Abstract
Background and Aims:
Second generation supraglottic airways are increasingly being used in surgical patients undergoing laparoscopic surgery. Preventing aspiration at higher airway pressures may be at the expense of a higher cuff pressure which can impair mucosal perfusion. We attempted to elucidate whether Ambu AuraGain™ (AAU) would provide a higher oropharyngeal leak pressure (OLP) with a lower mucosal pressure in comparison to ProSeal™ laryngeal mask airway (PLMA).
Methods:
This was a prospective randomised study involving sixty patients undergoing laparoscopic cholecystectomy under general anaesthesia, using either AAU (Group AAU [n = 30]) or PLMA (Group PLMA [n = 30]) for elective ventilation. Primary outcome measure was the OLP. Number of insertion attempts, ease of insertion, time required for placement and calculated pharyngeal mucosal pressure were the secondary outcome measures. Data were analysed using Student's t-test and Chi-square test.
Results:
No significant difference in the OLP was noted in both groups. The ease of insertion and success rate at first attempt was similar between the groups. Time taken for insertion in Group AAU was longer than Group PLMA (13.57 ± 1.94 vs. 11.60 ± 2.22 s). The calculated pharyngeal mucosal pressures were lower with Group AAU than Group PLMA for all 3 sizes. The minimum cuff pressure and minimum cuff volume required to prevent leak were found similar in both groups.
Conclusion:
AAU provides adequate sealing pressures and effective ventilation with lower calculated pharyngeal mucosal pressure, compared to PLMA.
Keywords: Airway Management, Ambu AuraGain™, oropharyngeal leak pressure, ProSeal™ laryngeal mask airway, supraglottic devices
INTRODUCTION
Supraglottic Airways (SGAs) have revolutionised the airway management.[1] Besides serving as a rescue device in the difficult airway, and as a conduit for the endotracheal tube insertion, SGAs provide a less invasive and less traumatic means of securing the airway in surgical patients.[2,3]
The introduction of the ProSeal™ laryngeal mask airway (PLMA) (Teleflex®, NC, USA), a second generation SGA, led to its clinical use in patients undergoing laparoscopic surgery.[4] The ability of an SGA to prevent aspiration at higher airway pressures is desirable, but it may be at the expense of a higher cuff pressure which may impair mucosal perfusion. This may result in greater airway morbidities. Thus, an ideal SGA would provide a high oropharyngeal leak pressure (OLP) with a low pharyngeal mucosal pressure.
The Ambu AuraGain™ (Ambu®, DK) is a disposable, preformed second generation SGA with integrated gastric access and intubation capability, introduced some time back.[5] We designed this study to compare the Ambu AuraGain™ (AAU) with the ProSeal™ LMA (PLMA) for patients undergoing laparoscopic cholecystectomy in terms of the OLP and pharyngeal mucosal pressure.
METHODS
This randomised, prospective study was conducted in a super specialty hospital from February 2016 to November 2016 and was approved by the Institutional Ethics Committee. We recruited sixty patients aged 18–65 years with the American Society of Anesthesiologists physical status I–II, who were to undergo elective laparoscopic cholecystectomy under general anaesthesia. Written informed consent was obtained from all patients. The exclusion criteria were obesity (body mass index ≥30 kg/m2), pregnancy, known or predicted difficult airway, reduced lung compliance, mouth opening <2.5 cm and high risk for pulmonary aspiration (nonfasted, gastroesophageal reflux disease).
Patients were wheeled in the operation theatre, monitors including heart rate, noninvasive blood pressure, electrocardiogram, oxygen saturation and temperature probe were connected, intravenous (i.v.) cannula placed and a maintenance fluid (Ringer lactate) was started at the rate of 4 ml/kg/h. Pre-medication was done with midazolam 0.03 mg/kg i.v. Induction of anaesthesia was done with fentanyl 2 μg/kg i.v. and propofol 2–2.5 mg/kg i.v. and maintenance with 50% oxygen and 50% air with 1 minimum alveolar concentration of isoflurane. Muscle relaxation was achieved with atracurium 0.5 mg/kg i.v. The patients were ventilated for 3 min. with a face mask till adequate jaw relaxation was achieved.
Before device insertion, the patients were divided into two groups (30 patients each) and were randomised to receive either the conventional reusable PLMA (Group PLMA) or single use disposable AAU (Group AAU). Randomisation of patients was done according to computer generated random codes that were maintained in sequentially numbered opaque envelopes.
