Abstract
Objective
Social impairment is a long recognized core feature of schizophrenia and common in other psychotic disorders. Still, to date the long-term trajectories of social impairment in psychotic disorders have rarely been studied systematically.
Methods
Data came from the Suffolk County Mental Health Project, a 20-year prospective study of first-admission patients with psychotic disorders. A never psychotic comparison group was assessed. We applied Latent Class Growth Analysis to longitudinal data on social functioning from 485 respondents with schizophrenia spectrum disorders and psychotic mood disorders and examined associations of the empirically derived trajectories with premorbid social adjustment, diagnosis, and 20-year outcomes.
Results
Four mostly stable trajectories of preserved (n = 82; 59th percentile of comparison group sample distribution), moderately impaired (n =148; 17th percentile), severely impaired (n = 181; 3rd percentile), and profoundly impaired (n = 74; 1st percentile) functioning best described the 20-year course of social functioning across diagnoses. Functioning in the preserved group did not differ from that of never psychotic individuals at 20-years, but the other groups functioned worse (all p < 0.001). Differences among trajectories were already evident in childhood. The two most impaired trajectories started to diverge in early adolescence. Poorer social functioning trajectories were strongly associated with other real-world outcomes at 20-years. Multiple trajectories were represented within each disorder. However, relatively more participants with schizophrenia spectrum disorders were in the impaired trajectories, and relatively more with mood disorders in the better functioning ones.
Conclusions
The results highlight substantial variability of social outcomes within diagnoses – albeit overall worse social outcomes in schizophrenia spectrum disorders- and show remarkably stable long-term impairments in social functioning after illness onset across all diagnoses.
1. Introduction
Impairment in social functioning is a core feature of schizophrenia. It is characterized by difficulties in achieving social milestones and establishing relationships, such as social network involvement, and marriage or family life (1-4). Real-world indices of functioning have gained increasing importance in investigations into recovery (5,6) and social functioning, defined as involvement in social interactions and social activities, has been recognized as a key outcome measure for determining treatment success (7,8).
In contrast to the growing awareness about its importance for tracking outcome, previous reports have left several issues unresolved. First, it has been shown that social outcomes in schizophrenia are poor (9) but prospective evaluations reported mixed findings, with improving (10-12) stable (13,14) and declining (15) social functioning after illness onset. In addition, studies generally examined group averages without taking differences between individuals within psychotic disorders into account. Averages can mask functional recovery or deterioration present in subgroups of patients. It is important to explicate the different long-term trajectories of social functioning in order to identify critical periods and specific trajectories that warrant intervention.
While considerable research has been done in schizophrenia, social outcomes in other psychotic illnesses have been less studied (15-17). It is generally assumed that schizophrenia is associated with worse social functional outcomes compared to other psychotic disorders, but the few studies that directly tested this assumption by comparing the longitudinal courses of social functioning between affective and non-affective psychoses have yielded conflicting findings. The pioneering work of Harrow and colleagues found evidence that social impairment was more severe in schizophrenia than other psychotic disorders at 7.5 and 15-year follow-up (9,18). However, two other studies reported comparable levels of social functioning between schizophrenia and affective psychosis. The first, a cross-sectional study, compared individuals with schizophrenia and bipolar disorder (19) and the second study compared affective disorders and schizophrenia 6-months after hospitalization (17). Thus, the evidence for diagnosis-specific differences in psychosocial functioning is inconsistent.
Moreover, while a wealth of research has shown that poor premorbid functioning is associated with poorer outcomes after illness onset at cross-sectional time-points, it remains unclear whether poor premorbid functioning is associated with continuously poor social trajectories. Finally, the findings across studies have been mixed in terms of how strongly social functioning is related to other daily life outcomes with results ranging from fairly weak to strong associations (20).
The current study aims to address these questions by examining differences in the trajectories of social functioning over 20 years across and within diagnostic groups in a large, countywide sample of first-admission individuals with affective and non-affective psychosis (21). We also sought to (a) examine associations of these trajectories with premorbid social functioning and (b) evaluate their associations with other areas of functioning at 20-year follow-up. Finally, we examined the severity of impairment of social functioning 20-years post-admission by comparing the trajectory groups to a never psychotic comparison group that was matched on demographic characteristics and neighborhood.
2. Method
2.1 Sample
Participants came from the Suffolk County Mental Health Project, a longitudinal countywide study of first-admission patients with a psychotic disorder (21,22). They were recruited from the 12 psychiatric inpatient units in the Suffolk County, NY between September 1989 and December 1995. Patients first hospitalized outside of Suffolk County or in non-psychiatric units were not sampled unless they were re-hospitalized within 6 months in one of the 12 study sites. Inclusion criteria were age 15–60, first admission either current or within six months, clinical evidence of psychosis, the ability to understand assessment procedures in English, IQ higher than 70; and the capacity to provide written informed consent. The study was approved annually by the Stony Brook IRB and IRBs of participating hospitals. Written informed consent was obtained. For participants aged 15–17, written consent was obtained from parents and verbal consent was obtained from participants. The response rate for individuals approached for baseline assessment during the recruitment period was 72%.
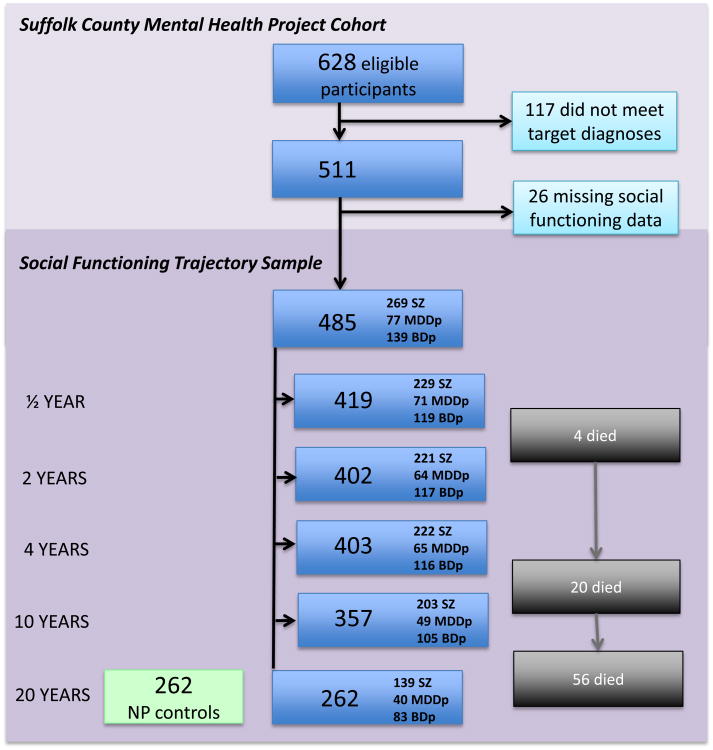
Initially, the Suffolk County Project interviewed 675 individuals. Of these 628 met the eligibility criteria (22). Figure 1 provides a flow chart of the analysis sample. Among the 628 eligible participants, 511 had one of the three target diagnoses included in this paper; schizophrenia spectrum disorder (schizophrenia, schizoaffective disorder, schizophreniform disorder), major depressive disorder with psychosis, and bipolar disorder with psychosis. Seventy-one patients with psychosis not otherwise specified and 46 individuals with drug-related psychoses were excluded from the current study. Further, 66 individuals did not complete any social functioning assessment, resulting in a final analysis sample of n = 485 individuals with at least one data point. The 66 drop-outs did not differ from the analysis sample in terms of sex, age or diagnosis (all p > 0.05). At the 20-year point, of the 485 included participants 262 were assessed and 56 had died. Non-response was primarily accounted for by refusal to participate and loss to follow-up. Overall, 40.6% of the 485 participants who took part in our study completed all five assessments, 21.2% four, 21.7% three, 10.5% two, and 6.0% one assessment. Attrition within the analysis sample seemed random, that is, the number of assessments was not associated with age, sex, negative symptoms, positive symptoms, employment, public assistance, independent living, homelessness, or baseline diagnosis.
