Abstract
Rationale: Pulmonologists frequently encounter indeterminate pulmonary nodules in practice, but it is unclear what clinical factors they rely on to guide the diagnostic evaluation.
Objectives: To assess the current approach to the management of indeterminate pulmonary nodules and to determine the extent to which the addition of a hypothetical diagnostic blood test will influence clinical decision making.
Methods: Selected pulmonologists practicing in the United States were invited to participate in a conjoint exercise based on 20 randomly generated cases of varying age, smoking history, and nodule size. Some cases included the result of a hypothetical blood test. Each respondent chose from among three diagnostic options for a patient: noninvasive monitoring (i.e., serial CT or positron emission tomography scan), a minor procedure (i.e., biopsy or bronchoscopy), or a major procedure (i.e., video-assisted thorascopic surgery or thoracotomy). Multivariate logistic regression was used to assess the impact of the three risk factors and the diagnostic blood test on decision making.
Measurements and Main Results: Four hundred nineteen physicians participated (response rate, 10%). One hundred fifty-three physician surveys met predetermined criteria and were analyzed (4% of all invitees). A diagnostic procedure was recommended for 23% of 6-mm nodules, versus 54, 66, 77, and 84% of nodules 10, 14, 18, and 22 mm, respectively (P < 0.001). Older age limited recommendations for invasive testing: 54% of 80-year-olds versus 61, 64, 63, and 61% of patients 71, 62, 53, and 44 years of age, respectively (P < 0.001). In multivariate analyses, nodule size, smoking history, age, and the blood test each influenced decision making (P < 0.001).
Conclusions: The pulmonologists who participated in this survey were more likely to proceed with invasive testing, instead of observation or additional imaging, as the size of the nodule increased. The use of a hypothetical blood test resulted in significant alterations in the decision to pursue invasive testing.
Keywords: solitary pulmonary nodule, lung neoplasms, decision making
An indeterminate pulmonary nodule is a small, focal opacity in the lung measuring up to 3 cm that does not have features strongly suggestive of a benign etiology (1, 2). Among patients with indeterminate nodules identified by CT scan, steps in the evaluation may include further serial CT surveillance, characterization with fluorodeoxyglucose positron emission tomography, nonsurgical biopsy, or surgical resection (3). Quantitative models have shown that the most important predictors of malignancy include nodule size and appearance, patient age, and smoking history (4–9). Although these clinical and radiographic risk factors for malignancy are well described, little is known about how physicians use these clinical factors to choose the most appropriate management strategy for an individual patient.
Although the primary clinical risk factors influencing decision making are known, there is considerable uncertainty associated with the evaluation of indeterminate nodules. Benign disease is identified in 10 to 55% of patients undergoing surgical evaluation of indeterminate nodules (10–16). Alternatively, a strategy of serial noninvasive imaging can cause significant anxiety (17–19) and may result in tumor growth before a cancer diagnosis. Given the diagnostic uncertainty that exists with current management strategies for indeterminate nodules, current research efforts are focused on identifying noninvasive biomarkers with the potential to aid and direct physician management decisions.
Conjoint analysis and discrete choice experiments are stated preference techniques that allow for quantitative assessment of decision making (20–22). Discrete choice experiments use a choice experiment technique whereby key attributes of sample cases are varied, with subsequent evaluation of variation in the respondents’ choices in relation to these attributes (20–22). We used conjoint analysis to identify factors that drive physician decision making in the evaluation of indeterminate lung nodules.
Some of the results of these studies have been previously reported in the form of an abstract (23).
Methods
Survey Instrument Design and Administration
Standard conjoint analysis methodology was used to design, implement, and analyze the web-based survey (20–22). The three key factors identified (age, nodule size, and smoking history) were combined with a fourth factor, a hypothetical diagnostic blood test performed after nodule identification, to create 400 case scenarios by using a fractional factorial design (Table 1). The blood test was described as a “rule-out” test with a negative predictive value of 95% and a positive predictive value of 50%. Respondents were told that a “low-risk” result indicated that a patient’s lung nodule had a 95 out of 100 likelihood of being benign, and a “high-risk” result indicated that a patient’s nodule had a 50% likelihood of being benign.
Table 1.
