Abstract
Background
The challenge of the primary prevention of cardiovascular disease (CVD) is to identify patients who would benefit from treatment with statins. Statins are currently prescribed to many patients, even those at a low 10-year risk of CVD. These latter patients may not be eligible for statins according to current guidelines.
Design
This study investigated the prescription of guideline-consistent (according to guidelines) and guideline-inconsistent (not according to guidelines) lipid-lowering treatment in primary prevention in a large contemporary Dutch cohort study (Lifelines).
Methods
Lifelines is a large cohort study from the Netherlands. Participants were recruited between 2006 and 2013. They completed questionnaires and underwent a physical examination. Participants with previous CVD were excluded. Statins and ezetimibe were grouped as statin treatment. The Dutch guideline on cardiovascular management was used to assess eligibility for statins.
Results
Of 147,785 participants, 7092 (4.8%) reported statin treatment. In 4667 (66%) participants, statin treatment was inconsistent with the Dutch guideline. A total of 78% of these participants had a low 10-year predicted CVD risk. Multivariable logistic regression analysis showed that female sex and smoking were strongly associated with guideline-inconsistent treatment. Interestingly, 65% of the these participants had low-density lipoprotein cholesterol levels above the 95th percentile, adjusted for age and sex, two or more major risk factors of CVD or a positive family history of premature CVD. Therefore treatment might be reasonable.
Conclusions
There is a large inconsistency between guideline recommendations and the prescription of statins in clinical practice in the Netherlands. This is especially true for patients with low CVD risk. Many of these patients probably had risk-increasing circumstances justifying treatment.
Keywords: Statin treatment, primary prevention, cohort study, low-risk patients, guidelines, cardiovascular disease, cardiovascular risk factors, lipids, overtreatment
Introduction
Cardiovascular disease (CVD) is the leading cause of death worldwide.1 Many prospective cohort studies have shown that high levels of low-density lipoprotein cholesterol (LDL-c) are a major risk factor for CVD. HMG-CoA reductase inhibitors (statins) reduce all-cause mortality and major vascular events by approximately 23% for each 1.0 mmol/l lowering of LDL-c.2 The challenge of statin treatment is the identification of patients who would benefit from treatment. Various guidelines have been developed to guide physicians.3 The Dutch guideline is comparable with international guidelines.4
Despite these guidelines, we have shown that 77% of patients without CVD who met the criteria for statin treatment in a large and representative cohort of the Dutch population did not receive lipid-lowering drugs.5 The prescription of statins to patients in the Netherlands who are not eligible for statin treatment according to guidelines may also be prevalent. Several previous cohort studies have shown a high frequency of guideline-inconsistent treatment, especially in low-risk patients.6–9 However, these studies were most often based on UK primary care records, involved relatively small numbers of patients, or did not focus on primary prevention.
The aim of this study was therefore to evaluate the proportion of guideline-inconsistent (statin treatment without guideline recommendation) and guideline-consistent treatment (statin treatment with guideline recommendation) in a primary prevention setting and to identify the factors associated with guideline-inconsistent statin treatment in a large sample of the Dutch population, the Lifelines cohort study.
Methods
Study design and participants
The Lifelines cohort study is a prospective population-based study of the three northern provinces of the Netherlands. Details of the design of the study have been published elsewhere.10 Participants were included in the study between 2006 and 2013. All general practitioners from the three northern provinces of the Netherlands were asked to invite patients aged between 25 and 50 years to participate in the Lifelines cohort study. For those who agreed to participate, first-degree family members were also invited. Participants could also register via the Lifelines website. In this analysis, we focused on primary prevention and therefore participants who reported myocardial infarction, stroke or coronary revascularization procedures, defined as coronary angioplasty or bypass surgery, were excluded. All participants provided written informed consent and the study protocol was approved by the medical ethical committee of the University Medical Center Groningen, the Netherlands.
Questionnaires and physical examination
At baseline, all participants received a number of questionnaires concerning demographics, family structure, medical history, lifestyle factors and use of medication. Statins and ezetimibe were classified as statin treatment. All participants visited the Lifelines research facility for a basic medical examination including blood pressure (ten times using a Dinamap automated blood pressure monitor), body height and weight. In addition, urine and blood samples were collected for storage and laboratory measurements. The estimated glomerular filtration rate was estimated using the MDRD formula. Total cholesterol, high-density lipoprotein cholesterol (HDL-c) and LDL-c levels were measured directly (Roche Modular P, Mannheim, Germany). Triglycerides were measured using an enzymatic colorimetric test (Roche Modular P).
