ABSTRACT
Tracheobronchopathia osteochondroplastica is a rare benign disease, of unknown cause, characterized by numerous sessile, cartilaginous, or bony submucosal nodules distributed throughout the anterolateral walls, projecting into the laryngotracheobronchial lumen. In general, tracheobronchopathia osteochondroplastica is diagnosed incidentally during bronchoscopy or autopsy and is not associated with a specific disease. We report the case of a male patient who was diagnosed with tracheobronchopathia osteochondroplastica via bronchoscopy and biopsy.
Keywords: Dyspnea, Tracheal diseases, Bronchoscopy
RESUMO
A traqueobroncopatia osteocondroplástica é uma doença benigna rara, de causa desconhecida, caracterizada por numerosos nódulos submucosos sésseis, cartilaginosos e/ou ósseos, distribuídos pelas paredes anterolaterais da traqueia, projetando-se no lúmen laringotraqueobrônquico. Em geral, a traqueobroncopatia osteocondroplástica é descoberta acidentalmente durante broncoscopias ou em necropsias e não é associada a uma doença específica. Relatamos o caso de um paciente que foi diagnosticado com traqueobroncopatia osteocondroplástica por broncoscopia e biópsia.
INTRODUCTION
Tracheobronchopathia osteochondroplastica (TO) is a rare benign disease, of unknown cause, characterized by numerous sessile, cartilaginous, or bony submucosal nodules distributed throughout the anterolateral walls of the trachea, projecting into the laryngotracheobronchial lumen. TO presents as round or polypoid osteocartilaginous projections covering the corrugated portion of the tracheobronchial mucosal surface and the narrow, rigid area in the respiratory tree. 1 - 3 The nodular lesions are sessile and calcified and vary from 1 to 10 mm in diameter. They are characterized by slow, progressive growth, being focal or diffuse, covered by metaplastic or normal epithelium, and extend from the perichondrium to the tracheal lumen, along the ring path, with active hematopoietic inclusion in nodular neoformations. TO can cause stenosis of the laryngotracheobronchial lumen, but without involvement of the posterior wall, with the possibility of progression to the main bronchi. 4
The first case of TO was described by Wilks, as early as in the 19th century, in a 38-year-old male patient with tuberculosis. Since then, hundreds of cases have been reported worldwide. 5 However, many patients go undiagnosed because of a lack of knowledge about TO on the part of physicians. The etiology and pathogenesis of TO remain unknown. In general, it is diagnosed incidentally during bronchoscopy or autopsy and is not associated with a specific disease. TO predominantly affects males in the fifth to seventh decade of life 1 , 2 and is usually asymptomatic. 6
In the present study, we report a case of TO found incidentally on a male patient's CT scan performed to investigate dyspnea.
CASE REPORT
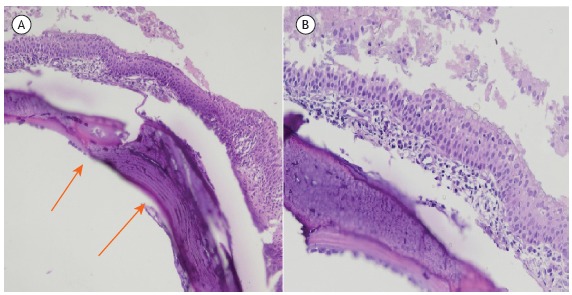
A 59-year-old male patient presented with a 1-month history of dyspnea on severe exertion, associated with a progressive cough and throat clearing. The patient had hepatitis B and chronic atrial fibrillation. He reported being a nonsmoker. His physical examination yielded normal findings. A chest X-ray revealed no significant changes. Pulmonary function testing indicated mild obstructive lung disease with a response to bronchodilator use. Echocardiography showed an ejection fraction of 49% and mild, diffuse left ventricular hypocontractility. Chest CT images are shown in Figure 1. At bronchoscopy, multiple granular lesions were seen in the trachea and bronchi (Figure 2). Biopsy revealed nodular areas consisting of ossified cartilaginous tissue in the subepithelial regions, with the underlying respiratory epithelium exhibiting a characteristic pattern and no atypia (Figure 3).