Attributes and levels used in case scenarios
| Attributes | Levels |
||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| Age, yr | 44 | 53 | 62 | 71 | 80 |
| Smoking history, pack-years | 0 | 12 | 24 | 36 | NA |
| Nodule size, mm | 6 | 10 | 14 | 18 | 22 |
| Hypothetical test | No test | High risk | Low risk | Indeterminate risk | |
Definition of abbreviation: NA = not applicable.
A subset of 16 randomly selected cases and 4 fixed cases were chosen for each participant. Respondents were asked to assume that the patient in all case scenarios was asymptomatic and a surgical candidate. In the final survey, each respondent was asked to choose from among three diagnostic options for a patient: noninvasive monitoring only (i.e., serial CT or positron emission tomography scan), a minimally invasive procedure (i.e., biopsy/fine needle aspiration or bronchoscopy), or a major invasive procedure (i.e., video-assisted thorascopic surgery or thoracotomy). No specific information on expected complication rates from these procedures was provided.
The survey was administered between October 4, 2012 and October 22, 2012 to pulmonary physicians, excluding other specialties. Potential respondents were identified by M3 Global Research using a proprietary database, including a panel of more than 1.7 million verified, worldwide physicians differentiated into more than 700 subspecialties (24). Prespecified eligibility criteria, self-reported by respondents, identified clinicians experienced in caring for patients with indeterminate lung nodules and included: board certification or board eligible; 3 to 25 years practice experience; at least 75% of time spent in direct clinical care; at least 50 patients seen monthly, including at least 10 for pulmonary nodules and at least 5 patients with a newly identified nodule; and no prior association with lung nodule diagnostic product development. Geographic quotas were used to ensure site diversity, with a goal of equal numbers of respondents from six regions (Northeast, Midwest, South Atlantic, South Central, Mountain, and Pacific). Once the quota for a region was reached, all subsequent respondents from that region were excluded from participation in the survey; no responses were recorded for these subjects. Each pulmonologist received $60 as compensation for participating. Further details on the survey are available in the online supplement. This study was approved by the University of Pennsylvania Institutional Review Board.
Statistical Analysis
Responses to the case scenarios were analyzed by using a modified Poisson regression model with robust variance estimates (25), yielding risk ratios for the probability of choosing a major or minor diagnostic procedure compared with the choice of noninvasive monitoring. Models were developed separately for case scenarios with all four variables as well as those that did not include the hypothetical blood test. All statistical tests were two-sided, and a P value < 0.05 was considered significant. Statistical analyses were performed with SAS/STAT (Version 9.2).
Results
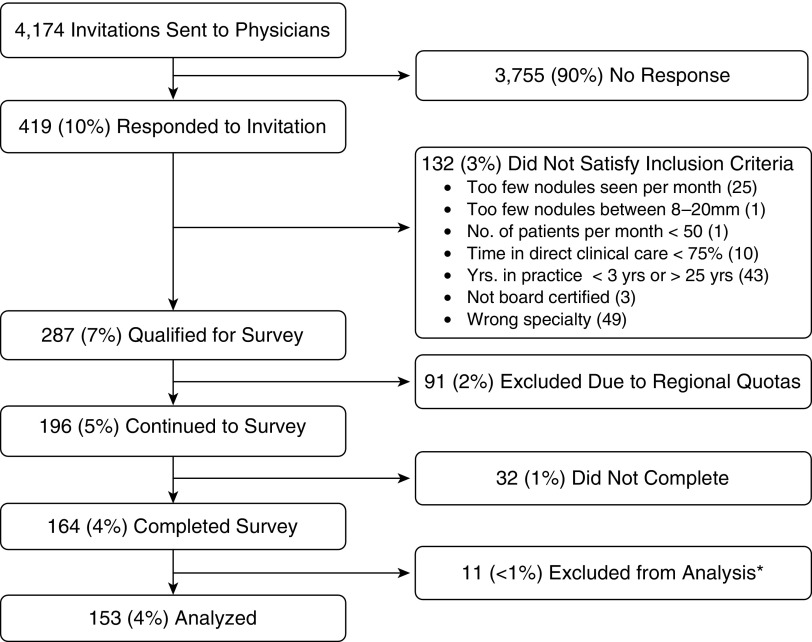
A total of 4,174 invitations were sent electronically, with 419 physicians responding (response rate, 10%; Figure 1). Due to various exclusion criteria and regional quotas, a total of 153 eligible and complete responses were analyzed (Table 2). A total of 2,448 completed scenarios were available for analysis. Of these, 1,861 scenarios included four variables, the three clinical factors and the hypothetical test, whereas the remaining 587 scenarios included only the three clinical risk factors.
