Abstract
BACKGROUND
When pain management has been studied in settings such as pediatric emergency departments, racial disparities have been clearly identified. To our knowledge, this has not been studied in the pediatric perioperative setting. We sought to determine whether there are differences based on race in the administration of analgesia to children suffering from pain in the post anesthesia care unit.
METHODS
A prospective, observational, study of 771 children aged 4–17 years who underwent elective outpatient surgery. Racial differences in probability of receiving analgesia for pain in the recovery room were assessed using bivariable and multivariable logistic regression analyses.
RESULTS
A total of 294 children (38.2%) received at least one class of analgesia (opioid or non-opioid); while 210 (27.2%) received intravenous opioid analgesia in the recovery room. Overall post anesthesia care unit analgesia utilization was similar between white and minority children (whites 36.8% vs. minority children 43.4%, OR 1.3; 95% CI = 0.92–1.89; p=0.134). We found no significant difference by racial/ethnic group in the likelihood of a child receiving intravenous opioid for severe postoperative pain (whites 76.0% vs. 85.7%, OR 1.89; 95% CI = 0.37–9.67; p=0.437). However, minority children were more likely to receive intravenous opioid analgesia than their white peers (whites 24.5% vs. minority children 34.2%, OR 1.5; 95% CI = 1.04–2.2; p=0.03). On multivariable analysis, minority children had a 63% higher adjusted odds of receiving intravenous opioids in the recovery room (OR =1.63; 95% CI, 1.05–2.62; p=0.03).
CONCLUSIONS
Receipt of analgesia for acute postoperative pain was not significantly associated with a child’s race. Minority children were more likely to receive IV opioids for the management of mild pain.
Keywords: Racial disparity, ethnic minority, pain management, pediatric ambulatory surgery, post-anesthesia care unit
Introduction
Controversies and concerns regarding racial disparities in health care for adults and children are well documented in the United States (1–2). Racial and ethnic differences in pain response and pain management have been persistently reported in a wide variety of settings (3–6). In the emergency department (ED), racial and ethnic differences in wait times, use of pain medications for abdominal pain including pain associated with acute appendicitis have been reported (7–9). Furthermore, black and Hispanic children have been shown to be less likely to receive opioid drugs for acute pain treatment in the ED (10).
About 3.3 million children undergo ambulatory surgical procedures every year in the United States (11). Unfortunately, many of these surgical procedures are associated with pain requiring intervention in the post anesthesia care unit (PACU) (12,13). Opioids are the mainstay of treatment for acute postoperative pain despite their known side effects and related adverse events (14). Most studies to date have focused on the anesthetic and surgical factors associated with higher acute postoperative pain (12, 13), thereby largely ignoring the inter-patient variability in pain behavior and opioid requirement.
One increasingly recognized determinant of postoperative pain experience and opioid requirement in children is the subject’s ethnicity (15). In this retrospective study, the investigators found that Latino children received 30% lower doses of opioids than their Caucasian peers. Given that this was a retrospective study with relatively small sample sizes, there is a clear need to critically examine the role of race/ethnicity in the PACU administration of analgesia.
To date, few investigators (15,16) have specifically examined race/ethnicity-based differences in PACU pain management of children following ambulatory surgical procedures. Consequently, the broad objective of this study was to evaluate race/ethnicity-based differences PACU analgesic treatment of pain among children who underwent painful elective ambulatory surgery. Based on existing data from the ED and other settings (8–9,15–16) we hypothesized that racial/ethnicity-based differences would be present in the PACU pain management of children recovering from anesthesia. Following the rationale that severe PACU pain will be associated with increased odds of opioid administration, we further tested the secondary hypothesis that children’s race/ethnicity does not determine the odds of PACU analgesic administration for postoperative pain (pain score ≥7). Exploring simple self-report measures such as race/ethnicity could help identify children who are likely to require analgesic intervention upon recovering from anesthesia in the PACU which could prove critical to the provision of “personalized analgesia”.
Methods
Study Design
This report is part of a larger on-going study to determine the incidence and risk factors for postoperative pain requiring treatment in the PACU among children aged 4–17years undergoing elective, ambulatory surgical procedures at the Mott Children’s Hospital (Ann Arbor, MI). The Institutional Review Board of the University of Michigan approved this prospective, observational, cross-sectional study. Present analyses included patients recruited from January 24, 2015 to December 16, 2015.
