Abstract
Objective
To assess the outcomes of a clinical decision support (CDS) intervention designed for home care patients with high medication regimen complexity (MRC) and to examine the correlates of CDS use and its relationship to patient outcomes.
Method
The intervention randomized nurses upon identification of an eligible patient. The CDS consisted of a computerized algorithm that identified high MRC patients, electronic clinician alerts, and a care management module. Analyses were completed on full intention to treat and intervention group-only samples. Regression-adjusted outcomes were hospitalization, emergency department use and reduction in MRC. Data sources included health records and administrative data.
Results
Five hundred nurses were randomized with 7,919 of their patients. Approximately 20% of the intervention group was hospitalized versus 21% in the control group; 16.5% of the intervention group had an emergency department visit versus 16.7% in the control group; and 6% in each group dropped below the high MRC threshold. No statistically significant differences were found in the intention to treat analysis. Eighty-two percent of intervention nurses used the CDS but for only 42% of their patients. Among intervention patients, CDS use (versus non-use) was associated with reduced MRC and hospitalization. CDS use was more likely among older nurses, those with higher study-patient caseload and, marginally, among salaried nurses and those with longer tenure. Significant patient characteristics were clinical conditions, payer, episode length, care continuity and race.
Conclusion
CDS use was limited, thus negating the impact of the intervention overall. The findings on correlates of CDS use and the relationship between CDS use and positive outcomes suggest that CDS use and outcomes could be enhanced by avoiding very short patient lengths of stay, improving continuity of care, increasing reliance on salaried nurses and/or increasing per diem nurses’ incentives to use CDS.
Keywords: clinical decision support, medication regimen complexity, MRCI, home health care, nurses, hospitalization risk
INTRODUCTION
Home health organizations provide post-acute care to a predominantly Medicare population characterized by multiple chronic conditions. The number and varied types of drugs and the complexity of medication regimens found among home health patients pose significant management challenges for both nurses and patients. Although attention has been paid to improving management of home health patients with designated “high risk” medications such as sliding scale insulin and benzodiazepines[1–3], proven strategies to address the problem of high medication regimen complexity (MRC) in the home health setting have been lacking. Our study addressed this information gap by mounting a randomized controlled trial (RCT) to examine outcomes of a multi-faceted clinical decision support (CDS) intervention designed for use in home health care. The primary objective was to assess the impact of the CDS on hospitalization, emergency department (ED) use, and change in MRC amount high MRC home health patients. The secondary objectives were to examine the correlates of CDS use and its relationship to patient outcomes.
In hospital and pharmacy settings, IT has proved successful in improving medication management – e.g., reconciling medications, avoiding contraindicated medications and monitoring dose administration[4,5]. Clinical alerts are often complemented by CDS tools providing clinicians with information about management choices. These interventions have focused primarily on medication prescribing and dispensing processes, with their main objective being patient safety improvement[6,7]. There is little information, to date, about how IT can help identify patients who, due to high MRC, may be at potential risk for poor medication management leading to poor outcomes.
Multiple studies have identified high MRC as one of the root causes of medication mismanagement, non-adherence and/or adverse outcomes[8–11]. Medication mismanagement can include taking medications at the wrong time of day, with incorrect fluid/food intake, in the wrong dosage, improperly storing medications, or running out of needed medications[12]. Higher numbers of medications and complicated schedules or special instructions (e.g., time of day, food interactions) can all contribute to greater patient difficulty in following treatment recommendations. Simplifying complex medication regimens and/or paying greater attention to managing complexity are potentially remedial interventions. Muir and colleagues[13] demonstrated a successful intervention that provided physicians of hospitalized patients with a visual grid depicting a patient’s 7 day regimen. Intervention patients were discharged with fewer medication and fewer doses per day. In another hospital-based study, an educational intervention targeting clinical pharmacists and junior medical officers along with a pharmacist medication review produced a lower increase in MRC[14]. Outside of these very few studies have touched on remedial strategies.
Given the age (69% aged 65 years or over) and clinical complexity of home health patients (average of 4.2 diagnoses at home care admission; majority taking 5 or more medications)[15–17], automated, evidence-based medication management tools offer great potential benefit. Moreover, a significant number of home health organizations have begun to adopt “point of service” technology[18]. Yet aside from the growing use of automated drug utilization review systems to assist with medication reconciliation, proven IT strategies to support other key aspects of medication management have not been systematically adopted.
METHODS AND MATERIALS
Study Design
Our intervention deployed an innovative, multifaceted CDS strategy to systematically, proactively assist nurses in identifying high MRC in their assigned patients, assessing patient adherence and supporting their patients through teaching and direct intervention. The CDS included an automated algorithm to identify patients with high MRC, an automated alert notifying the home health nurse of the patient’s high MRC status, and an electronic care management module embedded in the organization’s electronic health record (EHR) designed specifically for use with high MRC patients. Our primary aim was to assess the impact of the CDS on home health patients’ hospitalization, ED use, and change in MRC. Secondary aims were to explore correlates of CDS use and its impact on complexity reduction and patient outcomes.
The study employed a clustered, randomized design to assess the effectiveness of the CDS intervention compared to usual care in a large, urban, non-profit home health care organization. The organization’s institutional review board approved the study protocol and a HIPAA Waiver of Authorization (reference #I08-003) allowing the abstraction of patient-level data. Upon identification of an eligible patient, nurses were randomly assigned using an automated block randomization schema to either control (usual care) or intervention using a 2:1 allocation ratio of control to intervention. Randomization occurred at the patient’s admission to home health care. A nurse’s initial random assignment determined the nurse’s status for all eligible patients allocated to that particular nurse’s care for the study’s duration.
