Abstract
Background and Aims:
Ultrasonography has emerged as a novel, portable, non-invasive tool encouraging airway assessment and procedural interventions. This study assesses the feasibility of ultrasound for block of internal branch of superior laryngeal nerve (ibSLN) block during upper airway anaesthesia to aid awake fibre-optic intubation.
Methods:
Forty American Society of Anesthesiologists’ physical status I–II patients, aged 18–60 years, deemed to have a difficult airway (modified Mallampati class III–IV or inter-incisor distance <2.5 cm) and planned for awake fibre-optic intubation were randomised to either landmark group (L, n = 20) or ultrasound group (U, n = 20). All patients received nebulised 4% lignocaine (3 mL) and transtracheal injection 3 mL 2% lignocaine. Group L received landmark-guided bilateral ibSLN block with 1 mL 2% lignocaine. Group U received bilateral ibSLN block with 1 mL 2% lignocaine using a high-frequency ultrasound transducer to define the SLN space. The primary objective was assessment of quality of airway anaesthesia. Secondary objectives were time for intubation, haemodynamic parameters and patient perception of discomfort during procedure.
Results:
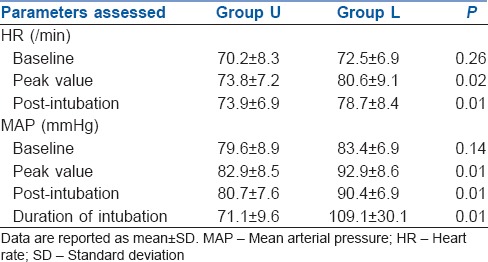
The quality of anaesthesia was significantly better in Group U than in Group L (P < 0.001). The mean time for intubation was shorter in Group U (71.05 ± 9.57 s) compared to Group L (109.05 ± 30.09 s, P < 0.001). Heart rate, mean arterial pressure and patient perception of discomfort were significantly increased in Group L.
Conclusion:
Ultrasound for ibSLN block as a part of preparation for awake fibre-optic intubation improves quality of airway anaesthesia and patient tolerance.
Keywords: Airway anaesthesia, fibre-optic intubation, superior laryngeal nerve, ultrasound
INTRODUCTION
Awake fibre-optic intubation is an established airway management technique in the management of the difficult airway. Psychological and pharmacological preparation of the patient plays a pivotal role in technical success of awake fibre-optic intubation.[1] Since awake intubation causes discomfort to patients, a variety of techniques have been described to achieve airway anaesthesia, such as topical application of local anaesthetics and injection of local anaesthetic agents at specific anatomic landmarks to block the afferent neural transmission from the oropharynx and larynx.[2]
The superior laryngeal nerve (SLN) has its origin from the vagus nerve and descends posterior to the carotid artery towards the larynx. At the level of hyoid bone, it divides into external and internal branches [Figure 1]. The internal branch provides sensory innervation of mucous membrane of the larynx above the level of vocal cords including base of the tongue and epiglottis. The internal branch passes immediately inferior to the greater horn of the hyoid bone and approaches the thyrohyoid membrane. The external branch provides motor supply to cricothyroid muscle.[3] In patients undergoing awake fibre-optic intubation as a part of airway anaesthesia, an internal branch of SLN (ibSLN) block is frequently performed and is conventionally done by recognising the greater horn of the hyoid bone and superior horn of the thyroid cartilage as anatomic landmarks.[4]
Figure 1.