Guideline-(in)consistent treatment
The indication to prescribe statins in the Netherlands is based on the Cardiovascular Risk Management (CVRM) guideline.4 In primary prevention, the presence of an extreme lipid profile (TC/HDL-c >8) is an indication for statin therapy. In all other cases, the 10-year predicted risk of morbidity or mortality of CVD is estimated using prediction charts based on the SCORE risk charts and national surveys. The estimated 10-year predicted CVD risk is stratified as high (≥20%), medium (10–19%) or low (<10%). The cardiovascular risk of participants with rheumatoid arthritis and diabetes mellitus is estimated by adding 15 years to their actual age. Those with a low 10-year predicted CVD risk do not have an indication for statin treatment. Subjects with a medium 10-year predicted CVD risk with one or more additional risk factors (sedentary lifestyle, positive family history of premature CVD, obesity and renal failure) and LDL-c > 2.5 mmol/l are eligible for treatment. Participants with a high 10-year predicted CVD risk and LDL-c > 2.5 mmol/l also have an indication for statin treatment. Patients treated with statins who fulfilled one of these criteria were classified as receiving guideline-consistent treatment. The remaining statin-treated patients were classified as receiving guideline-inconsistent treatment.
Evaluation of guideline-inconsistent treatment
In patients with guideline-inconsistent statin prescription, we analysed how many patients had an LDL-c level above the 95th percentile, adjusted for age and sex, had two or more major cardiovascular risk factors (based on their lifetime risk of CVD11) or a positive family history of premature CVD. In such patients, statin treatment might be justified although the 10-year predicted CVD risk is low.
Recalculation of LDL-c before statin treatment
The initiation of statin treatment is based on untreated cholesterol levels. Statins reduce LDL-c levels by 10–60% depending on the type and dose. If participants reported statin treatment at baseline, the LDL-c levels before statin treatment were unknown. Therefore correction factors were used to estimate the LDL-c and total cholesterol levels before the initiation of statin treatment.12 If the dose was not reported, the correction factor of the lowest available dose was chosen to minimize the risk of classifying a statin prescription as guideline-inconsistent.
Statistical analyses
PASW Statistics (version 23, IBM, Armonk, NY, USA) was used for the statistical analysis. Normally distributed characteristics are presented as mean ± standard deviation (SD) values. Categorical variables are presented as percentages. Student’s t-test was used to assess the difference of normally distributed variables between guideline-inconsistent and guideline-consistent treated patients. In the case of categorical variables, the Mann–Whitney U test was used. To identify risk factor associated with guideline-inconsistent treatment, we first identified all statistically significant subgroups in univariate logistic regression (data not shown); these risk factors were subsequently assessed in multivariate logistic regression (odds ratio with 95% confidence intervals).
Results
Baseline characteristics
Table 1 shows the baseline characteristics of the participants included in our study. In total, 147,785 participants were included in our analysis. The mean age was 44 years (range 18–93 years). The mean ± SD total cholesterol was 5.2 ± 1.1 mmol/l and the mean ± SD LDL-c was 3.3 ± 1.0 mmol/l. The cohort consisted of fewer men (n = 60,292 (41%)) than women. Based on the Dutch cardiovascular risk prediction score, 92% of the participants had a low 10-year predicted CVD risk, 4% had a medium risk and 4% had a high 10-year predicted CVD risk.
Table 1.
Baseline characteristics of the Lifelines cohort.
| Age (years) | 44 ± 13 |
| Male sex | 60,292 (41) |
| Systolic blood pressure (mmHg) | 125 ± 15 |
| Diastolic blood pressure (mmHg) | 74 ± 11 |
| Hypertension | 22,120 (15) |
| Body mass index (kg/m2) | 26 ± 4.3 |
| Current smoker | 30,589 (21) |
| Diabetes mellitus | 3319 (2.2) |
| Statin treatment | 7092 (4.8) |
| Lipid levels (mmol/l) | |
| Total cholesterol | 5.2 ± 1.1 |
| LDL-c | 3.3 ± 1.0 |
| HDL-c | 1.5 ± 0.4 |
| Triglycerides | 1.2 ± 0.80 |
| 10-year CVD risk | |
| Low (< 10%) | 135,301 (92) |
| Medium (10–19%) | 6573 (4) |
| High (≥ 20%) | 5911 (4) |
Data presented as mean ± SD values or n (%).