Figure 1. Flowchart of social functioning analyses sample.
Legend: Abbreviations: SZ=schizophrenia spectrum disorder; BDp =bipolar disorder with psychosis; MMDp = major depression with psychosis. NP = never psychotic comparison group. Diagnoses were made at the 10 -year follow-up point or last available assessment. The total number of participants with at least one social functioning assessment was 485.
Respondents completed face-to-face interviews at baseline, 6 months, 2 years, 4 years, 10 years, and 20 years. The initial social functioning assessment was taken at 6 months when participants were no longer in the hospital. Thus, the 6 months assessment was used as the starting point for the functional trajectories.
To obtain a benchmark for social functioning, a never-psychotic comparison group was recruited at the 20-year time point for respondents living within a 50- mile radius of Stony Brook University. We used a 2-step procedure approved by the Stony Brook IRB. Step 1, performed by the Stony Brook University Center for Survey Research, involved random digit dialing within zip codes selected in proportion to cases residing there. The goal was to obtain a sample with a similar age and sex distribution and no history of psychosis. The initial number of randomly-generated telephone numbers was 12,388; 2,594 were inactive, 4,321 went unanswered, and 4,291 were ineligible (outside the age/sex target for the zip code or had a psychosis diagnosis or psychiatric hospitalization). Of the eligible households (n = 1182), 750 refused participation, and 432 agreed to consider participating in the study and provided a time when they could best be re-contacted by study staff.
Step 2, conducted by trained study staff, involved telephone re-screening of the 432 potentially eligible participants. The re-screen included an adaptation of the 6-item psychosis screening questionnaire (23) covering visual and auditory hallucinations, thought insertion, paranoia, strange experiences, and diagnosis of schizophrenia or schizoaffective disorder. Twenty individuals could not be reached or were unavailable for re-screening. Of the remaining 412, 58 refused participation, 49 could not be scheduled, and 35 disclosed psychotic symptoms. Of the remaining 270 who participated in the study, 8 endorsed psychotic symptoms on the SCID and were removed from the sample. The final comparison group was composed of 262 participants and was closely matched to the cases on sex (55.94% vs. 56.70% male) and age (mean: 50.46 years (SD= 9.02) vs 48.14 years (SD= 9.14).
2.2 Measures of social functioning
The social functioning index was based on a composite of three items relating to relationships, and activities with other people (ranging from 0 (extremely poor) to 6 (satisfactory)) for social activity and social sexual relationships, and 1 to 5 for relationships with friends, from the Heinrichs-Carpenter Quality of Life Scale (24). The Quality of Life Scale is a semi-structured interview with multiple probes providing information for each interviewer rating. For example, questions in the ‘relationships with friends’ domain include: “Do you have friends with whom you are especially close other than your immediate family or the people you live with?”, “How many friends do you have?”, and “How often have you spoken with them recently, in person or by phone?”. Ratings were based on information from the participant, as well as information from significant others and medical records when available. Information of significant others was available for 66.83% of participants who completed the 6 months assessment and decreasing to 48.1% of participants who completed the assessment at 20 years. The availability of this information did not differ between classes at any of the time points. Medical records were available for 82.58% of participants at 6 months and 55.3% of participants at 20 year follow-up. At baseline significantly more records were available for lower functioning individuals (class 1 = 92%, class 2 = 84.5%, class 3 = 83.1% and class 4 = 73.1%). There was no difference between classes at 20 year follow-up. The composite score ranged from 1 to 17 and showed acceptable internal reliability at each assessment (α ranged from 0.79 to 0.88).
Premorbid social functioning
The Premorbid Adjustment Scale (25) was administered at 6 months follow-up. Ratings were based on a semi-structured interview developed to match Premorbid Adjustment Scale criteria, as well as information obtained from significant others, which was available for 79.6% of participants and school records, which were available for 63% of participants. Overall, 88.45% had additional information to complement PAS scores. Items were rated on a 7-point scale, with 6 reflecting lowest and 0 reflecting highest social functioning. To compare Premorbid Adjustment Scale scores with the Quality of Life Scale, items were re-scaled so that higher scores indicated better functioning. Three subscales relevant to social contact were included: sociability and social withdrawal (frequency of, and interest in social contact), peer relationships (the quality of relationships with people of own age), and socio-sexual relationships (sexual interest). Here we report Premorbid Adjustment Scale social functioning scores in childhood (up to age 11), early adolescence (age 12 to 15) and late adolescence (age 15 to 18). Childhood ratings did not include socio-sexual relationships. For comparability, we multiplied the childhood score by 1.5.
To equate the metrics of pre-and post-admission functioning, we compared distributions of the late adolescent Premorbid Adjustment Scale scores (ages 15-18) with Quality of Life Scale scores of participants first assessed before age 19 (n = 29), where the scores should be identical if they indeed reflected the same outcome. Distributions of the two composites were largely parallel, but Premorbid Adjustment Scale scores (mean = 13.38; SD = 3.35; median = 14; 10th = 8; 25th = 11 ½; 75th = 16; 90th = 18) were around three points higher than Quality of Life Scale scores (mean = 10.78; SD = 3.70; median = 11; 10th = 5; 25th = 9; 75th = 13; 90th = 15). To make the scores on both scales comparable, we therefore applied a transformation whereby we adjusted the Premorbid Adjustment Scale scores by subtracting three points. To avoid confounding of premorbid and post-admission social functioning at 6 months, Premorbid Adjustment Scale data for those whose age of first admission was <19 years (n = 29) were not included in the analyses.
Diagnosis
Face-to-face assessments were conducted by master-level mental health professionals at each time point, including the Structured Clinical Interview for DSM-IV (26). The assessors were blind to participants' research diagnoses. However, out of respect to the sample and to maximize the accuracy of information gathered in the interview, raters were asked to review past interview material. Thus they were aware of the SCID diagnoses (which did not always correspond with the research diagnosis). Primary DSM-IV diagnosis was formulated by consensus of 4 or more psychiatrists using all available longitudinal information, including SCID interviews, medical records, and significant other information. We used the last available diagnosis to select the study sample. For the majority of individuals, this was the 10 year follow-up consensus diagnosis. For 91 individuals without a 10 year diagnosis, we substituted the temporally most proximal prior diagnosis.
