Abstract
The intense pulsed light (IPL) and laser technologies are widely used for skin rejuvenation and for treating several dermatological disorders such as skin dyschromia and acne, and for non-ablative dermal remodeling of rhytides and hypertrophic scars. Technological evolution is rapid. The High Power Pulsed Light™ [HPPL™] and Incoherent Fast Light™ technologies [IFL™, Novavision Group S.p.A., 20826 Misinto (MB), Italy] are recent innovations in the field of IPL technologies; IFL™ is a further evolution of the already advanced HPPL™ system. The paper presents a selection of case histories of dermatological lesions treated with the HPPL™ and IFL™ technologies. All study materials were appropriately peer-reviewed for ethical problems.
Key words: Photorejuvenation, photoaging, intense pulsed light, dermal remodeling
Competing interest statement
Conflict of interest: the authors declare no potential conflict of interest.
The wide potential of intense pulsed light in dermatology
As in photoepilation, melanin is the target chromophore in the treatment of melanocytic and Becker’s nevi, lentigines and lentigo solaris, café-au-lait birthmarks and other variably pigmented lesions, of course taking care to adjust light fluency to the intensity of pigmentation.1
The selective thermolysis concept leading to irreversible thermal damage to chromophores in skin structures has also been applied to other fields of aesthetic dermatology besides photoepilation. The first intense pulsed light (IPL) medical device to treat benign hemangiomatous malformations, introduced in 1994, leveraged the selective absorption of light energy by oxyhemoglobin to target the abnormal skin blood vessels. Lesions at depths of up to 1.2 cm could be effectively treated with wavelengths of more than 590 nm, fluence between 40 and 70 J/cm², and relatively long pulses; more superficial vessels could be targeted with shorter multiple pulses and lower levels of fluence.2 Because IPL is often successful when pulsed dye lasers fail, it should be considered the gold standard in the everyday treatment of vascular lesions such as telangiectasia and port-wine stains.3,4
The scope for visible and near-infrared light therapy in dermatology goes beyond melanin-targeted selective thermolysis. Another biological effect of these wavelengths is non-ablative dermal remodeling with increased collagen I deposition and collagen reorganization into parallel arrays of compact fibrils. Clinically and aestetically, the deposition of new dermal collagen translates into improved skin texture, more elasticity and more normal pigmentation, as seen in the treatment of rhytides and stretch marks.5,6
Non-ablative dermal remodeling avoids the postoperative complications that are almost unavoidable after the destruction of the epidermis and the dermal wounds induced by ablative techniques such as dermabrasion, chemical peels, and char-free pulsed CO2 and erbium:yttrium-aluminiumgarnet lasers. Such complications include oozing, bleeding, infections, post-inflammatory pigmentary changes and the waste of time while waiting for the skin to reepithelialise.5
In 1997, the first attempt at non-ablative dermal remodeling to improve periorbital, perioral and forehead rhytides used a 1064-nm Q-switched neodymium:YAG laser; over the years pulsed dye and potassiumtitanyl-phosphate (KTP) green-light lasers joined the race for skin photorejuvenation.5,6 Pulsed dye lasers are widely used in spite of the frequent problem of cosmetically unacceptable purpura, especially when used with shorter pulse durations.5,6
IPL is also very useful against inflammatory acne. IPL targets the main mechanism at the basis of acne, the increased sebum secretion rate, thanks to photothermolysis of the blood vessels that supply the sebaceous glands. Absorption of IPL energy by the porphyrins produced by Propionibacterium acnes also generates oxygen radicals that destroy the pro-inflammatory microorganism proliferating in the sebum-rich follicle.
More focus on intense pulsed light in aging and photodamaged skin
IPL with filters to block shorter wavelengths first showed in 2000 both clinical and histologic evidence of new collagen formation.6,7 Dermal dendritic cells are the most likely biological target in IPL skin rejuvenation. This is suggested by the dendritic expression of the heat-induced protein hsp70 (Heat Shock Protein 70 kilodaltons) and pro-collagen 1 as markers of cell activation, the first event that is thought to lead to new collagen deposition by dermal fibroblasts.7
As in other aesthetic dermatology indications, also in rejuvenation of aging and photoaging skin IPL enjoys many advantages over the laser devices currently available: economy, robust technology, ease of treatment of large skin areas and, most importantly, the ability to target both melanin and hemoglobin thanks to wavelength versatility (Figure 1).8,9 The word photorejuvenation was indeed coined to describe the double improvement with IPL in both dyspigmentation and altered vascularity of photoaging skin.9
Figure 1.
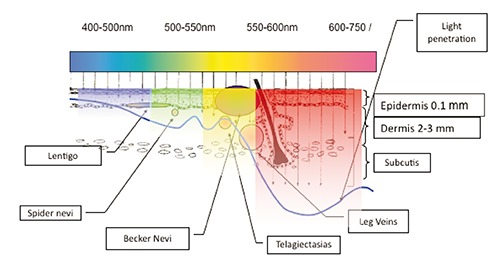
Relationship between the penetration of IPL wavelengths in the epidermis, dermis and subcutis, marked by the blue line, and the depth and type of some pigmentary and vascular lesions amenable to IPL phototherapy.
This explains another (psychological but useful) advantage of IPL appreciated by many patients with photodamaged skin: the perception of strong improvement due to decreases in altered pigmentation and telangiectasia, both apparent to the patient and more easily detected than the milder changes in rhytides.9 Pre-treatment with 5-aminolevulinic acid (5-ALA) may further enhance the pigmentary, vascular and wrinkle improvements.9
The double action of IPL on vasculature and pigmentation is also thought to explain its efficacy in improving the appearance and/or symptoms of hypertrophic scars and keloids. Functional modification of keloid fibroblasts is also likely to have a role.10,11
A collection of some skin rejuvenation and dermatological phototherapy case histories is herein presented. They have been collected over the last years by the main author in his everyday hospital and plastic dermatology private practice using IPL devices based on the HPPL™ and IFL™ technologies.
Clinical outcomes of second-generation intense pulsed light technologies
Figure 2 illustrates the rapid improvement of clinically severe stretch marks of the thigh after IPL biostimulation of new collagen deposition supplemented by peeling; inflammation was also rapidly relieved.
Figure 2.