Description of Usual Care
All field nurses at the study organization are equipped with pen-based tablet computers that run a secure EHR called the Patient Care Record System (PCRS). Information on new referrals and continuing patients is regularly uploaded onto the tablet. Multiple components within the PCRS inform the nurse’s work in the field. The critical units are 1) Plan of Care, 2) Visit, and 3) Medications. The Plan of Care (which constitutes the federally required CMS Form 485) contains the physician’s orders and informs the other units of what treatment should be delivered. The Visit unit, where the nurse documents the patient encounter, consists of two sections: (i) the Clinical Assessment, which includes the federally mandated Outcomes Assessment Information Set (OASIS)[19], and (ii) a set of Patient Care Plan Problems, where care goals, interventions and progress are recorded for each visit. The Medications unit consists of (i) an electronic medications database provided by a commercial source (First DataBank); (ii) drug utilization review (DUR) algorithms (also provided and updated by First DataBank) that identify all potential drug-drug interactions (DDI) and duplicative medications; and (iii) an alert system that flags DDI severity and duplicative therapy. For each patient, the PCRS “pushes” a list of the patient’s Care Plan Problems derived from the physician orders, the Clinical Assessment and the patient’s medications. Nurse then uses their clinical judgment to decide what issues to communicate to the patient’s physician, which problems to “pull down” from the PCRS and in what order. Before and/or during each patient visit, the nurse reviews the patient’s Plan of Care, reviews and updates the patient’s current medications and enters the Visit unit to document progress on the patient Care Plan Problems the nurse has selected to work on.
The Intervention
The CDS intervention consisted of three computer-automated components: (i) an algorithm that identified patients with high MRC and thus at increased potential for a serious medication problem or adverse outcome[20]; (ii) a clinical alert – an email delivered to the nurse’s tablet identifying a specific patient with high MRC and directing the nurse to the “medication regimen complexity care management module”; (iii) a high MRC care management module integrated into the Visit unit of the PCRS with specific recommendations for nursing goals and interventions appropriate to patients with multiple co-morbidities and high MRC. The CDS components included features found to be independent predictors of improved clinical practice, most notably: 1) computer-generated; 2) provided as part of clinician workflow; 3) offering recommendations rather than just assessments, and 4) delivered at the time and location of decision making [21].
Computerized Risk Algorithm
The study team worked with the organization’s IT department to automate the Medication Regimen Complexity Index (MRCI)[22] into the IT system to identify patients with high MRC. The MRCI was calculated based on medication data entered into the PCRS by field nurses as part of usual care. The automation process and MRCI are described elsewhere[20]. The MRCI has been validated and proposed as a tool to identify patients in need of intervention[23]. A binary variable (MRCI score of 24.5 or above versus below 24.5) was used to identify the target population with high MRC. The cutoff corresponded to the MRCI score highest quintile and was found, through prior internal analysis of 2008 data, to be associated with the highest emergency room and hospitalization use post-home care admission (VNSNY Center for Home Care Policy and Research, 2009, unpublished).
Electronic Clinical Alert
Once the computerized MRCI identified a patient, nurses in the intervention group received an email alert identifying the patient as someone at greater potential for medication problems due to high MRC. The initial alert was sent in the patient’s first week of care. A follow-up alert was sent four days later. Both alerts directed the nurse to the MRC care management module in the PCRS.
Electronic MRC Care Management Module
A multi-disciplinary committee of study team members, representatives from Quality Management and IT developed the MRC care management module. The module’s components, like other PCRS care plan problems, consisted of: (i) assessment, (ii) provision, (iii) teaching, (iv) management, (v) support, and (vi) evaluation recommendations. These recommendations focused on nurses’ comprehensive assessment of medication adherence and barriers, medication reconciliation, regimen simplification, and self-management guidance in the high MRC patient. The MRC care management module is not patient or medication specific but rather provides different strategies that can be used to help a patient who may be having trouble managing a high complexity regimen. For example, the module prompts the nurse to think about collaborating with the prescribing provider to: reduce the number of medications, increase use of combination pills, reduce the number of dosages a day or synchronize the times of day medications need to be taken, strategies referenced in the literature on medication simplification[9,13,24]. The module also prompts the nurse to think about potential strategies to improve patient self-management including: consolidating and synchronizing refills with one pharmacy, use of pill boxes and medication alert systems, and maintaining an accurate list of all prescribed and over the counter medications to be shared with provider on each visit.
Data Sources
Data were drawn from four sources: 1) the Outcomes Assessment and Information Set (OASIS); 2) the organization’s medications database; 3) the PCRS database; and 4) administrative and service use data routinely collected by the organization’s billing and human resources (HR) departments.
Outcome Measures
Medication Regimen Complexity Index (MRCI)
MRCI scores were calculated at home care admission and at 60 days post-home care admission or home care discharge, whichever was earlier. The 60 day timeframe was selected because Medicare, the predominant payer for home health, compiles publically reported hospitalization outcomes for 60 day episodes of home health care. The outcome variable was the percentage of patients whose MRCI score was below the established risk threshold of 24.5 at the follow-up assessment point.
Hospitalizations and Emergency Department (ED) Visits
These measures were derived from patients’ post-home care admission OASIS assessments, which include assessments when a patient is transferred out of home care (usually admitted to the hospital for temporary reasons), resumes home care, or is discharged from home care. We collected hospitalization and ED visit data from these follow-up assessments up to discharge or 60 days post-home care admission, whichever was earlier (the standard home care hospitalization metric mandated by CMS). All cause hospitalization was used because the reason for hospitalization is often listed as unknown in the home care record and it is hard to distinguish from the data source whether an admission for a disease exacerbation was from disease progression, suboptimal treatment or potentially medication non-adherence.
Independent Variables
Data on Nurse Characteristics and Care Management Practices
Data on nurses’ gender, age, level of education (e.g., licensed, bachelor’s or master’s level RN), job tenure, and employment status (staff versus per diem) were derived from the HR database. Service use data (specifically, nurse-level information on dates and numbers of visits) from the utilization tables the organization maintains to capture visit information of different home care professionals to each of their patients were used to construct patient caseload variables for each nurse each time he/she had an eligible patient.
Two of the three CDS components – calculation of the MRCI score and the alert to the nurse about a high MRC patient – were fully automated and therefore their use was 100%. However, use of the MRC care management module by intervention nurses was fully discretionary on their part. CDS use for the study, therefore, was equated with use of the care management module and was determined from data collected from the PCRS database. Use was captured at the patient-specific encounter level, making it possible to construct and aggregate measures per visit, per home health episode, per patient and per nurse.