Symptom Measures
At each time point, symptoms were assessed with the Scale for the Assessment of Positive Symptoms (SAPS) (27) and the Scale for the Assessment of Negative Symptoms (SANS) (28) which rate the presence of symptoms on a 6-point scale from absent (0) to severe (5). The SAPS assesses hallucinations, delusions, bizarre behavior, and thought disorder. We were interested in the psychosis subscale (SAPS-P), a composite of 16 ratings measuring hallucinations and delusions (range 0-80; α internal consistency ranged from 0.81 to 0.89). Factor analysis identified two dimensions within the SANS: inexpressivity and avolition/asociality, which parallel prior findings (29). We were particularly interested in inexpressivity (SANS-E), a composite of 9 items measuring blunted affect and alogia (range 0-45; α ranged from 0.89 to 0.91), because avolition/asociality is conceptually overlapping with social functioning.
Other functional outcomes
Other functional outcomes that were assessed in the 20 year follow-up interview were: having a high school diploma (yes/no), employment status (being employed yes/no), homelessness in past 10 years (yes/no), financial independence (on public assistance yes/no), and living independently (own household or not).
2.3 Data analyses
Analyses were conducted in STATA 13 (30) and MPlus version 7.2 (31). Demographic characteristics were compared using regression analyses or Chi-square tests.
To examine functioning trajectories of participants, we conducted Latent Class Growth Analyses, a method used to discover subgroups (classes) of individuals following distinct patterns of change over time. In our case, individual class membership was assigned on the basis of social functioning scores from 6 months to 20 years, making use of all available data with maximum likelihood estimation and robust standard errors to account for missing data (i.e., Full Information Maximum Likelihood) (31,32). To determine the appropriate number of latent classes, the analysis is run from a one-class model to increasing numbers of classes. To compare models with the different numbers of classes and determine the optimum model fit, we examined the recommended fit indices: entropy, Akaike's Information Criterion and Bayesian Information. Highest entropy and lowest Akaike's Information Criterion and Bayesian Information Criterion suggest the best fit and parsimony of the model (31). Values of 0.4, 0.6, and 0.8 represent low, medium, and high entropy (33). To assess model fit we also consulted the Vuong-Lo-Mendell-Rubin test (in which a significant p-value indicates that this model fits significantly better than a model with a lower number of classes (34,35)). Two piecewise multilevel regression analyses accounting for multiple observations within individuals were conducted to compare the slopes of the four different trajectories from 6 months to 4 years and from 10 to 20 years between classes.
To determine how functional trajectories map onto the current diagnostic classification, we calculated the distribution of schizophrenia spectrum disorder, major depressive disorder with psychosis and bipolar disorder with psychosis diagnoses across the resulting Latent Class Growth Analyses trajectories.
Regression analyses were used to examine how the Latent Class Growth Analyses trajectories were associated with premorbid functioning (childhood, early- and late adolescence), with differences in the change from premorbid functioning in late adolescence to functioning after illness onset, and with other 20-year functional outcomes. Overall differences in social functioning at 20-years follow-up between the latent trajectory groups and the comparison group were evaluated with Chi-square analyses.
3. Results
The sample consisted of 269 participants diagnosed with a schizophrenia spectrum disorder (76.6% schizophrenia, 21.9% schizoaffective, 1.5% schizophreniform; 65.8% male; mean age at baseline: = 29.0 (SD= 8.92, median=28.0), 77 with major depressive disorder with psychosis (41.6% male; mean age at baseline= 30.81 (SD=10.84, median=30.0)), and 139 participants with bipolar disorder with psychosis (47.5% male; mean age at baseline= 29.18, (SD= 9.81, median=27.0)).
3.1 Trajectories of social functioning in psychotic disorders
We selected the 4-class model as it performed best on most fit indices (Supplementary table). The 4-class model fit was best on the Akaike's Information Criterion and Bayesian Information Criterion. The Vuong-Lo-Mendell-Rubin test indicated that the fit was significantly better for the 4-class than 3-class model (p = 0.035), but the 5-class model did not significantly improve fit. Entropy was medium (0.65) for the 4-class model, and mean class probabilities were moderate to high (0.76- 0.81), suggesting that with the 4-class model individuals were likely to be correctly assigned to a latent class. Information clinical symptoms and antipsychotic treatment by trajectory class is presented in Table 1 and Table 2.
Table 1. Symptoms and medication.
| Variable | Class | Mean (SD) | Tukey Grouping* | Statistics | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| SANS-E** 6 mnths | (1) Profoundly Impaired | 12.26 (9.50) | A | t=-6.90, p<0.001 | |||
| (2) Severely Impaired | 9.75 (8.95) | B | |||||
| (3) Moderately Impaired | 5.53 (6.39) | C | |||||
| (4) Preserved | 1.44 (3.24) | D | |||||
|
| |||||||
| SANS-E 2 years | (1) Profoundly Impaired | 12.42 (9.01) | A | t=-8.02, p<0.001 | |||
| (2) Severely Impaired | 8.31 (8.23) | B | |||||
| (3) Moderately Impaired | 3.80 (5.32) | C | |||||
| (4) Preserved | 1.00 (1.69) | D | |||||
|
| |||||||
| SANS-E 4 years | (1) Profoundly Impaired | 12.12 (9.86) | A | t=-6.30, p<0.001 | |||
| (2) Severely Impaired | 7.93 (8.33) | B | |||||
| (3) Moderately Impaired | 3.76 (6.17) | C | |||||
| (4) Preserved | 0.72 (2.24) | C | |||||
|
| |||||||
| SANS-E 10 years | (1) Profoundly Impaired | 10.26 (9.56) | A | t=-4.02, p<0.001 | |||
| (2) Severely Impaired | 7.17 (7.95) | A | |||||
| (3) Moderately Impaired | 3.41 (5.61) | B | |||||
| (4) Preserved | 1.29 (3.22) | B | |||||
|
| |||||||
| SANS-E 20 years | (1) Profoundly Impaired | 14.70 (10.59) | A | t=-4.70, p<0.001 | |||
| (2) Severely Impaired | 9.24 (9.93) | B | |||||
| (3) Moderately Impaired | 6.19 (8.42) | B | C | ||||