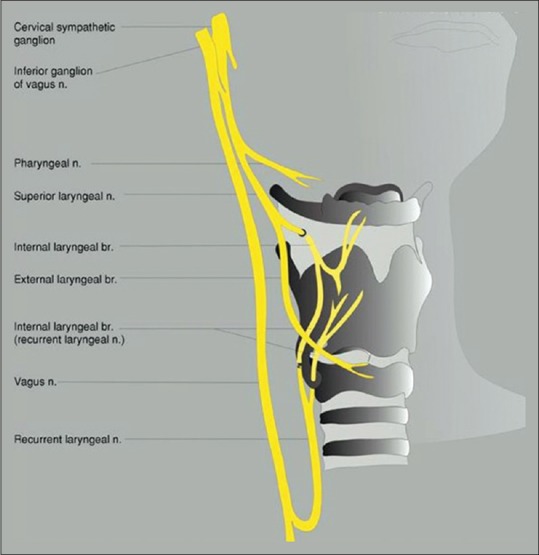
The course of superior laryngeal nerve and its branches
Ultrasonographic imaging is a novel, portable, non-invasive tool encouraging anaesthesia-related airway assessment and procedural interventions. To date, very few case reports are available assessing the usefulness of ultrasound over the conventional landmark-guided technique to block the ibSLN. Our study was designed to assess the feasibility of novel ultrasound guidance while performing ibSLN block for upper airway anaesthesia to aid awake fibre-optic intubation.
METHODS
After obtaining approval from the Hospital Research Ethics Committee, patient counselling was done regarding need and procedure of awake fibre-optic intubation, and a written informed consent was obtained from all the participating patients. Forty American Society of Anesthesiologists’ physical status I–II patients, aged 18–60 years, deemed to have difficult airway (modified Mallampati class III–IV or inter-incisor distance <2.5 cm) scheduled for various elective surgeries under general anaesthesia where awake fibre-optic intubation was planned were enrolled in this prospective randomised clinical trial.
Patients with local pathology of the neck, bleeding diathesis, allergy to local anaesthetic agents, intellectual impairment or psychiatric conditions precluding adequate communication and body mass index ≥30 kg/m2 were excluded from the study.
Patients were randomised to undergo ibSLN block with either anatomical landmark-guided or ultrasound technique. The allocation sequence was generated using online randomisation software (http://www.randomization.com). The allocation was concealed in sealed envelopes that were opened after patient consent had been obtained.
In the operation room, monitors were attached which included electrocardiogram, pulse oximeter, non-invasive blood pressure and end-tidal carbon dioxide.
Nebulisation with 3 mL 4% lignocaine was given over 10 min to all patients, and they were premedicated with intravenous glycopyrrolate 10 μg/kg and midazolam 0.03 mg/kg. Oxygen supplementation was given throughout the procedure.
In anatomical landmark technique (Group L), with patient in supine position and head slightly extended, greater horn of hyoid (GHH) bone and thyroid cartilage were identified, and under aseptic precautions, the ibSLN was blocked by inserting the 23-gauge hypodermic needle below and slightly anterior to the GHH. 1 mL 2% lignocaine was deposited, and the procedure was repeated on the contralateral side.
In ultrasound technique (Group U), the SonoSite MicroMaxx™ portable ultrasound device (SonoSite™, Bothell, WA, USA) and linear 6–13 MHz ultrasound transducer were used. Under aseptic precautions, the probe was placed over the submandibular area with parasagittal orientation. The GHH bone and thyroid cartilage were identified as hyperechoic structures on sonography. The thyrohyoid muscle and thyrohyoid membrane were between these two structures. SLN space was defined as that bounded by hyoid bone cephalad, thyroid cartilage caudally, thyrohyoid muscle anteriorly and thyrohyoid membrane and pre-epiglottic space posteriorly [Figure 2]. By the out-of-plane approach, 1 mL 2% lignocaine was injected using 23-gauge hypodermic needle between GHH bone and thyroid cartilage just above the thyrohyoid membrane. The procedure was repeated on the contralateral side.
Figure 2.
