Abstract
Initial research into seroadaptive strategies suggests that, individually, they are potentially effective behavioral methods to reduce risk of HIV transmission. Combining strategies, therefore, has the potential to increase risk reduction. The aim of this study was to determine how gay and bisexual men (GBM) combine strategies. To this end, a total of 774 sexually active GBM, aged ≥16 years, in Metro Vancouver, Canada were recruited. Stratified by self-reported HIV status, latent class analysis of self-reported condom use, strategic positioning, anal sex avoidance, serosorting, viral-load sorting, and withdrawal were conducted. Multinomial logistical regression identified explanatory variables of class membership (i.e., sensation seeking, treatment optimism, sexual altruism, relationship status, number of partners, anal sex preference). Four latent classes were identified: Condom Users, Multiple Prevention Users, Viral-Load Sorters, and Serosorters. The majority of HIV-negative/unknown men (72%) and a large proportion of HIV-positive men (42%) belonged to the Condom Users class. Class membership was associated with age, relationship status, treatment optimism, sexual altruism, sensation seeking, number of recent male anal sex partners, and recent condomless anal sex with a serodiscordant or unknown-status partner. Understanding these distinct patterns allows for tailored interventions addressing GBM’s sexual health needs.
Keywords: Seroadaptation, Latent Class Analysis, Gay and Bisexual Men, HIV
INTRODUCTION
Since the beginning of the HIV epidemic, North American gay, bisexual, and other men who have sex with men have been at a disproportionately higher risk for HIV infection compared to other North American men and women. Providing a partial explanation for this epidemic, a 2010 meta-analysis comparing condomless anal sex (CAS) to vaginal sex estimated that the per-contact probability of HIV-transmission was approximately 18 times greater during CAS (Baggaley, White, & Boily, 2010). However, the authors of that analysis, along with other commentators (Grulich & Zablotska, 2010), have noted that the risk for HIV transmission during CAS may be greatly reduced by biomedical interventions (Cohen et al., 2011; Grant et al., 2010; Roland et al., 2005) and associated seroadaptive practices (Vallabhaneni et al., 2012).
Seroadaptive practices consist of a range of sexual behaviors which take into account the known, perceived, or assumed HIV status (Jin et al., 2012; McFarland et al., 2011, 2012; Snowden, Wei, McFarland, & Raymond, 2014) or viral-load status (Cassels & Katz, 2013; Davidovich, van den Boom, Witlox, & Stolte, 2011; Horvath, Smolenski, Iantaffi, Grey, & Rosser, 2012; Mitchell, 2013) of individuals and their partners. While seroadaptive behavior may include avoiding any sexual intercourse with HIV-positive partners, the present study focuses specifically on seroadaptive behaviors that respond to risk associated with anal sex between serodiscordant or unknown-status partners (i.e., condom use, strategic positioning, anal sex avoidance, serosorting, viral-load sorting, withdrawal). This focus acknowledges the reality that (a) anal sex is the primary route of HIV transmission among gay and bisexual men, and (b) men may not necessarily know their or their partner’s HIV or viral-load status. Regardless of the specific practices used, the overall aim of these strategies is to reduce the risk of HIV transmission in serodiscordant partnerships (Rönn, White, Hughes, & Ward, 2014) or during casual sexual encounters (Berry, Raymond, Kellogg, & McFarland, 2008).
Recent research assessing the prevalence of seroadaptive behavior found that while these strategies are likely the result of intentional risk management, fewer than one in three gay and bisexual men adhered consistently to any intended strategy, and no strategy was used by more than half of sampled participants (Cassels & Katz, 2013; McFarland et al., 2012). Meanwhile, other studies have found that gay and bisexual men, in fact, use a range of seroadaptive strategies—employing different strategies to meet different contextual needs (Noor, Coleman, Brennan, Gardner, & Hart, 2015; Otis et al., 2016). The diversity of available strategies and the complex rationale underpinning their use may thus explain why individuals report low adherence to any one specific strategy and why some strategies appear to be used by only a small proportion of the population.
Hoping to articulate the complex motivators for seroadaptation, several researchers (Noor et al., 2015; Otis et al., 2016) have used a person-centered analytic approach known as latent class analysis (LCA; Lanza, Collins, Lemmon, & Schafer, 2007). This method uses a three-step approach to identify unmeasured characteristics, referred to as “latent classes.” In the context of seroadaptation, these latent classes may represent distinct risk contexts or perceptions that shape the sexual behavior of individuals belonging to these classes. By identifying these unmeasured classes and modeling the correlates associated therewith, public health and community leaders can tailor HIV prevention efforts for individuals whose risk management behavior (or lack thereof) might predispose them to increased risk for HIV.
While the etiology of seroadaptive behaviors remains unclear, existing literature highlights several important constructs that influence the sexual decisions of gay and bisexual men (Neville & Adams, 2009). Among these, sensation seeking (S. C. Kalichman & Rompa, 1995), treatment optimism (Van de Ven, Crawford, Kippax, Knox, & Prestage, 2000), and sexual altruism (O’Dell, Rosser, Miner, & Jacoby, 2008) have been shown to be predictive of condomless anal sex, with the last of these having a protective effect. Sensation seeking, for example, is conceptualized as a stable personality trait that corresponds with an attraction towards novel and thrilling sexual practices. Treatment optimism is a construct that measures the degree to which advances in biomedical HIV treatment and prevention has reduced the perceived risk of condomless sex (Van de Ven et al., 2000). Sexual altruism, coined by Nimmons (1998), measures the degree to which an individual’s values and risk-management behavior are motivated by altruistic (i.e., other-centered) concern for others (Nimmons & Folkman, 1999; O’Dell et al., 2008). In addition to these psycho-social motivators, other more tangible measures such as relationship status (Lachowsky, Dewey, et al., 2015), partner concurrency (Lachowsky, Saxton, et al., 2015), and anal sex positioning preference (Zhang et al., 2015) have also been shown to influence sexual behavior and risk management among gay men (Brady, Iantaffi, Galos, & Rosser, 2013). As the correlation between these etiologies and condom use has been well-established and finding little rationale to conceptualize seroadaptive behavior as wholly distinct from other risk management approaches, it is possible that these constructs likewise predict seroadaptive behavior.
Consistent with the observations, the present study aims to (1) use LCA to examine the patterns of how GBM in Vancouver, Canada use seroadaptive behaviors, and (2) use multinomial regression to determine whether factors predicting condom use (i.e., treatment optimism, sexual altruism, sexual sensation seeking, number of partners, relationship status, anal sex preference) are similarly associated with patterns of seroadaptive behavior. We hypothesize that LCA will identify distinct groups of GBM characterized by differing patterns of seroadaptive behavior and motivated by similar cognitive and contextual factors previously correlated with condom use.
METHODS
Study Setting
Eligible participants were (1) gay, bisexual, and other men who have sex with men, (2) aged 16 years and older, (3) residing in the Metro Vancouver area, (4) who reported sex with another man in the past six months, (5) were able to complete a questionnaire in English, and (6) were recruited through the use of respondent-driven sampling (RDS; Heckathorn, Semaan, Broadhead, & Hughes, 2002). Initial RDS seeds were recruited through community-based AIDS service organizations and later through a popular sex-seeking smartphone application. After confirming eligibility and securing written informed consent to participate, seeds were given up to six vouchers to use to recruit other eligible men into the study. Individuals presenting study vouchers at the downtown study office were screened for eligibility, provided written informed consent, completed the study protocol, and then were given vouchers of their own to recruit participants from within their social and/or sexual networks. Participants received $50 CAD honoraria for the study visits and could earn an additional $10 CAD honorarium for each recruit who successfully enrolled in the study. Honoraria could be taken as cash or used to purchase $10 draw tickets for either a monthly drawing for a $250.00 CAD gift card or a semi-annual drawing for a $2000.00 CAD travel voucher. Ethics approval for this study was received from research ethics boards at Simon Fraser University, the University of British Columbia, and the University of Victoria.
Study Design
Recruitment and baseline cross-sectional data collection began in February 2012 and closed in February 2014. Participants completed a 60- to 90-minute computer-administered questionnaire which collected data on a variety of sociodemographic, behavioral, and psychosocial measures. A study nurse administered a short clinical questionnaire and tested for HIV, hepatitis C, and syphilis; tests for chlamydia and gonorrhea were also available upon request.