CVD: cardiovascular disease; HDL-c: high-density lipoprotein cholesterol; LDL-c: low-density lipoprotein cholesterol.
Guideline-(in)consistent treatment
Table 2 shows the characteristics of the participants with guideline-consistent and guideline-inconsistent treatment. A total of 7092 (4.8%) participants reported statin treatment; 4667 (66%) did not have a guideline-based indication for statin prescription. Patients with guideline-inconsistent treatment had lower baseline total cholesterol levels (6.9 vs. 7.7 mmol/l; p < 0.001) and lower LDL-c levels (4.1 vs. 4.6 mmol/l; p < 0.001). Participants with guideline-consistent treatment had significantly higher systolic blood pressure (139 vs. 130 mmHg; p < 0.001). Women more often had guideline-inconsistent treatment compared with men (73 vs. 59%; p < 0.001). A total of 93% of the 3911 patients with a low 10-year predicted CVD risk did not have a direct recommendation for statin treatment. Of the statin-treated patients at medium 10-year CVD risk, 64% were guideline-inconsistent. About 10% of the patients with a high 10-year CVD risk were classified as guideline-inconsistent treatment because their LDL-c was <2.5 mmol/l before the initiation of statin treatment.
Table 2.
Comparison between guideline-consistent and guideline-inconsistent statin treatment.
| Characteristics | Statin treatment |
||
|---|---|---|---|
| Guideline-inconsistent | Guideline-consistent | p | |
| (n = 4667 (66)) | (n = 2425 (34)) | ||
| Age (years) | 55 ± 11 | 63 ± 11 | <0.001 |
| Male sex | 2056 (59) | 1450 (41) | <0.001 |
| Female sex | 2611 (73) | 975 (27) | <0.001 |
| Systolic blood pressure (mmHg) | 130 ± 15 | 139 ± 17 | <0.001 |
| Hypertension | 1070 (49) | 1088 (51) | <0.001 |
| Body mass index (kg/m2) | 28 ± 4.4 | 29 ± 4.6 | <0.001 |
| Current smoker | 764 (58) | 544 (42) | <0.001 |
| Diabetes mellitus | 801 (45) | 988 (55) | <0.001 |
| Lipid levels (mmol/l) | |||
| Total cholesterol | 6.9 ± 1.7 | 7.7 ± 1.9 | <0.001 |
| LDL-c | 4.1 ± 1.3 | 4.6 ± 1.6 | <0.001 |
| HDL-c | 1.5 ± 0.4 | 1.3 ± 0.4 | <0.001 |
| Triglycerides | 1.4 ± 0.8 | 1.9 ± 1.3 | <0.001 |
| 10-year CVD risk | |||
| Low (< 10%) | 3618 (93) | 293 (7) | <0.001 |
| Medium (10–19%) | 874 (64) | 488 (36) | <0.001 |
| High (≥ 20%) | 175 (10) | 1644 (90) | <0.001 |
Data presented as mean ± SD values or n (%).
CVD: cardiovascular disease; HDL-c: high-density lipoprotein cholesterol; LDL-c: low-density lipoprotein cholesterol.
Multivariate logistic regression analysis
In the multivariate analysis, the strongest predictors of guideline-inconsistent treatment were female sex (odds ratio (OR) 4.5; 95% confidence interval (CI) 3.9–5.2), current smoking (OR 4.2; 95% CI 3.6–5.1) and a positive family history of premature CVD (OR 2.4; 95% CI 2.0–2.9) (Table 3). Patients with higher LDL-c (OR 0.47 per mmol/l increase; 95% CI 0.45–0.50) and diabetes mellitus (OR 0.09; 95% CI 0.08–0.11) were more likely to be classified as guideline-consistent treatment.
Table 3.