Study Population and Data Source
Patient enrollment occurred on randomly selected weekdays during the preoperative interview. All patients scheduled for outpatient surgery on selected days were approached for possible inclusion in the study. Perioperative caregivers (anesthesiologists and nurses) did not know subject recruitment days in advance nor were they aware of the study’s hypotheses. Trained research assistants (RAs) collected baseline clinical and anthropometric data on study enrollees. In order not to interfere with nursing care and PACU throughput, postoperative data were abstracted in real time from nursing notes by the RAs. Patients with chronic pain disorders or those taking preoperative analgesic medications were excluded from the study. Patients were also excluded if they were unable to self-report their pain after surgery (significant cognitive impairment). Additionally, patients undergoing non-surgical or painless procedures like magnetic resonance imaging (MRI) or computerized tomographic (CT) scans were not enrolled in this study. Finally, we only included painful surgical procedures identified by the intraoperative administration of intravenous analgesia (opioid or non-opioid), use of local anesthetic infiltration or nerve block.
Outcome measures
Our primary outcome measure was the administration of PACU analgesia (total, IV opioid, and non-opioid) by race. After surgery, children were monitored in the PACU, where analgesic administration and consumption were recorded. PACU analgesic administration was recorded as categorical (yes/no), by type (opioid or non-opioid) as well as by type of opioid (morphine or fentanyl). The traditional approach in many PACUs (including ours) is to administer intravenous (IV) analgesia as first line treatment given that patients are just recovering from general anesthesia. Typically, the PACU nurses administer analgesics prescribed by the anesthesia caregiver for clinically significant postoperative pain (numeric pain score ≥4). Our secondary outcome measure was the association of PACU analgesia use with PACU length of stay, defined as the time in minutes from PACU admission to PACU discharge.
Covariates
Primary exposure variable was racial identity coded as white, black/African American, Latino, Asian, Pacific Islander, and American Indian/Alaska Native. The research team recorded race as described by parents and from patient’s electronic medical records. We then re-categorized the race variable as white or minority, which is consistent with our patient demographics and previous approach by other investigators (8).
Children were observed throughout their stay in the PACU by nurses. Postoperative pain was scored by each child’s bedside nurse upon recovery from anesthesia or within 15min of PACU admission and at scheduled intervals throughout the PACU stay using the Faces Legs Activity Cry Consolability (FLACC) behavioral observation scale or the numeric pain scale as applicable.
The following predictor variables were recorded: age (yr.), sex, surgical specialty, height (cm), weight (Kg), body mass index (BMI in kg/m2), as well as duration of surgery and anesthesia. Patient characteristics such as habitual snoring and history of obstructive sleep apnea were also noted. Intraoperative analgesia use was recorded as a categorical (yes/no) variable as well as by type (opioid or non-opioid). Morphine equivalents were calculated using generally accepted equivalents: fentanyl 0.02 mg per 1 mg of IV morphine (14).
Statistical Analysis
Data analysis was carried out using PASW Statistics v.22.0 program for Windows (SPSS Inc. Chicago, IL). Basic descriptive statistics, including means, standard deviations and percentages were calculated for demographic and clinical data. Univariate factors associated with PACU pain treatment were assessed with Chi-squared or t-test as necessary.
Multivariable Regression Analysis
To fit two multivariable logistic regression models, we estimated the Pr(Y=1|X), with Y being the binary dependent variables (receipt of any PACU analgesia and receipt of IV opioid yes/no) and X is the vector of the covariates. The probability of receipt of PACU analgesia (any and IV opioid) was thus modeled with age, gender, race, first recorded PACU pain score (modeled as a continuous variable), and intra-operative opioid use dose included as predictors. The results from the logistic regression analyses are presented as adjusted odds ratios (ORs) with 95% confidence intervals (CI).
In order to determine whether the relationship of racial class and PACU receipt of any analgesia or receipt of IV opioids in the PACU is moderated by first arousal pain score, we included the interaction between racial/ethnic identity and first arousal pain score in the logistic regression model. Goodness of fit of the logistic regression models was assessed using the Hosmer-Lemeshow test (17). All reported P values were two-sided and a P value of <0.05 was considered to be statistically significant.
An a priori sample size calculation was not performed for this study, because the sample size was drawn as a subset of a larger study population. A post-hoc power analysis showed that ethnic/racial group sizes of 152 and 619, respectively, have 84.6% power (two-tail test; α= 0.05) to detect a difference between the group proportions for the rates of PACU IV morphine administration (12.3% for whites vs. 22.1% for minorities). Sample size calculations were computed using PASS 14 (PASS 14 Power Analysis and Sample Size Software (2015).