Seroadaptation Measures
Participants were asked whether they used any of six seroadaptive strategies (i.e., consistent condom use, strategic positioning, anal sex avoidance, serosorting, viral-load sorting, and withdrawal) to prevent HIV transmission. It should be noted that the seroadaptive strategies used in the present analysis represent behaviors specifically relating to anal sex and condomless anal sex, while other research has sometimes included oral sex strategies and so called “pure” serosorting strategies, where partners with discordant serostatus are avoided for all types of sexual behavior and not just condomless anal sex (Cassels & Katz, 2013). In the Momentum questionnaire, these questions were introduced by saying: “Some guys use strategies to prevent getting/transmitting HIV. Do you do any of the following to prevent getting/transmitting HIV? (check ALL that apply)” with wording differences due to HIV status as reported by participants. The response text describing each seroadaptive strategy is provided in Table 1. While two items were asked similarly for HIV-negative/unknown and HIV-positive men, four items were asked in a manner specific to HIV status. Considering (a) the serostatus specific motivations underlying sexual behavior (Seth C. Kalichman, Cain, & Simbayi, 2010; Rönn et al., 2014) and (b) the rejection of the assumption of measurement invariance restriction in our LCA model-building procedure, all analyses were stratified by self-reported HIV status (negative/unknown vs. positive).
Table 1.
Seroadaptive strategy questions
| HIV-Negative/Unknown | |
| Consistent Condom Use | “Always using condoms for anal sex” |
| Strategic Positioning | “Being the top for anal sex” |
| Anal Sex Avoidance | “Having sex which doesn’t include anal sex” |
| Serosorting | “Having anal sex without condoms only with guys I know are HIV- negative” |
| Viral Load Sorting | “Having anal sex without condoms with HIV-positive guys who have low viral loads or are on HIV treatment” |
| Withdrawal | “Not letting my sex partners cum inside me” |
| HIV-Positive | |
| Consistent Condom Use | “Always using condoms for anal sex” |
| Strategic Positioning | “Being the bottom for anal sex” |
| Anal Sex Avoidance | “Having sex which doesn’t include anal sex” |
| Serosorting | “Having anal sex without condoms only with guys I know are HIV- positive” |
| Viral Load Sorting | “Having anal sex without condoms if my viral load is low or I’m on HIV treatment” |
| Withdrawal | “Not cumming inside my sex partners” |
Explanatory Measures
The present analysis included six demographic factors: age (continuous in years), sexual orientation (gay identified versus non-gay identified), education (≤ high school diploma, some college, > college degree), race/ethnicity (white versus non-white), annual income (< $30,000, $30,000–59,999, ≥ $60,000 CAD), and relationship status (monogamous, open, single).
To assess the relationship between sexual behavior and seroadaptation, participants were asked to report their anal sex preference (versatile, bottom, top, no anal sex), number of anal sex partners in the past six months (continuous), and whether they engaged in any CAS during the past six months (no, concordant CAS, serodiscordant/unknown CAS [sdCAS]). Based on previous work investigating socio-cognitive motivators underpinning HIV prevention related behavior (Adam, Husbands, Murray, & Maxwell, 2005; O’Dell et al., 2008; Roberti, 2004; Rowniak, 2009), three scales were used to assess sexual sensation seeking, treatment optimism, and HIV-prevention altruism. Additional information regarding these three scales is provided below:
Sexual Sensation Seeking (11 items). Participants rated their level of agreement with questions designed to assess sensation seeking personality traits (e.g., “I am interested in trying out new sexual experiences.”) using a 4-point Likert scale from “Not at all like me” to “Very much like me” (S. C. Kalichman & Rompa, 1995). Final scores were calculated from the zero-shifted sum of all items and range from 11–44, with higher scores indicating higher sexual sensation seeking (study α=0.73).
Treatment Optimism-Skepticism (12 items). Participants rated their level of agreement with items that assessed their attitudes towards HIV treatment and sexual risk (e.g., “If every HIV-positive person took the new treatments, the AIDS epidemic would be over.”) using a 4-point Likert scale from “Strongly Agree” to “Strongly Disagree” (Van de Ven et al., 2000). Final scores were calculated from the zero-shifted sum of all items and range from 0 “highly skeptical” to 23 “highly optimistic” (study α=0.82).
Personal and Communal Sexual Altruism (13 items). Participants rated their level of agreement with 7 items assessing their personal-/partner-related motivations (e.g., “Having safer sex shows I care about my partner”, α=.81) and 6 items assessing community-related motivations (e.g. “I have safer sex because I want the gay community to survive”) for safer sex using a 5-point Likert scale from “Strongly Agree” to “Strongly Disagree” (O’Dell et al., 2008). Final scores were calculated by calculating the zero-shifted sum of all items divided by the number of items in the scale. Possible scores ranged from 0–4, with higher scores indicating greater altruism. (study α=.88)
Statistical Analysis
All statistical analyses were conducted using SAS 9.4. To understand better the seroadaptive patterns of gay and bisexual men, latent class analysis (LCA; Lanza et al., 2007; Muthén & Muthén, 2000) was used to group participants based on self-reported seroadaptive behaviors. This method for identifying unmeasured class characteristics among study populations has recently been used to model partner frequency and concurrency (Ashenhurst, Wilhite, Harden, & Fromme, 2016), patterns of masculinity in heterosexual men (Casey et al., 2015), HIV-related stigma (Brinkley-Rubinstein & Craven, 2014), substance use (McCarty-Caplan, Jantz, & Swartz, 2014), and risk reduction (Noor et al., 2015) among gay and bisexual men. As applied in the present study, LCA allows us to consider the distinct behavioral repertoires gay and bisexual men use to manage their HIV risk.
LCA was conducted using the PROC LCA sub-routine. For each model, LCA creates a posterior class membership probabilities based on the model’s indicator variables. The number of classes included in this new categorical variable is determined by comparing goodness-of-fit statistics for each potential model and with consideration to interpretability and conceptual significance (Dias, 2006). For each fit statistic, a lower value indicates better model fit. In the present analysis, LCA models were conducted grouping by self-reported HIV status: HIV-positive and HIV-negative/unknown men. The assumption of measurement invariance restriction was rejected (p-value < 0.001), resulting in an unrestricted LCA solution, allowing indicators to load differently across HIV-negative/unknown and HIV-positive groups. Four models ranging from two to five classes were compared.
A four-class solution was selected for several reasons. First, a 42% drop of G-squared fit statistics was observed from a three-class model to a four-class model. Second, Akaike information criterion (AIC), adjusted Bayesian information criterion (aBIC), and the likelihood ratio tests (LRT) all showed that the four-class model was the best fit (see Table 2). Third, the four-class model was considered theoretically and conceptually appropriate as it clearly distinguished between each class. To assure the HIV-negative/unknown and HIV-positive men structured similarly, further stratified LCA models were generated, where the fit statistics led to four-class models for both groups.
Table 2.
Goodness-of-fit statistics for LCA Model selection
| # of Latent Class | 2 | 3 | 4 | 5 |
|---|---|---|---|---|
| HIV-Negative/Unknown | ||||
| Seeds | 100/100 | 8/100 | 66/100 | 5/100 |
| G-squared | 146 | 81 | 41 | 28 |
| Akaike information criterion | 172 | 121 | 95 | 96 |
| Bayesian information Criterion | 228 | 207 | 211 | 243 |
| Adjusted Bayesian information Criterion | 187 | 143 | 126 | 135 |
| Likelihood Ratio Test | <.0001 | <.0001 | 0.0756 | |
| HIV-Positive | ||||
| Seeds | 100/100 | 9/100 | 54/100 | 12/100 |
| G-squared | 93 | 70 | 47 | 39 |
| Akaike information criterion | 119 | 110 | 101 | 107 |
| Bayesian information Criterion | 163 | 178 | 192 | 222 |
| Adjusted Bayesian information Criterion | 122 | 115 | 107 | 114 |
| Likelihood Ratio Test | 0.0015 | 0.0015 | 0.2978 | |
| Grouped | ||||
| Seeds | 100/100 | 8/100 | 39/100 | 12/100 |
| G-squared | 239 | 151 | 88 | 66 |
| Akaike information criterion | 291 | 231 | 196 | 202 |
| Bayesian information Criterion | 412 | 417 | 447 | 518 |
| Adjusted Bayesian information Criterion | 330 | 290 | 275 | 302 |
| Likelihood Ratio Test | <.0001 | <.0001 | 0.0949 |
Bolded text indicated selected LCA model.
Using the final four-class solution, each participant was assigned to the latent classes by the membership probabilities, and bivariable and multivariable multinomial logistic regression was then conducted using the PROC LOGISTIC command with AIC minimization and Type III p-values to build three multivariable models for each HIV status to identify important explanatory variables for each class membership using the largest class as the referent. In these procedures, the explanatory measures included in the section above were treated as the independent variables, and LCA class membership was treated as a multi-level dependent variable.