| (4) Preserved | 2.55 (4.02) | C | |||||
|
| |||||||
| SAPS 6 months | (1) Profoundly Impaired | 5.73 (8.90) | A | t=-4.66, p<0.001 | |||
| (2) Severely Impaired | 4.46 (7.47) | A | |||||
| (3) Moderately Impaired | 1.51 (3.20) | B | |||||
| (4) Preserved | 0.63 (2.45) | B | |||||
|
| |||||||
| SAPS 2 years | (1) Profoundly Impaired | 4.56 (6.62) | A | t=-2.33, p=0.020 | |||
| (2) Severely Impaired | 4.13 (6.34) | B | |||||
| (3) Moderately Impaired | 2.41 (5.19) | A | |||||
| (4) Preserved | 0.89 (3.91) | A | |||||
|
| |||||||
| SAPS 4 years | (1) Profoundly Impaired | 4.20 (6.90) | A | t=-1.99, p=0.048 | |||
| (2) Severely Impaired | 3.80 (6.97) | A | |||||
| (3) Moderately Impaired | 1.98 (4.35) | A | |||||
| (4) Preserved | 0.82 (2.53) | A | |||||
|
| |||||||
| SAPS 10 years | (1) Profoundly Impaired | 6.28 (8.43) | A | t=-2.02, p=0.044 | |||
| (2) Severely Impaired | 6.36 (9.93) | B | |||||
| (3) Moderately Impaired | 3.25 (6.76) | A | |||||
| (4) Preserved | 0.42 (1.43) | A | |||||
|
| |||||||
| SAPS 20 years | (1) Profoundly Impaired | 8.58 (8.99) | A | t=-3.48, p=0.001 | |||
| (2) Severely Impaired | 6.52 (10.16 | A | |||||
| (3) Moderately Impaired | 2.80 (4.99) | B | |||||
| (4) Preserved | 0.31 (1.0) | B | |||||
|
| |||||||
| % (n) | |||||||
|
| |||||||
| AP use*** BL-6 mnths | (1) Profoundly Impaired | 85.1 (63) | A | t=-3.75, p<0.001 | |||
| (2) Severely Impaired | 78.3 (114) | A | |||||
| (3) Moderately Impaired | 75.0 (111) | A | |||||
| (4) Preserved | 58.5 (48) | B | |||||
|
| |||||||
| AP use 6 mnths – 2 years | (1) Profoundly Impaired | 79.5 (58) | A | t=-6.25, p<0.001 | |||
| (2) Severely Impaired | 65.2 (116) | B | |||||
| (3) Moderately Impaired | 52.7 (77) | C | |||||
| (4) Preserved | 36.6 (30) | D | |||||
|
| |||||||
| AP use 2 -4 years | (1) Profoundly Impaired | 74.0 (54) | A | t=-7.35, p<0.001 | |||
| (2) Severely Impaired | 59.3 (105) | B | |||||
| (3) Moderately Impaired | 44.2 (65) | C | |||||
| (4) Preserved | 24.4 (20) | D | |||||
|
| |||||||
| AP use At 10 years | (1) Profoundly Impaired | 87.7 (50) | A | t=-7.36, p<0.001 | |||
| (2) Severely Impaired | 72.0 (103) | B | |||||
| (3) Moderately Impaired | 58.9 (63) | C | |||||
| (4) Preserved | 31.2 (19) | D | |||||
|
| |||||||
| AP use At 20 years | (1) Profoundly Impaired | 77.8 (28) | A | t=-6.46, p<0.001 | |||
| (2) Severely Impaired | 73.9 (65) | A | |||||
| (3) Moderately Impaired | 56.2 (50) | B | |||||
| (4) Preserved | 26.4 (14) | C | |||||
Note: BL= baseline, SANS-E= Scale for the Assessment of Negative Symptoms – inexpressivity, SAPS= Scale for the Assessment of Positive Symptoms, AP= antipsychotics
Tukey grouping: Means with the same letter are not significantly different.
All SANS-E and SAPS scores are controlled for diagnosis, age and sex.
All AP analyses are controlled for gender, and age. AP use for BL-6 mnths, 6 mnths- years and 2-4 years reflects the % time on AP between the two time points first (25% cut off). AP use at 10 years and 20 years reflects use at time of assessment (25% cut off)
Table 2. Associations of sample characteristics and outcomes with trajectory class.
| Variable | Class | Mean/% | Tukey Grouping* | Statistics* | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Baseline / 6 mnths characteristics | % (n) | ||||||
|
| |||||||
| Male | Profoundly Impaired | 71.6 (53) | A | χ2(3)=27.06, p<0.001 | |||
| Severely Impaired | 64.7 (117) | A | |||||
| Moderately Impaired | 50.7 (75) | B | |||||
| Preserved | 36.6 (30) | C | |||||
|
| |||||||
| White-caucasian | Profoundly Impaired | 64.8 (48) | A | B | χ2(3)=23.74, p<0.001 | ||
| Severely Impaired | 69.9 (126) | A | |||||
| Moderately Impaired | 80.4 (119) | B | C | ||||
| Preserved | 92.7 (76) | C | |||||
|
| |||||||
| Unemployed 6 mnths | Profoundly Impaired | 76.1 (48) | A | χ2(3)=88.03, p<0.001 | |||
| Severely Impaired | 64.2 (106) | A | |||||
| Moderately Impaired | 35.5 (49) | B | |||||
| Preserved | 10.7 (8) | C | |||||
|
| |||||||
| Public assistance 6 mnths | Profoundly Impaired | 47.6 (30) | A | χ2(3)=41.08, p<0.001 | |||
| Severely Impaired | 46.3 (76) | A | |||||
| Moderately Impaired | 23.9 (33) | B | |||||
| Preserved | 10.7 (8) | C | |||||
|
| |||||||
| Independent living 6 mnths | Profoundly Impaired | 20.6 (13) | A | χ2(3)=26.04, p<0.001 | |||
| Severely Impaired | 26.8 (44) | A | |||||
| Moderately Impaired | 44.6 (62) | B | |||||
| Preserved | 52.6 (40) | B | |||||
|
| |||||||
| Homelessness** Baseline | Profoundly Impaired | 25 (14) | χ2(3)=7.47, p=.06 | ||||
| Severely Impaired | 26.5 (36) | ||||||
| Moderately Impaired | 18.6 (22) | ||||||
| Preserved | 10.8 (7) | ||||||
|
| |||||||
| Mean (SD) | |||||||
|
| |||||||
| Onset age*** | Profoundly Impaired | 30.15 (16.61) | t=-1.65, p=.10 | ||||
| Severely Impaired | 29.72 (14.29) | ||||||
| Moderately Impaired | 28.64 (13.11) | ||||||
| Preserved | 29.80 (11.16) | ||||||
|
| |||||||
| Age*** | Profoundly Impaired | 30.32 (9.43) | t=-1.79, p=.074 | ||||
| Severely Impaired | 29.51 (9.22) | ||||||
| Moderately Impaired | 28.11 (8.95) | ||||||
| Preserved | 30.30(10.99) | ||||||
|
| |||||||
| 20 year outcomes | % (n) | ||||||
|
| |||||||
| No diploma | Profoundly Impaired | 9.46 (7) | A | B | χ2(3)=11.78, p<0.01 | ||
| Severely Impaired | 10.50 (19) | A | |||||
| Moderately Impaired | 3.38 (5) | B | C | ||||
| Preserved | 1.22 (1) | C | |||||
|
| |||||||
| Unemployed | Profoundly Impaired | 97.2 (35) | A | χ2 (3) =46.36, p<0.001 | |||
| Severely Impaired | 80 (72) | B | |||||
| Moderately Impaired | 52.8 (47) | C | |||||
| Preserved | 40 (22) | C | |||||
|
| |||||||
| Public Assistance | Profoundly Impaired | 94.44 (34) | A | χ2(3)=62.83 p<0.001 | |||
| Severely Impaired | 85.56 (77) | A | |||||
| Moderately Impaired | 55.06 (49) | B | |||||
| Preserved | 30.91 (17) | C | |||||
|
| |||||||
| Independent living | Profoundly Impaired | 43.8 (14) | A | χ2(3)=30.77 p<0.001 | |||
| Severely Impaired | 48.9 (46) | A | |||||
| Moderately Impaired | 68.5 (63) | B | |||||
| Preserved | 90.4 (47) | C | |||||
|
| |||||||
| Homelessness | Profoundly Impaired | 16.67 (6) | χ2(3)=0.22, p=0.98 | ||||
| Severely Impaired | 14.77 (13) | ||||||
| Moderately Impaired | 13.48 (12) | ||||||
| Preserved | 14.5 (8) | ||||||
Note: BL = baseline,
Tukey grouping: Means with the same letter are not significantly different.