Figure 1.
Selection of survey participants. A total of 419 participants responded to the survey. One hundred fifty-three eligible and complete responses were analyzed. *Nine physician respondents indicated that they would never use the diagnostic test (data not presented). An additional two respondents were excluded from the analysis due to suspicion of survey speeding.
Table 2.
Characteristics of physician respondents
| Physician/Practice Characteristic (N = 153) | Value |
|---|---|
| Responding physician characteristics | |
| Yr in practice, mean (SD) | 14 (±6.7) |
| Percent of time spent in direct clinical care, mean (SD) | 94 (±7.3) |
| Practice characteristics | |
| No. of physicians in practice, mean (SD)* | 43 (±112.3) |
| No. of pulmonologists in practice, mean (SD) | 6 (±5.2) |
| No. of pulmonologist by region, n (%) | |
| Northeast | 36 (23.5) |
| Midwest | 31 (20.3) |
| South Atlantic | 32 (20.9) |
| South Central | 20 (13.1) |
| Mountain | 9 (5.9) |
| Pacific | 25 (16.3) |
| Hospital affiliation, n (%)† | |
| Academic medical center | 43 (28.1) |
| Community teaching hospital | 59 (38.6) |
| Community (nonteaching) hospital | 58 (37.9) |
| Other‡ | 3 (2.0) |
| No. of beds in primary hospital affiliation, mean (SD) | |
| Academic medical center | 505 (±235.0) |
| Community teaching hospital | 409 (±218.8) |
| Community (nonteaching) hospital | 304 (±160.2) |
| Patient population characteristics | |
| No. of patients seen per mo, mean (SD) | 344 (±145.6) |
| No. of patients with pulmonary nodules per mo, mean (SD) | 58 (±51.6) |
| No. of patients with newly identified pulmonary nodules per mo, mean (SD) | 28 (±23.3) |
One respondent reported 999 physicians in practice, and response could not be verified.
Respondents may be affiliated with more than one hospital type.
Other hospital types included long-term acute care hospital, Veterans Affairs medical center, and military teaching hospital.
Across all scenarios, an invasive evaluation was recommended for 60%, with 42% undergoing a minor procedure and 18% undergoing a major procedure. There was a strong association between nodule size and the decision to pursue an invasive diagnostic evaluation, with recommendations for invasive testing in 23, 54, 66, 77, and 84% of 6-, 10-, 14-, 18-, and 22-mm nodules, respectively (P < 0.001). Physicians were also more likely to recommend invasive testing in scenarios with greater overall tobacco use. Despite respondents being told that all patients were surgical candidates, older age limited recommendations for invasive procedures: 54% of 80-year-olds versus 61, 64, 63, and 61% of ages 71, 62, 53, and 44 years, respectively (P < 0.001). Finally, the hypothetical blood test also impacted the recommendations for invasive procedures: 86% of patients with a high-risk result were referred for invasive testing, compared with 48% with an intermediate result and 26% with a low-risk result.
In multiple regression, nodule size, age, smoking history, and the blood test were significant factors influencing the choice between invasive evaluation and noninvasive imaging (Table 3). Nodule size remained the dominant factor impacting choice of invasive testing, with an increased risk of invasive testing seen in scenarios with lesions 14, 18, and 22 mm in diameter compared with nodules 10 mm in size. Scenarios with 6-mm nodules were significantly less likely to receive a recommendation for invasive evaluation. The oldest age group (80 yr) also remained an independent predictor of less-invasive testing.
Table 3.