RESULTS
Descriptive Statistics
Of the 774 men enrolled in our study, four did not answer the questions regarding the six seroadaptive behaviors that comprised our outcome variable and were therefore excluded from this analysis. Overall, the sample’s median age was 34 years (Q1–Q3: 26–47), and the majority of men self-identified as gay (79.9%), made less than $30,000 CAD per year (72.9%), had a high school diploma or equivalent (71.0%), and were white (68.5%). Additional stratified sample characteristics are provided in Table 3 with p-values indicating significant differences between HIV-negative/unknown and HIV-positive men. Of note, HIV-positive men had higher treatment optimism and sensation seeking, and lower personal and community altruism. HIV-positive men also reported having had more recent male anal sex partners and were more likely to engage in sdCAS.
Table 3.
Descriptive statistics for HIV-negative/unknown (n=556) and HIV-positive men (n=218)
| Continuous Variables | HIV-negative N (%) |
HIV-positive N (%) |
p-value |
|---|---|---|---|
| Age | 30 (24,39)1 | 47 (39,51)1 | <0.001 |
| Sexual Orientation | |||
| Gay Identified | 470 (84.5) | 185 (84.9) | 0.879 |
| Non-Gay Identified | 86 (15.5) | 33 (15.1) | |
| Ethnicity | |||
| White | 412 (74.6) | 171 (78.4) | 0.268 |
| Non-White | 140 (25.4) | 47 (21.6) | |
| Education | |||
| ≤High school diploma | 112 (20.3) | 112 (42.4) | 0.012 |
| Some college | 162 (29.3) | 58.0 (22.0) | |
| ≥College degree | 278 (50.4) | 94.0 (35.6) | |
| Annual Income | |||
| <$30,000 | 328 (59.0) | 157 (72.0) | 0.003 |
| $30,000 – $59,999 | 154 (27.7) | 46 (21.1) | |
| ≥$60,000 | 74 (13.3) | 15 (6.9) | |
| Relationship Status | |||
| Monogamous Relationship | 92 (16.7) | 33 (15.1) | 0.823 |
| Open Relationship | 123 (22.3) | 47.0 (21.6) | |
| Single | 337 (61.1) | 138.0 (63.3) | |
| Anal Sex Preference | |||
| Versatile | 141 (25.4) | 69 (31.7) | 0.192 |
| Bottom | 184 (33.1) | 74 (33.9) | |
| Top | 206 (37.1) | 66 (30.3) | |
| No Anal Sex | 25 (4.5) | 9 (4.1) | |
| Treatment Optimism Scale | 24 (20, 27)1 | 28 (25, 32)1 | <0.001 |
| Personal Sexual Altruism | 3.57 (3.14, 3.86)1 | 3.43 (2.71, 3.86)1 | 0.001 |
| Community Sexual Altruism | 3.67 (3, 4)1 | 3.17 (2.33, 4)1 | <0.001 |
| Sexual Sensation Seeking | 30 (28, 33)1 | 32 (29, 35)1 | 0.001 |
| No. of Male Anal Sex Partners2 | 3 (1,6)1 | 4 (2,19)1 | 0.008 |
| Condomless Anal Sex (CAS)2 | 0.002 | ||
| No Condomless Anal Sex | 211 (38.9) | 57 (26.8) | |
| Concordant CAS | 140 (25.8) | 57 (26.8) | |
| Serodiscordant/Unknown CAS | 192 (35.4) | 99 (46.5) |
Median (Q1,Q3)
in the past six months
Regarding seroadaptation, Table 4 shows the proportion of HIV-positive and HIV-negative/unknown men reporting each seroadaptive behavior overall and by each latent class. A higher proportion of HIV-positive men than HIV-negative/unknown men reported inconsistent condom use (p < 0.001), no anal sex avoidance (p = 0.001) strategic positioning (p = 0.012), serosorting (p < 0.001), and viral-load sorting (p < 0.001). There were no statistically significant differences in the proportion who reported withdrawal (p = 0.276)
Table 4.
Latent class model for HIV-negative/unknown (n=552) and HIV-Positive men (n=218)
| Overall | Condom Users |
Multiple Prevention Users |
Viral-load Sorters |
Serosorters | |
|---|---|---|---|---|---|
| Prevention Strategies | N (%) | N (%) | N (%) | N (%) | N (%) |
| HIV-Negative/Unknown | 397 (71.9) | 50 (9.0) | 46 (8.3) | 59 (10.8) | |
| Consistent Condom Use | 353 (64.0) | 322 (81.0) | 29 (57.5) | 3 (6.2) | 0 (0.0) |
| Strategic Positioning | 147 (26.6) | 70 (17.5) | 45 (91.2) | 20 (44.2) | 12 (20.0) |
| Anal Sex Avoidance | 274 (49.6) | 188 (47.4) | 50 (100.0) | 0 (0.0) | 36 (61.1) |
| Serosorting | 195 (35.3) | 77 (19.5) | 41 (82.8) | 17 (37.4) | 59 (100.0) |
| Viral-load Sorting | 55 (10.0) | 0 (0.0) | 23 (46.3) | 32 (69.8) | 0 (0.0) |
| Withdrawal | 154 (27.9) | 101 (25.5) | 33 (65.5) | 16 (35.9) | 4 (6.6) |
| HIV-Positive | 92 (42.3) | 20 (9.2) | 30 (13.8) | 76 (34.8) | |
| Consistent Condom Use | 73 (33.5) | 58 (62.7) | 6 (31.7) | 0 (0) | 9 (11.7) |
| Strategic Positioning | 78 (35.8) | 18 (19.4) | 15 (74.4) | 12 (40.0) | 33 (43.8) |
| Anal Sex Avoidance | 78 (35.8) | 38 (41.1) | 18 (89.4) | 9 (30.0) | 13 (17.4) |
| Serosorting | 113 (51.8) | 17 (18.6) | 20 (100.0) | 0 (0.0) | 76 (100.0) |
| Viral-load Sorting | 85 (39.0) | 0 (0.0) | 20 (100.0) | 30 (100.0) | 35 (46.1) |
| Withdrawal | 65 (29.8) | 18 (19.5) | 14 (72.1) | 17 (56.7) | 16 (20.6) |
Bolded text indicates behaviors used by a majority of the participants belonging to each given class.
Latent Class Analysis
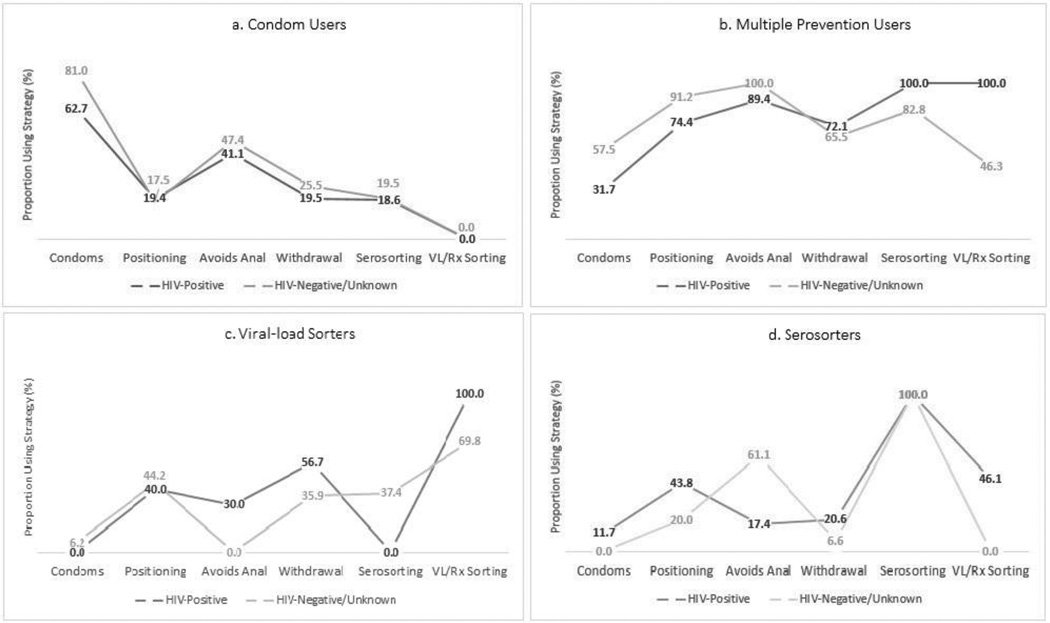
A four-class LCA model (Figure 1) was selected as described. Upon considering the frequencies of seroadaptive behavior reported by each class, our study team named each of the four LCA classes as follows: (a) Condom Users, (b) Multiple Prevention Users, (c) Viral-load Sorters, and (d) Serosorters. More information about each class is provided below:
Figure 1.