homelessness rating is based on any time in lifetime before baseline and between 10-20 years,
Controlled for diagnosis and sex
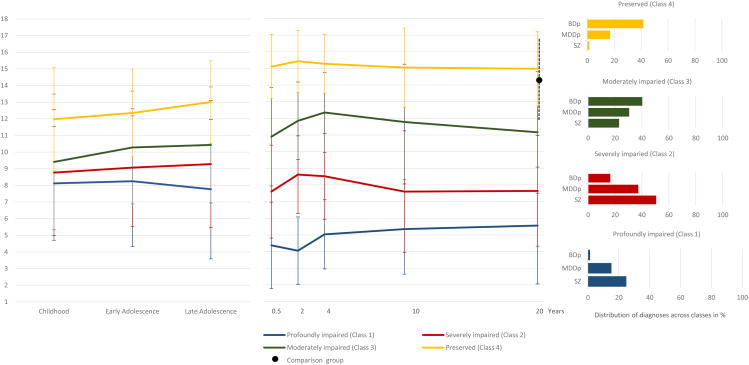
Figure 2 and Table 3 present the social functioning trajectories from 6 months to 20 years. The classes represented groups with profoundly impaired (Class 1; n = 74; 1st percentile of comparison group sample distribution), severely impaired (Class 2; n = 181; 3rd percentile), moderately impaired (n = 148; 17th percentile) and preserved (n = 82; 59th percentile of comparison group sample distribution) social functioning. Piecewise multilevel regression analyses were conducted to compare the slopes of the trajectories from 6 months to 4 years and from 10 to 20 years between classes. The results of the first analysis showed a significant effect of class (B = 3.55, SE = .12, p < .001) and time point (B = .54, SE = .23, p < .05), but no significant interaction. The second analysis from 10 to 20 years only revealed a significant class effect (B = 3.49, SE = .89, p < .001). The trajectories of the 4 classes were largely parallel, differing in degree of severity but not in shape. At the 20-year time point, the profoundly (B = -8.61, SE= .55, p < 0 .001), severely (B = -6.54, SE= .38, p < 0.001) and moderately (B = -3.02, SE= .37, p < 0.001) impaired trajectories showed significantly worse social functioning than the comparison group individuals. There was no significant difference in 20-year social functioning between those in the preserved class (B = .81, SE= .45, p = 0.07) and comparison group individuals (mean = 14.17, SD = 2.74).
Figure 2. Trajectories of functioning across psychotic disorders derived from Latent Class Growth Analyses.
Legend: Abbreviations: SZ=schizophrenia spectrum disorder; BDp =bipolar disorder with psychosis; MMDp = major depression with psychosis.
Table 3. Social functioning by time point and social engagement trajectory class.
| Variable | Class* | Mean (SD) | Tukey Grouping** | Statistics | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| PAS childhood*** | (1) Profoundly Impaired | 8.12 (3.42) | A | t=5.62, p<0.001 | |||
| (2) Severely Impaired | 8.77 (3.78) | A | B | ||||
| (3) Moderately Impaired | 9.41 (4.10) | B | |||||
| (4) Preserved | 12.00 (3.13) | C | |||||
|
| |||||||
| PAS Adolescence | (1) Profoundly Impaired | 8.25 (3.93) | A | t=6.38, p<0.001 | |||
| (2) Severely Impaired | 9.07 (3.54) | A | |||||
| (3) Moderately Impaired | 10.28(3.39) | B | |||||
| (4) Preserved | 12.36 (2.69) | C | |||||
|
| |||||||
| PAS late adolescence | (1) Profoundly Impaired | 7.75 (4.25) | A | t=5.67, p<0.001 | |||
| (2) Severely Impaired | 9.23 (3.88) | B | |||||
| (3) Moderately Impaired | 10.44 (3.52) | B | |||||
| (4) Preserved | 13.03 (2.541) | C | |||||
|
| |||||||
| Social functioning 6 mnths**** | (1) Profoundly Impaired | 4.37 (2.60) | A | t=21.81, p<0.001 | |||
| (2) Severely Impaired | 7.60 (2.79) | B | |||||
| (3) Moderately Impaired | 10.90 (2.96) | C | |||||
| (4) Preserved | 15.11 (1.93) | D | |||||
|
| |||||||
| Social functioning 2 years | (1) Profoundly Impaired | 4.05 (2.03) | A | t=27.65, p<0.001 | |||
| (2) Severely Impaired | 8.62 (2.33) | B | |||||
| (3) Moderately Impaired | 11.85 (2.33) | C | |||||
| (4) Preserved | 15.43 (1.86) | D | |||||
|
| |||||||
| Social functioning 4 years | (1) Profoundly Impaired | 5.03 (2.08) | A | t=24.81, p<0.001 | |||
| (2) Severely Impaired | 8.52 (2.58) | B | |||||
| (3) Moderately Impaired | 12.35 (2.39) | C | |||||
| (4) Preserved | 15.28 (1.76) | D | |||||
|
| |||||||
| Social functioning 10 years | (1) Profoundly Impaired | 5.35 (2.71) | A | t=14.03, p<0.001 | |||
| (2) Severely Impaired | 7.60 (3.65) | B | |||||
| (3) Moderately Impaired | 11.78 (3.47) | C | |||||
| (4) Preserved | 15.05 (2.38) | D | |||||
|
| |||||||
| Social functioning 20 years | (1) Profoundly Impaired | 5.56 (3.51) | A | t=13.18, p<0.001 | |||
| (2) Severely Impaired | 7.64 (3.32) | B | |||||
| (3) Moderately Impaired | 11.16 (3.66) | C | |||||
| (4) Preserved | 14.98 (2.24) | D | |||||
Note.
Tukey grouping: Means with the same letter are not significantly different
Number of participants per class: Class 1=74, Class 2=181, Class 3=148, Class 4=82.
Adjusted Premorbid Adjustment Scale (PAS) scores. All PAS analyses are controlled for diagnosis and sex.