Data on Patient Characteristics
Data on patients’ clinical and functional status, patient demographics, living arrangements and informal supports were obtained from OASIS. Data included: co-morbidities and symptom severity, risk factors, prognosis, therapies, pain status, wounds, neurological/cognitive/behavioral status, activities of daily living (ADLs) and instrumental activities of daily living (IADLs). These data, collected at start of care as part of usual care, were used to adjust for any potential baseline differences in patient severity between patients served by intervention and control group nurses.
Data Analysis
A priori power calculations indicated that, for the anticipated number of nurses, average number of patients treated by each individual nurse, and assumed intra-cluster correlation, the study would enable us to detect a 4 percentage point difference in hospitalization with 80% statistical power. When conducting our intention to treat (ITT) analyses of primary outcomes, we first identified nurse and patient characteristics that differed between the two study groups using chi-square or t-tests where appropriate. Characteristics that were significantly different at a p<0.20 level were subsequently included in multivariate models. We modeled the effect of the study intervention on the 3 patient outcomes using 3 separate Generalized Estimating Equations (GEE) models to adjust for clustering at the nurse level, and adjusted for nurse and patient characteristics that differed significantly across study groups.
Secondary analyses focusing on intervention group nurses were conducted to examine factors associated with CDS use and its association with intervention patient outcomes. Nurses were classified as CDS-users if they documented at least one use, for one patient, in the provision, teaching or management section of the MRC care management module. Data were tabulated on how many nurses used the module at least once, the percentage of patients whose record indicated their nurse used the module, and the number of actions taken per patient. We relied on bivariate analysis to explore nurse and patients characteristics associated with CDS use. Characteristics significantly different at a p<0.20 level were then included in multivariate GEE models.
Because intervention nurses could choose whether to use the CDS or not, we used propensity scores, defined as the conditional probabilities of using CDS given patients’ and nurses’ characteristics, to reduce potential bias by balancing these characteristics in the use/non-use groups through regression adjustment. We included the propensity scores as covariates when estimating the relationship between CDS use and the outcomes of interest within the intervention group.
RESULTS
Sample Characteristics
Figure 1 provides a depiction of the study flow and Table 1a reports the characteristics of the 500 nurses, serving 7,919 eligible patients, who were randomized to usual care and intervention groups. Usual care nurses were more likely to be female (p=0.04), slightly older (p=0.10), and had longer job tenure (p=.10) than intervention group nurses, although differences were generally not statistically significant at conventional levels.
Figure 1.
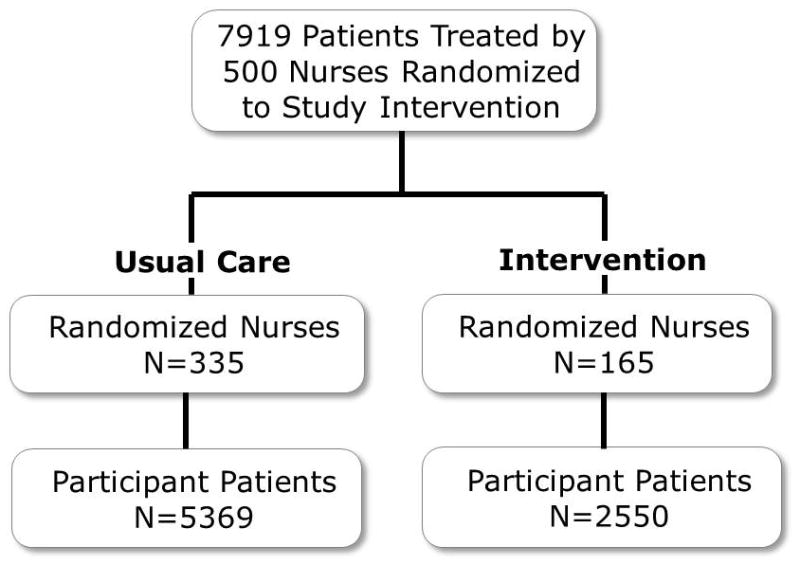
Nurse/Patient Flow Diagram
Note: All patients who were identified as having a complex medication regimen were randomized along with their nurses; no exclusion criteria were applied. Intervention components were automated so all nurses in the intervention group received the alert and access to the CDS for each of their eligible patients – so there were no intervention drops.
Table 1a.
Basic Characteristics of the Full Intention to Treat Nurse Population (N=500)
| Usual Care (n=335) | Intervention (n=165) | p-value | |
|---|---|---|---|
| Female (%) | 90% | 83% | 0.04 |
| Mean age in years (SD) | 46.3 (10.6) | 44.7 (9.8) | 0.10 |
| Race/Ethnicity (%) | 0.17 | ||
| Black, non-Hispanic | 41% | 33% | |
| Hispanic | 9% | 14% | |
| White, non-Hispanic | 29% | 33% | |
| Other or unknown | 20% | 20% | |
| Per Diem – paid per patient visit (%) | 35% | 40% | 0.27 |
| Mean Years of Employment (SD) | 10.8 (7.8) | 9.6 (7.5) | 0.10 |
| Educational Level (%) | 0.60 | ||
| Diploma | 10% | 8% | |
| Associate | 26% | 32% | |
| Bachelor | 55% | 51% | |
| Advanced degree | 6% | 5% | |
| Missing | 3% | 4% | |
| Number of Eligible Patients (%) | 0.53 | ||
| Only one | 5% | 2% | |
| Only two | 1% | 2% | |
| Only three | 3% | 4% | |
| Four or more | 91% | 92% |
Table 1b shows selected sociodemographic and baseline health characteristics of the 7,919 patients included in the ITT analysis. The majority of patients were female and 65 years of age or older. Patients in the usual care arm were slightly younger (p<0.001), more likely to be Black, non-Hispanic (p<0.001), have worse health status at baseline (p=0.01), and more likely to be covered by Medicaid than patients in the intervention arm (p=0.001).
Table 1b.