Figure 1. Chest CT scan showing multiple parietal calcifications and intraluminal nodular protrusions in the trachea and main bronchi, sparing the posterior membrane.
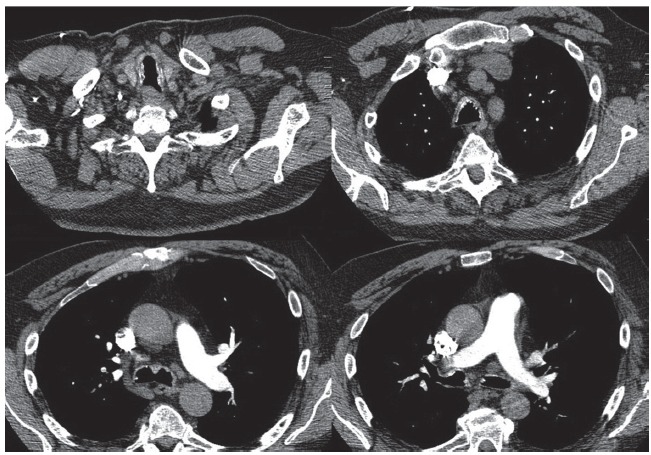
Figure 2. Bronchoscopic images showing that the tracheal caliber was preserved; the mucosa had a diffuse, coarse, granular whitish aspect, but without causing stenosis; and the main carina was thinner and mobile and had granular lesions. The ostia of the subsegmental bronchi were patent and covered by intact mucosa.
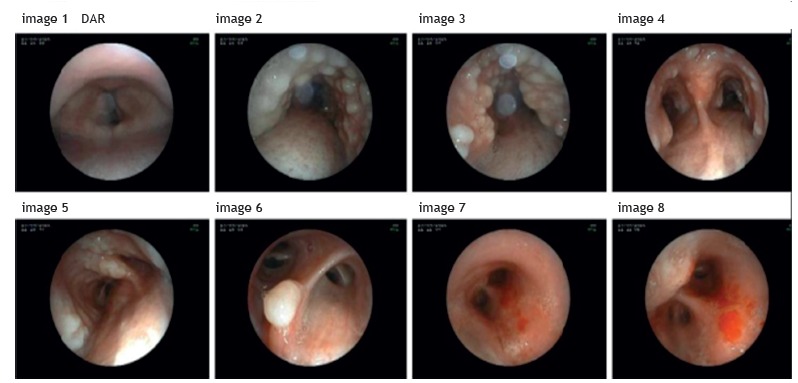
Figure 3. In A, abnormal cartilaginous tissue in the submucosal region, with metaplastic ossification (arrows; H&E; magnification, ×40). In B, same section at greater magnification showing metaplastic squamous epithelium covering the metaplastic bone tissue (H&E; magnification, ×100).
DISCUSSION
TO is a rare benign disease of unknown cause. It was described macroscopically by Rokitansk in 1855 and microscopically by Wilks in 1857. Some etiopathogenic theories have been postulated. In 1863, Virchow postulated that echondrosis and exostosis lead to calcium deposition in and ossification of the tracheal rings. In 1947, Dalgaard postulated that the elastic tissue undergoes metaplasia to form cartilage and calcium deposition. In 1910, Aschoff-Freiburg attributed TO to changes in the elastic tissue in the trachea, introducing the term tracheopathia osteoplastica; and, in 1964, Secrest et al. labeled the disease as tracheobronchopathia osteoplastica. 7
TO is usually asymptomatic. The most common symptoms are dyspnea; chronic cough; expectoration, which is often abundant; and occasionally hemoptysis. Pulmonary function testing generally does not show airflow limitation. Only a small fraction of patients have ventilation anomalies, most commonly bronchial obstruction. CT and bronchoscopy remain the gold standard for identifying TO.