Prevalence of the seroadaptive strategies employed in each latent class stratified/separated by HIV status.
Class 1: Condom Users
The first, and most common latent class, represented 81% of HIV-negative/unknown men, but only 42% of HIV-positive men. Among men in this class, 63% of HIV-positive men and 81% of HIV-negative/unknown men reported “always using condoms.” The next most prevalent seroadaptive behavior among men in this class was anal sex avoidance, which was used by 41% of HIV-negative/unknown men and 47% of HIV-positive men. Aside from these, no other seroadaptive strategy was reported by more than one-third of the men in this class. Despite high rates of reported consistent condom use, 23% (n = 88/385) of HIV-negative/unknown men and 19% (n = 17/90) of HIV-positive men reported concordant CAS. Further, 26% (n = 98/385) of HIV-negative/unknown men and 33% (n = 29/90) of HIV-positive men in this class reported serodiscordant/unknown CAS.
Class 2: Multiple Prevention Users
The second latent class represented nearly 9% of HIV-negative/unknown and 9% of HIV-positive men. Individuals in this class are described as Multiple Prevention Users due to moderate to high reported rates of multiple prevention strategies including anal sex avoidance, serosorting, strategic positioning, viral-load sorting, withdrawal, and consistent condom use. In this class, a higher proportion of HIV-positive men reported withdrawal, serosorting, and viral-load sorting; while a higher proportion of HIV-negative men reported consistent condom use, strategic positioning, and anal sex avoidance.
Class 3: Viral-load Sorters
The third latent class represented only 8% of HIV-negative/unknown men and 14% of HIV-positive men. This class was characterized by low levels of consistent condom use and high levels of viral-load sorting, which was more common among HIV-positive men than HIV-negative/unknown men (p < 0.001). A higher proportion of HIV-positive men also reported withdrawal and anal sex avoidance compared to HIV-negative/unknown men (p < 0.001); while a higher proportion of HIV-negative men reported serosorting in this class (p < 0.001).
Class 4: Serosorters
The fourth latent class represented 11% of HIV-negative/unknown men, but 35% of HIV-positive men. In both the HIV-positive and the HIV-negative/unknown LCA models, 100% men belonging to this class reported using serosorting. Consistent condom use was reported by only 12% of HIV-negative/unknown men and by 0% of HIV-positive men in this class. Among HIV-positive Serosorters, 46% reported viral-load sorting, while none of the HIV-negative Serosorters did so. Conversely, only 17% of HIV-positive Serosorters reported anal sex avoidance compared to 61% of HIV-negative Serosorters.
Multinomial Logistic Regression
Table 5 provides the multivariable multinomial logistic regression models identifying the correlates of class membership, with Condom Users as the referent group. Among HIV-negative/unknown men, class membership was associated with age, relationship status, treatment optimism, personal altruism, sensation seeking, number of recent male anal sex partners, and recent sdCAS. Similarly, among HIV-positive men, class membership was associated with relationship status, treatment optimism, community altruism, number of recent male anal sex partners, and recent sdCAS.
Table 5.
| Multivariable multinomial logistic regression models, with Condom Users as the referent group | |||
|---|---|---|---|
| Multiple Prevention aOR1 (95% CI2) |
Viral-load Sorters aOR1 (95% CI2) |
Serosorters aOR1 (95% CI2) |
|
| HIV-Negative/Unknown | |||
| Age | 1.00 (0.98, 1.03) | 1.04 (1.01, 1.07) | 1.00 (0.97, 1.02) |
| Relationship Status | |||
| Monogamous Relationship | 1.00 | 1.00 | 1.00 |
| Open Relationship | 0.63 (0.25, 1.61) | 0.59 (0.20, 1.78) | 0.50 (0.23, 1.10) |
| Single | 0.40 (0.17, 0.93) | 0.39 (0.15, 1.03) | 0.98 (0.94, 1.02) |
| Treatment Optimism | 1.08 (1.01, 1.16) | 1.17 (1.09, 1.27) | 1.11 (1.04, 1.18) |
| Personal Altruism | 1.56(0.74, 3.28) | 0.46 (0.23, 0.90) | 0.63 (0.35, 1.13) |
| Sexual Sensation Seeking | 1.09 (1.01, 1.18) | 1.01 (0.91, 1.10) | 1.04 (0.96, 1.12) |
| No. of Anal Sex Partners3 | 1.02 (1.00, 1.03) | 1.02 (1.01, 1.04) | 0.98 (0.94, 1.02) |
| sdCAS (vs. none)3,4 | 2.87 (1.47, 5.62) | 8.60 (3.35, 22.06) | 1.33 (0.69, 2.57) |
| HIV-Positive | |||
| Relationship Status | |||
| Monogamous Relationship | 1.00 | 1.00 | 1.00 |
| Open Relationship | 0.58 (0.11, 3.12) | 0.69 (0.18, 2.58) | 1.61 (0.50, 5.17) |
| Single | 0.40 (0.10, 1.61) | 0.13 (0.04, 0.46) | 1.28 (0.56, 3.54) |
| Treatment Optimism | 1.05 (0.95, 1.16) | 1.15 (1.05, 1.26) | 1.03 (0.97, 1.09) |
| Community Altruism | 0.64 (0.36, 1.13) | 0.63 (0.37, 1.06) | 0.59 (0.41, 0.86) |
| No. of Anal Sex Partners1 | 1.02 (1.00, 1.03) | 1.02 (1.01, 1.04) | 0.98 (0.94, 1.02) |
| sdCAS (vs. none)1,2 | 4.82 (1.55, 14.99) | 5.29 (1.89, 14.76) | 1.56 (0.79, 3.07) |
| Bivariable multinomial logistic regression models, with Condom Users as the referent group, comparing covariates of class membership. | |||
|---|---|---|---|
| Multiple Prevention | Viral-load Sorters | Serosorters | |
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| HIV-Negative/Unknown | |||
| Age | 1.01 (0.98, 1.04) | 1.04 (1.01, 1.06) | 1.00 (0.98, 1.03) |
| Non-Gay Identity (vs. Gay) | 0.78 (0.33, 1.84) | 0.53 (0.19, 1.46) | 0.83 (0.38, 1.8) |
| Non-White Ethnicity (vs. White) | |||
| Education | |||
| ≤High school diploma | 1.00 | 1.00 | 1.00 |
| Some college | 1.76 (0.66, 4.72) | 0.57 (0.22, 1.46) | 1.29 (0.56, 2.95) |
| ≥College degree | 2.16 (0.86, 5.38) | 1.11 (0.52, 2.37) | 1.46 (0.68, 3.12) |
| Annual Income | |||
| <$30,000 | |||
| $30,000 – $59,999 | 1.45 (0.73, 2.86) | 1.31 (0.62, 2.74) | 1.66 (0.92, 3.01) |
| ≥$60,000 | 2.13 (0.96, 4.75) | 2.85 (1.31, 6.17) | 1.05 (0.42, 2.62) |
| Relationship Status | |||
| Monogamous Relationship | 1.00 | 1.00 | 1.00 |
| Open Relationship | 0.85 (0.35, 2.07) | 0.69 (0.27, 1.76) | 0.53 (0.25, 1.11) |
| Single | 0.51 (0.23, 1.13) | 0.52 (0.23, 1.15) | 0.22 (0.12, 0.44) |
| Anal Sex Preference | |||
| Bottom (vs. Versatile) | 0.34 (0.14, 0.81) | 0.80 (0.34, 1.86) | 0.96 (0.47, 1.94) |
| Top (vs. Versatile) | 0.90 (0.46, 1.79) | 1.35 (0.62, 2.91) | 0.93 (0.46, 1.90) |
| No Anal Sex (vs. Versatile) | 0.57 (0.13, 2.55) | 0.03 (0.00, 34.7) | 0.47 (0.09, 2.56) |
| Treatment Optimism Scale | 1.11 (1.04, 1.18) | 1.26 (1.18, 1.35) | 1.13 (1.07, 1.20) |
| Personal Sexual Altruism | 0.98 (0.5, 1.91) | 0.22 (0.12, 0.39) | 0.50 (0.3, 0.85) |
| Community Sexual Altruism | 0.72 (0.43, 1.2) | 0.27 (0.17, 0.45) | 0.54 (0.34, 0.85) |
| Sexual Sensation Seeking | 1.14 (1.07, 1.23) | 1.15 (1.07, 1.24) | 1.06 (0.99, 1.13) |
| No. of Male Anal Sex Partners8 | 1.03 (1.01, 1.04) | 1.04 (1.02, 1.05) | 0.98 (0.94, 1.02) |
| sdCAS (vs. none)8,2 | 4.32 (2.35, 7.97) | 17.80 (7.48, 42.39) | 9.94 (3.48, 28.39) |
| HIV-Positive | |||
| Age | 0.97 (0.92, 1.02) | 1.01 (0.97, 1.06) | 1.01 (0.97, 1.04) |
| Non-Gay Identity (vs. Gay) | 0.80 (0.23, 2.84) | 0.60 (0.19, 1.91) | 0.37 (0.14, 0.95) |
| Non-White Ethnicity (vs. White) | 0.49 (0.13, 1.93) | 0.62 (0.22, 1.84) | 0.91 (0.44, 1.87) |
| Education | |||
| ≤High school diploma | 1.00 | 1.00 | 1.00 |
| Some college | 7.28 (1.51, 35.13) | 2.11 (0.70, 6.31) | 2.06 (0.90, 4.73) |
| ≥College degree | 4.41 (0.95, 20.51) | 1.72 (0.64, 4.64) | 2.08 (1.01, 4.29) |
| Annual Income | |||
| <$30,000 | 1.00 | 1.00 | 1.00 |
| $30,000 – $59,999 | 2.27 (0.78, 6.66) | 3.21 (1.24, 8.28) | 0.91 (0.40, 2.06) |
| ≥$60,000 | 0.26 (0.01, 12.31) | 3.25 (0.81, 13.09) | 1.03 (0.30, 3.60) |
| Relationship Status | |||
| Monogamous Relationship | 1.00 | 1.00 | 1.00 |
| Open Relationship | 0.74 (0.15, 3.68) | 1.10 (0.35, 3.50) | 1.63 (0.53, 5.03) |
| Single | 0.71 (0.20, 2.55) | 0.30 (0.10, 0.89) | 1.52 (0.58, 3.98) |
| Anal Sex Preference | |||
| Bottom (vs. Versatile) | 1.67 (0.53, 5.30) | 3.89 (1.11, 13.60) | 1.40 (0.67, 2.06) |