Before inserting the device, the cuff was inflated with maximum permissible air (as per manufacturer's recommendation), and the cuff pressure (ex vivo) was measured with a cuff pressure monitor (Mallinckrodt™ VBM Medizintechnik GmbH® DE).
All SGAs were fully deflated and lubricated with a water-soluble gel. After the adequate depth of anaesthesia and muscle relaxation was achieved, insertion of both devices was performed by an anesthesiologist with more than 10 years’ experience in using the two SGA devices. The patient's head was placed in a “sniffing” position (neck flexion and head extension). In Group AAU, AAU of appropriate size was inserted as per manufacturers’ instructions, and in Group PLMA, ProSeal™ LMA of appropriate size was inserted by introducer tool technique as per manufacturers’ instructions. A size 3, 4 or 5 of either device was selected according to the patient's weight.[6]
After insertion, the device was inflated with the maximum permissible volume of air, and the air entry was checked on both sides of the chest. The in vivo cuff pressure was measured. The pharyngeal mucosal pressure was calculated as: P = Pin vivo − Pex vivo.[7]
We recorded the number of insertion attempts and the time needed for SGA placement, (measured from when the SGA was picked up until the connection to the breathing circuit). The ease of insertion was graded as 1 - easy or 2 - difficult (when deep rotation and jaw thrust or a second attempt was used for proper device insertion).[8] An effective airway was judged by an absence of leak, normal thoracoabdominal movement and square wave capnograph trace. If there was a leak, the SGA was repositioned. If leak persisted after a total of three attempts, the patient was intubated with an endotracheal cuffed tube and recorded as failed insertions.
After confirmation of adequacy of ventilation, airway pressure was maintained at an arbitrarily determined pressure of 18 cm H2O by squeezing the reservoir bag for 10 s. Inflation pressure was measured using an airway pressure gauge. The incidence of airleak around the mask was recorded by detection of an audible noise over the mouth. If there was no leak and ventilation was adequate, air from the cuff was aspirated slowly till leak appeared. At this point, 1cc aliquots of air were reinjected into the cuff till leak disappeared. The residual volume of air left behind in the cuff was considered as the minimum effective volume of air. The minimum effective volume of air and the minimum pressure in the cuff (at this cuff volume) to prevent leak at airway pressure of 18 cm H2O were noted.[7]
Before commencement of the surgery, the cuff was inflated with a manometer and cuff pressure was set to 60 cm of H2O. OLP was measured by closing the expiratory valve of the breathing circuit and delivering a gas flow of 3 L/min until the seal pressure or a maximum pressure of 40 cm H2O was reached. A lubricated 16 Fr gastric tube was introduced via the drain tube of both the devices to aspirate gastric contents. If resistance was felt during the introduction, a 14 Fr gastric tube was used instead.
Peak inspiratory airway pressure was measured before and after the creation of carboperitoneum keeping a constant intra-abdominal pressure of 14 mm Hg in the two groups.
The primary outcome was the OLP. With the help of a pilot study of ten patients per group, the mean OLP was calculated as 29 cm H2O in the PLMA group and 34 cm H2O in the AAU group. The total sample size was calculated as 38 calculated from an effect size of 0.83, a power of 80% and α of 0.05 where the standard deviation of two groups was 6 and 5, respectively. For better validation of our result, the total sample size was set at 60 (a minimum of 30 per group).
Statistical testing was conducted with the International Business Machines Corporation SPSS Statistics for windows (version 17.0, Armonk, NY, USA). Demographic data were analysed using the Student's unpaired t-test and Chi-square test. Ease of insertion, time taken for insertion and OLP were categorised and compared using Mann–Whitney U-test and Chi-square test. For all statistical tests, a P < 0.05 was taken to indicate a significant difference.
RESULTS
Our study enrolled a total of sixty participants who were analysed for the primary outcome. Since there were no exclusions or losses, all participants completed the study [Figure 1].
Figure 1.