Key Sociodemographic and Baseline Health Characteristics of Full Intention to Treat Patient Sample(N=7919)
| Usual Care (n=5369) | Intervention (n=2550) | p-value | |
|---|---|---|---|
| Sociodemographic Characteristics | |||
| Female (%) | 61% | 61% | 0.92 |
| Age | |||
| Mean age in years (SD) | 67.1 (14.4) | 68.4 (14.1) | <0.001 |
| 65+(%) | 59% | 63% | <0.001 |
| Race/Ethnicity (%) | <0.001 | ||
| Black, non-Hispanic | 31% | 24% | |
| Hispanic | 30% | 30% | |
| White, non-Hispanic | 33% | 40% | |
| Other or unknown | 6% | 6% | |
| Medicaid enrollee (%) | 36% | 33% | 0.001 |
| Lives alone (%) | 44% | 46% | 0.14 |
| Baseline Health Status | |||
| Chronic Condition Co-morbidity Score, Mean (SD)a | 2.8 (1.2) | 2.7 (1.2) | 0.01 |
| ADL/IADL Score, Mean (SD)a | 3.0 (1.9) | 3.1 (1.9) | 0.03 |
| Baseline Medication Profile | |||
| No. of Medications, Mean (SD) | 12.8 (3.2) | 12.9 (3.2) | 0.59 |
Scores and ratings were based on standardized start of care assessment data completed by a home care nurse blinded to study group. Higher values indicate greater disability. The Chronic Condition Score was based on the tabulation of up to 18 conditions.
SD = standard deviation; ADL/IADL = activities of daily living/instrumental activities of daily living
As shown in Figure 2, about 6% of the patients from each randomized group had dropped below the MRCI threshold that designated high MRC, nearly 17% had an ED visit and approximately one out of five had been hospitalized by the 60-day (or home-care discharge) follow-up point. No statistically significant differences were found between the randomized groups for any of these outcomes.
Figure 2.
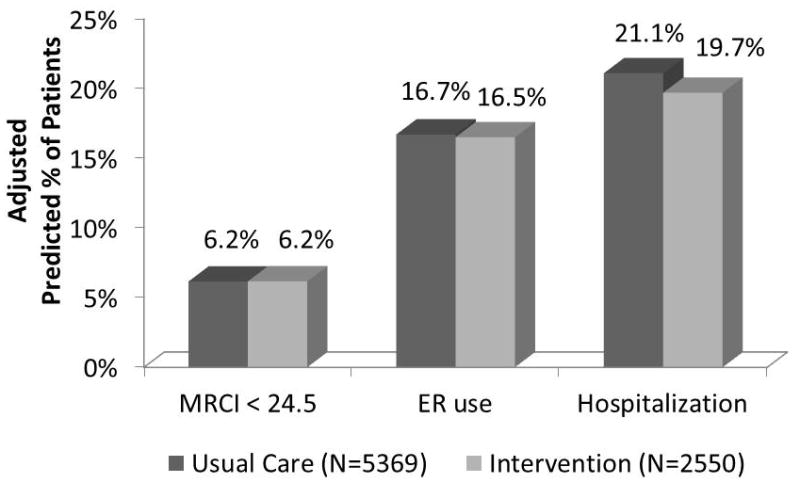
Patient Outcomes by Study Group – Full Intention to Treat sample
Note: Patient and nurse characteristics that were significantly different at a p<0.20 level were included in multivariate models. Analysis is adjusted for clustering at the nurse level.
Findings from Intervention Group Analyses
As documented in Table 2, 82% of the 165 intervention nurses documented an action within the MRC care management module with at least one of their targeted patients. However, only 42% of the 2,550 patients had an intervention nurse action documented in their record; on average CDS-use nurses documented 7.2 (SD= 2.8) actions per patient (range: 1–13).
Table 2.
Intervention Nurse Use of Electronic Clinical Decision Support Tool
| % of nurses who documented a CDS-recommended action with at least one of their patients in target population (N=165) | % of patient records in the intervention group with documented action (N=2550) | |
|---|---|---|
| Indicator that nurse took at least one action from decision support tool | 82% | 42% |
| Mean number of actions per patient when used at least once (SD); possible range = 1–13 | 7.2 (2.8) | |
| Provision | ||
| Provided medication list | 58% | 15% |
| Provided pre-pour box | 50% | 11% |
| Teaching | ||
| Importance of adherence to the medication regimen | 78% | 33% |
| To keep the medication list up to date | 79% | 39% |
| To bring the medication list to each physician visit | 81% | 39% |
| To develop system or plan to obtain medication refills on time | 69% | 31% |
| To remove/discard old and/or expired medications | 75% | 33% |
| To contact physician with any immediate concerns about medications or side effects | 74% | 31% |
| To work with pharmacist to synchronize refills | 60% | 22% |
| To use one pharmacy if possible | 72% | 30% |
| To discuss medication simplification with physician | 48% | 11% |
| Strategies to help with medication adherence | 64% | 24% |
| Management | ||
| Contacted physician to discuss medication simplification | 13% | 2% |
CDS = clinical decision support; SD = standard deviation
Table 3 describes the characteristics of nurses in the use and non-use groups. Nurses who were older (p=0.03) and served a higher number of patients in the study (p=0.003) were more likely to use CDS. Borderline significant findings found that nurses with shorter job tenure and “per diem” nurses (i.e. those who were paid per visit) were less likely than staff (salaried) nurses to use the CDS.
Table 3.