Results
A total of 807 parents were approached to participate in the study of whom 36 were not recruited. Six patients were excluded because of surgical cancellation while the remaining 30 subjects did not consent to participate in the study. Refusal to participate in the study did not vary by ethnicity. Therefore, to date, 771 children (boys = 426 (55.6%) have been enrolled. The mean (±SD) age of the subjects was 9.64±4.03 years and majority of the enrollees were white (80.3%). Other described racial identities were as follows: African American 8.3%; Latino American 5.8%; Asians Americans 4.0 and others 1.7%. Due to the low proportion of patients belonging to the non-white racial categories, the race/ethnicity variable was collapsed into a white vs. minority variable and subsequent analyses were along these lines. Baseline clinical and perioperative variables were comparable between the two groups except for a significantly higher prevalence of overweight/obesity among minority children (Table 1). Analysis of BMI with one-way ANOVA indicated a statistically significant difference among the groups (F =4.19; p=0.016). Further analysis with Tukey’s pairwise comparison procedure to adjust for multiple testing indicates that the mean BMI of black children (20.88±5.4kg/m2) was significantly greater than for white children (18.88±4.9kg/m2) and other races (18.04±5.0kg/m2). Many children underwent procedures in otolaryngology, although there was no significant difference in patient distribution by race across surgical specialties (Fig. 1). In the intraoperative period, use of non-opioid and multimodal analgesia was similar between the groups (Table 1).
Table 1.
Patient perioperative characteristics according to racial group
| Variables | Whites (N=619) | Minorities (152) | Total (771) | p- value |
|---|---|---|---|---|
| Continuous variables (Mean ±SD) | ||||
| Age (years) | 9.64±4.03 | 9.46±4.15 | 9.61±4.1 | |
| Weight (kg) | 38.52±20.8 | 39.41±22.6 | 38.69±21.2 | |
| BMI (kg/m2) | 18.88±4.9 | 19.60±5.3 | 19.02±5.01 | |
| PACU time (min) | 101.41±59.6 | 114.14±53.6 | 103.87±58.7 | 0.019 |
| Surgery duration | 42.74±44.5 | 35.18±31.49 | 41.22±42.3 | 0.065 |
| MS equivalents/kg | 0.08±0.08 | 0.09±0.06 | 0.08±0.07 | 0.433 |
| Categorical variables (%) | ||||
| Sex (male) | 54.8 | 57.2 | 55.3 | 0.583 |
| Snoring history | 27.5 | 34.2 | 28.8 | 0.102 |
| OSA history | 7.1 | 10.5 | 7.8 | 0.159 |
| Oral premedication | 32.1 | 39.5 | 33.6 | 0.087 |
| Overweight/Obese | 27.5 | 38.2 | 29.6 | 0.012 |
| OR opioid | 84.2 | 88.2 | 85.0 | 0.218 |
| OR Non-opioid | 55.1 | 58.6 | 55.8 | 0.441 |
| MM analgesia | 51.2 | 53.3 | 51.6 | 0.646 |
| Regional anesthesia | 1.6 | 2.0 | 1.7 | 0.759 |
| Local infiltration | 31.8 | 29.6 | 31.8 | 0.597 |
| PACU Nausea | 9.0 | 7.2 | 8.7 | 0. 478 |
| PACU vomiting | 4.8 | 5.3 | 4.8 | 0. 832 |
| Emergence agitation | 6.0 | 6.6 | 6.1 | 0. 781 |
Abbreviations: OSA = Obstructive sleep apnea; OR= Operating room; PACU = post-anesthesia care unit; BMI = Body mass index; MS = Morphine sulfate; MM analgesia = multi-modal analgesia
Fig. 1.
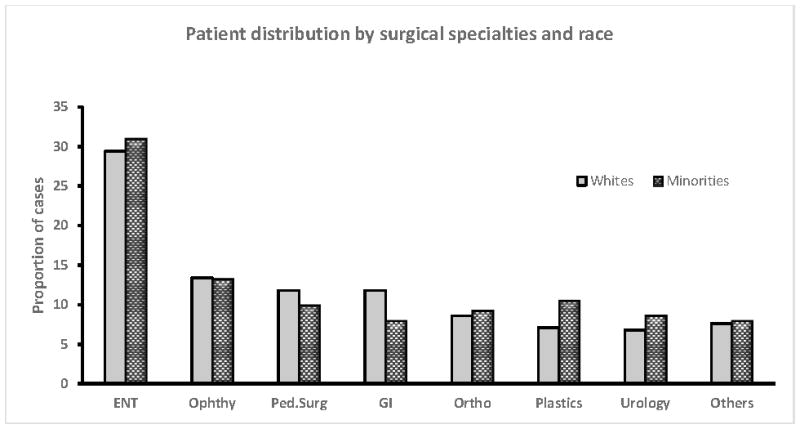
Showing patient distribution according to surgical specialties and race. There was no significant difference in the distribution of cases across specialties by race (χ2 = 5.5; p=0.69).
