m not as good as others because I have HIV” and “Having HIV makes me feel like I'm a bad person”, responded to on a 5-point scale 1 = Strongly agree, 5 = Strongly disagree. Second, we assessed anticipated stigma using nine items that indicate the degree to which a person with HIV expects to be mistreated and discriminated against because they are HIV positive. Example anticipated stigma items include “Because of my HIV status, community or social workers will discriminate against me”, “Because of my HIV status, family members will avoid me”, and “Because of my HIV status, healthcare workers will avoid touching me”, responded to on a 5-point scale 1 = Very unlikely, 5 = Very likely. Finally, we used eight items indicating enacted AIDS stigma, representing experiences of prejudice and discrimination across social spheres that are directly associated with living with HIV and experienced since being diagnosed with HIV infection. Example enacted stigma items include “People have discriminated against me because of my HIV status”, “People have avoided touching me because of my HIV status” and “Because of my HIV status, family members have looked down on me”, responded to dichotomously as 0 = No this is not true for me, or 1 = Yes this is true for me. For the internalized and anticipated AIDS stigma scales we calculated the mean responses and for enacted stigma we summed the occurrence of experiences. The internalized, anticipated and enacted AIDS stigma scales were internally consistent, alphas = .91, .92, .86, respectively.
Procedures
We conducted a cross-sectional survey of people living with HIV in and around Atlanta and Macon, GA during the period between November 2014 and August 2015. Participants were recruited from infectious disease clinics and community services in Atlanta (N = 481) and Macon (N = 215), cities with poverty rates of 21% and 26%, respectively. Individuals came to one of two research sites, one in Atlanta and one in Macon, to complete the study measures. The Atlanta site was established in 1996 as a community-based research program located in central downtown within walking distance of major AIDS service providers and infectious disease clinics serving Atlanta and surrounding areas. The Macon site was located within a public HIV care center that serves the North-Central Georgia health district. People living with HIV were notified through postings as well as direct contacts at local infectious disease clinics and AIDS-related social services, as well as word-of-mouth that they could obtain $20 for completing an anonymous survey. The only entry criteria to participation in the study were age 18 and older and proof of being HIV positive. Participants were required to prove their HIV positive status by presenting a form of photo-identification along with a name matching ART prescription, medication bottle, HIV clinic card, or other verification of HIV status. A total of 696 individuals completed surveys using a computer-assisted administration on tablet computers. The university Institutional Review Boards approved all of the study procedures.
Data Analyses
We used participant zip codes to determine the population density of their current place of residence. Population density was defined as persons living per square mile and was obtained from the 2010 US census. The 696 participants reported living in 113 different zip code areas in the state of Georgia. The number of participants living in zip code areas ranged from 1 to 42. At the community level, we categorized zip code locations based on cut-offs of population density used by the US government to define zip codes (Data, 2015): Large-urban 3,000+ persons per square mile, small-urban 1,000 to 3,000 persons per square mile, and rural less than 1,000 persons per square mile. Individuals living in metropolitan Atlanta (population density 3,199 people per square mile) were therefore defined as living in large-urban areas, and persons living in areas outside of downtown Atlanta as well as in the city of Macon (population density 1,644 people per square mile) were defined as small-urban, whereas individuals in more sparsely populated communities were defined as living in rural areas. Data were structured as follows: (a) 150 individuals nested in 49 zip codes defined as large-urban, (b) 246 individuals nested in 36 zip codes defined as small-urban, (c) 300 individuals nested in 28 zip codes defined as rural communities.
Individual-level effects
Because individual-level data were not independent with respect to population density, analyses performed for individual participants within zip codes were subject to inflated error. We therefore conducted generalized linear models with robust variance estimates to adjust for non-independence in the clustering that occurred within zip codes (Williams, 2000; White, 1994).