Intervention Nurse CharacteristicsRelated to CDS Use (N=165)
| No CDS use (n=29) | CDS Use (n=136) | p-Value | |
|---|---|---|---|
| Female (%) | 76% | 85% | 0.26 |
| Mean age in years (SD) | 41 (8) | 45 (10) | 0.03 |
| Race/Ethnicity (%) | 0.38 | ||
| Black, non-Hispanic | 28% | 34% | |
| Hispanic | 21% | 13% | |
| White, non-Hispanic | 24% | 34% | |
| Other or unknown | 27% | 19% | |
| Per Diem – paid per patient visit (%) | 55% | 37% | 0.07 |
| Mean Years of Employment (SD) | 8.0 (5) | 9.9 (8) | 0.08 |
| Educational Level (%) | 0.62 | ||
| Diploma | 10% | 7% | |
| Associate | 38% | 31% | |
| Bachelor | 48% | 51% | |
| Advanced degree | 0% | 7% | |
| Missing | 4% | 4% | |
| Borough (%) | 0.55 | ||
| Bronx | 17% | 21% | |
| Brooklyn | 10% | 20% | |
| Manhattan | 38% | 32% | |
| Queens | 35% | 27% | |
| Mean Number of Patients in study (SD) | 14 (8) | 19 (9) | 0.003 |
| Mean Caseload (cases) (SD) | 20 (7) | 21 (8) | 0.37 |
| Mean Caseload (visits) (SD) | 51 (25) | 58 (27) | 0.18 |
CDS = clinical decision support; SD = standard deviation
Factors associated with CDS use among intervention nurses
Table 4 presents the results for the multivariate models used to examine factors associated with use of the CDS among intervention nurses. Patient clinical characteristics associated with higher probability of use were a cardiac condition (p=0.01), stroke diagnosis (p=0.01) and shortness of breath at admission (p=0.01). A higher number of chronic conditions (p=0.01) and a cancer diagnosis (p=0.06), on the other hand, were associated with lower CDS use. The CDS also was less likely to be used if the patient was African-American (p=0.01), Medicaid beneficiary or privately insured (relative to Medicare beneficiaries, p=0.01), or if the patient’s Coordinator of Care (main nurse) had changed during the study period (p<0.01).
Table 4.
Patient LevelPredictors of CDS Use, Multivariate Models (N=2550)
| OR* (95% CI) | p-value | OR** (95% CI) | p-value | |
|---|---|---|---|---|
|
| ||||
| Age | 0.99 (0.98, 1.003) | 0.20 | 1.00 (0.99, 1.004) | 0.30 |
|
| ||||
| Female gender | 1.06 (0.88, 1.28) | 0.51 | 1.07 (0.91, 1.27) | 0.40 |
|
| ||||
| Race (vs. White) | ||||
| Black, non-Hispanic | 0.53 (0.40, 0.69) | <0.001 | 0.65 (0.49, 0.88) | 0.01 |
| Hispanic | 1.00 (0.72, 1.39) | 0.98 | 0.99 (0.70, 1.33) | 0.84 |
| Other | 1.31 (0.85, 2.04) | 0.21 | 1.24 (0.80, 1.91) | 0.34 |
|
| ||||
| Payer (vs. Medicare only) | ||||
| Private | 0.69 (0.50, 0.94) | 0.01 | 0.68 (0.53, 0.87) | 0.003 |
| Dually Eligible | 1.02 (0.76, 1.36) | 0.91 | 1.00 (0.79, 1.29) | 0.97 |
| Medicaid only | 0.66 (0.51, 0.87) | 0.003 | 0.73 (0.57, 0.92) | 0.01 |
| Other | 0.52 (0.28, 0.96) | 0.04 | 0.65 (0.37, 1.14) | 0.13 |
|
| ||||
| Language (vs. English-blank) | ||||
| Spanish | 0.95 (0.69, 1.31) | 0.76 | 0.88 (0.66, 1.18) | 0.39 |
| Other | 1.25 (0.84, 1.87) | 0.27 | 0.88 (0.61, 1.28) | 0.51 |
|
| ||||
| Number of medications | 1.02 (0.99, 1.05) | 0.20 | 1.02 (1.00, 1.05) | 0.06 |
|
| ||||
| Discharged from acute hospital within 14 days of home care admission? | 1.06 (0.87, 1.29) | 0.54 | 1.11 (0.94, 1.31) | 0.21 |
|
| ||||
| Discharged from inpatient rehabilitation hospital or unit within 14 days of home care admission? | 1.23 (0.92, 1.63) | 0.16 | 1.24 (0.96, 1.60) | 0.10 |
|
| ||||
| AIDS | 0.76 (0.26, 2.20) | 0.61 | 0.97 (0.43, 2.20) | 0.95 |
|
| ||||
| Cancer | 0.77 (0.55, 1.08) | 0.13 | 0.78 (0.59, 1.01) | 0.06 |
|
| ||||
| Hypertension | 1.21 (0.96, 1.52) | 0.11 | 1.22 (0.95, 1.56) | 0.12 |
|
| ||||
| Cardiac Condition | 1.48 (1.10, 1.98) | 0.01 | 1.43 (1.10, 1.86) | 0.01 |
|
| ||||
| Stroke | 1.53 (1.07, 2.19) | 0.02 | 1.49 (1.08, 2.05) | 0.01 |
|
| ||||
| History of falls (2 or more falls - or any fall with an injury - in the past year | 1.11 (0.86, 1.44) | 0.40 | 1.03 (0.81, 1.30) | 0.83 |
|
| ||||
| The patient is stable with no heightened risk(s) for serious complications and death (beyond those typical of the patient’s age). | 0.89 (0.67, 1.20) | 0.46 | 1.09 (0.83, 1.44) | 0.55 |
|
| ||||
| The patient is temporarily facing high health risk(s) but is likely to return to being stable without heightened risk(s) for serious complications and death (beyond those typical of the patient’s age) - OR patient’s situation is unknown or unclear | 1.04 (0.82, 1.32) | 0.74 | 1.08 (0.89, 1.30) | 0.44 |
|
| ||||
| Cognitive function | 1.06 (0.83, 1.34) | 0.66 | 1.00 (0.84, 1.19) | 0.99 |
|
| ||||
| Ever short of breath | 1.23 (1.02, 1.47) | 0.03 | 1.22 (1.04, 1.42) | 0.01 |
|
| ||||
| Human assistance needed with oral medications | 1.11 (0.90, 1.36) | 0.32 | 0.96 (0.82, 1.13) | 0.65 |
|
| ||||
| Number of nurse visits | 1.03 (1.01, 1.04) | <0.001 | 1.01 (1.003, 1.02) | 0.01 |
|
| ||||
| Index COC changed | 0.66 (0.53, 0.82) | <0.001 | 0.71 (0.56, 0.90) | 0.004 |
|
| ||||
| Sum of Chronic Conditions | 0.91 (0.83, 0.99) | 0.03 | 0.92 (0.86, 0.98) | 0.01 |
|
| ||||
| Sum of ADL/IADL dependencies | 0.94 (0.89, 0.99) | 0.04 | 0.97 (0.93. 1.02) | 0.22 |
|
| ||||
| Length of stay | 1.02 (1.01, 1.03) | <0.001 | 1.03 (1.02, 1.03) | <0.001 |
Not adjusted for nurse clustering
Adjusted for nurse clustering at the Coordinator of Care level
CDS = clinical decision support; OR = odds ratio; CI = Confidence Interval; COC = Nurse coordinator of care (nurse in charge of case); ADL/IADL = activities of daily living/instrumental activities of daily living
Patient Outcomes by CDS Group Use – Intervention Group Only
Figure 3 shows the regression-adjusted predicted probabilities (in percentages) based on GEE models for each of the three outcomes that controlled for patient and nurses characteristics as well as propensity scores. Patients whose nurse used CDS for their cases had significantly better outcomes. A little over 8% of patients moved below the high MRC threshold when CDS was used relative to 4.5% of patients when CDS was not used (p<0.01). Similarly, the hospitalization rate was17.9% when CDS was used relative to 21.3% when CDS was not used (p<0.01).