All Social functioning analyses are controlled for diagnosis, sex and age
3.2 Characteristics of the social functioning trajectory groups
3.2.1 Trajectories and diagnosis
The distribution of the three diagnostic groups varied widely across the trajectory classes (χ2(6) = 171.26, p < .001, see Figure 2), showing that there is substantial individual variation in social functioning within each of the three disorders.
3.2.2. Trajectories and premorbid functioning
Figure 2 also demonstrates the association of the social functioning trajectories with premorbid social development. The two main findings are that, at group level, differences in social functioning between the four classes are already evident in childhood, and that those with worse social functioning in childhood experience a larger decline in social functioning from adolescent Premorbid Adjustment Scale scores to Quality of Life Scale scores 6 months after first admission. This decline from premorbid to post morbid functioning was significant in the two lowest profoundly and severely impaired functioning classes (Class 1: mean difference = -4.49, SD = 4.06, p < 0.001; Class 2: mean difference= -1.98, SD = 3.94; p < 0.001). Functioning in the moderately impaired Class 3 remained stable (mean difference = -.28, SD = 3.89; p = .49). In line with normal developmental changes, there was a significant improvement in the level of social functioning from premorbid to post-morbid functioning in Class 4 (mean difference = 2.22, SD = 2.96; p < 0.001).
3.2.3. Trajectories and 20-year functional outcomes
Table 3 presents the associations of the social functioning trajectories with demographics and outcomes at year 20. The trajectories of profoundly (Class 1) and severely impaired social functioning (Class 2) were associated with worse 20-year real life functional outcomes in a variety of domains, such as not having obtained a high school diploma, unemployment, not living independently, and the use of public assistance. The moderately impaired (Class 3) and the preserved trajectory (Class 4) only differed from each other in independent living and public assistance.
4. Discussion
Psychotic disorders are associated with profound social impairments (32,33). It is often implicitly assumed that these impairments fluctuate and that the course of social functioning is worse in schizophrenia compared to other affective psychotic disorders (34). Yet, only limited research directly addressed cross-diagnostic and individual variation in patients' social outcomes over time. Our study went beyond investigations that considered individual disorders by examining latent trajectories in the 20-year course of social functioning across three broad psychotic disorder groups. Using Latent Growth Curve modeling we detected four remarkably stable trajectories of preserved, moderately, severely, and profoundly impaired social functioning. Interestingly, our findings reveal that multiple of these classes were found in schizophrenia spectrum disorders, psychotic bipolar disorder and psychotic depression.
In addition, our findings suggest that differences in the level of social functioning among these 20-year trajectories were already evident in childhood. The years between early adolescence and first hospitalization appear to be a period in which a substantial number of individuals who later develop a psychotic disorder display a steep decline in social functioning. This extends the findings of earlier research that investigated social functioning within diagnostic categories by showing that premorbid adjustment is not only a strong predictor of social functioning over three years following illness onset in schizophrenia spectrum disorders (35), but that premorbid adjustment also predicts social outcome for patients with bipolar disorder with psychosis and major depressive disorder with psychosis. Besides, the level of social functioning after the acute illness phase in schizophrenia spectrum disorders, bipolar disorder with psychosis and major depressive disorder with psychosis turned out to be relatively stable (12,15,36,37).
Particularly the two lower social functioning trajectories were associated with other unfavorable psychosocial outcomes at 20-year follow-up. This suggests that social functioning is a valuable indicator of long-term outcome and that it may be an important treatment target in psychotic disorders that could lead to improvements in other areas of functioning. It also shows the value of a recovery-oriented perspective of mental health services; in the sense of helping patients to formulate adjusted but meaningful (social) goals (38).
In sum, the current findings expand existing knowledge on social functioning in psychotic disorders by showing that severe and persistent social impairment preceded by a drop in social functioning in adolescence is common in schizophrenia spectrum disorders (75%), but is not limited to the schizophrenia spectrum, because it is also present in about 35% of participants with major depressive disorder with psychosis and about 18% of cases with bipolar disorder with psychosis. On the other hand, a substantial number of individuals with bipolar disorder with psychosis (42%) and major depressive disorder with psychosis (26%), but hardly any individuals with schizophrenia spectrum disorders (1.5%), achieved levels of social functioning after illness onset that were similar to that of the comparison group. Our results suggest that, at group level, the trajectories of social functioning do not exhibit marked changes after illness onset (e.g. showing improvement or deterioration) as previously suggested (39,40). Whereas small improvements in social functioning are visible in all classes in the first years after onset, the overall trajectories follow comparable, rather stable courses, which are mostly characterized by differences in severity. These differences are also reflected by differences in medication intake: the more severe social impairment, the higher the anti-psychotic medication intake. This finding, of course, does not imply causality (arguably, it may be that both antipsychotic use and social impairment are the direct consequences of symptom severity), yet it would be interesting to investigate the effect of prolonged medication on real-life outcomes.
Our findings are in line with those of the FUNCAP study, wherein real-world outcomes and its determinants were being examined in individuals with schizophrenia and bipolar disorder. Also here, social impairment was found to be more prominent but not limited to schizophrenia (45,46). Their results also provided important etiological clues, suggesting that social functioning in both schizophrenia and bipolar disorder seems largely driven by performance on functional capacity measures (measuring the capacity to perform everyday task, such as communication skills needed in daily interactions). Although this hypothesis needs further testing, it may explain at least part of our findings and suggests that similar pathways to poor social functioning apply across mental disorders.
Of interest is our finding that, in contrast to research that compared patients diagnosed with major depression versus bipolar disorder without psychosis (47), Suffolk County participants with bipolar disorder had consistently better outcomes than individuals with psychotic depression. A potential explanation is that psychotic depression is a more severe illness than major depressive disorder without psychosis, which is the majority of what was examined in prior comparisons.
Our results should be interpreted in light of the following limitations. First, the Suffolk County project provided a unique opportunity to prospectively follow-up a large sample for two decades; however the gaps between the later follow-up assessments were large (6 and 10 years, respectively) and may have overlooked short-term changes in social functioning. Second, premorbid functioning was assessed retrospectively, which may limit the reliability of these data. We sought to mitigate this issue by integrating participant data with information from family members and school records. Third, critical data on factors that might more directly influence unfavorable social outcomes in people with psychosis, such as social-cognitive ability; effects of early social modeling from parents, relatives, and friends; and idiographic experiences (early social reinforcement and social rejection), was not available and we were therefore not able to perform analyses of the potential determinants of poor functional outcome. Fourth, raters were aware of previous SCID diagnoses, which might be a source of bias. However, raters were unaware of both the study diagnosis (decided by study psychiatrists) and hypotheses of the current study, and social functioning was not a primary target of the study. Fifth, our focus was to investigate associations of social functioning trajectories with other 20-year outcomes; however, in order to assess the value of social functioning in relation to other real world outcomes, it will be important to establish experimentally whether improvement in social functioning (e.g., with treatment) can indeed lead to other favorable outcomes and to determine whether trajectories of functioning in other domains (e.g., employment; life satisfaction) are parallel to the social functioning trajectories. The current sample had no systematic treatment aimed at social functioning and future studies should examine how specific treatment might influence social functioning in the long run. Finally, Latent Class Growth Curve Analysis offers a powerful method for studying between-person differences in longitudinal change. However, because it models a single trajectory for all members of a class (35), we may have missed patterns where a few individuals show greater change than the rest of the class. Importantly, our results show large individual variation within groups (as indicated by the error-bars in figure 2), and do not allow for conclusions about individual performance.