The clinical incidence of TO is estimated to range from 2 to 7 cases per 1,000 population, and its onset occurs between 25 and 85 years of age, most commonly in the fifth decade of life. There is no gender predominance. The interval between the first symptoms and diagnosis is approximately 4 years in 45% of cases; however, it may be longer than 25 years. 7 Incidental findings on bronchoscopy occur at a ratio of approximately 3:2,000-5,000 population. According to Secrest et al., it is estimated that only 51% of cases will be diagnosed during the patient's lifetime. 7 No correlation has been found between TO and smoking; however, some studies indicate an association between TO and chronic tracheal inflammation, arguing that this is possibly a factor of disease progression. 8 , 9
Histologically, the mucosal bed may appear normal, with alternating areas of inflammation and necrosis and proliferative abnormal cartilage or bone formation in the submucosa, and there may be squamous metaplasia of the columnar epithelium, calcium deposits, fragments of adipocytes, and active hematopoietic bone marrow tissue. 9 , 10 There is bony tissue, which is often cartilaginous, adjacent to the cartilaginous rings. Microscopically, the benign bony-cartilaginous tissue grows and replaces the bronchial submucosa and compresses the mucous glands. Bone marrow may be present. The epithelium covering these nodules is usually intact, metaplastic, sometimes dysplastic, or ulcerated. In the case presented here, transbronchial biopsy revealed the presence of cartilaginous tissue, with foci of metaplastic ossification, in the submucosal region. Metaplastic squamous epithelium, which was intact and exhibited no atypia, covered the osteocartilaginous nodule.
The differential diagnosis of TO consists mainly of papillomatoses, sarcoidosis, chondrosarcoma, hamartomas, amyloidoses, tuberculoid calcifications, dermatomyositis, scleroderma, Wegener's granulomatosis, and paratracheal calcified lymph nodes. 11 , 12
To date, there is no definitive therapy for eradicating TO. Treatment is nonspecific; antibiotics are used to treat respiratory tract infections, and antitussives and inhaled corticosteroids are used to treat cough. Surgical treatment is indicated when the symptoms do not respond to clinical treatment; tracheal segmental resection, anterior laryngofissure, partial laryngectomy, and bronchoscopic removal of lesions can be performed. 8 Neodymium:yttrium-aluminum-garnet (Nd:YAG) laser photocoagulation, as well as placement of a silicone mold, can be a treatment option. 13 - 16
The prognosis of patients with TO is favorable. Many cases in the literature have reported little progression over the years. However, it has been demonstrated that some patients died from severe respiratory infections. 17
Footnotes
Study carried out at the Serviço de Doenças do Aparelho Respiratório, Hospital do Servidor Público Estadual de São Paulo, São Paulo (SP) Brasil.
Financial support: None.
REFERENCES
- 1.Corrin B, Nicholson AG. Corrin B, Nicholson AG. Pathology of the lungs. 2. London: Churchill Livingstone; 2006. Diseases of the airways; pp. 87–130. [Google Scholar]
- 2.Travis WD, Colby TV, Koss MN, Rosado-di-Christenson ML, Muller NL, King TE., Jr . Non-neoplastic disorders of the lower respiratory tract: Atlas of Nontumor Pathology. 1st . Washington: Armed Forces Institute of Pathology (U.S.); American Registry of Pathology; 2002. Miscellaneous diseases of uncertain etiology; pp. 857–893. [Google Scholar]