Figure 3.
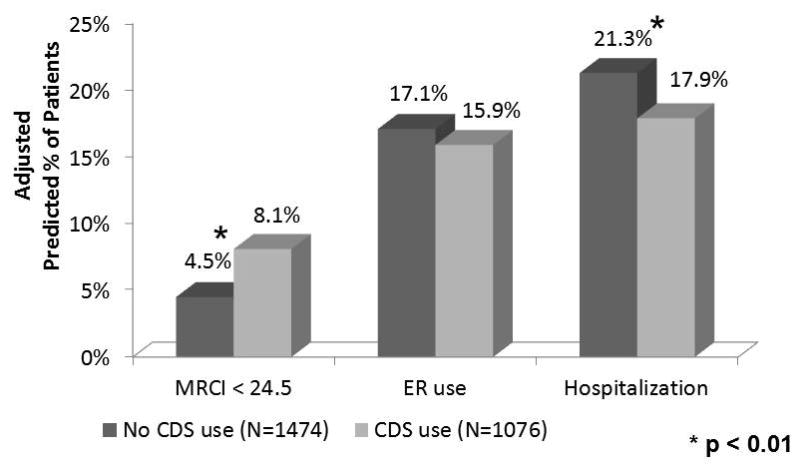
Patient Outcomes by CDS Group
Note: Patient and nurse characteristics that were significantly different at a p<0.20 level were included in multivariate models. Analysis is adjusted for clustering at the nurse level.
DISCUSSION
This study describes the results of a CDS intervention designed to provide patient level alerts and care management decision support to nurses caring for an especially challenging population of chronically ill older adults receiving health services at home – patients with high MRC. The CDS combined two features – automated identification of high risk patients and email clinical alerts – previously demonstrated to improve home care nurses’ use of evidence-based heart failure practices and related patient outcomes[25,26]. The CDS also incorporated additional features found to be significant independent predictors of improved clinical practice: integration into the clinician’s workflow, delivery at the point of decision making and care management recommendations not just assessments[21].
Despite automation, integration, timeliness and evidence-based content, our intention to treat analysis found no significant intervention impact on patients’ MRC, ED visits or hospitalizations. Yet our intervention group-only analysis, using propensity scoring to minimize use/non-use bias, found reduced MRC and less hospitalization among patients whose nurses documented that they had addressed medication regimen complexity with them. What might explain these perplexing findings? A possible reason for significant benefits of CDS use within the intervention group may be the relatively robust use of the care management module for the patients whose nurses used it for them. Nurse users of the MRC care management module documented on average 7.2 of 13 possible actions for each patient for whom they used the module. However, this use extended to fewer than half (42%) of patients served by nurses in the intervention group. Thus a possible, even likely, reason for the negligible impact of the intervention overall may be that it failed to reach nearly 6 in 10 patients whose nurses potentially could have used the MRC care management module once they received the alert indicating their patient’s high MRC status.
By design, and in accord with other care plan modules in the organization’s PCRS, the nurse had complete discretion over whether to use the MRC care management module for a specific patient once that patient’s alert was received. The nurse also had discretion to decide which of the many care management actions available in the module to select. A better understanding of nurses’ professional decision making regarding when and for whom to use CDS is therefore critical to improve its uptake.
Analysis of the number and type of care management actions chosen by intervention group nurses provides some insights into their decision making. The most frequently documented care management actions were advising patients to keep their medication list up-to-date and advising patients to bring the complete list of medications to their doctors’ appointments. Taken together, these two actions may have stimulated physicians to focus on medication regimen complexity issues that might otherwise have gone unnoticed. In fewer cases the nurse documented advising the patient to speak with the doctor about simplifying their medication regimen, and in only a small number of cases the nurse documented asking the doctor directly to work on simplification. These differences may reflect the nurse’s level of (dis)comfort with selected care management practices. Simplifying medications requires consideration of use of combination tablets, sustained-release formulas, and/or reducing the number of different times during the day a patient needs to take their medication The nurse may want to determine what could be simplified before contacting the physician or before advising the patient to speak to the doctor. Nurses lacking this knowledge or confidence may have been hesitant to take these actions.
Little is known about the relationship between clinician characteristics and CDS use, although one study of physicians found that older and more experienced physicians were more likely to use novel EHR functionality[27]. Our bivariate associations suggest a similar pattern whereby nurses who were older, had longer job tenure or who worked in salaried staff positions (as opposed to per diem nurses), were more likely to use the CDS, perhaps an indication that more experienced nurses had comfort with the organization’s electronic systems. Compared to per diem nurses, whose earnings are proportional to the number of visits they provide, salaried nurses may spend more time at each patient visit, allowing them greater opportunity to review more complicated care management strategies with patients. Overall nurse caseload was not associated with CDS use; however, the more patients identified with complex medication regimens for which a nurse was responsible in the study, the more likely he/she was to use the CDS. Because intervention nurses received an email alert directing them to the MRC module for every patient identified at-risk, repeated prompts may have led to greater familiarity with the tool, encouraging greater use.