Association of clinical variables with invasive procedures
| Multivariate Model | ||
|---|---|---|
| Predictor Variable | Minor or Major Procedure | |
| Risk Ratio | 95% CI | |
| Age, yr | ||
| 44 | 0.97 | 0.94, 0.99 |
| 53 | 0.99 | 0.96, 1.02 |
| 62 | Ref. | — |
| 71 | 0.98 | 0.95, 1.00 |
| 80 | 0.91 | 0.88, 0.94 |
| Smoking history, pack-years | ||
| 0 | Ref. | — |
| 12 | 1.13 | 1.10, 1.16 |
| 24 | 1.14 | 1.11, 1.17 |
| 36 | 1.17 | 1.14, 1.20 |
| Nodule size, mm | ||
| 6 | 0.79 | 0.77, 0.82 |
| 10 | Ref. | — |
| 14 | 1.07 | 1.04, 1.10 |
| 18 | 1.16 | 1.12, 1.19 |
| 22 | 1.20 | 1.16, 1.23 |
| Hypothetical test | ||
| No test | Ref. | — |
| Low risk | 0.91 | 0.89, 0.94 |
| Indeterminate | 1.07 | 1.04, 1.10 |
| High risk | 1.21 | 1.18, 1.25 |
Definition of abbreviation: CI = confidence interval; Ref = reference.
To further evaluate the impact of the three clinical risk factors, and to exclude the effect of the hypothetical test on the observed effects, we performed an additional regression analysis using scenarios that included only nodule size, age, and tobacco use (n = 587). The impact of these three factors on recommendations for invasive testing remained similar to effects seen in the full model (Table 4).
Table 4.
Association of clinical variables with invasive procedures (model limited to age, smoking history and nodule size)
| Multivariate Model | ||
|---|---|---|
| Predictor Variable | Minor or Major Procedure | |
| Risk Ratio | 95% CI | |
| Age, yr | ||
| 44 | 0.98 | 0.91, 1.05 |
| 53 | 1.03 | 0.97, 1.09 |
| 62 | Ref. | — |
| 71 | 0.96 | 0.91, 1.02 |
| 80 | 0.95 | 0.89, 1.01 |
| Smoking history, pack-years | ||
| 0 | Ref. | — |
| 12 | 1.17 | 1.10, 1.25 |
| 24 | 1.19 | 1.12, 1.27 |
| 36 | 1.22 | 1.15, 1.30 |
| Nodule size, mm | ||
| 6 | 0.79 | 0.74, 0.85 |
| 10 | Ref. | — |
| 14 | 1.13 | 1.06, 1.21 |
| 18 | 1.23 | 1.14, 1.31 |
| 22 | 1.24 | 1.16, 1.34 |
Definition of abbreviation: CI = confidence interval; Ref = reference.
Discussion
To our knowledge, this is the first study to quantitatively assess decision making for indeterminate pulmonary nodules by a geographically diverse group of experienced pulmonologists. This study using standardized scenarios incorporating various levels of key clinical variables in lung nodule management allowed us to identify the factors that were most relevant to physician decision making. This study has three important findings. First, the factors most associated with the decision to pursue invasive testing are, as expected, based on patient age, history of smoking, and the size of the nodule. Second, these factors are not sufficient for decision making, as we found that the addition of a diagnostic blood test would strongly and independently affect management decisions. In scenarios including the test, decision making based on the results followed a predictable pattern—a high-risk result led to more frequent recommendations for invasive testing and a low-risk result led to less invasive testing at all levels of nodule size. Finally, despite being told that all patients regardless of age were surgical candidates, pulmonologists were less likely to recommend invasive procedures in older patients.
The risk of lung cancer for an indeterminate nodule is known to increase with nodule size, greater tobacco use, and increased patient age. Specifically, for nodule size, studies have shown that lesions measuring more than 20 mm in size have a risk of malignancy ranging from 30 to 82% (26–28). Our analysis suggests that pulmonologists appropriately use nodule size as the dominant factor in decision making for individuals with indeterminate-sized lesions. For example, an invasive evaluation for the largest sized nodules (i.e., 22 mm) was recommended in 84% of scenarios, compared with lower rates for smaller lesions.