Improvement of thigh stretch marks after 1 and 2 weeks of biostimulation (red and near-infrared wavelengths) supplemented by peeling.
The production and deposition of new dermal collagen after HPPL™/IFL™ biostimulation is also at the basis of phototherapy of rhytides as well as rejuvenation of aging or photodamaged skin and atrophic skin. Figures 3 shows the aesthetic outcome with periocular rhytides after four HPPL™/IFL™ sessions; Figures 4 the rapid improvement of skin texture after four sessions of HPPL™/IFL™ skin rejuvenation and six weeks of follow-up; Figure 5 the dramatic long-term improvement of dermal atrophy in a patient with severely excoriated acne as result of repeated picking at skin inflammatory blemishes. As regards inflammatory acne, it is another ideal target for IPL phototherapy, thanks to reduced sebum production and density of comedones and, at the same time, control of skin inflammatory lesions (Figure 6).
Figure 3.
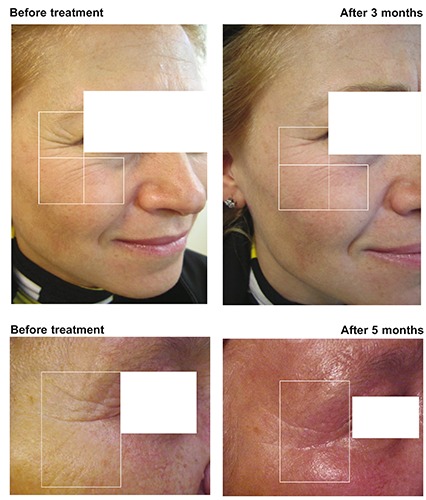
Periocular rhytides after 5 weekly sessions of HPPL™/IFL™ biostimulation. Top: single flash, 45 J, 40 msec, cut-off filter 520 nm; below: single flash (2 passages), 35-40 J, 35 msec, cut-off filters 520 and 590 nm.
Figure 4.

Non-ablative HPPL™/IFL™ photorejuvenation, 4 weekly treatments. Top: aesthetic outcome of basal abdominal skin laxity after 6 weeks; below: improvement of skin texture leading to more compact skin (microphotographs, X50).
Figure 5.