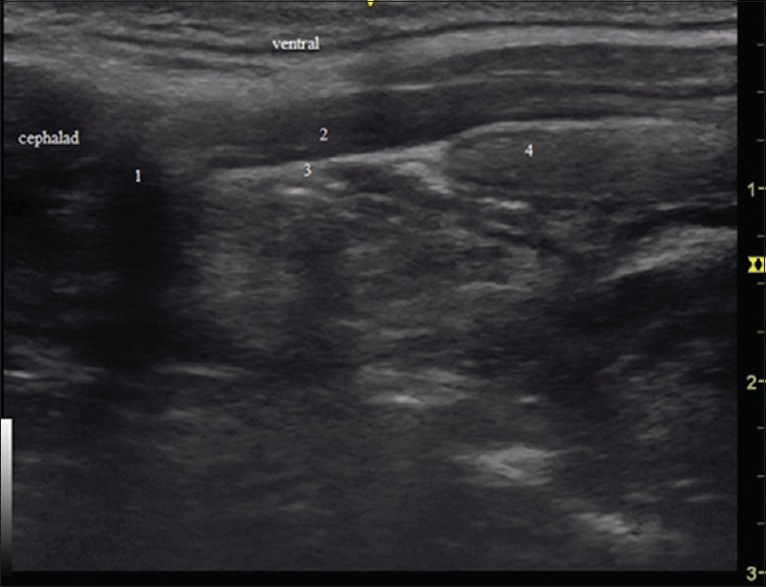
Left parasagittal sonography (1) greater horn of hyoid bone, (2) thyrohyoid muscle, (3) thyrohyoid membrane, (4) thyroid cartilage
Transtracheal injection with 3 mL 2% lignocaine between thyroid cartilage and cricoid ring was administered to all patients. The primary objective was an assessment of quality of airway anaesthesia assessed on a 5-point scale[5] by an observer blinded to technique of block, who entered the operation room after the airway block. Airway anaesthesia was graded as: 0 = no coughing or gagging in response to intubation, 1 = mild coughing and/or gagging that did not hinder intubation, 2 = moderate coughing and/or gagging that interfered minimally with intubation, 3 = severe coughing and/or gagging that made intubation difficult and 4 = very severe coughing and/or gagging that required additional local anaesthetic and/or change in technique to achieve successful intubation.
The secondary objectives were time for intubation, effects on haemodynamic variables, and patient perception of pain and discomfort during intubation. Time to intubation was defined as time between insertion of fibrescope through nostril to successful placement of endotracheal tube and confirmation by the presence of end-tidal CO2. Effect on haemodynamic variables such as heart rate (HR), mean arterial pressure (MAP) and oxygen saturation were recorded before intubation (baseline), peak value during intubation and 1 min after intubation. Patient perception of pain and discomfort during intubation was assessed 12 h postoperatively using numerical rating scale (NRS) (0–10 scale, with 0 being no discomfort and 10 being worst discomfort).
Sample size calculation was based on the quality of airway anaesthesia score results of an initial pilot study. The difference in mean score was 0.86 and standard deviation in Group L was 0.70 and Group U 0.73. For 80% power of the study with an α error 0.05, sample size turned out to be 17 in each group. Hence, twenty patients were enrolled in each group. Statistical analysis was done using SPSS software version 20. All values are expressed as mean ± standard deviation. Chi-square test and Student's unpaired t-test were applied and P < 0.05 was considered statistically significant.
RESULTS
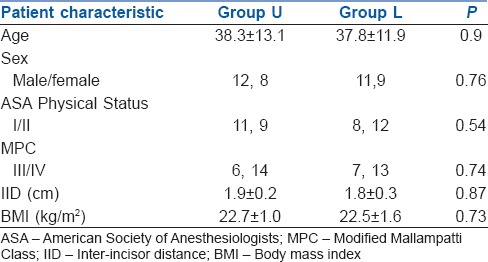
A total of forty consenting patients with anticipated difficult airway were enrolled in this prospective clinical trial, and there were no dropouts. Demographic profile and airway parameters [Table 1] were comparable between the two groups. All patients were successfully intubated.
Table 1.