There were two important areas in which recommendations for testing were not well aligned with current guidelines. First, invasive testing was recommended for 23% of patients with a 6-mm nodule. However, the risk of malignancy in subcentimeter nodules ranges from less than 1% for lesions less than or equal to 6 mm to less than 2% for nodules between 7 and 10 mm (28). Given this level of risk and the high likelihood of nondiagnostic results from either bronchoscopy or transthoracic needle aspiration, current guidelines recommend a strategy of serial imaging as the primary management strategy for nodules less than 8 mm in size (3, 29). In this study, the rate of invasive testing is far higher than what is likely to be clinically appropriate given the low risk of lung cancer in nodules of this size. The use of unneeded procedures has also been demonstrated in a recent Veterans Affairs–based study assessing lung nodule evaluation in the usual care setting (30).
The second area where respondents’ recommendations did not align with current guidelines was the approach to elderly patients, particularly octogenarians. Patients in this age group were approximately half as likely to undergo invasive testing when compared with 62-year-old patients, after controlling for smoking and nodule size. There are many potential reasons for this result. Although the study instructions explicitly noted that all patients should be considered as surgical candidates, some respondents may have assumed a greater risk of invasive testing in patients within this age group. Guidelines recommend against using age alone as a criterion to deny resection in those otherwise fit to undergo the procedure (3). That this study found such a disparity in recommendations for invasive testing in older patients suggests the possibility of ageism—a form of bias characterized by discrimination against individuals based on their age. Chronologic age has been shown to significantly influence treatment decisions in a wide range of clinical scenarios, and our findings suggest that this disparity may exist for patients with indeterminate lung nodules.
Our study had a number of important limitations. Although standardization allows for isolation of relevant factors for decision making, this approach does not measure actual physician behavior in practice. For example, the choice of diagnostic approach is likely to be influenced by other practitioners, including thoracic surgeons and radiologists, as well as individual patient preferences regarding acceptance of invasive procedures. Second, the choice of diagnostic approach is also likely to be influenced by multiple other clinical variables, including nodule location, degree of emphysema, level of experience with advanced diagnostic approaches (e.g., navigational bronchoscopy), and access to thoracic surgery services. Finally, our overall response rate was 10%, with only 4% included in the analysis, which raises the question of whether our sample is representative of pulmonologists in general who care for patients with lung nodules. The reduced number of surveys included in our analysis was partly due to the prespecified requirement that our study sample represent a geographically diverse population of physicians. Because we did not know the characteristics of the nonrespondents, we were not able to evaluate whether the study participants were representative of all pulmonologists.
In conclusion, for United States pulmonologists who participated in this e-mail survey, the choice of diagnostic strategy for indeterminate nodules varied, but it was largely driven by the size of the lesion and was significantly impacted by patient age and smoking history. Physicians also seemed willing to use an informative noninvasive test that provides additional diagnostic information. However, our results also found evidence of inappropriately aggressive strategies for some small nodules and evidence for ageism among older patients with indeterminate lesions. Future discrete choice experiments should consider inclusion of more complex scenarios, including incorporation of patient preferences. Further investigations to examine the appropriateness of real-world decision making are also warranted.
Additional material
Supplementary data supplied by authors.
Footnotes
Supported by Integrated Diagnostics, Inc.
Author Contributions: Study concept and design: A.V., N.T.T., J.A., C.M., P.K., K.C.F., G.S., and G.B.D. Acquisition of data: J.A., C.M., and K.C.F. Analysis and interpretation of data: A.V., N.T.T., C.M., P.K., K.C.F., G.S., and G.B.D. Drafting of the manuscript: A.V., N.T.T., J.A., C.M., G.S., and G.B.D. Critical revision of the manuscript for important intellectual content: A.V., N.T.T., J.A., C.M., P.K., K.C.F., G.S., and G.B.D.