| Top (vs. Versatile) | 0.84 (0.24, 2.98) | 3.75 (1.11, 12.73) | 0.70 (0.32, 1.53) |
| Treatment Optimism Scale | 1.09 (0.99, 1.20) | 1.19 (1.09, 1.30) | 1.06 (1.00, 1.12) |
| Personal Sexual Altruism | 0.45 (0.22, 0.90) | 0.50 (0.27, 0.93) | 0.52 (0.32, 0.84) |
| Community Sexual Altruism | 0.56 (0.33, 0.98) | 0.55 (0.34, 0.89) | 0.53, 0.35, 0.77) |
| Sexual Sensation Seeking | 1.14 (1.02, 1.28) | 1.12 (1.01, 1.23) | 1.09 (1.02, 1.17) |
| No. of Male Anal Sex Partners8 | 1.01 (1.00, 1.02) | 1.01 (0.99, 1.02) | 1.01 (1.00, 1.02) |
| sdCAS (vs. none)8,2 | 4.94 (1.70, 14.38) | 4.81 (1.96, 11.80) | 1.86 (0.99, 3.52) |
Past six months
Serodiscordant/Unknown Condomless Anal Sex
Bolded text indicates p<0.05.
Past six months
Serodiscordant/Unknown Condomless Anal Sex
Bolded text indicates p<0.05.
DISCUSSION
In the present study, we identified four classes of gay and bisexual men who employed distinct patterns of seroadaptive behavior: Condom Users, Multiple Prevention Users, Viral-load Sorters, and Serosorters. While fundamental differences in study design make it difficult to compare our findings to those of previous studies, Noor et al. (2015) and Otis et al. (2016) serve as valuable comparisons. For example, Noor et al. (2015) identified three latent classes based on five risk management strategies. Their LCA described three classes of men who (i) did not consistently use any risk management strategies (44%), (ii) were inconsistent in employing these strategies (33%), and (iii) consistently employed multiple strategies (23%). While not directly analogous to the LCA model presented in the present study, this work describes the frequency and consistency of gay and bisexual men’s use of risk management behavior and alludes to the presence of underlying motivators for such behavior.
Offering a more direct comparison, Otis et al. (2016), presented a five class LCA model, in which all participants used a range of seroadaptive behaviors. While Otis et al. (2016) argues that 72% of the sample—those in the “strict-serosorting” and “condom using” classes—were sufficiently protected by their seroadaptive behaviors, three smaller classes (i.e., “anal sex serosorters,” “strategic positioners,” and “viral-load sorters”) were exposed to unique risks attributable to their seroadaptive behavior. While recent evidence suggests that viral-load sorting may also offer sufficient protection against HIV—as so long as individuals can accurately gauge their partner’s HIV and viral load status (See Rodger et al., 2016), our findings support Otis’s overall conclusion that seroadaptive strategies can serve to reduce the HIV risks associated with anal sex among gay and bisexual men. Similarly, our findings support McFarland’s (2011) assertion that gay and bisexual men are able to achieve a high level of risk reduction by using a combination of seroadaptive behaviors. In their study, McFarland et al. (2011) estimated that less than 2% of sexual episodes actually exposed individuals to a high level of risk for HIV acquisition or transmission.
Consistent with these studies, the present analysis suggests that gay and bisexual men attempt to protect themselves through diverse combinations of seroadaptive behaviors, including condom use. Indeed, while 42% of men in the present study and 18% of men in Otis et al. (2016) were classified as “Condom Users,” our results indicate that seroadaptation is an important component of risk management for the majority of gay and bisexual men. Even among those who were identified as consistent Condom Users a sizeable proportion of men practiced other seroadaptive strategies to reduce their risk. Further, the reported prevalence of CAS (n = 232) among Condom Users was higher than the total number of men in this class who reported not engaging in consistent condom use (n = 109). This indicates that while individuals may report “always using condoms,” some may not actually use condoms consistently. This agrees with previous research by McFarland et al. (2012) suggesting that intentions to engage in risk management have low consistent adherence. In their study, 71% of HIV-negative men and 42% of HIV-positive men reported the intention to always use condoms, and yet, only 30% of HIV-negative men and 20% of HIV-positive men who intended to adhere to this strategy actually reported doing so after 1 year of follow-up.
When taken together, the results presented here, suggest that seroadaptation is used for context-specific risk reduction and is highly dependent on the needs of individuals and their partners (Rönn et al., 2014). Indeed, Otis et al. (2016) found that class membership was associated with a variety of factors, including relationship status and the serostatus of partners. In our study, this is made clear when looking at our second latent class (Multiple Prevention Users). These men practiced a wide range of seroadaptive behaviors and this class is somewhat analogous to the “inconsistent” LCA class presented in Noor et al. (2015). For instance, 100% of HIV-negative/unknown Multiple Prevention Users reported avoidance of anal sex and 91.2% reported strategic positioning. As these two strategies are incompatible we argue that these individuals are sometimes using strategic positioning, and sometimes avoiding anal sex — employing each strategy when they feel it is most appropriate or when contextual and/or interpersonal factors may otherwise necessitate one strategy over another.
Indeed, our multivariable results indicate that context-dependent and interpersonal factors have direct influence on seroadaptive behavior and are correlated with membership in a given class. For example, compared to Condom Users, HIV-negative/unknown Multiple Prevention Users and HIV-positive Viral-load Sorters were much more likely to be in a monogamous relationship compared to being single. This indicates that HIV-positive men in monogamous relationships may be more likely to rely on viral-load sorting with their committed partners to reduce the risk of HIV-transmission (Rönn et al., 2014). For HIV-negative men, this may indicate a more diverse repertoire of seroadaptive behaviors among men who are single and who may have a greater number of sexual partners. These finding are consistent with previous research finding that relationship status, partner concurrency, and personal sexual preferences are all important predictors of sexual behavior (Lachowsky, Saxton, et al., 2015; Zhang et al., 2015). For Instance, Zhang et al. (2015) found that men who prefer to be the receptive partner during anal sex were less likely to engage in CAS; and Lachowsky, Dewey, et al., (2015) found that more frequent condom use was associated with men with more sexual partners and shorter relationships. With respect to seroadaptive behavior, these findings are further supported by McFarland et al., (2011), who identified different patterns of seroadaptation with main partners and non-main partners, and by our own recent work indicating that men with more partners use seroadaptive strategies as a way to offset the risks associated with CAS (Card et al., 2016). We also note that both HIV-positive and HIV-negative/unknown Viral-load Sorters were also more likely to have more sexual partners. Together, these findings suggest that interpersonal dynamics (as measured by relationship status and number of partners) have significant influence on the types of risk management strategies used by individuals to protect themselves and their partners (Brady et al., 2013; Braine, van Sluytman, Acker, Friedman, & Des Jarlais, 2011; Leung, Poon, & Lee, 2014; Ryzin, Johnson, Leve, & Kim, 2010). This framework captures a growing body of literature that suggests seroadaptive practices are the result of myriad complex personal, interpersonal, and situational factors (Cassels & Katz, 2013; McFarland et al., 2012; Rönn et al., 2014).