Abbreviations: ENT = Ear, Nose and Throat; Ophthy. = Ophthalmology; Ped.surg =Pediatric Surgery; GI = Gastrointestinal
There was no statistically significant difference by racial group in the frequency of moderately severe PACU pain (whites 26.0% vs. minority children 28.9%; P=0.46). In general, 38.2% (95% CI = 34.7%-41.5%) of patients received some class of analgesic in the PACU, while 27.2% (95% CI = 24.0%-30.3%) received at least one intravenous opioid analgesic. Correspondingly, 15.7% (95%CI = 13.1%-18.3%) received at least one non-opioid analgesic. Expectedly, a higher first recorded PACU pain score was significantly associated with higher unadjusted odds of receiving any analgesia (OR = 1.50, 95%CI = 1.40–1.60; p<0.001) or IV opioid analgesia (OR = 1.53, 95%CI = 1.43–1.63; p<0.001).
In the initial bivariate analyses, there was no evidence of statistically significant differences between the racial groups in the rates of PACU administration of any analgesia (Whites 36.8% vs. minority children 43.4%, P=0.134) or non-opioid analgesia (15.8% for white children vs. 15.1% for minority children; P=0.832). We did, however, find that minority children were significantly more likely to receive IV opioid analgesia in the PACU than their white peers (Fig. 2a). Indeed, among those with mild pain (N=566), minority children were twice as likely as their white peers to be given IV opioids (22.2% for minority children and 11.1% for white children; P=0.002). Furthermore, minority children were also more likely to receive IV morphine overall (Fig. 2a) and for treating severe postoperative pain (Fig. 2b). We found no significant differences in our setting between the racial groups in the likelihood of a child being treated with any IV analgesic for severe postoperative pain (Fig. 2b). Interestingly a higher proportion of white children were treated for severe PACU pain with a faster onset and shorter acting opioid (IV fentanyl) than minority children. This difference was however not statistically significant (Fig. 2b).
Fig. 2.
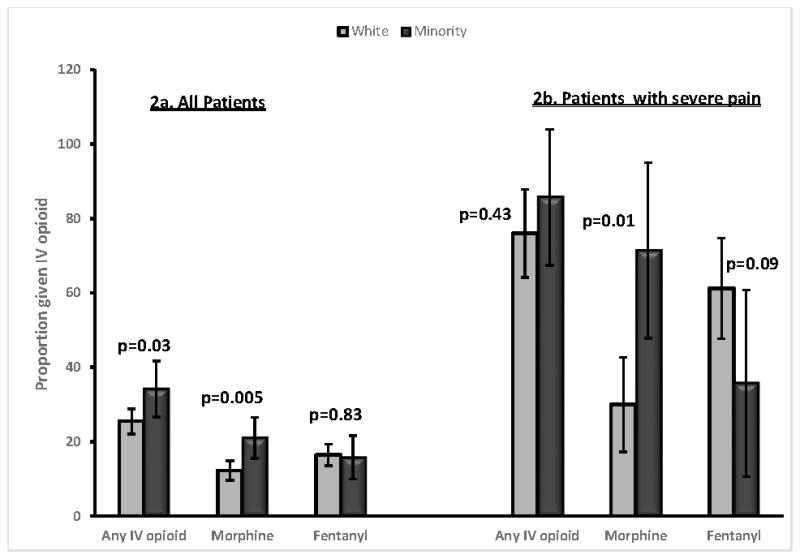
Proportion of patients receiving PACU opioid analgesia overall and among those with documented severe pain by race/ethnicity. Unadjusted bivariable comparisons and p-values generated with Pearson χ2 test.
Abbreviations: PACU = Post anesthesia care unit; IV= intravenous
Surgical procedure sub-group analysis
Given that surgical procedures are associated with varying degrees of invasiveness and thus postoperative pain, we conducted subgroup analysis of patients who underwent tonsillectomy ±adenoidectomy (T&A, N=105). T&A is a very common procedure in children and it is known to be associated with significant perioperative pain (12,17). In this subset of patients, minority children were more likely to have undergone T&A than their white peers (minority children 19.6% vs. white children 9.8%; p=0.01). There was however no difference by race in the odds of receiving PACU IV opioids among those with clinically important pain (documented pain score ≥4). In this analysis, 88.2% of minority children vs. 75.6% of white children received PACU IV opioids for moderately severe pain (OR 2.4, 95%CI = 0.47–12.45; p=0.2).
Next, we also examined the two most frequent orthopedic procedures in this ambulatory surgical cohort to determine whether there are racial differences in the distribution of these orthopedic procedures. The two most frequent procedures were “hardware removal” N=36 and open reduction and internal fixation (ORIF), N=22. There was no significant difference by racial category in the distribution of these procedures (hardware removal minority children 42.1% vs. white children 50.7%; p=0.506); ORIF, minority children 26.7% vs. white children 36.5%; p=0.478).