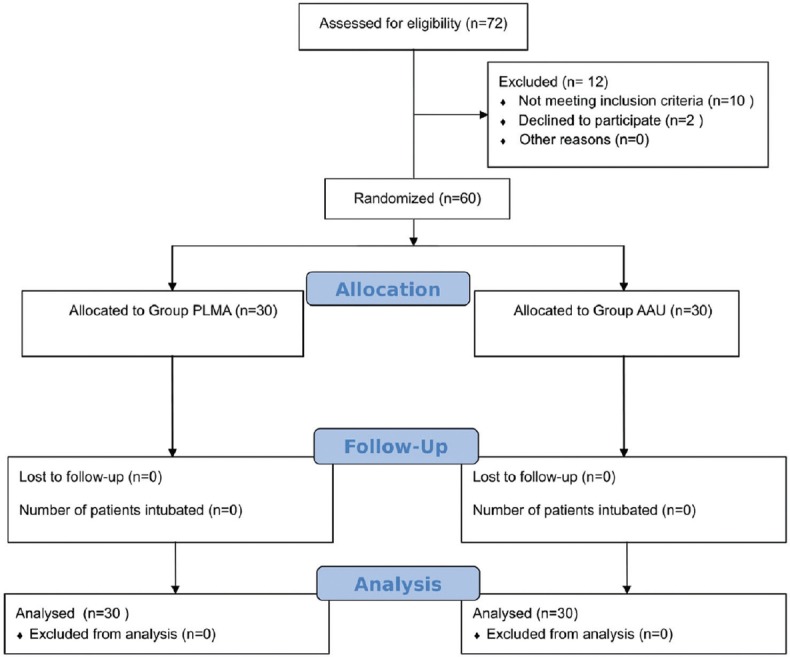
CONSORT flowchart
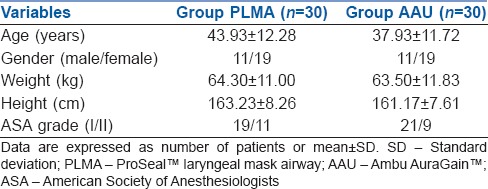
There were no statistically significantly differences between the groups regarding age, gender, weight, height and ASA grade [Table 1].
Table 1.
Patient characteristics
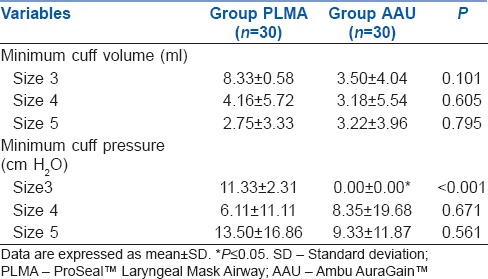
The distribution of the size of SGA used in each group was similar. The ease of insertion and success rate at first attempt was similar amongst both groups. The time taken for insertion of AAU was longer than PLMA. No significant difference in the OLPs was noted in both groups. The peak inspiratory airway pressures before and after insufflation in both groups were comparable. In Group PLMA, a size 14 Fr Ryles Tube was inserted in all the patients, whereas in group AAU, size 16 Fr Ryles Tube was used in 70% of the patients [Table 2]. The calculated pharyngeal mucosal pressures were lower with AAU than PLMA for all 3 sizes of the SGAs. However, the difference was statistically significantly only for a size 4 AAU [Table 3]. The minimum cuff volume required to prevent leak (at 18 cm H2O airway pressure) was found similar in both groups, notably, these values were lower than the maximum recommended values. In size 3 AAU, the minimum cuff pressure (at the minimum cuff volume) required to prevent leak was significantly lower than for a size 3 PLMA [Table 4].
Table 2.
Airway management details
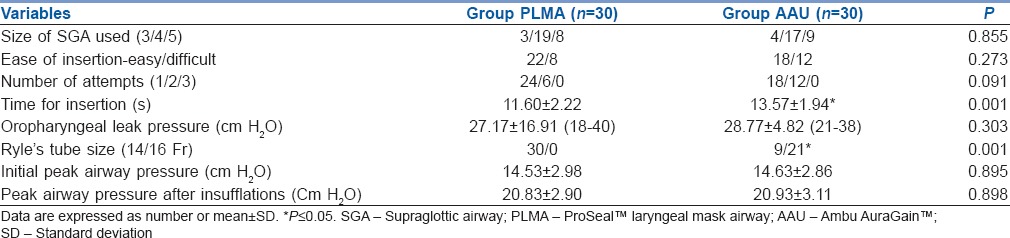
Table 3.
Ex vivo pressure, in vivo pressure and calculated pharyngeal mucosal pressure
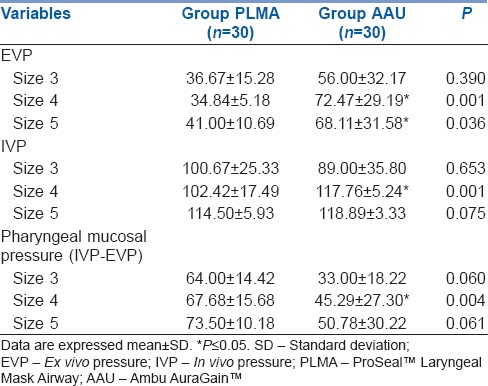
Table 4.