- 3.Kanat F, Teke T, Ozer F. Tracheopathia osteoplastica associated with iron deficiency anemia. Indian J Chest Dis Allied Sci. 2005;47(1):47–51. [PubMed] [Google Scholar]
- 4.Härmä RA, Suukari S. Tracheopathia condro-osteoplastica a clinical study of thirty cases. Acta Otolaryngol. 1997;84(1-2):118–123. doi: 10.3109/00016487709123949. [DOI] [PubMed] [Google Scholar]
- 5.Hussain K, Gilbert S. Tracheopathia osteochondroplastica. Clin Med Res. 2003;1(3):239–242. doi: 10.3121/cmr.1.3.239. https://doi.org/10.3121/cmr.1.3.239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Faig-Leite FS, Defaveri J. Traqueobroncopatia osteocondroplástica em portador de tumor de Klatskin. J Bras Patol Med Lab. 2008;44(6):459–462. https://doi.org/10.1590/S1676-24442008000600010 [Google Scholar]
- 7.Jabbardarjani HR, Radpey B, Kharabian S, Masjedi MR. Tracheobronchopathia osteochondroplastica presentation of ten cases and review of the literature. Lung. 2008;186(5):293–297. doi: 10.1007/s00408-008-9088-4. https://doi.org/10.1007/s00408-008-9088-4 [DOI] [PubMed] [Google Scholar]
- 8.Willms H, Wiechmann V, Sack U, Gillissen A. Tracheobronchopathia osteochondroplastica A rare cause of chronic cough with haemoptysis. Cough. 2008;4:4–4. doi: 10.1186/1745-9974-4-4. https://doi.org/10.1186/1745-9974-4-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Doshi H, Thankachen R, Philip MA, Kurien S, Shukla V, Korula RJ. Tracheobronchopathia osteochondroplastica presenting as an isolated nodule in the right upper lobe bronchus with upper lobe collapse. J Thorac Cardiovasc Surg. 2005;130(3):901–902. doi: 10.1016/j.jtcvs.2005.01.020. https://doi.org/10.1016/j.jtcvs.2005.01.020 [DOI] [PubMed] [Google Scholar]
- 10.Pinto JA, Silva LC, Perfeito DJ, Soares Jdos S. Osteochondroplastic tracheobronchopathy report on 02 cases and bibliographic review. Braz J Otorhinolaryngol. 2010;76(6):789–793. doi: 10.1590/S1808-86942010000600019. https://doi.org/10.1590/S1808-86942010000600019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chroneou A, Zias N, Gonzalez AV, Beamis JF., Jr Tracheobronchopathia Osteochondroplastica An underrecognized entity? Monaldi Arch Chest Dis. 2008;69(2):65–69. doi: 10.4081/monaldi.2008.398. [DOI] [PubMed] [Google Scholar]
- 12.Marom EM, Goodman PC, McAdams HP. Diffuse abnormalities of the trachea and main bronchi. AJR Am J Roentgenol. 2001;176(3):713–717. doi: 10.2214/ajr.176.3.1760713. https://doi.org/10.2214/ajr.176.3.1760713 [DOI] [PubMed] [Google Scholar]
- 13.Tadjeddein A, Khorgami Z, Akhlaghi H. Tracheobronchopathia osteoplastica cause of difficult tracheal intubation. Ann Thorac Surg. 2006;81(4):1480–1482. doi: 10.1016/j.athoracsur.2005.04.013. https://doi.org/10.1016/j.athoracsur.2005.04.013 [DOI] [PubMed] [Google Scholar]
- 14.Lazor R, Cordier JF. Tracheobronchopathia osteochondroplastica. Orphanet Encyclopedia; 2002. 4p. https://www.orpha.net/data/patho/GB/uk-TO.pdf [Google Scholar]
- 15.Dutau H, Musani AI. Treatment of severe tracheobronchopathia osteochondroplastica. J Bronchol. 2004;11(3):182–185. https://doi.org/10.1097/01.lab.0000131026.05007.34 [Google Scholar]
- 16.Abu-Hijleh M, Lee D, Braman SS. Tracheobronchopathia osteochondroplastica a rare large airway disorder. Lung. 2008;186(6):353–359. doi: 10.1007/s00408-008-9113-7. https://doi.org/10.1007/s00408-008-9113-7 [DOI] [PubMed] [Google Scholar]
- 17.Leske V, Lazor R, Coetmeur D, Crestani B, Chatté G, Cordier JF. Tracheobronchopathia osteochondroplastica a study of 41 patients. Medicine (Baltimore) 2001;80(6):378–390. doi: 10.1097/00005792-200111000-00004. https://doi.org/10.1097/00005792-200111000-00004 [DOI] [PubMed] [Google Scholar]