Patient characteristics
The quality of airway anaesthesia, as assessed by an observer blinded to the technique of the block, was significantly (P < 0.001) better in Group U with lower quality of airway anaesthesia score (mean 0.45 ± 0.60) as compared to Group L (mean 1.60 ± 0.88) [Figure 3]. The duration of tracheal intubation was shorter in Group U (mean 71.05 ± 9.57s) as compared to Group L (mean 109.05 ± 30.09 s, P < 0.001).
Figure 3.
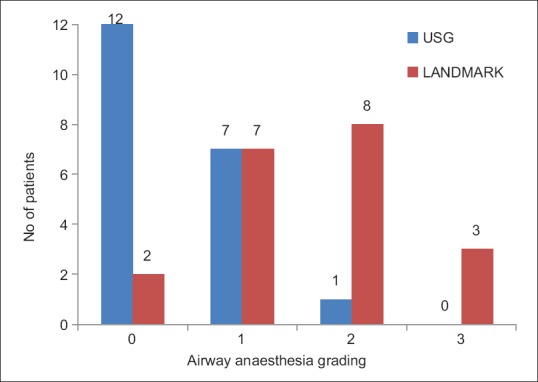
Distribution of participants based on four-point quality of airway anaesthesia grades. USG - Group U, Landmark - Group L
The effect of tracheal intubation on HR and MAP was significantly higher in Group L with a higher peak (during intubation) and post-intubation values with reference to pre-intubation baseline value in contrast to Group U [Table 2].
Table 2.
Data of haemodynamic profile and time required for intubation with each technique of airway block
The patient perception of pain and discomfort during intubation assessed postoperatively based on NRS [Figure 4] was significantly lower with better patient tolerance in Group U with mean NRS score of 2.75 ± 0.78 as compared to Group L with mean NRS score of 4.0 ± 1.14 (P < 0.001). There was no difference between the groups with regard to success rate of intubation or adverse events.
Figure 4.
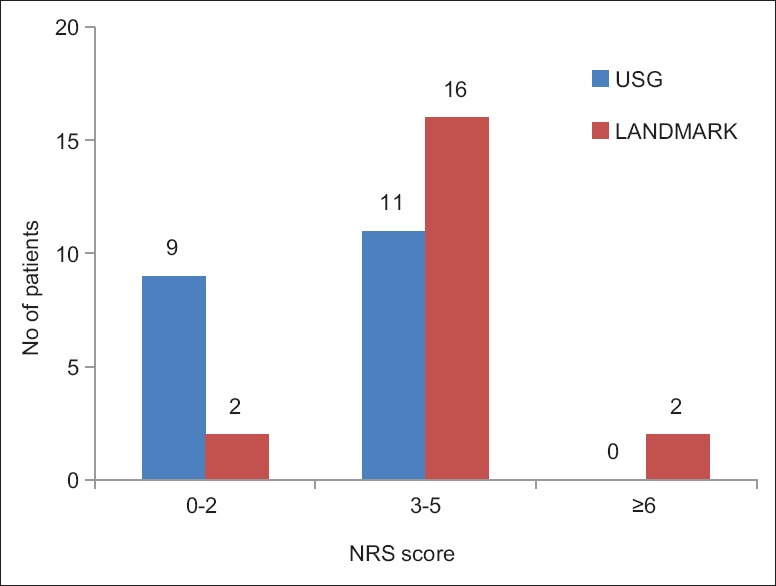
Distribution of patients according to perception of discomfort during intubation based on numerical rating scale score (0–10). USG - Group U, Landmark - Group L
DISCUSSION
There are several techniques described to anaesthetise the tracheobronchial tree, each with its own potential advantages and disadvantages. The ideal anaesthetic technique would require a lower dose of local anaesthetic agent with higher block success rate. It would be safe and tolerable for the patient and at the same time would provide acceptable conditions for intubation. Our study assessed a novel method for ibSLN under ultrasound guidance. Using the high-frequency linear array probe and defining SLN space, through out-of-plane technique, we injected local anaesthetic agent. The quality of airway anaesthesia as assessed by a blinded observer was significantly better in Group U with shorter duration of intubation, better patient tolerance and haemodynamic stability.