Community-level effects
We constructed models to account for clustering within zip code areas. We conducted fixed-effects restricted maximum likelihood models (Peugh & Enders, 2005) tested in SPPS (v. 23) Mixed Models. Tests for fixed effects are reported with parameter estimates examined for differences between the three community groupings. All predictor variables were grand mean centered for multilevel models. Bivariate models were tested for participant characteristics across the three levels of community types. For multivariate models predicting internalized stigma, depression scores were included among covariates. For models predicting anticipated and enacted stigma, we controlled for perceived medical mistrust. For all analyses, we used the log-transformed value of population per square mile as a continuous measure to adjust skew and restrict the influence of outliers. All analyses defined statistical significance as p < .05.
Results
The sample consisted of two-thirds men and nearly 90% of participants were African-American, with 8% Caucasian, and 2% Hispanic. On average, participants were in their late 40’s, had 12.6 years of education, and had been living with an HIV diagnosis for 15 years (see Table 1).
Table 1.
Unadjusted and adjusted associations between population density and participant characteristics at the individual level (N = 696).
| Unadjusted | Adjusted | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| M | SD | β | se | β | se | |
| Age | 49.6 | 10.3 | −.007** | .002 | −.004 | .002 |
| Men (n, %) | 473 | 68% | ||||
| Women (n, %) | 223 | 32% | −.029 | .044 | −.004 | .043 |
| Education | 12.6 | 1.8 | .018 | .011 | .019 | .011 |
| Years HIV+ | 15.1 | 8.7 | −.008** | .002 | −.005 | .002 |
| Depression | 7.9 | 6.4 | −.007 | .003 | −.001 | .003 |
| Medical Mistrust | 2.6 | 0.7 | −.003 | .029 | .039 | .032 |
| Internalized Stigma | 2.3 | 1.1 | −.088** | .019 | −.091** | .021 |
| Anticipated Stigma | 2.1 | 0.9 | −.022 | .023 | .033 | .029 |
| Enacted Stigma | 1.2 | 1.9 | −.015 | .011 | −.003 | .014 |
Note: Unadjusted parameters are bivariate and adjusted parameters include all variables in a simultaneous model.
p < .05,
p < .01.
Individual-level associations between population density and participant characteristics
Associations between participant characteristics and population density within zip code areas at the individual-level are shown in Table 1. Unadjusted bivariate analyses with robust variance estimates indicated that age, years living with HIV and internalized AIDS-related stigma were associated with population density; individuals living in less densely populated zip codes were older, living with HIV for more years, and experiencing more internalized stigma. When all variables were included in a simultaneous model, only internalized stigma was significantly associated with population density.
Community-level associations between population density and participant characteristics
Table 2 shows the characteristics of communities defined by numbers of individuals living per square mile. Results of models adjusting for clustering show that rural communities were characterized as older in age and greater number of years since testing HIV positive. In addition, there was a significant association between community size and where individuals had tested HIV positive, showing a tendency for persons living in small-urban and rural areas to have tested HIV positive in Atlanta, whereas a majority of individuals living in Atlanta had tested HIV positive in a different area of Georgia. As shown in Table 3, AIDS-related internalized stigma in small-urban and rural communities was greater than internalized stigma in large-urban areas. Differences for anticipated and enacted stigma were not statistically significant.
Table 2.
Demographic and health characteristics of people living with HIV in large-urban, small-urban, and rural areas.