Several approaches have been used to describe the influence of complex situational, psychosocial, and intrapersonal factors on condom use (McKechnie, Bavinton, & Zablotska, 2013) and when expanded to other seroadaptive behaviors (Rönn et al., 2014), these models may help explain how attitudes, intentions, and beliefs influence gay and bisexual men’s seroadaptive strategies to prevent HIV transmission (Albarracín, Johnson, Fishbein, & Muellerleile, 2001). For instance, we observed that when compared to Condom Users, treatment optimism was higher among HIV-negative/unknown Multiple Prevention Users, Viral-load Sorters, and Serosorters, as well as HIV-positive Viral-load Sorters. This finding suggests that reduced HIV risk perceptions and optimistic attitudes towards HIV treatment may influence an individual’s willingness to engage in inconsistent condom use and uptake other seroadaptive strategies instead (Brennan et al., 2010; Stephenson, White, & Mitchell, 2015). This is particularly clear when noting that the strongest effect for treatment optimism was seen among Viral-Load Sorters—a behavioral strategy directly linked with awareness of HIV-prevention and risk awareness (Rodger et al., 2016). Another clear example of the influence that psychosocial and cognitive factors have on sexual behavior was the observation that higher sexual altruism was associated with being a Condom User, at least when compared to HIV-negative/unknown Viral-load Sorters and HIV-positive Serosorters. In this case, it seems to indicate that altruistic traits move individuals towards “safer” seroadaptation strategies, such as condom use (O’Dell et al., 2008). Conversely, higher sensation seeking was associated with being a Multiple Prevention User for HIV-negative men. In this case, sensation seeking may be driving more frequent sexual partnering and abandonment of condoms (Roberti, 2004). In turn, and contrary to research suggesting that men with high sensation seeking do not care about HIV prevention (Crawford et al., 2003), the increased risk profile of these individuals may be a core motivator for the robust repertoire of prevention behavior exhibited in this class. This would be consistent with earlier qualitative work by Van de Ven et al. (2002) which found that among the minority of gay and bisexual men who engaged in condomless anal sex seroadaptation was employed as a risk reduction strategy.
Strengths and Limitations
Readers should be cautious when interpreting our results as the reported use of seroadaptive behaviors does not necessarily mean that individuals are successfully managing their risk for HIV transmission. Not only are some strategies not necessarily effective in stopping the risk of HIV transmission (e.g. withdrawal), but individuals may also be unable to properly adhere to these strategies due to contextual restraints (e.g., condom availability, power dynamics) or due to inaccurate perceptions of their or their partner’s HIV-status. The problem of window-periods, combined with infrequent testing, may further make it difficult for individuals to successfully seroadapt. This is especially true in environments with high rates of HIV seroconversion. Additionally, due to the cross-sectional nature of this analysis and simplicity of our study measures, it is not clear whether behaviors within each class are used concurrently, how frequently behavioral strategies are used, or whether behaviors are adopted and relinquished over time. Further, as our sample (n = 774), was stratified both by HIV-status and then again by class membership, some classes and factors had small counts—increase the probability of Type I and Type II errors in this analyses. Our study may also be limited by the use of LCA, which may produce differing class structures in different populations. Further, as noted by Vermunt (2010), the use of a three-step LCA approach, as opposed to a single step approach, may underestimate the correlation between explanatory factors and class membership. Additionally, the seroadaptive anal sex strategies used to construct our LCA models do not fully characterize all potential seroadaptive approaches (e.g., PrEP, nPEP, “pure” serosorting, etc.) and differences in how seroadaptive behaviors are defined may result in significantly different LCA classes. For example, biomedical prevention strategies, especially HAART and PrEP, may have significant influence on the sexual decisions of gay and bisexual men (Chen, Snowden, McFarland, & Raymond, 2016). This is especially true given their potential to reduce or eliminate the risk of HIV infection (Grant et al., 2010; Rodger et al., 2016). Finally, we also note that some associations may be attributable to the nature of scale items rather than to a meaningful relationship between constructs. For example, the communal sexual altruism scale refers directly to “safe-sex,” meaning it’s possible that conflation between “safe-sex” and “condom use” (rather than other seroadaptive strategies) may explain the observed associations.
Future Research
Considering these limitations, future research efforts should identify the most acceptable and effective strategies, or combination of strategies, for preventing HIV transmission, especially in settings where HIV incidence remains high and where individuals feel that condoms detract from their sexual needs. Further, our findings necessitate the need for a better understanding of how these strategies are used by each class of GBM and whether seroadaptive class membership is stable over time. We hope that our results will be used in the development of longitudinal and event-level analyses, and in preparation for qualitative work that will better inform us as to the nature of seroadaptive behavior and how to promote effective seroadaptation among gay and bisexual men.
CONCLUSION
In Conclusion, this research highlights a variety of factors that shape patterns of seroadaptation and suggests that gay and bisexual men intentionally use a variety of risk reduction strategies, especially in the absence of consistent condom use, to prevent HIV transmission. Further, these findings suggest that individual prevention strategies appear in concert with other strategies as part of empirically distinct patterns of behavior. For instance, Serosorters and Viral-load Sorters were unlikely to report engaging in consistent condom use, while Condom Users did not report engaging in viral-load sorting. These findings suggest that when seroadaptive strategies are considered as part of a holistic and combination approach to reducing HIV transmission, biomedical interventions and other prevention campaigns might be more effective than traditional single-strategy programs. Antecedent to this, our findings also highlight the need to educate men regarding the effectiveness of seroadaptive behaviors, especially when considering that some strategies (i.e., viral-load sorting) are likely to be very effective at preventing seroconversion (Cohen et al., 2011; Rodger et al., 2016), while other behaviors (i.e., withdrawal or strategic positioning) may still allow for viral transmission even when consistently used. Combination prevention campaigns which include seroadaptive behavior as a component of program messaging must also aim to promote regular and appropriate HIV testing, as the successful implementation of all seroadaptive behaviors relies on an individual’s ability to accurately gauge their and their partner’s HIV status.
Supplementary Material
Acknowledgments
The authors would like to thank the Momentum Health Study participants, office staff, and community advisory board, Kirk J. Hepburn, who edited this manuscript, as well as our community partner agencies: Health Initiative for Men, YouthCO HIV & Hep C Society, and Positive Living Society of BC. Momentum is funded through the National Institute on Drug Abuse (R01DA031055-01A1) and the Canadian Institutes for Health Research (MOP-107544, 143342). Dr. Lachowsky is supported by a CANFAR/CTN Postdoctoral Fellowship Award. Dr. Moore is supported by a Scholar Award from the Michael Smith Foundation for Health Research (#5209).
Footnotes
Compliance with Ethical Standards
Ethical Approval:
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committees at Simon Fraser University, The University of British Columbia, and the University of Victoria and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent was obtained from all individual participants included in the study.
This article does not contain any studies with animals performed by any of the authors.
Conflict of Interest:
Kiffer G. Card declares that he has no conflict of interest.
Nathan J. Lachowsky declares that he has no conflict of interest.
Zishan Cui declares that she has no conflict of interest.
Allison Carter declares that she has no conflict of interest.
Susan Shurgold declares that she has no conflict of interest.
Heather Armstrong declares that she has no conflict of interest.
David Moore declares that he has no conflict of interest.
Robert S. Hogg declares that he has no conflict of interest.
Eric A. Roth declares that he has no conflict of interest.