Practice features measured at the patient level also were associated with CDS use. Lack of continuity in care had a large impact on CDS use. The original nurse assigned to the case received the email alert and specific mention of the MRC module; however, when the nurse in charge of a patient’s care was changed during the course of a care episode, the MRC module was less likely to be used. This suggests that handoffs from one nurse to another were not as effective as they could have been, despite the presence of the EHR to facilitate communication. Longer home care episodes and more nursing visits also were associated with higher CDS use, perhaps because nurses had more opportunity to use the module. Alternatively, higher service use may have been produced by CDS use.
Consistent with the literature, we also found certain patient characteristics to be associated with CDS use[28,29]. While some of the associations are easily interpretable, others are less intuitive. For example, nurses were more likely to use the CDS with patients taking a greater number of medications. While all patients for whom the nurses received an alert had complex medication regimens, it is possible that a nurse was “more convinced” of the patient’s risk when the number of medications was greater. Perceptions of risk also might help explain why nurses were more likely to use CDS with patients who were short of breath at admission or had a cardiac condition or stroke. Conversely, nurses were less likely to use CDS for cancer patients and those with a higher number of chronic conditions. The medications of many cancer patients are time limited, so nurses may have concentrated on helping patients understand their purpose and administration instructions as opposed to simplifying the regimen and focusing on the long-term management strategies offered in the CDS. In the case of patients with multiple co-morbidities, nurses may have given higher priority to other condition-specific care management interventions.
Perhaps the most disconcerting finding was the lower use of CDS when caring for African American patients. It is possible that patient’s race is a proxy for unmeasured sociodemographic factors, including health literacy, which would explain a nurse’s decision to focus on more pressing issues related to the patient’s management of their health conditions rather than on strategies for simplifying medication regimens or synchronizing refills. A similar rationale may apply to our finding of lower CDS use among Medicaid beneficiaries. Finally, privately insured patients often have a narrowly defined purpose and length of home care service, so nurses caring for them may have felt more restricted in their scope of practice.
Limitations
Three main limitations should be considered when reflecting on the implementation and methods of this study. First, the intervention was implemented in an active home care organization – where patient service delivery needs and operational constraints, of necessity, may have impeded the “purity” of the intervention and affected nurses’ exposure to it, or their opportunity to pursue a sustained effort to address medication regimen complexity. For example, our study protocol identified the nurse who was assigned as the coordinator of care (COC) for the newly admitted patient and transmitted the electronic components of the intervention to her (intention to treat approach). In 3% of the cases, however, the COC changed during the course of care (e.g., in case of the clinician’s illness or leave of absence) to a COC in a different randomized group than the originally identified COC. Thus some ‘contamination’ of the intervention was not reflected in our intention to treat analysis. Second, there was no in-service orientation to the MRC module. The availability of the module was “introduced” in the clinical alert the nurses received when a risk patient was identified. This was not an uncommon practice at the organization as in-service meetings are costly and time consuming, but it may have contributed to the lower than expected use among patients in the intervention group. Third, episode length was also variable amongst the study population. Moreover, ED visits and hospitalizations were measured at discharge or 60 days post-admission, whichever was earlier (the standard home care hospitalization metric mandated by CMS). Thus not all patients had the same exposure period for the intervention and the endpoints were not all measured at the same interval.
Conclusion
Although the intention to treat analyses revealed no significant intervention impact on patient outcomes, possibly due to limited use of the CDS among intervention nurses, evidence from our analyses of “treatment on treated” effects suggested a sizeable and significant association between use of CDS and reduction in both MRC and probability of hospitalization. CDS use was affected by both nurse and patient characteristics – some remediable and some not. Additional research is needed to elucidate under what clinical, economic and environmental circumstances clinicians opt for using CDS. Further research is also needed to understand barriers to CDS uptake and to explore incentives to promote use of CDS with the goal of improving outcomes for a greater number of patients.
Acknowledgments
We would like to acknowledge the significant support the research team received from several members of the Visiting Nurse Service of New York Information Technology department. In addition, we would like to thank Melissa Trachtenberg for her project coordination support, Janice Foust, PhD, RN and Polina Kogan, PharmD for their collaborative support on the development of the intervention.
FUNDING
This project was supported by grant number R18HS017837 from the Agency for Healthcare Research and Quality (Principal Investigator: Penny H. Feldman, PhD). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
REFERENCE LIST
- 1.American Geriatrics Society. Beers Criteria Update Expert Panel. (2012) American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. Journal of the American Geriatrics Society. 2012;60(4):616–631. doi: 10.1111/j.1532-5415.2012.03923.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bao Y, Shao H, Bishop TF, Schackman BR, Bruce ML. Inappropriate medication in a national sample of US elderly patients receiving home health care. Journal of General Internal Medicine. 2012;27(3):304–310. doi: 10.1007/s11606-011-1905-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hu SH, Capezuti E, Foust JB, Boltz MP, Kim H. Medication discrepancy and potentially inappropriate medication in older Chinese-American home-care patients after hospital discharge. American Journal of Geriatric Pharmacotherapy. 2012;10(5):284–295. doi: 10.1016/j.amjopharm.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 4.McKibbon KA, Lokker C, Handler SM, et al. Enabling medication management through health information technology (Health IT) Evidence Report Technology Assessment (Full Rep) 2011;201:1–951. [PMC free article] [PubMed] [Google Scholar]