| Large-Urban | Small-Urban | Rural | |||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Characteristic | M | SD | M | SD | M | SD | F |
| Age | 46.2a | 12.3 | 47.1a | 10.0 | 49.0b | 9.49 | 5.1** |
| Years of education | 12.3 | 1.9 | 12.3 | 1.9 | 12.6 | 1.7 | 1.3 |
| Years since testing HIV+ | 13.7a | 8.9 | 14.9 | 8.3 | 16.1b | 8.7 | 3.7** |
| CD4 cell count | 660.6 | 562.3 | 682.5 | 511.5 | 625.9 | 442.9 | 0.7 |
| Depression symptoms | 9.9 | 6.0 | 8.4 | 5.5 | 9.0 | 5.4 | 1.2 |
| Medical mistrust | 3.3 | 0.6 | 3.3 | 0.7 | 3.3 | 0.7 | 0.4 |
|
|
|||||||
| N | % | N | % | N | % | ||
|
|
|||||||
| Men | 101 | 68 | 159 | 65 | 213 | 71 | |
| Women | 49 | 32 | 87 | 35 | 87 | 29 | 1.13 |
| African-American | 127 | 85 | 223 | 90 | 276 | 91 | 2.59 |
| Currently unemployed | 115 | 77 | 194 | 77 | 249 | 82 | 0.77 |
| Place tested HIV + | |||||||
| Atlanta | 34 | 23 | 124 | 50 | 204 | 68 | |
| Georgia, not Atlanta | 92 | 62 | 86 | 35 | 28 | 9 | |
| Outside Georgia | 22 | 15 | 39 | 16 | 70 | 23 | 11.04** |
| Currently treated with ART | 128 | 86 | 214 | 86 | 254 | 84 | 0.17 |
| CD4 count < 200 cell/cc | 11 | 13 | 18 | 10 | 26 | 10 | 0.38 |
| Viral load undetectable | 97 | 76 | 192 | 85 | 261 | 89 | 0.47 |
Note:
p < .05,
p < .01; Means with different superscripts are significantly different.
Table 3.
Univariate models predicting stigma scores at large urban, small urban, and rural community levels.
| Large-Urban | Small-Urban | Rural | |||||
|---|---|---|---|---|---|---|---|
|
|
|||||||
| Stigma Score | M | SD | M | SD | M | SD | F |
| Internalized stigma | 3.3a | 1.2 | 3.7b | 1.1 | 3.8b | 1.1 | 8.81** |
| Anticipated stigma | 2.2 | 0.9 | 2.1 | 0.8 | 2.1 | 0.9 | 1.02 |
| Enacted stigma | 1.4 | 2.1 | 1.0 | 1.7 | 1.3 | 2.0 | 2.36+ |
Note:
p < .10,
p < .01.
Multivariate community-level models predicting dimensions of AIDS-related stigma
Figure 1 shows the geographical dispersion of internalized AIDS-related stigma across the communities represented by participant zip codes. The image illustrates that areas outside metropolitan Atlanta present greater internalized AIDS-related stigma, relative to small-urban communities outside of both cities. The associations of AIDS-related stigma and community defined by population density (i.e., large-urban, small-urban, rural) were tested in multilevel models. All models included participant age, gender, education, and years since testing HIV positive as covariates. In addition, depression was controlled in the model of internalized stigma and medical mistrust was controlled in models for anticipated and enacted stigma (see Table 4).
Figure 1.
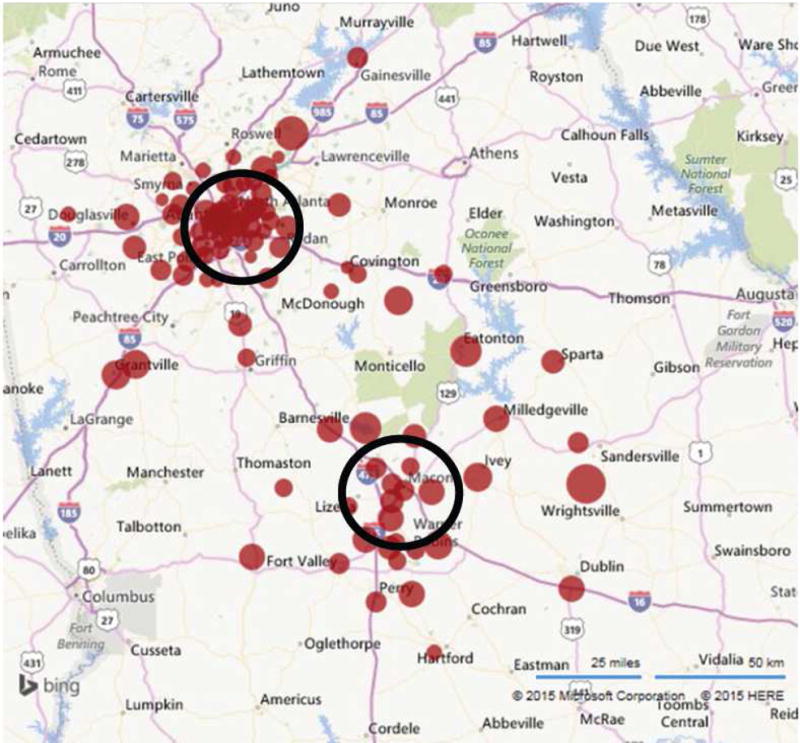
Geographical distribution of internalized stigma across northern and central Georgia. Larger dots represent greater mean internalized AIDS-related stigma scores. Black perimeters represent approximately 25-mile diameter encircling Atlanta and Macon center cities.