The minimum cuff volume required to prevent a leak, and cuff pressure at that volume
DISCUSSION
PLMA is an established airway device for use in laparoscopic surgeries. AAU has been compared to LMA supreme in a few studies,[9,10,11] but to the best of our knowledge, there is no literature available that compares the clinical efficacy of AAU to PLMA in laparoscopic cholecystectomy. Hence, this study was undertaken to evaluate the safety profile of AAU in a clinical setting.
In our study, we found that both the AAU and PLMA are easy to insert, with a similar successful insertion rate on the first attempt. However, the time for insertion of AAU was significantly higher, and this may be attributed to its rigid PVC preformed structure in contrast to the flexible silicone structure of the PLMA. Gastric tubes were successfully inserted on the first attempt in both the devices. However, AAU allowed the passage of a larger bore gastric tube, making it favourable in situations where a larger tube may help in better gastric decompression.
In laparoscopic surgeries, the incidence of suboptimal and failed ventilation is often high with SGAs owing to the high peak airway pressures required during carboperitoneum. Second generation SGAs allow higher airway pressures due to their effective seal. In our study, we observed that the OLP of AAU was comparable to that of PLMA. A recent study reports higher OLP of AAU in comparison to LMA Supreme™ in patients undergoing gynaecologic laparoscopy.[9] Another study reports similar OLP of AAU and LMA Supreme™ in children during controlled ventilation under general anaesthesia.[10] However, the OLP of AAU was comparable to that of other SGAs such as i-gel, PLMA and LMA Supreme™ as reported in some other studies.[8,12,13] In our study, the OLP of both AAU and PLMA was higher than the peak airway pressure and was sufficient to prevent aspiration while ventilating the study patients during carboperitoneum.
A study reports a progressive reduction in the pharyngeal mucosal perfusion when mucosal pressure increases from 25 to 60 mmHg while using a cuffed oropharyngeal airway.[14] The cuffs exert pressure on the pharyngeal mucosa which causes a concomitant decrease of pharyngeal perfusion and increase in the incidence of post-operative complications including sore throat, dysphonia and nerve damage.[15] We found that the calculated pharyngeal mucosal pressure exerted by AAU was less than PLMA and this may lead to a lower incidence of airway morbidities. However, we did not study the post-operative airway morbidity which may be a limitation of our study.
A study showed that intracuff pressure increased as the cuff volume increased. The pressure exerted on the pharynx by the SGA is usually higher than the mucosal capillary perfusion pressure when the cuff is inflated with the recommended maximum volume of air.[15] However, if the cuff is deflated excessively, it may not protect the airway from soiling, due to the regurgitated fluid from the stomach.[16] Therefore, it is desirable to inflate the cuff of the SGA with a minimum volume of air which provides a seal around the mask. In our study, there was no statistically significant difference between the PLMA and AAU in terms of the minimum effective cuff volume for all three sizes. However, these values were much less than the company recommended maximum values. Hence, removal of air from the cuff of the SGA (from the recommended maximum volume to the effective minimum volume to prevent leak) reduces the intracuff pressure and pressure exerted on the pharynx. Since these values were obtained at an airway pressure of 18 cm H2O, this cuff pressure and volume can be used only for mechanical ventilation in non-laparoscopic surgeries.
Our study has some limitations. First, our study was a single-centre study with a relatively small sample size. More studies are required to confirm the overall safety profile of AAU. Second, we did not measure the mucosal pressures in the pharynx directly with a microchip sensor but used an indirect derived value. Furthermore, the pharyngeal mucosal pressure at the cuff pressure of 60 cm H2O is not known, since it was measured by inflating the cuff with the maximum volume of air recommended. Our study involved patients with a normal airway and whether the same outcome can be extrapolated to patients with difficult airway needs further study. Finally, after repeated use, PLMA may lose its elasticity and cuff permeability may increase leading to higher cuff pressures and mucosal pressures.
CONCLUSION
Ambu AuraGain provides adequate sealing pressures and effective ventilation, hence, it may be considered for use in clinical practice. However, further studies are required to assess how this device compares to other widely utilised SGAs
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We acknowledge the assistance and cooperation received from our departmental colleagues.