In Table 2 we display the results of our multivariable analysis adjusted for racial group, age, gender, intraoperative use of opioid and first PACU pain scores. We found no statistically significant differences between race groups in the odds of receiving any analgesic medication in the PACU. First postoperative pain score and intraoperative use of opioid were the strongest predictors of PACU analgesic administration. However, in the model predicting IV opioid use, racial group was a significant predictor of PACU IV opioid use. Specifically, holding all the other covariates in the model constant, minority children had adjusted odds of receiving IV opioids in the PACU that were 63% higher than their white peers (adjusted OR=1.63; 95% CI=1.05–2.62).
Table 2.
Multivariable predictors of any analgesic and IV opioid administration in the post-anesthesia care unit by race/ethnicity (N=771).
| Variables | IV opioid given OR (95%CI) |
p-value | Any Analgesic given OR (95%CI) |
p- value |
|---|---|---|---|---|
| Age (years) | 1.00 (0.95–1.05) | 0.97 | 0.99 (0.95–1.04) | 0.94 |
| Male sex | 0.81 (0.55–1.20) | 0.81 | 0.84 (0.60–1.12) | 0.34 |
| Regional block use | 0.99 (0.65–1.51) | 0.96 | 0.87 (0.59–1.28) | 0.49 |
| Race/Ethnicity | ||||
| White | 1(Reference) | 1(Reference) | ||
| Minority | 1.63 (1.05–2.62) | 0.03 | 1.30 (0.86–1.97) | 0.21 |
| Arousal pain score | 1.52 (1.42–1.62) | <0.001 | 1.48 (1.38–1.58) | <0.001 |
| OR MS equivalents/kg | 2.87 (1.37–6.03) | 0. 005 | 2.09 (1.21–3.61) | 0.008 |
| Race*Arousal pain | 0.86 (0.74–0.99) | 0.046 | 0.94 (0.79–1.11) | 0.492 |
| Pseudo R2= 0.39 | Pseudo R2= 0.32 | |||
| H-L test = χ2 = 7.54, df=8; p=0.48 | H-L test = χ2 = 8.82, df=8; p=0.34 | |||
Abbreviations: OR= Operating room; IV = Intravenous; H-L = Hosmer-Lemeshow test; OR =odds ratio; CI = confidence interval; χ2 = Chi- squared.
Considering the race by arousal pain score interaction in the model for use of IV opioids, we found significantly lower odds of receiving IV opioids for a unit increase in first arousal pain score when race was white (OR = 0.86, 95%CI= 0.74–0.99), thus suggesting that the effect of race was still present even with increasing pain scores. However, the significant negative coefficient for the interaction means that this strong minority effect becomes weaker as the pain score increases. That is, the gap between minority and white children in the probability of PACU IV opioid use becomes smaller with increasing pain scores.
To test the hypothesis that PACU pain was associated with longer PACU length of stay (LOS) and that this varied by racial category, we first compared the mean PACU LOS across pain categories (pain score <3 vs. >3). Expectedly, children with moderately severe first arousal pain had significantly longer mean PACU stay than those in the mild pain category (117.7±72.7 minutes vs. 98.9±52.0 minutes; p<0.001). On average, minority children had slightly longer PACU stays. Next we compared the mean PACU LOS by pain treatment categories (any analgesia yes/no). On average, children who received any analgesia stayed 33 minutes longer in the PACU than their peers who did not require analgesic intervention (124.1±70.8 minutes vs. 91.5±45.6 minutes; p<0.001).
Discussion
In this prospective cross-sectional study of children and adolescents, we report for the first time in an ambulatory surgical cohort, that race/ethnicity did not appear to affect the overall likelihood of a child receiving analgesic medication in the PACU. More importantly, race/ethnicity was not a factor in the administration of IV opioid or any analgesia for documented severe pain. Indeed, we demonstrated that minority children were more likely than their white peers to receive IV opioid overall and for documented mild postoperative pain. There thus appear to be a “minority advantage” in the frequency of IV opioid use among our subjects.
Acute postoperative pain is associated with increased postoperative complications, prolonged post anesthesia care unit (PACU) and hospital stay, delayed ambulation, unplanned hospital admission, increased hospital costs, and patient dissatisfaction (18–20). To this end, patients and their family members expect good perioperative pain control. Additionally, the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) has determined that prompt assessment and management of pain are required standards for all hospitals (21). Identification of specific patient group at risk for early postoperative pain will encourage individual attention to their management. Determining whether postoperative pain is worsened by race or ethnicity, and why this occurs, should facilitate the development of “personalized analgesic” regimens for children undergoing ambulatory surgical procedures.