Clinical implications
Persistent impairments observed in approximately half of the sample emphasize the need for targeted, long-term care aimed at improving social inclusion for those with low social functioning at illness onset. Our findings indicate that 53% of the cases decline markedly in their social functioning between late adolescence and first hospitalization, a finding that has been supported by two other studies using Latent Class Growth Curve Analysis (41,42). This and the high temporal stability of the trajectories extend previous findings suggesting that the level of social functioning may be determined in adolescence. Consequently, our findings are consistent with recent programs of research focused on adolescence as the critical intervention window and support current early intervention strategies for high-risk individuals (43) and those that offer intensive treatment to first admission patients (44) aimed to prevent social withdrawal in severe psychotic illnesses.
Supplementary Material
Supplementary table. Fit indices LCGA
Acknowledgments
Disclosures: Dr Kotov and Dr Bromet received grant support of National Institutes of Health [#MH094398 and #MH44801 respectively]. Dr. Velthorst received support from the Netherland Organization for Scientific Research (NWO) VENI Grant [#916-15-005]. Dr. Fett received support from the Netherland Organization for Scientific Research (NWO) VENI Grant [#451-13-035] and a [2015] NARSAD Young Investigator Award from the Brain and Behavior Foundation. Dr. Perlman was supported by a [2013] NARSAD Young Investigator Award from the Brain and Behavior Foundation.
The National Institutes of Health and the Netherland Organization for Scientific Research had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. All authors report no financial relationships with commercial interests. We thank the mental health professionals in Suffolk County, the project psychiatrists and staff, and most of all, the study participants and their families and friends. The project psychiatrists and staff received their usual salary support; no others were paid for their services.
References
- 1.Fett AK, Viechtbauer W, Dominguez MD, Penn DL, van Os J, Krabbendam L. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: a meta-analysis. Neurosci Biobehav Rev. 2011 Jan;35(3):573–588. doi: 10.1016/j.neubiorev.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 2.Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “right stuff”? Schizophr Bull. 2000;26(1):119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- 3.Harvey PD. Disability in schizophrenia: contributing factors and validated assessments. J Clin Psychiatry. 2014;75(1):15–20. doi: 10.4088/JCP.13049su1c.03. [DOI] [PubMed] [Google Scholar]
- 4.Bellack AS, Green MF, Cook JA, Fenton W, Harvey PD, Heaton RK, et al. Assessment of community functioning in people with schizophrenia and other severe mental illnesses: a white paper based on an NIMH-sponsored workshop. Schizophr Bull. 2007 May;33(3):805–822. doi: 10.1093/schbul/sbl035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Charzynska K, Kucharska K, Mortimer A. Does employment promote the process of recovery from schizophrenia? A review of the existing evidence. Int J Occup Med Environ Health. 2015;28(3):407–418. doi: 10.13075/ijomeh.1896.00341. [DOI] [PubMed] [Google Scholar]
- 6.Liberman RP, Gutkind D, Mintz J, Green M, Marshall BD, Jr, Robertson MJ, et al. Impact of risperidone versus haloperidol on activities of daily living in the treatment of refractory schizophrenia. Compr Psychiatry. 2002 Nov-Dec;43(6):469–473. doi: 10.1053/comp.2002.33499. [DOI] [PubMed] [Google Scholar]
- 7.Green MF, Hellemann G, Horan WP, Lee J, Wynn JK. From perception to functional outcome in schizophrenia: modeling the role of ability and motivation. Arch Gen Psychiatry. 2012 Dec;69(12):1216–1224. doi: 10.1001/archgenpsychiatry.2012.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burns T, Patrick D. Social functioning as an outcome measure in schizophrenia studies. Acta Psychiatr Scand. 2007 Dec;116(6):403–418. doi: 10.1111/j.1600-0447.2007.01108.x. [DOI] [PubMed] [Google Scholar]
- 9.Harrow M, Sands JR, Silverstein ML, Goldberg JF. Course and outcome for schizophrenia versus other psychotic patients: a longitudinal study. Schizophr Bull. 1997;23(2):287–303. doi: 10.1093/schbul/23.2.287. [DOI] [PubMed] [Google Scholar]
- 10.Harrow M, Sands JR, Silverstein ML, Goldberg JF. Course and outcome for schizophrenia versus other psychotic patients: a longitudinal study. Schizophr Bull. 1997;23(2):287–303. doi: 10.1093/schbul/23.2.287. [DOI] [PubMed] [Google Scholar]
- 11.Robinson DG, Woerner MG, McMeniman M, Mendelowitz A, Bilder RM. Symptomatic and functional recovery from a first episode of schizophrenia or schizoaffective disorder. Am J Psychiatry. 2004 Mar;161(3):473–479. doi: 10.1176/appi.ajp.161.3.473. [DOI] [PubMed] [Google Scholar]
- 12.Wiersma D, Wanderling J, Dragomirecka E, Ganev K, Harrison G, An Der Heiden W, et al. Social disability in schizophrenia: its development and prediction over 15 years in incidence cohorts in six European centres. Psychol Med. 2000 Sep;30(5):1155–1167. doi: 10.1017/s0033291799002627. [DOI] [PubMed] [Google Scholar]
- 13.Strauss GP, Harrow M, Grossman LS, Rosen C. Periods of recovery in deficit syndrome schizophrenia: a 20-year multi-follow-up longitudinal study. Schizophr Bull. 2010 Jul;36(4):788–799. doi: 10.1093/schbul/sbn167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hafner H, Nowotny B, Loffler W, an der Heiden W, Maurer K. When and how does schizophrenia produce social deficits? Eur Arch Psychiatry Clin Neurosci. 1995;246(1):17–28. doi: 10.1007/BF02191811. [DOI] [PubMed] [Google Scholar]
- 15.Furukawa TA, Azuma H, Takeuchi H, Kitamura T, Takahashi K. 10-Year Course of Social Adjustment in Major Depression. Int J Soc Psychiatry. 2011 Sep;57(5):501–508. doi: 10.1177/0020764010371273. [DOI] [PubMed] [Google Scholar]
- 16.Judd LL, Schettler PJ, Solomon DA, Maser JD, Coryell W, Endicott J, et al. Psychosocial disability and work role function compared across the long-term course of bipolar I, bipolar II and unipolar major depressive disorders. J Affect Disord. 2008 May;108(1-2):49–58. doi: 10.1016/j.jad.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 17.Tohen M, Strakowski SM, Zarate C, Jr, Hennen J, Stoll AL, Suppes T, et al. The McLean-Harvard first-episode project: 6-month symptomatic and functional outcome in affective and nonaffective psychosis. Biol Psychiatry. 2000 Sep 15;48(6):467–476. doi: 10.1016/s0006-3223(00)00915-x. [DOI] [PubMed] [Google Scholar]