Risk factors for guideline-inconsistent treatment based on multivariate logistic regression analysis.
| Variable | OR | 95% CI |
|---|---|---|
| Female sex | 4.5 | 3.9–5.2 |
| Current smoker | 4.2 | 3.6–5.1 |
| Positive family history of CVD | 2.4 | 2.0–2.9 |
| Sedentary lifestyle | 1.7 | 1.2–2.3 |
| Systolic blood pressure per mmHg | 0.97 | 0.97–0.97 |
| Body mass index per kg/m2 | 0.90 | 0.89–0.91 |
| Age per year | 0.87 | 0.86–0.88 |
| LDL-c per mmol/l | 0.47 | 0.45–0.50 |
| Diabetes mellitus | 0.09 | 0.08–0.11 |
Abbreviations: CI: confidence interval; CVD: cardiovascular disease; LDL-c: low-density lipoprotein cholesterol; OR: odds ratio.
Evaluation of guideline-inconsistent treatment
The presence of cardiovascular risk factors (based on lifetime risks of CVD;11 see Supplementary Table 1, available online) is shown for those with guideline-inconsistent treatment (n = 4667; Table 4), separately for men and women. When evaluating 4667 guideline-inconsistent treated patients, 975 (21%) had LDL-c levels above the 95th percentile adjusted for age and sex, 2259 (48%) had two or more major risk factors and 738 (16%) reported a positive family history of premature CVD. Because some patients had multiple risk factors, a total of 1644 patients (35% of the total guideline-inconsistent treatment) had no discernible cause for statin treatment (Figure 1).
Table 4.
Risk factor profile of patients reporting statin treatment without indication.
| Risk factor profile | Total | Male | Female |
|---|---|---|---|
| (n = 4667) | (n = 2056) | (n = 2611) | |
| All risk factors optimum | 31 (1.0) | 10 (.5) | 21 (1.0) |
| ≥1 risk factor not optimum | 132 (3.0) | 84 (4.0) | 48 (2.0) |
| ≥1 risk factor elevated | 224 (5.0) | 126 (6.0) | 98 (4.0) |
| 1 major risk factor | 1979 (42) | 946 (46) | 1033 (40) |
| ≥2 major risk factors | 2301 (49) | 890 (43) | 1411 (54) |
Risk factor profile based on Berry et al.11
Figure 1.
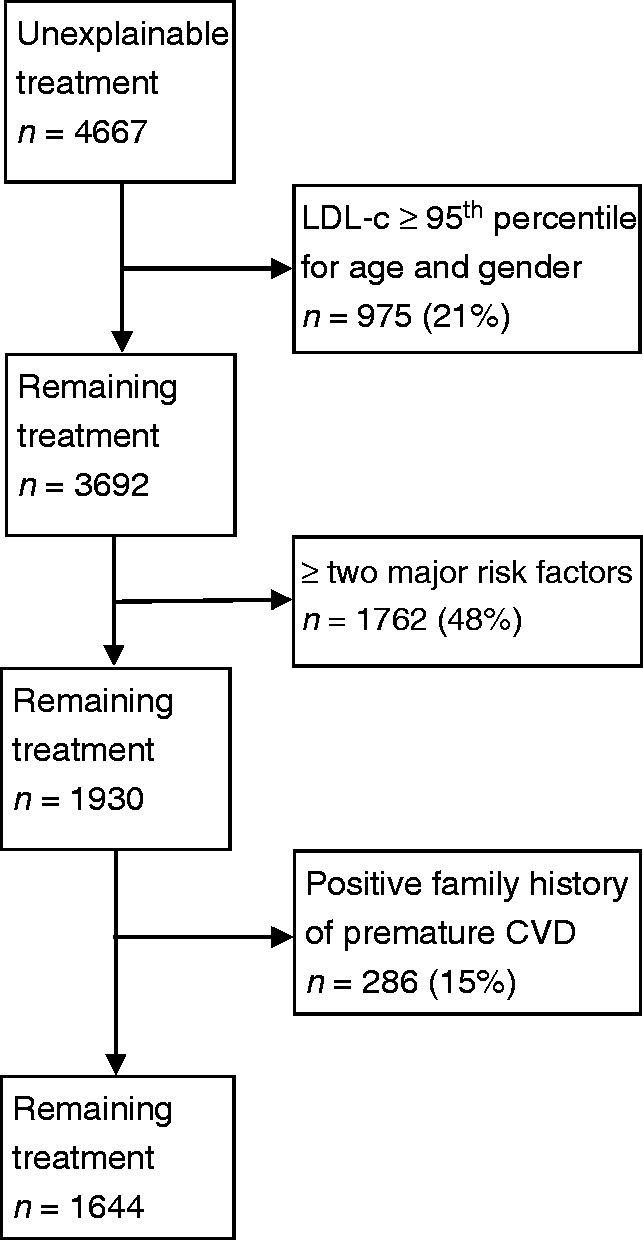
Evaluation of guideline-inconsistent treatment.