Racial disparity is a highly charged and contentious topic in contemporary America. That disparity in health care exists is well documented (3, 5–10), so much so that achieving health equity is one of the major goals of the Healthy People 2020 (22). Disparities in acute pain management have been most extensively documented in the ED where ethnic/racial minorities have been shown to receive pain medications less frequently and in lower doses than their white peers. Perhaps more disconcerting is the report that minority patients were less likely than whites to receive strong analgesia for documented severe pain (8).
Despite the widely reported racial differences in pain management in other settings, much remains to be known about the effect of race on the treatment of pain among children recovering from anesthesia in the PACU. It is reassuring that our findings do not mirror the findings from many ED studies in that we found no ethnic/racial disparity in our setting in the overall treatment of pain nor the treatment of severe pain. The only difference appears to be in the choice of analgesic medication used. Minority children were significantly more likely to receive IV morphine than their white peers for mild pain and for the same category of severe pain.
Very few prospective studies on the influence of race on the treatment of acute pain in the pediatric PACU have been published (23). In a prospective, observational study of 194 children who underwent tonsillectomy, Sadhasivam et al concluded that African American children were significantly more likely to require opioid analgesic intervention in the PACU, which indicates they received opioid analgesic more frequently than their white peers. Our study of a much larger sample of children who underwent a wide variety of painful surgical procedures concurs with Sadhasivam’s observations. While these authors investigated the role of race as a predictor of PACU opioid requirement, our finding that race/ethnic category was not a significant factor among children with clinically important PACU pain is highly reassuring.
Although pain is a highly subjective experience, we can surmise that even if the etiology of pain among children presenting to the ED is different from postoperative pain, it is improbable that the subjective experience will differ substantially. Consequently, we speculate that practical differences between the ED and PACU may partially explain some our findings. Most PACU have “open ward design” and possibly more favorable nurse: patient ratio than the ED. An open ward design permits direct line of sight to the children and relatively short distances between bays which facilitates simultaneous observation of several patients, thus making for prompt identification and treatment of a child in pain. Furthermore, symptoms such as abdominal pain, dental pain commonly investigated in ED studies may be considered “non-definitive conditions” (24) and therefore subject to misinterpretation and reluctance to treat. On the other hand, postoperative pain is due (for the most part) to what was “done” to the patient in the operating room and it can be confirmed by simple observation thus warranting prompt treatment.
We realize that physical differences between the ED and PACU construction are insufficient to explain the racial differences in opioid analgesic administration observed in our study subjects. Previously reported biologic differences (23,25) may partly explain the higher rates of opioid requirements by minority children. There may also be cultural dissonance in the interpretation of pain behavior by the predominantly white PACU nurses in our hospital. Whereas a PACU nurse may elect to attempt non-pharmacologic methods to pacify a distressed Caucasian child with documented mild pain, he/she may opt for pharmacotherapy for a minority child. Health provider factors have been previously shown to affect pain assessment and treatment of minority adult patients (25). There is unfortunately no way to confirm this from the present study design.
Our findings of the association of PACU pain and pain intervention with longer PACU LOS agrees with previous studies (27, 28). That patient with moderately severe pain on arousal from anesthesia have longer PACU LOS is not surprising because they were more likely to require pain treatment which may further add to delay in PACU discharge. Identifying factors such as race as an important predictor of PACU IV opioid analgesia requirement may help with planning PACU throughput and should be taken into consideration in future studies of PACU LOS following ambulatory surgery.
Limitations
This study has several strengths including large sample size and prospectively collected variables which reduces the likelihood of misclassification bias. Analgesic (especially opioid) administration in the PACU is strictly monitored; therefore, patients with documented analgesia did receive the drugs thus removing the confounding effect of prescribed drugs not actually getting to the patient. Despite these, the present report does have some limitations. First, we could not determine the invasiveness of the surgical procedures which could affect pain severity or the nurses’ decision to treat pain in the PACU. Second, we did not collect data on our subjects’ pain coping skills, their socio-economic status or their genetic makeup, factors that could potentially affect pain perception and the need to receive analgesics. We did not collect insurance data on our subjects but know from hospital data that 20% of our patients are on Medicare/Medicaid. However, the focus of the present study was on recovery room pain, so we had no reason to believe that insurance status would be a factor in the recovery room since this information would have been collected at the pre-surgical visit. Whereas insurance status may be highly relevant to choice of care in emergency department setting (9) or in the choice of regional anesthesia care offered to patients (29), most providers do not consider a patient’s insurance status in the PACU. We do recognize the strong association between insurance status and socioeconomic standing and the strong possibility that socioeconomic status is likely NOT equally distributed between minorities and non-minorities. To this end, caregivers could easily determine for themselves what kind of social group a given patient/family is coming from and this could affect the care given (just as race might). Future investigators should endeavor to explore the possible association of insurance and socio-economic status on the PACU pain management in children.