Several limitations have been reported with the landmark-guided technique. The deep palpation of hyoid bone can be uncomfortable to the patient and is difficult in patients who have a short or thick neck, with higher failure rates. Hypotension and bradycardia have also been associated as a result of excessive manipulation of the larynx causing vasovagal reaction.[6] Similarly, in our study, the need for deep palpation of hyoid and excessive manipulation of larynx in Group L resulted in higher patient perception of discomfort and pain during intubation as depicted by significantly higher NRS score in Group L as compared to Group U.
Combination of bilateral SLN block with topical airway anaesthesia has been reported to produce better haemodynamic stability and patient comfort.[7] However, literature search revealed no randomised studies comparing landmark- and ultrasound-guided technique for ibSLN block. There are very few case reports on the application of ultrasound imaging technique for upper airway anaesthesia.
The first case report on ultrasound-guided ibSLN block was described in a patient scheduled for posterior cervical spine fixation. The authors placed the transducer in the transverse orientation and used an in-plane technique and recognised the superior laryngeal artery as a surrogate marker while performing block of ibSLN, which advanced along with the artery. The local anaesthetic agent was injected near the superior laryngeal artery after negative aspiration of blood, following which awake intubation was performed without complications.[8] However, it has been reported that there exist wide variations in origin of superior thyroid artery and its branch, the superior laryngeal artery.[9]
A study using 8–15 MHz transducer reported that it is possible to identify and target the SLN accurately under ultrasound guidance.[10] Our report also confirmed that ultrasound-guided SLN block is feasible. However, differences exist between these two studies, as we have used SLN space as a surrogate marker. Visualisation of SLN has been reported to be unsuccessful.[11,12,13] This is most likely attributed to small size of the nerve which demands good ultrasonographic experience and a high-resolution transducer. However, the use of higher frequency transducer compromises the penetration depth, particularly in obese patients.
The feasibility of ultrasound-guided ibSLN block was reported in a study using fresh cadavers. The probe was placed longitudinally over the submandibular area, and after identification of the greater horn of the hyoid bone and thyroid cartilage, 2 ml methylene blue dye was injected using an out-of-plane method. Another anatomist dissected the tissue to determine if the nerve was bathed in the dye. It was concluded that ultrasound-guided nerve block was successful in 11 of 12 ibSLN block.[14] Similarly, in our study, the GHH and thyroid cartilage were used as landmarks to define SLN space with the transducer in parasagittal orientation. The use of hockey stick-shaped transducer for ibSLN block has been reported to provide better space for administration of block without compromising the image.[15]
We acknowledge that there are few limitations with regard to our study. The ibSLN was not identified; instead, we used SLN space as a surrogate marker, and the local anaesthetic was deposited in that space. Second, in our study, ultrasound-guided block was performed by experienced anaesthesiologist, and thus the results are variable in the hands of novice. Finally, the sample size was small.
The application of ultrasound marks a new era in airway management. Further studies are required to assess feasibility of ultrasound-guided airway blocks, particularly in obese patients and patients with limited neck extension where identification of anatomical landmarks is difficult.
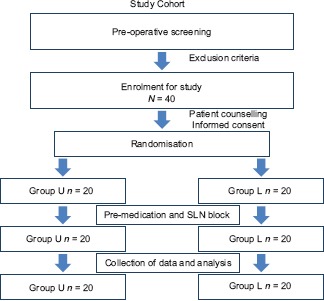
CONSORT flow chart
CONCLUSION
Ultrasound-guided block of ibSLN used as a part of preparation of the airway for awake fibre-optic intubation improves the quality of airway anaesthesia and patient tolerance during the procedure.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We sincerely thank Dr. Manjula R, Associate Professor, Department of Community Medicine, SN Medical College, Bagalkot, Karnataka, India, for the statistical assistance.