Discussion
This study shows that, despite evidence-based recommendations, 66% of the statin prescriptions in a large (relatively young) primary prevention cohort (n =147,785) were not in accordance with the Dutch guideline. Based on multivariate regression analysis, female sex and current smoking had the strongest association with guideline-inconsistent treatment. When evaluating this guideline-inconsistency, 65% of these patients had LDL-c above the 95th percentile adjusted for age and sex, two or more major risk factors of CVD or a positive family history of premature CVD. Therefore treatment might be reasonable in view of their lifetime risk.
Implications for research and practice
We have shown that evidence-based guidelines do not always translate into accurate prescribing behaviour. Our study was not designed to explain this inconsistency, but one possible explanation is that current guidelines do not identify young patients at increased risk of CVD because the 10-year CVD risk calculator is primarily driven by age. Many cardiovascular events occur before the age of 60 years, i.e. before the threshold levels of the risk calculators.13 This is an important shortcoming because early identification of patients who will develop CVD later in life is of utmost importance. It has been shown that the lifespan gain from primary prevention interventions is greater in younger patients.14 This is also supported by treating young patients with familial hypercholesterolaemia.15 The idea behind this is that lifelong exposure to elevated risk factors accelerates the progression of atherosclerosis.16 Unfortunately, a randomized controlled trial in patients with low short-term risk and increased non-familial hypercholesterolaemia range LDL-c levels has never been performed. The positive effect of statin treatment in medium-risk patients has previously been shown.17 A meta-analysis of 27 statin trials shows that statin treatment safely reduces major vascular events in low-risk patients.18
It is possible that physicians already acknowledged this shortcoming and used diagnostic gut feeling to prescribe statins in addition to evidence-based guidelines. Several alternative approaches to determine statin eligibility have recently been suggested, including lifetime risk,19 age- and sex-specific CVD risk thresholds,20 individualized statin benefit21 and lifespan gain from statin treatment.14 All come with advantages and disadvantages. It could also be possible to use the 95th percentile for age and sex of LDL-c levels to identify young and low-risk patients who could benefit from statin treatment.
Apparently, based on this and other studies, physicians and patients are willing to take the ‘risk’ of treating low-risk patients despite the known side-effects of statins. However, this report does not necessarily advocate statin treatment in low-risk patients. Although the latest Cholesterol Treatment Trialists meta-analysis showed that lowering LDL-c in low-risk patients reduces CV events,18 many questions were raised after publication.22 Closer examination shows that statin treatment in low-risk patients does not reduce overall mortality and the reduction in major vascular events is small. This reduction is driven by revascularization procedures, which is a soft cardiovascular outcome. On the other side, some serious unwanted side-effects of statins are present.22 However, total mortality cannot be fully captured in the Cholesterol Treatment Trialists meta-analysis as the duration of the trials is usually only a few years and cumulative exposure might make the story different in the long term. Larger effect sizes of statin treatment could be expected with increasing duration of follow-up. It may be safe to assume that common practice is too simply end-stage CVD based using evidence produced by short lived (5 years) LDL-c lowering intervention studies in elderly patients.
True data on the (long-term) benefits and harms of statin treatment in low-risk patients is missing. In the meantime, we are convinced that guidelines should include more detailed recommendations on the treatment of low short-term risk, but high lifetime risk patients and simultaneously stimulate more cautious treatment.
Comparison with existing literature
Of the total 7092 patients reporting treatment, 4667 (66%) were classified as guideline-inconsistent. This was 3.2% of the total study cohort (n = 147,785). Other studies have also found a large proportion of statin prescriptions not in accordance with guidelines. In a sample of 27,450 patients without CVD, Abookire et al.6 showed that a total of 2.7% reported inappropriate statin use. The percentages of guideline-inconsistent treatment were comparable (69 vs. 66%). In a large retrospective cohort analysis from >400 UK general practices, 14% reported statin treatment and almost 60% was guideline-inconsistent.7 More recently, 6.9% of >300,000 patients from the UK reported statin treatment, of which 56% was guideline-inconsistent.8 In the same study, 3.9% of the patients at low 10-year predicted CVD risk reported statin treatment. Another study, using data from the Clinical Practice Research Datalink in the UK, showed that 5.0% of participants at low 10-year predicted CVD risk received statins.9 Of the patients at low 10-year predicted CVD risk in our study (n = 135,301), 3911 (2.9%) reported statin treatment, corresponding to 55% of the statin users. This percentage is lower than in other studies, possibly related to the relatively young age of our population.