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Ost D, Fein AM, Feinsilver SH. Clinical practice: the solitary pulmonary nodule. N Engl J Med. 2003;348:2535–2542. doi: 10.1056/NEJMcp012290. [DOI] [PubMed] [Google Scholar]
- 2.Tuddenham WJ. Glossary of terms for thoracic radiology: recommendations of the Nomenclature Committee of the Fleischner Society. AJR Am J Roentgenol. 1984;143:509–517. doi: 10.2214/ajr.143.3.509. [DOI] [PubMed] [Google Scholar]
- 3.Gould MK, Donington J, Lynch WR, Mazzone PJ, Midthun DE, Naidich DP, Wiener RS.Evaluation of individuals with pulmonary nodules: when is it lung cancer? Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelinesChest 2013143e93S–e120S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cummings SR, Lillington GA, Richard RJ. Estimating the probability of malignancy in solitary pulmonary nodules: a Bayesian approach. Am Rev Respir Dis. 1986;134:449–452. doi: 10.1164/arrd.1986.134.3.449. [DOI] [PubMed] [Google Scholar]
- 5.Gould MK, Ananth L, Barnett PG Veterans Affairs SNAP Cooperative Study Group. A clinical model to estimate the pretest probability of lung cancer in patients with solitary pulmonary nodules. Chest. 2007;131:383–388. doi: 10.1378/chest.06-1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gurney JW, Lyddon DM, McKay JA. Determining the likelihood of malignancy in solitary pulmonary nodules with Bayesian analysis: part II: application. Radiology. 1993;186:415–422. doi: 10.1148/radiology.186.2.8421744. [DOI] [PubMed] [Google Scholar]
- 7.May BJ, Levsky JM, Godelman A, Jain VR, Little BP, Mahadevia PS, Burton WB, Haramati LB. Should CT play a greater role in preventing the resection of granulomas in the era of PET? AJR Am J Roentgenol. 2011;196:795–800. doi: 10.2214/AJR.10.5190. [DOI] [PubMed] [Google Scholar]
- 8.Swensen SJ, Silverstein MD, Ilstrup DM, Schleck CD, Edell ES. The probability of malignancy in solitary pulmonary nodules: application to small radiologically indeterminate nodules. Arch Intern Med. 1997;157:849–855. [PubMed] [Google Scholar]
- 9.Yonemori K, Tateishi U, Uno H, Yonemori Y, Tsuta K, Takeuchi M, Matsuno Y, Fujiwara Y, Asamura H, Kusumoto M. Development and validation of diagnostic prediction model for solitary pulmonary nodules. Respirology. 2007;12:856–862. doi: 10.1111/j.1440-1843.2007.01158.x. [DOI] [PubMed] [Google Scholar]
- 10.Davies B, Ghosh S, Hopkinson D, Vaughan R, Rocco G. Solitary pulmonary nodules: pathological outcome of 150 consecutively resected lesions. Interact Cardiovasc Thorac Surg. 2005;4:18–20. doi: 10.1510/icvts.2004.091843. [DOI] [PubMed] [Google Scholar]
- 11.Grogan EL, Weinstein JJ, Deppen SA, Putnam JB, Jr, Nesbitt JC, Lambright ES, Walker RC, Dittus RS, Massion PP. Thoracic operations for pulmonary nodules are frequently not futile in patients with benign disease. J Thorac Oncol. 2011;6:1720–1725. doi: 10.1097/JTO.0b013e318226b48a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Isbell JM, Deppen S, Putnam JB, Jr, Nesbitt JC, Lambright ES, Dawes A, Massion PP, Speroff T, Jones DR, Grogan EL. Existing general population models inaccurately predict lung cancer risk in patients referred for surgical evaluation. Ann Thorac Surg. 2011;91:227–233, discussion 233. doi: 10.1016/j.athoracsur.2010.08.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aberle DR, Adams AM, Berg CD, Black WC, Clapp JD, Fagerstrom RM, Gareen IF, Gatsonis C, Marcus PM, Sicks JD National Lung Screening Trial Research Team. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395–409. doi: 10.1056/NEJMoa1102873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reed CE, Harpole DH, Posther KE, Woolson SL, Downey RJ, Meyers BF, Heelan RT, MacApinlac HA, Jung SH, Silvestri GA, et al. American College of Surgeons Oncology Group Z0050 trial. Results of the American College of Surgeons Oncology Group Z0050 trial: the utility of positron emission tomography in staging potentially operable non-small cell lung cancer. J Thorac Cardiovasc Surg. 2003;126:1943–1951. doi: 10.1016/j.jtcvs.2003.07.030. [DOI] [PubMed] [Google Scholar]