- 18.Harrow M, Grossman LS, Jobe TH, Herbener ES. Do patients with schizophrenia ever show periods of recovery? A 15-year multi-follow-up study. Schizophr Bull. 2005 Jul;31(3):723–734. doi: 10.1093/schbul/sbi026. [DOI] [PubMed] [Google Scholar]
- 19.Dickerson FB, Sommerville J, Origoni AE, Ringel NB, Parente F. Outpatients with schizophrenia and bipolar I disorder: Do they differ in their cognitive and social functioning? Psychiatry Res. 2001 May 10;102(1):21–27. doi: 10.1016/s0165-1781(01)00247-5. [DOI] [PubMed] [Google Scholar]
- 20.Green MF, Llerena K, Kern RS. The “Right Stuff” Revisited: What Have We Learned About the Determinants of Daily Functioning in Schizophrenia? Schizophr Bull. 2015 Jul;41(4):781–785. doi: 10.1093/schbul/sbv018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bromet EJ, Kotov R, Fochtmann LJ, Carlson GA, Tanenberg-Karant M, Ruggero C, et al. Diagnostic shifts during the decade following first admission for psychosis. Am J Psychiatry. 2011 Nov;168(11):1186–1194. doi: 10.1176/appi.ajp.2011.11010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kotov R, Leong SH, Mojtabai R, Erlanger AC, Fochtmann LJ, Constantino E, et al. Boundaries of schizoaffective disorder: revisiting Kraepelin. JAMA Psychiatry. 2013 Dec;70(12):1276–1286. doi: 10.1001/jamapsychiatry.2013.2350. [DOI] [PubMed] [Google Scholar]
- 23.Bebbington PNT. The Psychosis Screening Questionnaire. International Journal of Methods in Psychiatric Research. 1995;5(1):11–19. [Google Scholar]
- 24.Heinrichs DW, Hanlon TE, Carpenter WT., Jr The Quality of Life Scale: an instrument for rating the schizophrenic deficit syndrome. Schizophr Bull. 1984;10(3):388–398. doi: 10.1093/schbul/10.3.388. [DOI] [PubMed] [Google Scholar]
- 25.Cannon-Spoor HE, Potkin SG, Wyatt RJ. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull. 1982;8(3):470–484. doi: 10.1093/schbul/8.3.470. [DOI] [PubMed] [Google Scholar]
- 26.First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID), Clinician Version. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- 27.Andreasen NC. The Scale for the Assessment of Positive Symptoms. Iowa City: The University of Iowa; 1984. [Google Scholar]
- 28.Andreasen NC. The Scale for the Assessment of Negative Symptoms (SANS) Iowa City: The University of Iowa; 1983. [Google Scholar]
- 29.Blanchard JJ, Cohen AS. The structure of negative symptoms within schizophrenia: implications for assessment. Schizophr Bull. 2006 Apr;32(2):238–245. doi: 10.1093/schbul/sbj013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013. [Google Scholar]
- 31.Muthén LK, Muthén BO. Mplus user's guide. 7th. Los Angeles, CA: Author; 1998-2012. [Google Scholar]
- 32.Green MF, Horan WP, Lee J. Social cognition in schizophrenia. Nat Rev Neurosci. 2015 Oct;16(10):620–631. doi: 10.1038/nrn4005. [DOI] [PubMed] [Google Scholar]
- 33.Harvey PD, Sabbag S, Prestia D, Durand D, Twamley EW, Patterson TL. Functional milestones and clinician ratings of everyday functioning in people with schizophrenia: overlap between milestones and specificity of ratings. J Psychiatr Res. 2012 Dec;46(12):1546–1552. doi: 10.1016/j.jpsychires.2012.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jobe TH, Harrow M. Long-term outcome of patients with schizophrenia: a review. Can J Psychiatry. 2005 Dec;50(14):892–900. doi: 10.1177/070674370505001403. [DOI] [PubMed] [Google Scholar]
- 35.Bailer J, Brauer W, Rey ER. Premorbid adjustment as predictor of outcome in schizophrenia: results of a prospective study. Acta Psychiatr Scand. 1996 May;93(5):368–377. doi: 10.1111/j.1600-0447.1996.tb10662.x. [DOI] [PubMed] [Google Scholar]
- 36.Harrow M, Jobe TH. Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications: a 15-year multifollow-up study. J Nerv Ment Dis. 2007 May;195(5):406–414. doi: 10.1097/01.nmd.0000253783.32338.6e. [DOI] [PubMed] [Google Scholar]
- 37.MacQueen GM, Young LT, Joffe RT. A review of psychosocial outcome in patients with bipolar disorder. Acta Psychiatr Scand. 2001 Mar;103(3):163–170. doi: 10.1034/j.1600-0447.2001.00059.x. [DOI] [PubMed] [Google Scholar]
- 38.Yarborough BJ, Yarborough MT, Janoff SL, Green CA. Getting By, Getting Back, and Getting On: Matching Mental Health Services to Consumers' Recovery Goals. Psychiatr Rehabil J. 2015 Sep 28; doi: 10.1037/prj0000160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rietschel M, Georgi A, Schmael C, Schirmbeck F, Strohmaier J, Boesshenz KV, et al. Premorbid adjustment: a phenotype highlighting a distinction rather than an overlap between schizophrenia and bipolar disorder. Schizophr Res. 2009 May;110(1-3):33–39. doi: 10.1016/j.schres.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 40.Uzelac S, Jaeger J, Berns S, Gonzales C. Premorbid adjustment in bipolar disorder: comparison with schizophrenia. J Nerv Ment Dis. 2006 Sep;194(9):654–658. doi: 10.1097/01.nmd.0000235767.00901.e2. [DOI] [PubMed] [Google Scholar]
- 41.Cole VT, Apud JA, Weinberger DR, Dickinson D. Using latent class growth analysis to form trajectories of premorbid adjustment in schizophrenia. J Abnorm Psychol. 2012 May;121(2):388–395. doi: 10.1037/a0026922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hodgekins J, Birchwood M, Christopher R, Marshall M, Coker S, Everard L, et al. Investigating trajectories of social recovery in individuals with first-episode psychosis: a latent class growth analysis. Br J Psychiatry. 2015 Dec;207(6):536–543. doi: 10.1192/bjp.bp.114.153486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fusar-Poli P, Yung AR, McGorry P, van Os J. Lessons learned from the psychosis high-risk state: towards a general staging model of prodromal intervention. Psychol Med. 2014 Jan;44(1):17–24. doi: 10.1017/S0033291713000184. [DOI] [PubMed] [Google Scholar]
- 44.Kane JM, Schooler NR, Marcy P, Correll CU, Brunette MF, Mueser KT, et al. The RAISE Early Treatment Program for first-episode psychosis: background, rationale, and study design. J Clin Psychiatry. 2015 Mar;76(3):240–246. doi: 10.4088/JCP.14m09289. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary table. Fit indices LCGA