Table 4.
Multivariable multilevel models predicting internalized, anticipated, and enacted stigma scores at the rural, small urban, and large urban community levels.
| Community Level Models
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Internalized Stigma | Anticipated Stigma | Enacted Stigma | |||||||
| Variable | β | se | Wald X2 | β | se | Wald X2 | β | se | Wald X2 |
| Age | −.012 | .004 | −2.6** | −.009 | .003 | 2.47* | −.015 | .007 | 1.91+ |
| Gender | .021 | .087 | 0.24 | .029 | .071 | 0.40 | .186 | .151 | 1.22 |
| Education | −.008 | .021 | 0.39 | −.020 | .017 | 1.16 | .032 | .037 | 0.86 |
| Years HIV+ | −.001 | .005 | 0.27 | −.008 | .004 | 1.87 | .006 | .009 | 0.69 |
| Depression | .064 | .006 | 10.46** | ||||||
| Medical Mistrust | .482 | .046 | 10.38** | .990 | .098 | 10.04** | |||
| Community | |||||||||
| Rural | .376 | .106 | 3.53** | −.010 | .087 | 0.12 | .142 | .185 | 0.77 |
| Small-Urban | .076 | 0.90 | 0.84 | −.139 | .073 | 1.88+ | −.330 | .156 | 2.11* |
| Large-Urban | Reference | Reference | Reference | ||||||
Note: =
p < .06,
p < .05,
p < .01.
In the first model participant age and depression scores were significantly related to internalized stigma. In addition, there was a significant association between community size and internalized stigma, F = 6.39, p <.01; rural communities indicated greater internalized stigma over and above the other variables in the model. For Anticipated stigma, age was again a significant predictor as well as medical mistrust. However, the association for community size was not significant, F = 2.0, p > .1. Age marginally predicted AIDS-related enacted stigma and medical mistrust significantly predicted enacted stigma as did community size, F = 3.72, p < .05; small-urban areas indicated greater enacted stigma scores. Models that examined rural communities entered as the reference category did not indicate differences with small-urban areas (coefficients not shown).
Discussion
Results demonstrated that internalized AIDS stigma is associated with population density, with individuals living in small-urban and rural areas indicating greater internalized AIDS-related stigma than people living with HIV in large-urban areas. In addition, communities defined as small-urban areas indicated greater enacted stigma than large-urban communities. However, communities defined by population density did not differ in terms of anticipated stigma. The associations for internalized stigma were therefore observed when population density was treated as a continuous variable conducted at the individual-level as well as when population density was used to define large-urban, small-urban, and rural communities. These findings are consistent with past research showing enacted as well as internalized stigma are associated with the size of communities, with stigmas along both dimensions being greater in more rural areas (Gonzalez et al., 2009).
Analyses conducted at the individual and community levels showed similar patterns of associations. In both cases, we found that population density was related to internalized stigma over and above demographic characteristics including depression symptoms. Overall, population density contributed uniquely to the explained variance at the individual and community levels. These results suggest that the sense of being less worthy or inferior to others as a result of having HIV occurs at a greater magnitude among individuals living with HIV outside of urban centers. However, we only observed an association between population density and enacted stigma at the community level, with people living in small-urban areas reporting less enacted stigma than large-urban areas. The participant characteristics included among our measures do not shed light on protective mechanisms that may account for less enacted stigma in small-urban areas, indicating the need for additional research.