REFERENCES
- Adam BD, Husbands W, Murray J, Maxwell J. AIDS optimism, condom fatigue, or self-esteem? Explaining unsafe sex among gay and bisexual men. Journal of Sex Research. 2005;42(3):238–248. doi: 10.1080/00224490509552278. https://doi.org/10.1080/00224490509552278. [DOI] [PubMed] [Google Scholar]
- Albarracín D, Johnson BT, Fishbein M, Muellerleile PA. Theories of reasoned action and planned behavior as models of condom use: a meta-analysis. Psychological Bulletin. 2001;127(1):142–161. doi: 10.1037/0033-2909.127.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashenhurst JR, Wilhite ER, Harden KP, Fromme K. Number of Sexual Partners and Relationship Status Are Associated With Unprotected Sex Across Emerging Adulthood. Archives of Sexual Behavior. 2016:1–14. doi: 10.1007/s10508-016-0692-8. https://doi.org/10.1007/s10508-016-0692-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baggaley RF, White RG, Boily M-C. HIV transmission risk through anal intercourse: systematic review, meta-analysis and implications for HIV prevention. International Journal of Epidemiology. 2010;39(4):1048–1063. doi: 10.1093/ije/dyq057. https://doi.org/10.1093/ije/dyq057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry M, Raymond HF, Kellogg T, McFarland W. The Internet, HIV serosorting and transmission risk among men who have sex with men, San Francisco. AIDS (London, England) 2008;22(6):787–789. doi: 10.1097/QAD.0b013e3282f55559. https://doi.org/10.1097/QAD.0b013e3282f55559. [DOI] [PubMed] [Google Scholar]
- Brady SS, Iantaffi A, Galos DL, Rosser BRS. Open, closed, or in between: relationship configuration and condom use among men who use the internet to seek sex with men. AIDS and Behavior. 2013;17(4):1499–1514. doi: 10.1007/s10461-012-0316-9. https://doi.org/10.1007/s10461-012-0316-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braine N, van Sluytman L, Acker C, Friedman S, Des Jarlais DC. Sexual contexts and the process of risk reduction. Culture, Health & Sexuality. 2011;13(7):797–814. doi: 10.1080/13691058.2011.582688. https://doi.org/10.1080/13691058.2011.582688. [DOI] [PubMed] [Google Scholar]
- Brennan DJ, Welles SL, Miner MH, Ross MW, Rosser BRS Positive Connections Team. HIV treatment optimism and unsafe anal intercourse among HIV-positive men who have sex with men: findings from the positive connections study. AIDS Education and Prevention: Official Publication of the International Society for AIDS Education. 2010;22(2):126–137. doi: 10.1521/aeap.2010.22.2.126. https://doi.org/10.1521/aeap.2010.22.2.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brinkley-Rubinstein L, Craven K. A Latent Class Analysis of Stigmatizing Attitudes and Knowledge of HIV Risk among Youth in South Africa. PLoS ONE. 2014;9(2):e89915. doi: 10.1371/journal.pone.0089915. https://doi.org/10.1371/journal.pone.0089915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card KG, Lachowsky NJ, Cui Z, Sereda P, Rich A, Jollimore J, Roth EA. Seroadaptive Strategies of Gay & Bisexual Men (GBM) with the Highest Quartile Number of Sexual Partners in Vancouver, Canada. AIDS and Behavior. 2016:1–15. doi: 10.1007/s10461-016-1510-y. https://doi.org/10.1007/s10461-016-1510-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey EA, Masters NT, Beadnell B, Wells EA, Morrison DM, Hoppe MJ. A Latent Class Analysis of Heterosexual Young Men’s Masculinities. Archives of Sexual Behavior. 2015;45(5):1039–1050. doi: 10.1007/s10508-015-0616-z. https://doi.org/10.1007/s10508-015-0616-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassels S, Katz DA. Seroadaptation among Men Who Have Sex with Men: Emerging Research Themes. Current HIV/AIDS Reports. 2013;10(4):305–313. doi: 10.1007/s11904-013-0188-2. https://doi.org/10.1007/s11904-013-0188-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y-H, Snowden JM, McFarland W, Raymond HF. Pre-exposure Prophylaxis (PrEP) Use, Seroadaptation, and Sexual Behavior Among Men Who Have Sex with Men, San Francisco, 2004–2014. AIDS and Behavior. 2016:1–7. doi: 10.1007/s10461-016-1357-2. https://doi.org/10.1007/s10461-016-1357-2. [DOI] [PubMed] [Google Scholar]
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, Fleming TR. Prevention of HIV-1 Infection with Early Antiretroviral Therapy. New England Journal of Medicine. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243. https://doi.org/10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford I, Hammack PL, McKirnan DJ, Ostrow D, Zamboni BD, Robinson B, Hope B. Sexual sensation seeking, reduced concern about HIV and sexual risk behaviour among gay men in primary relationships. AIDS Care. 2003;15(4):513–524. doi: 10.1080/0954012031000134755. https://doi.org/10.1080/0954012031000134755. [DOI] [PubMed] [Google Scholar]
- Davidovich U, van den Boom W, Witlox R, Stolte IG. The emergence of intentional viral sorting as a frequently performed risk reduction strategy among HIV-positive MSM (Vol. 87, pp. A250–A251) Sexually Transmitted Infections. 2011 https://doi.org/10.1136/sextrans-2011-050108.359. [Google Scholar]
- Dias JG. Latent Class Analysis and Model Selection. In: Spiliopoulou PDM, Kruse PDR, Borgelt DC, Nürnberger J-PDA, Gaul PDW, editors. From Data and Information Analysis to Knowledge Engineering. Springer Berlin Heidelberg: 2006. pp. 95–102. Retrieved from http://link.springer.com/chapter/10.1007/3-540-31314-1_10. [Google Scholar]
- Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, Glidden DV. Preexposure Chemoprophylaxis for HIV Prevention in Men Who Have Sex with Men. The New England Journal of Medicine. 2010;363(27):2587–2599. doi: 10.1056/NEJMoa1011205. https://doi.org/10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grulich AE, Zablotska I. Commentary: probability of HIV transmission through anal intercourse. International Journal of Epidemiology. 2010;39(4):1064–1065. doi: 10.1093/ije/dyq101. https://doi.org/10.1093/ije/dyq101. [DOI] [PubMed] [Google Scholar]
- Heckathorn DD, Semaan S, Broadhead RS, Hughes JJ. Extensions of Respondent-Driven Sampling: A New Approach to the Study of Injection Drug Users Aged 18–25. AIDS and Behavior. 2002;6(1):55–67. https://doi.org/10.1023/A:1014528612685. [Google Scholar]
- Horvath KJ, Smolenski D, Iantaffi A, Grey JA, Rosser BRS. Discussions of viral load in negotiating sexual episodes with primary and casual partners among men who have sex with men. AIDS Care. 2012;24(8):1052–1055. doi: 10.1080/09540121.2012.668168. https://doi.org/10.1080/09540121.2012.668168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin F, Prestage GP, Templeton DJ, Poynten IM, Donovan B, Zablotska I, Grulich AE. The impact of HIV seroadaptive behaviors on sexually transmissible infections in HIV-negative homosexual men in Sydney, Australia. Sexually Transmitted Diseases. 2012;39(3):191–194. doi: 10.1097/OLQ.0b013e3182401a2f. https://doi.org/10.1097/OLQ.0b013e3182401a2f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Cain D, Simbayi LC. Behavioral Changes Associated With Testing HIV-Positive Among Sexually Transmitted Infection Clinic Patients In Cape Town, South Africa. American Journal of Public Health. 2010;100(4):714–719. doi: 10.2105/AJPH.2009.162602. https://doi.org/10.2105/AJPH.2009.162602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D. Sexual sensation seeking and Sexual Compulsivity Scales: reliability, validity, and predicting HIV risk behavior. Journal of Personality Assessment. 1995;65(3):586–601. doi: 10.1207/s15327752jpa6503_16. https://doi.org/10.1207/s15327752jpa6503_16. [DOI] [PubMed] [Google Scholar]
- Lachowsky NJ, Dewey CE, Dickson NP, Saxton PJW, Hughes AJ, Milhausen RR, Summerlee AJS. Habitual condom use across partner type and sexual position among younger gay and bisexual men: findings from New Zealand HIV behavioural surveillance 2006–2011. Sexually Transmitted Infections. 2015 doi: 10.1136/sextrans-2014-051759. sextrans-2014-051759. https://doi.org/10.1136/sextrans-2014-051759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachowsky NJ, Saxton PJW, Hughes AJ, Dickson NP, Summerlee AJS, Milhausen RR, Dewey CE. Younger Gay and Bisexual Men’s Condom Use With Main Regular Sexual Partner in New Zealand. AIDS Education & Prevention. 2015;27(3):257–274. doi: 10.1521/aeap.2015.27.3.257. https://doi.org/10.1521/aeap.2015.27.3.257. [DOI] [PubMed] [Google Scholar]