Furthermore, we did not examine the consequences of PACU analgesia treatment such as pruritus and respiratory depression. It would have been informative to see whether these varied by racial group and whether these complications affected the nurses’ decision to treat a particular child’s pain. We also recognize the problem with aggregating all minority ethnic groups into one category, which we did because of sample size considerations. Differences in biological and socio-economic profiles among ethnic minorities may account for some of our results. Finally, our findings may not be applicable to populations with substantially different racial mix from ours.
In conclusion, we found no persuasive evidence in our setting that disparities in pain management exist among children recovering from surgery and anesthesia, a particularly vulnerable population. Indeed, we found that minority children were more likely to receive strong opioid analgesia for mild pain and they were just as likely as their white peers to be treated for documented severe pain. Despite these findings from a single center study, studies such as ours are needed to foster future research and improve education about ethnic differences in pain experiences and management in the perioperative setting. There is a clear need to direct increased efforts towards the improvement of perioperative analgesia for all patients and healthcare providers ought to strive for the difficult but attainable goal of personalized analgesia for all patients. To this end, future investigators should expand on our study by exploring the role of specific race/ethnic classification on perioperative care in general and postoperative analgesia use in particular. Exploring whether or not perioperative care-gaps exists based on specific racial grouping in future studies should help clarify some of the issues we were unable to address in the present report.
What is known on the subject
There is compelling evidence suggesting that minority children are at a disadvantage when acute pain treatment has been critically examined in hospital settings especially in the Emergency Department. Disparity in early postoperative pediatric pain management has not been previously studied.
What this study adds
We examined early postoperative pain management of children recovering from anesthesia and found no evidence in our setting of ethnic/racial bias against minority children. There was a “minority advantage” when it comes to using strong opioid analgesia. Race was not a significant factor in the treatment of severe postoperative pain.
Clinical Implications
Considering patient-specific determinants of early postoperative pain is critical to providing optimal analgesia for children undergoing surgery and anesthesia.
Acknowledgments
Funding source: National Institute of General Medical Sciences (NIGMS) grant number K23 GM104354 supported all phases of Dr. Nafiu’s involvement in this research.
Footnotes
Financial Disclosure: All the authors have indicated they have no financial relationships relevant to this article.
Conflict of Interest: All the authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Kirby JB, Taliaferro G, Zuvekas SH. Explaining racial and ethnic disparities in health care. Med Care. 2006;44:I64–I72. doi: 10.1097/01.mlr.0000208195.83749.c3. [DOI] [PubMed] [Google Scholar]
- 3.Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA. 1993;269(12):1537–9. [PubMed] [Google Scholar]
- 4.Fiscella K, Franks P, Gold MR, Clancy CM. Inequality in quality: addressing socioeconomic, racial, and ethnic disparities in health care. JAMA. 2000;283(19):2579–2584. doi: 10.1001/jama.283.19.2579. [DOI] [PubMed] [Google Scholar]
- 5.Green CR, Baker TA, Smith EM, Sato Y. The effect of race in older adults presenting for chronic pain management: A comparative study of African and Caucasian Americans. J Pain. 2003;4:82–90. doi: 10.1054/jpai.2003.8. [DOI] [PubMed] [Google Scholar]
- 6.Green CR, Baker TA, Sato Y, Washington TL, Smith EM. Race and chronic pain: A comparative study of young African and Caucasian Americans presenting for management. J Pain. 2003;4:176–83. doi: 10.1016/s1526-5900(02)65013-8. [DOI] [PubMed] [Google Scholar]
- 7.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;299(1):70–78. doi: 10.1001/jama.2007.64. [DOI] [PubMed] [Google Scholar]
- 8.Goyal MK, Kuppermann N, Cleary SD, Teach SJ, Chamberlain JM. Racial Disparities in Pain Management of Children with Appendicitis in Emergency Departments. JAMA Pediatr. 2015;169(11):996–1002. doi: 10.1001/jamapediatrics.2015.1915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.James CA, Bourgeois FT, Shannon MW. Association of race/ethnicity with emergency department wait times. Pediatrics. 2005;115(3):e310–e315. doi: 10.1542/peds.2004-1541. [DOI] [PubMed] [Google Scholar]