In this study internalized stigma varied by the population density of the area in which people lived. One explanation for this finding is that people with greater internalized stigma migrate to more rural areas, whereas people with less stigmatized self-perceptions are drawn to urban centers. We observed a pattern of relocating after testing HIV positive that suggests people do move out of the city when tested in Atlanta, while those who tested HIV positive outside the city migrated in. In addition, there were no clear patterns of geographical differences in enacted and anticipated stigma. Thus, people with less internalized stigma may seek the multiple social and supportive resources available in the city, while those with greater internalized stigma may seek environments in which they can more easily conceal their HIV status. Future research is needed to determine whether AIDS stigmas are a precursor to or the result of living in areas of lower or higher population density. Also in need of further research are the likely intersections of AIDS-related stigma with other stigmatized attributes and discrimination that vary geographically, such as racism, homophobia, and stigmatization of substance abuse. Specifically, our interpretation of findings for AIDS-related stigma may be due to intersecting stigmas not assessed in this study.
Results of the current study should be interpreted in light of the methodological limitations. Although we sampled a broad geographical area within a state with high HIV prevalence, the sample was still one of convenience and cannot be considered representative of people living with HIV in the state of Georgia. For example, while 9% of the state population and 6% of people with HIV in Georgia are Hispanic, our sample was only 2% Hispanic. In addition, the study was conducted in just one state in the southeastern United States, and is therefore also geographically constrained. While there were small-urban and rural communities located around both cities, all of the large-urban communities were in Atlanta. Thus, differences observed in our models may reflect characteristics of the cities beyond population density that were not assessed. We also relied on self-reported measures for all of the variables in this study. Although we used state-of-the-science measures delivered by computerized interviews, the results are still subject to reporting biases. Finally, the study design was cross-sectional and therefore does not allow for directional or causal inferences among variables. With these limitations in mind, we believe that the current study findings have implications for designing interventions aimed to address AIDS-related stigma.
There are few interventions designed to reduce HIV stigma or alleviate the adverse effects of stigma on people living with HIV. Although AIDS-related stigma is ubiquitous, stigma has not been adequately addressed in interventions. People who experience AIDS-related stigma may not label their experiences as stigmatizing, and individuals who hold negative attitudes toward people living with HIV may not recognize their beliefs as stigmatizing. One intervention approach that demonstrated promise in addressing stigma was tested in the southern United States. Barroso et al. (2014) tested the effects of a video that depicted women living with HIV and managing the stigma they had experienced. The video was delivered over a mobile device and demonstrated reductions in internalized stigma compared to a control condition that did not receive a stigma reduction intervention. These findings are intriguing because of the low cost of the intervention and the potential for broad access among people living in rural areas. However, implementing interventions in small-urban and rural communities will face unique challenges with respect to reaching, enrolling and retaining populations in need of intervention. People outside of urban centers will have less exposure to billboards, posters, and other forms of intervention advertisement. In addition, people who experience greater internalized and enacted stigma may experience greater fear of encountering others in one's social network for group-based interventions.
Mobile health offers avenues that may address the stigma-related barriers to intervention. Video-based interventions, as noted above, can now be delivered to mobile devises and effectively overcome barriers posed by distance and transportation. More intense interventions, such as interactive groups and counseling, can also be delivered using remote communication technologies such as telephones and video-phones (Marhefka, Fuhrmann, Gilliam, Lopez, & Baldwin, 2012). Alternatively, less intense interventions such as brief messages and ongoing supportive contact can be achieved with people in remote places using interactive text messaging systems (Lester et al., 2010). With new technologies improving our ability to reach people outside urban centers, research is needed to take advantage of these opportunities and develop efficacious interventions to address AIDS-related stigma designed to reach individuals residing across geographic areas.
Acknowledgments
Funding
This research was supported by National Institute of Alcohol Abuse and Alcoholism Grants R01-AA021471 and R01-AA023727.
Footnotes
The authors declare no conflicts of interest.
The University of Connecticut and Mercer University Institutional Review Boards approved all of the study procedures. All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
All participants provided informed consent in compliance with conducting self-administered anonymous surveys.