- Lanza ST, Collins LM, Lemmon DR, Schafer JL. PROC LCA: A SAS Procedure for Latent Class Analysis. Structural Equation Modeling: A Multidisciplinary Journal. 2007;14(4):671–694. doi: 10.1080/10705510701575602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung KK, Poon CM, Lee SS. A Comparative Analysis of Behaviors and Sexual Affiliation Networks among Men Who Have Sex With Men in Hong Kong. Archives of Sexual Behavior. 2014 doi: 10.1007/s10508-014-0390-3. https://doi.org/10.1007/s10508-014-0390-3. [DOI] [PubMed] [Google Scholar]
- McCarty-Caplan D, Jantz I, Swartz J. MSM and drug use: A latent class analysis of drug use and related sexual risk behaviors. AIDS and Behavior. 2014;18(7):1339–1351. doi: 10.1007/s10461-013-0622-x. https://doi.org/10.1007/s10461-013-0622-x. [DOI] [PubMed] [Google Scholar]
- McFarland W, Chen Y-H, Nguyen B, Grasso M, Levine D, Stall R, Raymond HF. Behavior, intention or chance? A longitudinal study of HIV seroadaptive behaviors, abstinence and condom use. AIDS and Behavior. 2012;16(1):121–131. doi: 10.1007/s10461-011-9936-8. https://doi.org/10.1007/s10461-011-9936-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarland W, Chen Y-H, Raymond HF, Nyugen B, Colfax G, Mehrtens J, Truong H-HM. HIV seroadaptation among individuals, within sexual dyads, and by sexual episodes, men who have sex with men, San Francisco, 2008. AIDS Care. 2011;23(3):261–268. doi: 10.1080/09540121.2010.507748. https://doi.org/10.1080/09540121.2010.507748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKechnie ML, Bavinton BR, Zablotska IB. Understanding of norms regarding sexual practices among gay men: literature review. AIDS and Behavior. 2013;17(4):1245–1254. doi: 10.1007/s10461-012-0309-8. https://doi.org/10.1007/s10461-012-0309-8. [DOI] [PubMed] [Google Scholar]
- Mitchell JW. HIV-negative and HIV-discordant Gay Male Couples’ Use of HIV Risk-Reduction Strategies: Differences by Partner Type and Couples’ HIV-status. AIDS and Behavior. 2013;17(4):1557–1569. doi: 10.1007/s10461-012-0388-6. https://doi.org/10.1007/s10461-012-0388-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B, Muthén LK. Integrating person-centered and variable-centered analyses: growth mixture modeling with latent trajectory classes. Alcoholism, Clinical and Experimental Research. 2000;24(6):882–891. [PubMed] [Google Scholar]
- Neville S, Adams J. Condom use in men who have sex with men: a literature review. Contemporary Nurse. 2009;33(2):130–139. doi: 10.5172/conu.2009.33.2.130. [DOI] [PubMed] [Google Scholar]
- Nimmons D. In This Together. Journal of Psychology & Human Sexuality. 1998;10(3–4):75–87. https://doi.org/10.1300/J056v10n03_06. [Google Scholar]
- Nimmons D, Folkman S. Other-Sensitive Motivation for Safer Sex Among Gay Men: Expanding Paradigms for HIV Prevention. AIDS and Behavior. 1999;3(4):313–324. https://doi.org/10.1023/A:1025437418276. [Google Scholar]
- Noor SW, Coleman T, Brennan DJ, Gardner S, Hart TA. Safer sex strategies as risk reduction: Use of Latent Class Analysis approach to examine use of safe sex strategies among gay, bisexual and men who have sex with men in Toronto, Canada. Presented at the 2015 APHA Annual Meeting & Expo; APHA; Oct. 31 – Nov. 4, 2015; 2015. Retrieved from https://apha.confex.com/apha/143am/webprogram/Paper336896.html. [Google Scholar]
- O’Dell BL, Rosser BRS, Miner MH, Jacoby SM. HIV prevention altruism and sexual risk behavior in HIV-positive men who have sex with men. AIDS and Behavior. 2008;12(5):713–720. doi: 10.1007/s10461-007-9321-9. https://doi.org/10.1007/s10461-007-9321-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otis J, McFadyen A, Haig T, Blais M, Cox J, Brenner B Spot Study Group. Beyond Condoms: Risk Reduction Strategies Among Gay, Bisexual, and Other Men Who Have Sex With Men Receiving Rapid HIV Testing in Montreal, Canada. AIDS and Behavior. 2016 doi: 10.1007/s10461-016-1344-7. https://doi.org/10.1007/s10461-016-1344-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberti JW. A review of behavioral and biological correlates of sensation seeking. Journal of Research in Personality. 2004;38(3):256–279. https://doi.org/10.1016/S0092-6566(03)00067-9. [Google Scholar]
- Rodger A, Cambiano V, Brunn T, Vernazza P, Collins S, van Lunzen J PARNTER Study Group. Sexual activity without condoms and risk of hiv transmission in serodifferent couples when the hiv-positive partner is using suppressive antiretroviral therapy. JAMA. 2016;316(2):171–181. doi: 10.1001/jama.2016.5148. https://doi.org/10.1001/jama.2016.5148. [DOI] [PubMed] [Google Scholar]
- Roland ME, Neilands TB, Krone MR, Katz MH, Franses K, Grant RM, Martin JN. Seroconversion following nonoccupational postexposure prophylaxis against HIV. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America. 2005;41(10):1507–1513. doi: 10.1086/497268. https://doi.org/10.1086/497268. [DOI] [PubMed] [Google Scholar]
- Rönn M, White PJ, Hughes G, Ward H. Developing a Conceptual Framework of Seroadaptive Behaviors in HIV-Diagnosed Men Who Have Sex With Men. The Journal of Infectious Diseases. 2014;210(Suppl 2):S586–S593. doi: 10.1093/infdis/jiu482. https://doi.org/10.1093/infdis/jiu482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowniak S. Safe Sex Fatigue, Treatment Optimism, and Serosorting: New Challenges to HIV Prevention Among Men Who Have Sex With Men. Journal of the Association of Nurses in AIDS Care. 2009;20(1):31–38. doi: 10.1016/j.jana.2008.09.006. https://doi.org/10.1016/j.jana.2008.09.006. [DOI] [PubMed] [Google Scholar]
- Ryzin MJV, Johnson AB, Leve LD, Kim HK. The Number of Sexual Partners and Health-Risking Sexual Behavior: Prediction from High School Entry to High School Exit. Archives of Sexual Behavior. 2010;40(5):939–949. doi: 10.1007/s10508-010-9649-5. https://doi.org/10.1007/s10508-010-9649-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snowden JM, Wei C, McFarland W, Raymond HF. Prevalence, correlates and trends in seroadaptive behaviours among men who have sex with men from serial cross-sectional surveillance in San Francisco, 2004–2011. Sexually Transmitted Infections. 2014;90(6):498–504. doi: 10.1136/sextrans-2013-051368. https://doi.org/10.1136/sextrans-2013-051368. [DOI] [PubMed] [Google Scholar]
- Stephenson R, White D, Mitchell JW. Sexual Agreements and Perception of HIV Prevalence Among an Online Sample of Partnered Men Who Have Sex with Men. Archives of Sexual Behavior. 2015;44(7):1813–1819. doi: 10.1007/s10508-015-0532-2. https://doi.org/10.1007/s10508-015-0532-2. [DOI] [PubMed] [Google Scholar]
- Vallabhaneni S, Li X, Vittinghoff E, Donnell D, Pilcher CD, Buchbinder SP. Seroadaptive practices: association with HIV acquisition among HIV-negative men who have sex with men. PloS One. 2012;7(10):e45718. doi: 10.1371/journal.pone.0045718. https://doi.org/10.1371/journal.pone.0045718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van de Ven P, Crawford J, Kippax S, Knox S, Prestage G. A scale of optimism-scepticism in the context of HIV treatments. AIDS Care. 2000;12(2):171–176. doi: 10.1080/09540120050001841. https://doi.org/10.1080/09540120050001841. [DOI] [PubMed] [Google Scholar]
- Ven DPVD, Kippax S, Crawford J, Rawstorne P, Prestage G, Grulich A, Murphy D. In a minority of gay men, sexual risk practice indicates strategic positioning for perceived risk reduction rather than unbridled sex. AIDS Care. 2002;14(4):471–480. doi: 10.1080/09540120208629666. https://doi.org/10.1080/09540120208629666. [DOI] [PubMed] [Google Scholar]
- Vermunt JK. Latent Class Modeling with Covariates: Two Improved Three-Step Approaches. Political Analysis. 2010;18(4):450–469. https://doi.org/10.1093/pan/mpq025. [Google Scholar]
- Zhang H, Lu H, Pan SW, Xia D, Zhao Y, Xiao Y, Shao Y. Correlates of unprotected anal intercourse: the influence of anal sex position among men who have sex with men in Beijing, china. Archives of Sexual Behavior. 2015;44(2):375–387. doi: 10.1007/s10508-014-0396-x. https://doi.org/10.1007/s10508-014-0396-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.