- 10.Caperell K, Pitetti R, Cross KP. Race and acute abdominal pain in a pediatric emergency department. Pediatrics. 2013;131(6):1098–1106. doi: 10.1542/peds.2012-3672. [DOI] [PubMed] [Google Scholar]
- 11.Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Report. 2009;11:1–25. [PubMed] [Google Scholar]
- 12.Beauregard L, Pomp A, Choiniere M. Severity and impact of pain after day-surgery. Can J Anaesth. 1998;45:304–311. doi: 10.1007/BF03012019. [DOI] [PubMed] [Google Scholar]
- 13.Chung F, Ritchie E, Su J. Postoperative pain in ambulatory surgery. Anesth Analg. 1997;85:808–816. doi: 10.1097/00000539-199710000-00017. [DOI] [PubMed] [Google Scholar]
- 14.Coda BA. Opioids. In: Barash PG, Cullen BF, Stoelting RK, editors. Clinical anesthesia. 5. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. pp. 353–83. [Google Scholar]
- 15.Jimenez N, Seidel K, Martin LD, Rivara FP, Lynn AM. Perioperative analgesic treatment in Latino and non-Latino pediatric patients. J Health Care Poor Underserved. 2010;21(1):229–36. doi: 10.1353/hpu.0.0236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rabbitts JA, Groenewald CB, Räsänen J. Geographic differences in perioperative opioid administration in children. Paediatr Anaesth. 2012;22(7):676–81. doi: 10.1111/j.1460-9592.2012.03806.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hosmer DW, Hosmer T, Le Cessie S, Lemeshow S. A comparison of goodness-of-fit tests for the logistic regression model. Stat Med. 1997;16(9):965–980. doi: 10.1002/(sici)1097-0258(19970515)16:9<965::aid-sim509>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 18.Warnock F, Lander J. Pain progression, intensity and outcomes following tonsillectomy. Pain. 1998;75:37–45. doi: 10.1016/S0304-3959(97)00202-9. [DOI] [PubMed] [Google Scholar]
- 19.Svensson I, Sjostrom B, Haljamae H. Influence of expectations and actual pain experiences on satisfaction with postoperative pain management. Eur J Pain. 2001;5:125–133. doi: 10.1053/eujp.2001.0227. [DOI] [PubMed] [Google Scholar]
- 20.Beauregard L, Pomp A, Choiniere M. Severity and impact of pain after day-surgery. Can J Anaesth. 1998;45:304–311. doi: 10.1007/BF03012019. [DOI] [PubMed] [Google Scholar]
- 21.Phillips DM. JCAHO pain management standards are unveiled. Joint Commission on Accreditation of Healthcare Organizations. JAMA. 2000;284(4):428–429. doi: 10.1001/jama.284.4.423b. [DOI] [PubMed] [Google Scholar]
- 22.U.S. Department of Health and Human Services. Office of Disease Prevention and Health Promotion, Healthy People, 2020. Washington, DC: 2014. [Accessed 02/29/2016]. Available at http://www.healthypeople.gov/2020/ [Google Scholar]
- 23.Sadhasivam S, Chidambaran V, Ngamprasertwong P, Esslinger HR, Prows C, Zhang X, Martin LJ, McAuliffe J. Race and unequal burden of perioperative pain and opioid related adverse effects in children. Pediatrics. 2012;129(5):832–8. doi: 10.1542/peds.2011-2607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Singhal A, Tien YY, Hsia RY. Racial-Ethnic Disparities in Opioid Prescriptions at Emergency Department Visits for Conditions Commonly Associated with Prescription Drug Abuse. PLoS One. 2016;11(8):e0159224. doi: 10.1371/journal.pone.0159224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhou HH, Sheller JR, Nu H, Wood M, Wood AJ. Ethnic differences in response to morphine. Clin Pharmacol Ther. 1993;54(5):507–513. doi: 10.1038/clpt.1993.182. [DOI] [PubMed] [Google Scholar]
- 26.Avenanti A, Sirigu A, Aglioti SM. Racial bias reduces empathic sensorimotor resonance with other-race pain. Curr Biol. 2010;20(11):1018–1022. doi: 10.1016/j.cub.2010.03.071. [DOI] [PubMed] [Google Scholar]
- 27.Seago JA, Weitz S, Walczak S. Factors influencing stay in the postanesthesia care unit: a prospective analysis. J Clin Anesth. 1998;10(7):579–87. doi: 10.1016/s0952-8180(98)00084-1. [DOI] [PubMed] [Google Scholar]
- 28.Edler AA, Mariano ER, Golianu B, Kuan C, Pentcheva K. An analysis of factors influencing postanesthesia recovery after pediatric ambulatory tonsillectomy and adenoidectomy. Anesth Analg. 2007;104(4):784–9. doi: 10.1213/01.ane.0000258771.53068.09. [DOI] [PubMed] [Google Scholar]
- 29.Memtsoudis SG, Poeran J, Zubizarreta N, Rasul R, Opperer M, Mazumdar M. Anesthetic Care for Orthopedic Patients: Is There a Potential for Differences in Care? Anesthesiology. 2016;124(3):608–23. doi: 10.1097/ALN.0000000000001004. [DOI] [PubMed] [Google Scholar]