References
- Barroso J, Relf MV, Williams MS, Arscott J, Moore ED, Caiola C, Silva SG. A randomized controlled trial of the efficacy of a stigma reduction intervention for HIV-infected women in the Deep South. AIDS Patient Care and STDs. 2014;28(9):489–498. doi: 10.1089/apc.2014.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Data G. Rural Urban Suburban Data. 2015 Retrieved from http://greatdata.com/rural-urban-data.
- Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS and Behavior. 2009;13(6):1160–1177. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV Stigma Mechanisms and Well-Being Among PLWH: A Test of the HIV Stigma Framework. AIDS and Behavior. 2013;17(5):1785–1795. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton LA, Driffin DD, Kegler C, Smith H, Conway-Washington C, White D, Cherry C. The role of stigma and medical mistrust in the routine health care engagement of black men who have sex with men. American Journal of Public Health. 2015;105(2):e75–82. doi: 10.2105/AJPH.2014.302322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman AS, Terras A, Zhu W, McCallum J. Depression, negative self-image, and suicidal attempts as effects of substance use and substance dependence. Journal of Addictive Disorders. 2004;23(4):55–71. doi: 10.1300/J069v23n04_05. [DOI] [PubMed] [Google Scholar]
- Georgia Departmemnt of Public Health. o. P. HIV Surveillance Summary Georgia, 2013. 2013 Available at https://dph.georgia.gov/georgias-hivaids-epidemiology-surveillance-section.
- Gonzalez A, Miller CT, Solomon SE, Bunn JY, Cassidy DG. Size matters: community size, HIV stigma, & gender differences. AIDS and Behavior. 2009;13(6):1205–1212. doi: 10.1007/s10461-008-9465-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman TG, Somlai AM, Kalichman SC, Franzoi SL, Kelly JA. Psychosocial differences between urban and rural people living with HIV/AIDS. Journal of Rural Health. 1998;14(2):138–145. doi: 10.1111/j.1748-0361.1998.tb00615.x. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Pellowski J, Kalichman MO, Cherry C, Detorio M, Caliendo AM, Schinazi RF. Food insufficiency and medication adherence among people living with HIV/AIDS in urban and peri-urban settings. Prevention Science. 2011;12(3):324–332. doi: 10.1007/s11121-011-0222-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. Journal of Nervous and Mental Disorders. 2000;188(10):662–670. doi: 10.1097/00005053-200010000-00004. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Cloete A, Ginindza T, Mthembu P, Cherry C, Cain D. Measuring AIDS stigmas in people living with HIV/AIDS: The Internalized AIDS-Related Stigma Scale. AIDS Care. 2009;21(1):87–93. doi: 10.1080/09540120802032627. [DOI] [PubMed] [Google Scholar]
- Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, Tsai AC. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. Journal of the International AIDS Society. 2013;16(3 Suppl 2):18640. doi: 10.7448/IAS.16.3.18640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVeist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health Services Research. 2009;44(6):2093–2105. doi: 10.1111/j.1475-6773.2009.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lester RT, Ritvo P, Mills EJ, Kariri A, Karanja S, Chung MH, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): a randomised trial. Lancet. 2010;376(9755):1838–1845. doi: 10.1016/S0140-6736(10)61997-6. [DOI] [PubMed] [Google Scholar]
- Lieber E, Li L, Wu Z, Rotheram-Borus MJ, Guan J. HIV/STD stigmatization fears as health-seeking barriers in China. AIDS and Behavior. 2006;10(5):463–471. doi: 10.1007/s10461-005-9047-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marhefka S, Fuhrmann H, Gilliam P, Lopez B, Baldwin J. Interest in, concerns about, and preferences for potential video-group delivery of an effective behavioral intervention among women living with HIV. AIDS and Behavior. 2012;16(7):1961–1969. doi: 10.1007/s10461-011-0040-x. [DOI] [PubMed] [Google Scholar]