Strengths and limitations
The strengths of our study are the large number of patients included and the highly representative sample of the population of the Netherlands.23 However, middle-aged patients (25–49 years) are overrepresented in Lifelines. Because most of the patients reporting statin treatment are between 50 and 74 years (70%), our findings could be an underestimate of the true statin prescription at the population level. Another advantage is the availability of the complete cardiovascular risk profile of the patients without statin treatment.
Our study has several limitations. First, the lipid values used in this analysis were corrected for statin use. Despite the use of validated correction factors, inconsistencies may be present on an individual level. The correction factors were based on meta-analyses and many randomized controlled trials, including patients from young to old and from low to high LDL-c levels. Percentage reductions (with 95% CIs) were calculated. The percentage reductions were independent of the pre-treatment conditions and therefore suitable for our cohort. The 95% CIs of the percentage reductions were relatively wide. For example, the 95% CI of the percentage reduction of atorvastatin 5 mg daily was 27–36%.12 We assume that the large cohort size will cancel out any individual inconsistencies. Second, we assessed eligibility for statin treatment based on the CVRM guideline. However, some physicians might prefer to use internationally accepted guidelines, although the Dutch CVRM guideline is the most commonly used guideline in the Netherlands and is broadly in line with international guidelines. Therefore our findings can probably be generalized to the related international guidelines and risk calculators in other countries. Third, the CVRM guideline was updated in June 2011, i.e. during the inclusion period. Some of the participants were included in a time period in which the previous guideline was applicable, but most of the participants were included in 2012 and 2013.23 Only minor differences exist between the guidelines. Therefore we do not think that this has any meaningful impact on our results. Fourth, the risk of patients treated for hypertension is an underestimation of the true risk. In the Dutch guideline, the estimated 10-year CVD risk depends on systolic blood pressure, irrespective of antihypertensive medication. Using antihypertensive medication is not considered to be an additional risk factor. Therefore short-term antihypertensive medication will underestimate the risk of CVD and sometimes misclassify patients to a lower risk category. However, in the analysis of guideline-inconsistent treatment, the use of antihypertensive medication is considered to be a major risk factor. In patients reporting statin treatment, some missing variables were present, such as body mass index (n = 3), estimated glomerular filtration rate (n = 100) and daily activity (n = 950).
Conclusions
Taken together, our results reveal a discrepancy between cardiovascular risk guidelines and current prescribing practice for statins in primary prevention. Two-thirds of the patients reporting statins had no indication for treatment based on the guidelines. However, two-thirds of these guideline-inconsistent patients did have high LDL-c levels, two or more major risk factors for CVD or a positive family history of premature CVD, exposing them to increased risk of future cardiovascular events. This discrepancy calls for better identification of low-risk patients who could benefit from long-term statin treatment in guidelines.