REFERENCES
- 1.Pennant JH, White PF. The laryngeal mask airway. Its uses in anesthesiology. Anesthesiology. 1993;79:144–63. doi: 10.1097/00000542-199307000-00021. [DOI] [PubMed] [Google Scholar]
- 2.Kovac AL. Controlling the hemodynamic response to laryngoscopy and endotracheal intubation. J Clin Anesth. 1996;8:63–79. doi: 10.1016/0952-8180(95)00147-6. [DOI] [PubMed] [Google Scholar]
- 3.Prys-Roberts C, Greene LT, Meloche R, Foëx P. Studies of anaesthesia in relation to hypertension. II. Haemodynamic consequences of induction and endotracheal intubation. Br J Anaesth. 1971;43:531–47. doi: 10.1093/bja/43.6.531. [DOI] [PubMed] [Google Scholar]
- 4.Maltby JR, Beriault MT, Watson NC, Liepert D, Fick GH. The LMA-ProSeal is an effective alternative to tracheal intubation for laparoscopic cholecystectomy. Can J Anaesth. 2002;49:857–62. doi: 10.1007/BF03017420. [DOI] [PubMed] [Google Scholar]
- 5.AMBU. Baltorpbakken (DK): ABMU A/S. AuraGain™ Disposable Laryngeal Mask. [Last updated on 2015 Nov 13; Last cited on 2017 May 15]. Available from: http://www.ambu.com/corp/products/anaesthesia/product/auragain%E2%84%A2_disposable_laryngeal_mask-prod18315.aspx .
- 6.Dorsch JA, Dorsch SE. Understanding Anesthesia Equipment. 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2007. pp. 474–5. [Google Scholar]
- 7.Asai T, Howell TK, Koga K, Morris S. Appropriate size and inflation of the laryngeal mask airway. Br J Anaesth. 1998;80:470–4. doi: 10.1093/bja/80.4.470. [DOI] [PubMed] [Google Scholar]
- 8.Singh I, Gupta M, Tandon M. Comparison of clinical performance of I-Gel with LMA-Proseal ™ in elective surgeries. Indian J Anaesth. 2009;53:302–5. [PMC free article] [PubMed] [Google Scholar]
- 9.Lopez AM, Agusti M, Gambus P, Pons M, Anglada T, Valero R. A randomized comparison of the Ambu AuraGain™ versus the LMA supreme in patients undergoing gynaecologic laparoscopic surgery. J Clin Monit Comput. 2016 doi: 10.1007/s10877-016-9963-0. Epub 2016 Nov 26. [DOI] [PubMed] [Google Scholar]
- 10.Jagannathan N, Hajduk J, Sohn L, Huang A, Sawardekar A, Gebhardt ER, et al. A randomised comparison of the Ambu® AuraGain™ and the LMA® supreme in infants and children. Anaesthesia. 2016;71:205–12. doi: 10.1111/anae.13330. [DOI] [PubMed] [Google Scholar]
- 11.Lopez AM, Sala-Blanch X, Valero R, Prats A. Cross-over assessment of the AmbuAuraGain, LMA supreme new cuff and intersurgical I-Gel in fresh cadavers. Open J Anesthesiol. 2014;4:332–9. [Google Scholar]
- 12.López AM, Valero R, Hurtado P, Gambús P, Pons M, Anglada T. Comparison of the LMA Supreme™ with the LMA Proseal™ for airway management in patients anaesthetized in prone position. Br J Anaesth. 2011;107:265–71. doi: 10.1093/bja/aer104. [DOI] [PubMed] [Google Scholar]
- 13.Gasteiger L, Brimacombe J, Perkhofer D, Kaufmann M, Keller C. Comparison of guided insertion of the LMA ProSeal ™ vs. the i-gel ™. Anaesthesia. 2010;65:913–6. doi: 10.1111/j.1365-2044.2010.06422.x. [DOI] [PubMed] [Google Scholar]
- 14.Brimacombe J, Keller C, Pühringer F. Pharyngeal mucosal pressure and perfusion: A fiberoptic evaluation of the posterior pharynx in anesthetized adult patients with a modified cuffed oropharyngeal airway. Anesthesiology. 1999;91:1661–5. doi: 10.1097/00000542-199912000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Marjot R. Pressure exerted by the laryngeal mask airway cuff upon the pharyngeal mucosa. Br J Anaesth. 1993;70:25–9. doi: 10.1093/bja/70.1.25. [DOI] [PubMed] [Google Scholar]
- 16.Brimacombe J, Berry A, Brain AI. Optimal intracuff pressures with the laryngeal mask. Br J Anaesth. 1996;77:295–6. doi: 10.1093/bja/77.2.295-a. [DOI] [PubMed] [Google Scholar]


