Sir,
We report perioperative anaesthetic concerns related to the first robotic nipple sparing mastectomy with breast expander implant (BEI). This relatively new surgical technique provides satisfactory surgical results, less pain and better patient compliance in addition to hidden scar.[1] Toesca et al. who pioneered this technique have highlighted the surgical aspects. General anaesthesia is required similar to other robotic surgeries with a few variations as highlighted below.
The position of the robotic cart in relation to the anaesthesia workstation is crucial for smooth conduct of surgery. The patient's cart was placed on contralateral side of the operation [Figure 1] with robotic arms near parallel to the floor [Figure 2]. As our workstation was fixed to the pendant, it was kept towards the foot end to provide ample working space. The position of anaesthesia workstations is optional until it does not interfere in surgical field, and still we recommend to keep it at foot end. This layout requires long breathing circuit (two standard circuits of 180 cm connected in series) and a 100 cm extension line connected to intravenous (IV) infusion set, as the cannula is not easily accessible in docked position, additional IV in foot is desirable as a precautionary measure.
Figure 1.

Robotic patient cart positioned on the contralateral side of the operation and the robotic arms come above the patient for docking
Figure 2.
Robotic arms docked through patient access system device which are aligned nearly parallel to the floor
Initially, the patient was positioned supine till resection of breast tissue and BEI insertion and later semi-reclined for the assessment of breast symmetry. We suggest pelvic straps and foot restrains to be applied to prevent sliding down of the patient in semi-recline position. Wide-opened elbow is a prerequisite for surgical access which can be achieved by placing the patient supine at the edge of table with the ipsilateral upper limb sagging below it [Figure 3], and the contralateral limb resting by the side of the patient. Such a position could lead to brachial plexus injury due to gravitational pull and stretching on the unsupported limb, though Toesca et al. have not reported any nerve injury.[2] Placing a silicone gel pad between the edge of the table and arm [Figure 3] prevents brachial plexus and pressure injury on the medial aspect of the operative limb. Resting the ipsilateral hand on pelvis with adhesive tapes also supports limb and prevents overstretching of limb. Inserting a small scaffold from the edge of table underneath the elbow may be helpful to reduce the stretching force on the brachial plexus.
Figure 3.
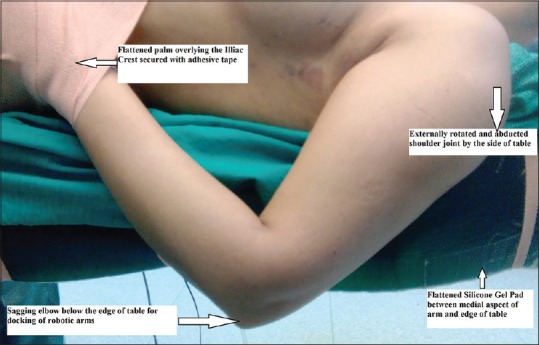
Silicone gel pad placed underneath the sagging left upper limb with wide-opened elbow for docking of robotic arms
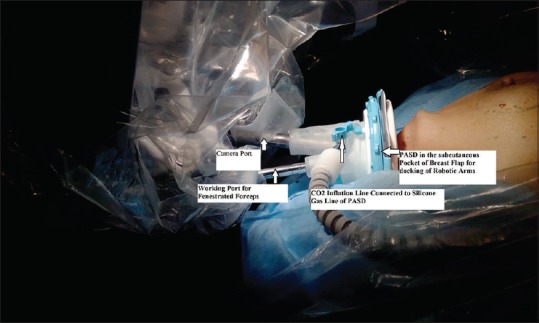
Subcutaneous pocket was lifted to insert single patient access system device [Figure 4], through which robotic arms were docked. CO2 was insufflated at 2–7 mmHg with flow rate at 20 L/min to keep the breast flap elevated, which could cause hypercarbia and post-operative surgical emphysema. Limiting insufflation pressure up to 6 mmHg is sufficient to maintain the surgical space while preventing significant CO2 absorption through the subcutaneous tissue.[3] CO2 insufflation in closed body cavities usually necessitates change in ventilator settings, but in spite of not changing the ventilator settings, no post-operative surgical emphysema and capnothorax was observed.
Figure 4.