- Niyonsenga T, Trepka MJ, Lieb S, Maddox LM. Measuring socioeconomic inequality in the incidence of AIDS: rural-urban considerations. AIDS and Behavior. 2013;17(2):700–709. doi: 10.1007/s10461-012-0236-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton W. Relationship between self-image and depression in adolescents. Psychological Reports. 1991;68(3 Pt 1):867–870. doi: 10.2466/pr0.1991.68.3.867. [DOI] [PubMed] [Google Scholar]
- Pellowski JA. Barriers to care for rural people living with HIV: a review of domestic research and health care models. Journal of the Association of Nurses in AIDS Care. 2013;24(5):422–437. doi: 10.1016/j.jana.2012.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peugh JL, Enders C. Using the SPSS Mixed procedrue to fit cross-sectional and longitudinal multilevel models. Educational and Psychological Measurement. 2005;65:717–741. [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general populatio. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rao D, Feldman BJ, Fredericksen RJ, Crane PK, Simoni JM, Kitahata MM, Crane HM. A Structural Equation Model of HIV-Related Stigma, Depressive Symptoms, and Medication Adherence. AIDS and Behavior. 2011;16:711–716. doi: 10.1007/s10461-011-9915-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reif S, Golin CE, Smith SR. Barriers to accessing HIV/AIDS care in North Carolina: rural and urban differences. AIDS Care. 2005;17(5):558–565. doi: 10.1080/09540120412331319750. [DOI] [PubMed] [Google Scholar]
- Sheehan DM, Trepka MJ, Fennie KP, Dillon FR, Madhivanan P, Maddox LM. Neighborhood Latino ethnic density and mortality among HIV-positive Latinos by birth country/region, Florida, 2005–2008. Ethnicity and Health. 2015;21:268–283. doi: 10.1080/13557858.2015.1061104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweeney SM, Vanable PA. The Association of HIV-Related Stigma to HIV Medication Adherence: A Systematic Review and Synthesis of the Literature. AIDS and Behavior. 2015;20:29–50. doi: 10.1007/s10461-015-1164-1. [DOI] [PubMed] [Google Scholar]
- Trepka MJ, Fennie KP, Sheehan DM, Lutfi K, Maddox L, Lieb S. Late HIV diagnosis: Differences by rural/urban residence, Florida, 2007–2011. AIDS Patient Care and STDs. 2014;28(4):188–197. doi: 10.1089/apc.2013.0362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Bangsberg DR, Kegeles SM, Katz IT, Haberer JE, Muzoora C, Weiser SD. Internalized stigma, social distance, and disclosure of HIV seropositivity in rural Uganda. Annals of Behavioral Medicine. 2013b;46(3):285–294. doi: 10.1007/s12160-013-9514-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanable PA, Carey MP, Blair DC, Littlewood RA. Impact of HIV-related stigma on health behaviors and psychological adjustment among HIV-positive men and women. AIDS and Behavior. 2006;10(5):473–482. doi: 10.1007/s10461-006-9099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyavaharkar M, Moneyham L, Corwin S, Saunders R, Annang L, Tavakoli A. Relationships between stigma, social support, and depression in HIV-infected African American women living in the rural Southeastern United States. Journal of the Association of Nurses in AIDS Care. 2010;21(2):144–152. doi: 10.1016/j.jana.2009.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weis KE, Liese AD, Hussey J, Gibson JJ, Duffus WA. Associations of rural residence with timing of HIV diagnosis and stage of disease at diagnosis, South Carolina 2001–2005. Journal of Rural Health. 2010;26(2):105–112. doi: 10.1111/j.1748-0361.2010.00271.x. [DOI] [PubMed] [Google Scholar]
- Whetten-Goldstein K, Nguyen TQ, Heald AE. Characteristics of individuals infected with the human immunodeficiency virus and provider interaction in the predominantly rural Southeast. Southern Medical Journal. 2001;94(2):212–222. [PubMed] [Google Scholar]
- White H. Estimation, Inference, and Specification Analysis. New York: Cambridge Press; 1994. [Google Scholar]
- Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000;56:645–646. doi: 10.1111/j.0006-341x.2000.00645.x. [DOI] [PubMed] [Google Scholar]
- Wong LP. Prevalence and factors associated with HIV/AIDS-related stigma and discriminatory attitudes: a cross-sectional nationwide study. Preventive Medicine. 2013;57(Suppl):S60–63. doi: 10.1016/j.ypmed.2013.03.013. [DOI] [PubMed] [Google Scholar]