- 15.Smith MA, Battafarano RJ, Meyers BF, Zoole JB, Cooper JD, Patterson GA.Prevalence of benign disease in patients undergoing resection for suspected lung cancer Ann Thorac Surg 2006811824–1828.discussion 1828–1829 [DOI] [PubMed] [Google Scholar]
- 16.Stiles BM, Altes TA, Jones DR, Shen KR, Ailawadi G, Gay SB, Olazagasti J, Rehm PK, Daniel TM. Clinical experience with radiotracer-guided thoracoscopic biopsy of small, indeterminate lung nodules. Ann Thorac Surg. 2006;82:1191–1196, discussion 1196–1197. doi: 10.1016/j.athoracsur.2006.04.059. [DOI] [PubMed] [Google Scholar]
- 17.Slatore CG, Press N, Au DH, Curtis JR, Wiener RS, Ganzini L. What the heck is a “nodule”? A qualitative study of veterans with pulmonary nodules. Ann Am Thorac Soc. 2013;10:330–335. doi: 10.1513/AnnalsATS.201304-080OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wiener RS, Gould MK, Woloshin S, Schwartz LM, Clark JA. ‘The thing is not knowing’: patients’ perspectives on surveillance of an indeterminate pulmonary nodule. Health Expect. (In press). [DOI] [PMC free article] [PubMed]
- 19.Wiener RS, Gould MK, Woloshin S, Schwartz LM, Clark JA. What do you mean, a spot?: a qualitative analysis of patients’ reactions to discussions with their physicians about pulmonary nodules. Chest. 2013;143:672–677. doi: 10.1378/chest.12-1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bridges JF. Stated preference methods in health care evaluation: an emerging methodological paradigm in health economics. Appl Health Econ Health Policy. 2003;2:213–224. [PubMed] [Google Scholar]
- 21.Louviere JJ, Hensher DA, Swait JD. Cambridge, UK: Cambridge University Press; 2000. Stated choice methods: analysis and applications. [Google Scholar]
- 22.Ryan M, Farrar S. Using conjoint analysis to elicit preferences for health care. BMJ. 2000;320:1530–1533. doi: 10.1136/bmj.320.7248.1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vachani A, Tanner NT, Aggarwal J, Mathews C, Kearney P, Fang KC, Silvestri GA, Diette GB.The potential impact of a non-invasive diagnostic test on clinical decision-making for indeterminate pulmonary nodules [abstract] Am J Respir Crit Care Med 2014189:A6312 [Google Scholar]
- 24.M3 Global Research. M3 home page; 2014 [accessed 11 May 2014]. Available from: http://research.m3.com
- 25.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 26.Henschke CI, Yankelevitz DF, Mirtcheva R, McGuinness G, McCauley D, Miettinen OS, Group E ELCAP Group. CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol. 2002;178:1053–1057. doi: 10.2214/ajr.178.5.1781053. [DOI] [PubMed] [Google Scholar]
- 27.Takashima S, Sone S, Li F, Maruyama Y, Hasegawa M, Matsushita T, Takayama F, Kadoya M. Small solitary pulmonary nodules (< or =1 cm) detected at population-based CT screening for lung cancer: reliable high-resolution CT features of benign lesions. AJR Am J Roentgenol. 2003;180:955–964. doi: 10.2214/ajr.180.4.1800955. [DOI] [PubMed] [Google Scholar]
- 28.Church TR, Black WC, Aberle DR, Berg CD, Clingan KL, Duan F, Fagerstrom RM, Gareen IF, Gierada DS, Jones GC, et al. National Lung Screening Trial Research Team. Results of initial low-dose computed tomographic screening for lung cancer. N Engl J Med. 2013;368:1980–1991. doi: 10.1056/NEJMoa1209120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.MacMahon H, Austin JH, Gamsu G, Herold CJ, Jett JR, Naidich DP, Patz EF, Jr, Swensen SJ, Fleischner S Fleischner Society. Guidelines for management of small pulmonary nodules detected on CT scans: a statement from the Fleischner Society. Radiology. 2005;237:395–400. doi: 10.1148/radiol.2372041887. [DOI] [PubMed] [Google Scholar]
- 30.Wiener RS, Gould MK, Slatore CG, Fincke BG, Schwartz LM, Woloshin S. Resource use and guideline concordance in evaluation of pulmonary nodules for cancer: too much and too little care. JAMA Intern Med. 2014;174:871–880. doi: 10.1001/jamainternmed.2014.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.