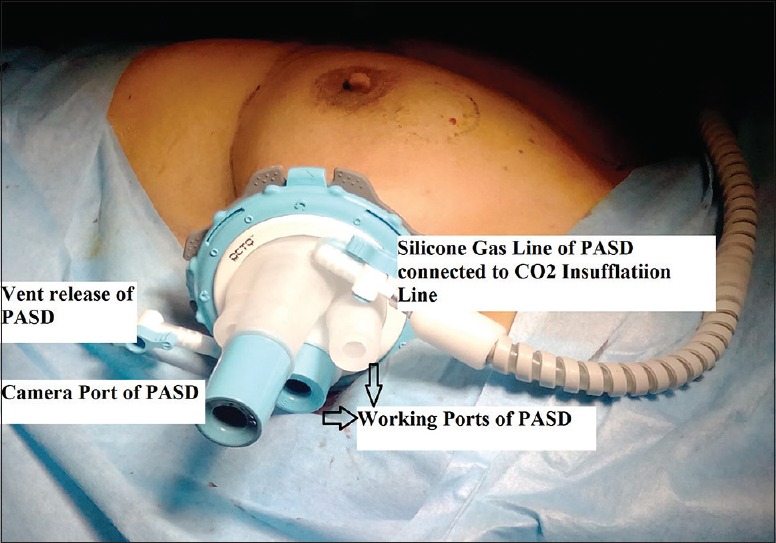
Patient access system device fitted into the subcutaneous pocket of breast flap, allowing camera and other robotic instrument to work through a small incision
Thermal injury of flap due to fibre-optic light and heated fumes from electrocautery[4] is prevented by intermittent evacuation of CO2, smoke and cooling of the flap with wet gauze. Variable heat conductance in the body tissue (lower conductance in adipose tissue as compared to muscle and skin) further protects against thermal injury.[5,6]
Pectoral nerve blocks (PECS I and II) were performed through the open surgical wound by surgeons before BEI insertion, which provided excellent post-operative analgesia and considerably reduced the opioid requirement. Bashandy and Abbas have recommended the use of PECS blocks to reduce the post-operative pain, morphine consumption, nausea and vomiting with lesser sedation scores for radical breast surgery.[7] We suggest PECS block through open surgical incision as BEI hampers with post-operative block.
Robotic surgery may require innovations with regard to patient positioning and overall arrangement of operative equipment and personnel, which may go against conservative nature of anaesthesia care. Anaesthesiologists should become familiar with these changes by learning basic features to offer better anaesthetic care and promote patient safety.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Toesca A, Peradze N, Manconi A, Galimberti V, Intra M, Colleoni M, et al. Robotic nipple-sparing mastectomy for the treatment of breast cancer: Feasibility and safety study. Breast. 2017;31:51–6. doi: 10.1016/j.breast.2016.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Toesca A, Manconi A, Peradze N, Loschi P, Panzeri R, Granata M, et al. Preliminary report of robotic nipple-sparing mastectomy and immediate breast reconstruction with implant. Eur J Cancer. 2015;51:S309. [Google Scholar]
- 3.Ochiai R, Takeda J, Noguchi J, Ohgami M, Ishii S. Subcutaneous carbon dioxide insufflation does not cause hypercarbia during endoscopic thyroidectomy. Anesth Analg. 2000;90:760–2. doi: 10.1097/00000539-200003000-00046. [DOI] [PubMed] [Google Scholar]
- 4.Hindle AK, Brody F, Hopkins V, Rosales G, Gonzalez F, Schwartz A. Thermal injury secondary to laparoscopic fiber-optic cables. Surg Endosc. 2009;23:1720–3. doi: 10.1007/s00464-008-0219-z. [DOI] [PubMed] [Google Scholar]
- 5.Advincula AP, Wang K. The evolutionary state of electrosurgery: Where are we now? Curr Opin Obstet Gynecol. 2008;20:353–8. doi: 10.1097/GCO.0b013e3283073ab7. [DOI] [PubMed] [Google Scholar]
- 6.Neufeld GR. Principles and hazards of electrosurgery including laparoscopy. Surg Gynecol Obstet. 1978;147:705–10. [PubMed] [Google Scholar]
- 7.Bashandy GM, Abbas DN. Pectoral nerves I and II blocks in multimodal analgesia for breast cancer surgery: A randomized clinical trial. Reg Anesth Pain Med. 2015;40:68–74. doi: 10.1097/AAP.0000000000000163. [DOI] [PubMed] [Google Scholar]