Supplementary Material
Author contribution
All authors contributed to the conception or design of the work. JWB contributed to the acquisition. All authors contributed to the analysis. JWB and PWK contributed to the interpretation. JWB and PWK drafted the manuscript. JKV and DJM critically revised the manuscript. All gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Laslett LJ, Alagona P, Jr, Clark BA, III, et al. The worldwide environment of cardiovascular disease: Prevalence, diagnosis, therapy, and policy issues: A report from the American College of Cardiology. J Am Coll Cardiol 2012; 60: S1–S49. [DOI] [PubMed] [Google Scholar]
- 2.Taylor F, Huffman MD, Macedo AF, et al. Statins for the primary prevention of cardiovascular disease. Cochrane Database System Rev 2013; 1: D004816. DOI: 10.1002/14651858.CD004816.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piepoli MF, Hoes AW, et al. Authors/Task Force Members. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts): Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur J Prev Cardiol 2016; 23: NP1–N96. [DOI] [PubMed] [Google Scholar]
- 4.Wiersma T, Smulders YM, Stehouwer CD, et al. Summary of the multidisciplinary guideline on cardiovascular risk management (revision 2011). Ned Tijdschr Geneeskd 2012; 156: A5104–A5104. [PubMed] [Google Scholar]
- 5.Balder JW, Scholtens S, de Vries JK, et al. Adherence to guidelines to prevent cardiovascular diseases: The LifeLines cohort study. Neth J Med 2015; 73: 316–323. [PubMed] [Google Scholar]
- 6.Abookire SA, Karson AS, Fiskio J, et al. Use and monitoring of “statin” lipid-lowering drugs compared with guidelines. Arch Intern Med 2001; 161: 53–58. [DOI] [PubMed] [Google Scholar]
- 7.Wu J, Zhu S, Yao GL, et al. Patient factors influencing the prescribing of lipid lowering drugs for primary prevention of cardiovascular disease in UK general practice: A national retrospective cohort study. PLoS One 2013; 8: e67611–e67611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Homer K, Boomla K, Hull S, et al. Statin prescribing for primary prevention of cardiovascular disease: A cross-sectional, observational study. Br J Gen Pract 2015; 65: e538–e544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van Staa TP, Smeeth L, Ng ES, et al. The efficiency of cardiovascular risk assessment: Do the right patients get statin treatment? Heart 2013; 99: 1597–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scholtens S, Smidt N, Swertz MA, et al. Cohort profile: LifeLines, a three-generation cohort study and biobank. Int J Epidemiol 2015; 44: 1172–1180. [DOI] [PubMed] [Google Scholar]
- 11.Berry JD, Dyer A, Cai X, et al. Lifetime risks of cardiovascular disease. N Engl J Med 2012; 366: 321–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Law MR, Wald NJ, Rudnicka AR. Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: Systematic review and meta-analysis. BMJ 2003; 326: 1423–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sniderman AD, Thanassoulis G, Williams K, et al. Risk of premature cardiovascular disease vs the number of premature cardiovascular events. JAMA Cardiol 2016; 1: 492–494. [DOI] [PubMed] [Google Scholar]
- 14.Finegold JA, Shun-Shin MJ, Cole GD, et al. Distribution of lifespan gain from primary prevention intervention. Open Heart 2016; 3: e000343–e000343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wiegman A, Gidding SS, Watts GF, et al. Familial hypercholesterolaemia in children and adolescents: Gaining decades of life by optimizing detection and treatment. Eur Heart J 2015; 36: 2425–2437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hulsegge G, Smit HA, van der Schouw YT, et al. Quantifying the benefits of achieving or maintaining long-term low risk profile for cardiovascular disease: The Doetinchem Cohort Study. Eur J Prev Cardiol 2015; 22: 1307–1316. [DOI] [PubMed] [Google Scholar]
- 17.Yusuf S, Bosch J, Dagenais G, et al. Cholesterol lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med 2016; 374: 2021–2031. [DOI] [PubMed] [Google Scholar]
- 18.Mihaylova B, Emberson J, et al. Cholesterol Treatment Trialists’ (CTT) Collaborators. The effects of lowering LDL cholesterol with statin therapy in people at low risk of vascular disease: Meta-analysis of individual data from 27 randomised trials. Lancet 2012; 380: 581–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.JBS3 Board. Joint British Societies’ consensus recommendations for the prevention of cardiovascular disease (JBS3). Heart 2014; 100(Suppl 2): ii1–ii67. [DOI] [PubMed] [Google Scholar]
- 20.Navar-Boggan AM, Peterson ED, D’Agostino RBS, et al. Using age- and sex-specific risk thresholds to guide statin therapy: One size may not fit all. J Am Coll Cardiol 2015; 65: 1633–1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thanassoulis G, Williams K, Kimler Altobelli K, et al. Individualized statin benefit for determining statin eligibility in the primary prevention of cardiovascular disease. Circulation 2016; 133: 1574–1581. [DOI] [PubMed] [Google Scholar]
- 22.Abramson JD, Rosenberg HG, Jewell N, et al. Should people at low risk of cardiovascular disease take a statin? BMJ 2013; 347: f6123–f6123. [DOI] [PubMed] [Google Scholar]
- 23.Klijs B, Scholtens S, Mandemakers JJ, et al. Representativeness of the LifeLines Cohort Study. PLoS One 2015; 10: e0137203–e0137203. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