- 5.Jaspers MW, Smeulers M, Vermeulen H, Peute LW. Effects of clinical decision-support systems on practitioner performance and patient outcomes: a synthesis of high-quality systematic review findings. Journal of the American Medical Informatics Association. 2011;18(3):327–334. doi: 10.1136/amiajnl-2011-000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hemens BJ, Holbrook A, Tonkin M, Mackay JA, Weise-Kelly L, Navarro T, Wilczynski NL, Haynes RB CCDSS Systematic Review Team. Computerized clinical decision support systems for drug prescribing and management: a decision-maker-researcher partnership systematic review. Implementation Science. 2011;6:89. doi: 10.1186/1748-5908-6-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nieuwlaat R, Connolly SJ, Mackay JA, Weise-Kelly L, Navarro T, Wilczynski NL, Haynes RB CCDSS Systematic Review Team. Computerized clinical decision support systems for therapeutic drug monitoring and dosing: a decision-maker-researcher partnership systematic review. Implementation Science. 2011;6:90. doi: 10.1186/1748-5908-6-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mansur N, Weiss A, Beloosesky Y. Looking Beyond Polypharmacy: Quantification of Medication Regimen Complexity in the Elderly. American Journal of Geriatric Pharmacotherapy. 2012;10(4):223–229. doi: 10.1016/j.amjopharm.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 9.Ingersoll KS, Cohen J. The impact of medication regimen factors on adherence to chronic treatment: a review of literature. Journal of Behavioral Medicine. 2008;31(3):213–224. doi: 10.1007/s10865-007-9147-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Corsonello A, Pedone C, Lattanzio F, Lucchetti M, Garasto S, Carbone C, Greco C, Fabbietti P, Incalzi RA. Regimen complexity and medication nonadherence in elderly patients. Journal of Therapeutics and Clinical Risk Management. 2009;5(1):209–216. doi: 10.2147/tcrm.s4870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Willson MN, Greer CL, Weeks DL. Medication regimen complexity and hospital readmission for an adverse drug event. Annals of Pharmacotherapy. 2014;248(1):26–32. doi: 10.1177/1060028013510898. [DOI] [PubMed] [Google Scholar]
- 12.Orwig D, Brandt N, Gruber-Baldini AL. Medication management assessment for older adults in the community. Gerontologist. 2006;46(5):661–668. doi: 10.1093/geront/46.5.661. [DOI] [PubMed] [Google Scholar]
- 13.Muir AJ, Sanders LL, Wilkinson WE, Schmader K. Reducing medication regimen complexity: a controlled trial. Journal of General Internal Medicine. 2001;16(2):77–82. doi: 10.1046/j.1525-1497.2001.016002077.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Elliott RA, O’Callaghan C, Paul E, George J. Impact of an intervention to reduce medication regimen complexity for older hospital inpatients. International Journal of Clinical Pharmacy. 2013;35(2):217–224. doi: 10.1007/s11096-012-9730-3. [DOI] [PubMed] [Google Scholar]
- 15.Caffrey C, Sengupta M, Moss A, Harris-Kojetin L, Valverde R. National health statistics reports; no 38. Hyattsville, MD: National Center for Health Statistics; 2011. Home health care and discharged hospice care patients: United States, 2000 and 2007. [PubMed] [Google Scholar]
- 16.Ellenbecker CH, Samia L, Cushman JJ, Alster K. Patient safety and quality in home health care (chapter 13) In: Hughes R, editor. Patient Safety and Quality: An Evidence-Based Handbook. Washington, DC: 2008. AHRQ Publication No. 08-0043. [PubMed] [Google Scholar]
- 17.Murtaugh C, Peng T, Totten A, Costello B, Moore S, Aykan H. Complexity in geriatric home healthcare. Journal for Healthcare Quality. 2009;31(2):34–43. doi: 10.1111/j.1945-1474.2009.00017.x. [DOI] [PubMed] [Google Scholar]
- 18.Bercovitz AR, Park-Lee E, Jamoom E. National health statistics reports; no 66. Hyattsville, MD: National Center for Health Statistics; 2013. Adoption and use of electronic health records and mobile technology by home health and hospice care agencies. [PubMed] [Google Scholar]
- 19.Madigan EA, Fortinsky RH. Interrater reliability of the outcomes and assessment information set: results from the field. Gerontologist. 2004;44(5):689–692. doi: 10.1093/geront/44.5.689. [DOI] [PubMed] [Google Scholar]
- 20.McDonald MV, Peng TR, Sridharan S, Foust JB, Kogan P, Pezzin LE, Feldman PH. Automating the medication regimen complexity index. Journal of the American Medical Informatics Association. 2013;20(3):499–505. doi: 10.1136/amiajnl-2012-001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kawamoto K, Houlihan CA, Balas EA, Lobach DF. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. British Medical Journal. 2005;330(7494):765. doi: 10.1136/bmj.38398.500764.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.George J, Phun YT, Bailey MJ, Kong DC, Stewart K. Development and validation of the medication regimen complexity index. Annals of Pharmacotherapy. 2004;38(9):1369–1376. doi: 10.1345/aph.1D479. [DOI] [PubMed] [Google Scholar]
- 23.Hirsch JD, Metz KR, Hosokawa PW, Libby AM. Validation of a patient-level medication regimen complexity index as a possible tool to identify patients for medication therapy management intervention. Pharmacotherapy. 2014;34(8):826–835. doi: 10.1002/phar.1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McDonald HP, Garg AX, Haynes RB. Interventions to enhance patient adherence to medication prescriptions: scientific review. Journal of the American Medical Association. 2002;288(22):2868–2879. doi: 10.1001/jama.288.22.2868. [DOI] [PubMed] [Google Scholar]
- 25.Murtaugh CM, Pezzin LE, McDonald MV, Feldman PH, Peng TR. Just-in-time evidence-based e-mail “reminders” in home health care: impact on nurse practices. Health Services Research. 2005;40(3):849–864. doi: 10.1111/j.1475-6773.2005.00388.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feldman PH, Murtaugh CM, Pezzin LE, McDonald MV, Peng TR. Just-in-time evidence-based e-mail “reminders” in home health care: impact on patient outcomes. Health Services Research. 2005;40(3):865–885. doi: 10.1111/j.1475-6773.2005.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Linder JA, Rigotti NA, Schneider LI, Kelley JH, Brawarsky P, Schnipper JL, Middleton B, Haas JS. Clinician characteristics and use of novel electronic health record functionality in primary care. Journal of the American Medical Informatics Association. 2011;18(Suppl 1):i87–90. doi: 10.1136/amiajnl-2011-000330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Moxey A, Robertson J, Newby D, Hains I, Williamson M, Pearson SA. Computerized clinical decision support for prescribing: provision does not guarantee uptake. Journal of the American Medical Informatics Association. 2010;17(1):25–33. doi: 10.1197/jamia.M3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sittig DF, Krall MA, Dykstra RH, Russell A, Chin HL. A survey of factors affecting clinician acceptance of clinical decision support. BMC Medical Informatics and Decision Making. 2006;6:6. doi: 10.1186/1472-6947-6-6. [DOI] [PMC free article] [PubMed] [Google Scholar]