REFERENCES
- 1.Ramkumar V. Preparation of the patient and the airway for awake intubation. Indian J Anaesth. 2011;55:442–7. doi: 10.4103/0019-5049.89863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simmons ST, Schleich AR. Airway regional anesthesia for awake fiberoptic intubation. Reg Anesth Pain Med. 2002;27:180–92. doi: 10.1053/rapm.2002.30659. [DOI] [PubMed] [Google Scholar]
- 3.Kundra P, Mishra SK, Ramesh A. Ultrasound of the airway. Indian J Anaesth. 2011;55:456–62. doi: 10.4103/0019-5049.89868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Furlan JC. Anatomical study applied to anesthetic block technique of the superior laryngeal nerve. Acta Anaesthesiol Scand. 2002;46:199–202. doi: 10.1034/j.1399-6576.2002.460214.x. [DOI] [PubMed] [Google Scholar]
- 5.Reasoner DK, Warner DS, Todd MM, Hunt SW, Kirchner J. A comparison of anesthetic techniques for awake intubation in neurosurgical patients. J Neurosurg Anesthesiol. 1995;7:94–9. doi: 10.1097/00008506-199504000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Wiles JR, Kelly J, Mostafa SM. Hypotension and bradycardia following superior laryngeal nerve block. Br J Anaesth. 1989;63:125–7. doi: 10.1093/bja/63.1.125. [DOI] [PubMed] [Google Scholar]
- 7.Kundra P, Kutralam S, Ravishankar M. Local anaesthesia for awake fibreoptic nasotracheal intubation. Acta Anaesthesiol Scand. 2000;44:511–6. doi: 10.1034/j.1399-6576.2000.00503.x. [DOI] [PubMed] [Google Scholar]
- 8.Manikandan S, Neema PK, Rathod RC. Ultrasound-guided bilateral superior laryngeal nerve block to aid awake endotracheal intubation in a patient with cervical spine disease for emergency surgery. Anaesth Intensive Care. 2010;38:946–8. doi: 10.1177/0310057X1003800523. [DOI] [PubMed] [Google Scholar]
- 9.Vázquez T, Cobiella R, Maranillo E, Valderrama FJ, McHanwell S, Parkin I, et al. Anatomical variations of the superior thyroid and superior laryngeal arteries. Head Neck. 2009;31:1078–85. doi: 10.1002/hed.21077. [DOI] [PubMed] [Google Scholar]
- 10.Kaur B, Tang R, Sawka A, Krebs C, Vaghadia H. A method for ultrasonographic visualization and injection of the superior laryngeal nerve: Volunteer study and cadaver simulation. Anesth Analg. 2012;115:1242–5. doi: 10.1213/ANE.0b013e318265f75d. [DOI] [PubMed] [Google Scholar]
- 11.Vaghadia H, Lawson R, Tang R, Sawka A. Failure to visualise the superior laryngeal nerve using ultrasound imaging. Anaesth Intensive Care. 2011;39:503. [PubMed] [Google Scholar]
- 12.Green JS, Tsui BC. Applications of ultrasonography in ENT: Airway assessment and nerve blockade. Anesthesiol Clin. 2010;28:541–53. doi: 10.1016/j.anclin.2010.07.012. [DOI] [PubMed] [Google Scholar]
- 13.Singh M, Chin KJ, Chan VW, Wong DT, Prasad GA, Yu E. Use of sonography for airway assessment: An observational study. J Ultrasound Med. 2010;29:79–85. doi: 10.7863/jum.2010.29.1.79. [DOI] [PubMed] [Google Scholar]
- 14.Lan CH, Cheng WC, Yang YL. A new method for ultrasound-guided superior laryngeal nerve block. Tzu Chi Med J. 2013;25:161–3. [Google Scholar]
- 15.Sawka A, Tang R, Vaghadia H. Sonographically guided superior laryngeal nerve block during awake fiberoptic intubation. A A Case Rep. 2015;4:107–10. doi: 10.1213/XAA.0000000000000136. [DOI] [PubMed] [Google Scholar]