Improvement of dermal atrophy in an adolescent girl with excoriated acne, monthly HPPL™/IFL™ treatment, 5 sessions. Settings: 3 single-flash passages, 35-45 msec, 30-55 J; cut-off filters at different passages, 520, 590 and 650 nm.
Figure 6.
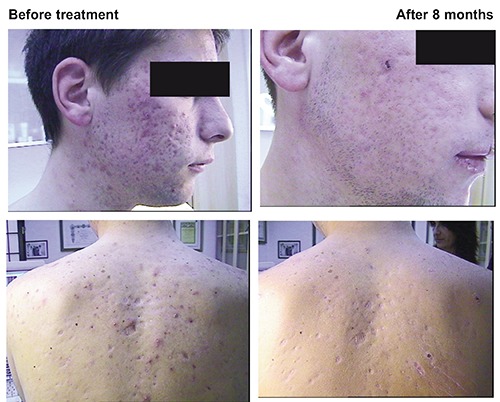
Acne phototherapy in adolescent male treated with oral isotretinoin, monthly HPPL™/IFL™ treatment, 5 sessions. Settings: 4 flashes per session, interval between flashes 400 msec, 15 J; cut-off filter 420 nm.
In the IFL™ technology, the latest evolution of HPPL™ devices, all wavelengths of the xenon flash lamp but those corresponding to the three energy emission peaks (700, 800 and 890 nm) are filtered away electronically and by the built-in filter systems. Biostimulation with new collagen deposition and more orderly spatial disposition of elastin and collagen dermal fibers are the likely mechanism leading to improvement of skin texture after only 6 weeks (Figure 7). The new IFL™ technology is effective not only in improving the appearance of hypertrophic scars and keloids regardless of their origin, but also in reducing the height, redness, and hardness of scars (Figure 8). As conclusion, Figure 9 shows the efficacy of six IFL™ biweekly sessions on highly inflammatory acne in a young woman intolerant to the usual therapies for severely inflammatory forms of the skin disorder.
Figure 7.

Improvement of skin texture, 1 treatment per week for 6 weeks; follow-up: 3 months. IFL™ settings: 45-msec flash, 50 J; cut-off filter 520 nm.
Figure 8.

Phototherapy of hypertrophic scar. IFL™ settings: 5 flashes, repeated 4-5 times per session, interval between flashes 400 msec, 20 J; cut-off filter 590 nm. Concomitant therapy: infiltration of steroids.
Figure 9.

Improvement of thigh stretch marks after 1 and 2 weeks of biostimulation (red and near-infrared wavelengths) supplemented by peeling.
References
- 1.Bjerring P, Christiansen K. Intense pulsed light source for treatment of small melanocytic nevi and solar lentigines. J Cutan Laser Ther 2000;2:177-81. [DOI] [PubMed] [Google Scholar]
- 2.Goldman MP. Treatment of benign vascular lesions with the Photoderm VL high-intensity pulsed light source. Adv Dermatol 1997;13:503-21. [PubMed] [Google Scholar]
- 3.Tanghetti EA. Split-face randomized treatment of facial telangiectasia comparing pulsed dye laser and an intense pulsed light handpiece. Lasers Surg Med 2012;44:97-102. [DOI] [PubMed] [Google Scholar]
- 4.Bjerring P, Christiansen K, Troilius A. Intense pulsed light source for the treatment of dye laser resistant port-wine stains. J Cosmet Laser Ther 2003;5:7-13. [PubMed] [Google Scholar]
- 5.Goldberg DJ, Cutler KB. Nonablative treatment of rhytids with intense pulsed light. Lasers Surg Med 2000;26:196-200. [DOI] [PubMed] [Google Scholar]
- 6.Goldberg DJ. New collagen formation after dermal remodeling with an intense pulsed light source. J Cutan Laser Ther 2000;2:59-61. [DOI] [PubMed] [Google Scholar]
- 7.Prieto VG, Diwan AH, Shea CR, et al. Effects of intense pulsed light and the 1,064 nm Nd:YAG laser on sun-damaged human skin: histologic and immunohistochemical analysis. Dermatol Surg 2005;31:522-5. [DOI] [PubMed] [Google Scholar]
- 8.Babilas P, Schreml S, Szeimies RM, Landthaler M. Intense pulsed light (IPL): a review. Lasers Surg Med 2010;42:93-104. [DOI] [PubMed] [Google Scholar]
- 9.Alexiades-Armenakas MR, Dover JS, Arndt KA. The spectrum of laser skin resurfacing: nonablative, fractional, and ablative laser resurfacing. J Am Acad Dermatol 2008;58:719-37. [DOI] [PubMed] [Google Scholar]
- 10.Kontoes PP, Marayiannis KV, Vlachos SP. The use of intense pulsed light in the treatment of scars. Eur J Plastic Surg 2003;25:374-7. [DOI] [PubMed] [Google Scholar]
- 11.Mamalis AD, Lev-Tov H, Nguyen DH, Jagdeo JR. Laser and light-based treatment of keloids-a review. J Eur Acad Dermatol Venereol 2014;28:689-99. [DOI] [PMC free article] [PubMed] [Google Scholar]


