Abstract
Background:
The biomechanical effects of lateral meniscal posterior root tears with and without meniscofemoral ligament (MFL) tears in anterior cruciate ligament (ACL)–deficient knees have not been studied in detail.
Purpose:
To determine the biomechanical effects of the lateral meniscus (LM) posterior root tear in ACL-intact and ACL-deficient knees. In addition, the biomechanical effects of disrupting the MFLs in ACL-deficient knees with meniscal root tears were evaluated.
Study Design:
Controlled laboratory study.
Methods:
Ten paired cadaveric knees were mounted in a 6-degrees-of-freedom robot for testing and divided into 2 groups. The sectioning order for group 1 was (1) ACL, (2) LM posterior root, and (3) MFLs, and the order for group 2 was (1) LM posterior root, (2) ACL, and (3) MFLs. For each cutting state, displacements and rotations of the tibia were measured and compared with the intact state after a simulated pivot-shift test (5-N·m internal rotation torque combined with a 10-N·m valgus torque) at 0°, 20°, 30°, 60°, and 90° of knee flexion; an anterior translation load (88 N) at 0°, 30°, 60°, and 90° of knee flexion; and internal rotation (5 N·m) at 0°, 30°, 60°, 75°, and 90°.
Results:
Cutting the LM root and MFLs significantly increased anterior tibial translation (ATT) during a pivot-shift test at 20° and 30° when compared with the ACL-cut state (both Ps < .05). During a 5-N·m internal rotation torque, cutting the LM root in ACL-intact knees significantly increased internal rotation by between 0.7° ± 0.3° and 1.3° ± 0.9° (all Ps < .05) except at 0° (P = .136). When the ACL + LM root cut state was compared with the ACL-cut state, the increase in internal rotation was significant at greater flexion angles of 75° and 90° (both Ps < .05) but not between 0°and 60° (all Ps > .2). For an anterior translation load, cutting the LM root in ACL-deficient knees significantly increased ATT only at 30° (P = .007).
Conclusion:
The LM posterior root was a significant stabilizer of the knee for ATT during a pivot-shift test at lower flexion angles and internal rotation at higher flexion angles.
Clinical Relevance:
Increased knee anterior translation and rotatory instability due to posterior lateral meniscal root disruption may contribute to increased loads on an ACL reconstruction graft. It is recommended that lateral meniscal root tears be repaired at the same time as an ACL reconstruction to prevent possible ACL graft overload.
Keywords: root tear, meniscofemoral ligaments, pivot shift, lateral meniscus, anterior cruciate ligament, biomechanical
It has been recently reported that lateral meniscus (LM) posterior root tears are present in 8% to 14% of patients with an anterior cruciate ligament (ACL) tear.4,7,10,17 While the ACL is the primary knee restraint to anterior tibial translation,21 the menisci provide secondary restraint to anterior-posterior translation and rotatory movement.16,19,24 Disruption of the posterior medial or lateral meniscal roots has been reported to have a similar effect on knee joint loading as a meniscectomy.1,15,18 In addition, lateral meniscal root injuries have been associated with an increased risk of osteoarthritis over time23 due to increased joint contact pressures.11
The posterior horn of the LM is stabilized by its root attachment on the tibia14 and the meniscofemoral ligaments (MFLs), which originate at the superior surface of the posterior horn and course obliquely to their respective attachment sites anterior and posterior to the posteromedial bundle of the posterior cruciate ligament (PCL).2,3 Disruption of the MFLs has been reported to significantly increase contact pressure in the tibiofemoral joint compared with the intact state in isolated posterior horn meniscal root tears.9,11
Although it has been reported that the LM posterior root attachment has an important role in stabilizing the ACL-deficient knee,24 no study has evaluated its contribution to knee stability in an ACL-intact state. In addition, there is a paucity of information in the literature on the role of the MFLs in providing rotational stability in the setting of an LM posterior root tear. Thus, the purposes of this study were to define the effect of an LM posterior root tear on a simulated pivot shift and rotational stability in ACL-intact and ACL-deficient knees and the effect of the MFL injury in ACL-deficient knees with concomitant LM posterior root tears. It was hypothesized that an LM posterior root tear would result in a significant increase in anterior tibial translation (ATT) and internal rotation during a simulated pivot-shift test and internal rotation during an internal rotation torque compared with the ACL-intact and ACL-deficient states. Furthermore, we hypothesized that cutting the MFLs would increase ATT and internal rotation during a simulated pivot-shift test.
Methods
Specimen Preparation
Ten paired fresh-frozen, male human cadaveric knees without history or evidence of prior injury, meniscal pathology, ligament tear, severe osteoarthritis (Outerbridge 3-4), or surgical history were used in this study (mean age, 57 years; range, 49-62 years). The cadaveric specimens were donated to a tissue bank for the purpose of medical research and then purchased by our institution. Knees were stored in a freezer at −20°C and thawed overnight prior to testing. All soft tissue structures 10 cm proximal and distal to the joint line were removed. The femur, tibia, and fibula were potted in poly(methyl methacrylate) (Fricke Dental).
Anatomic Dissection
Prior to robotic testing, a standard medial arthrotomy was performed to evaluate the cartilage, menisci, and cruciate ligaments to exclude pathology and facilitate cutting the structures during testing. The synovium covering the PCL was excised to visualize the PCL and the anterior meniscofemoral ligament (aMFL). The arthrotomy was then closed.
To visualize the posterior meniscofemoral ligament (pMFL), a posterior approach to the knee joint was performed. The oblique popliteal ligament (OPL) was identified, and a 2-cm mini-arthrotomy was performed just distal to the OPL in the direction of the fibers. Using this incision, the pMFL was identified and tagged for later resection at its meniscal attachment. Six pairs of knees had both the aMFL and pMFL, 3 pairs had isolated aMFL (ligament of Humphrey), and 1 pair had isolated pMFL (ligament of Wrisberg). The arthrotomy was then closed.
Robotic Setup
Each knee was secured into the robotic system. The tibia was clamped using a custom fixture mounted to a universal force-torque sensor (Delta F/T Transducer; ATI Industrial Automation) and installed on the end effector of a 6-degrees-of-freedom robotic system (KR 60-3; KUKA Robotics). Prior to mounting, each knee was weighed using a uniaxial dynamometer (GTX-500; Dillon). The same dynamometer was then used to compensate the weight of the tibial side of the specimen when zeroing the force-torque sensor. Specimens were kept moist using a 0.9% saline solution throughout the experiment. A coordinate measuring device (MicroScribe MX; GoMeasure3D) digitized anatomic landmarks to define the coordinate systems for the femur, tibia, and knee joint.13,25 Anatomic locations of the medial and lateral femoral epicondyles and medial and lateral tibial plateaus were obtained with the knee in a fully extended neutral position. Before testing the intact state, a passive path was run from 0° to 90° of flexion with a 10-N axial load while minimizing the forces and torques on all other axes.
Biomechanical Testing
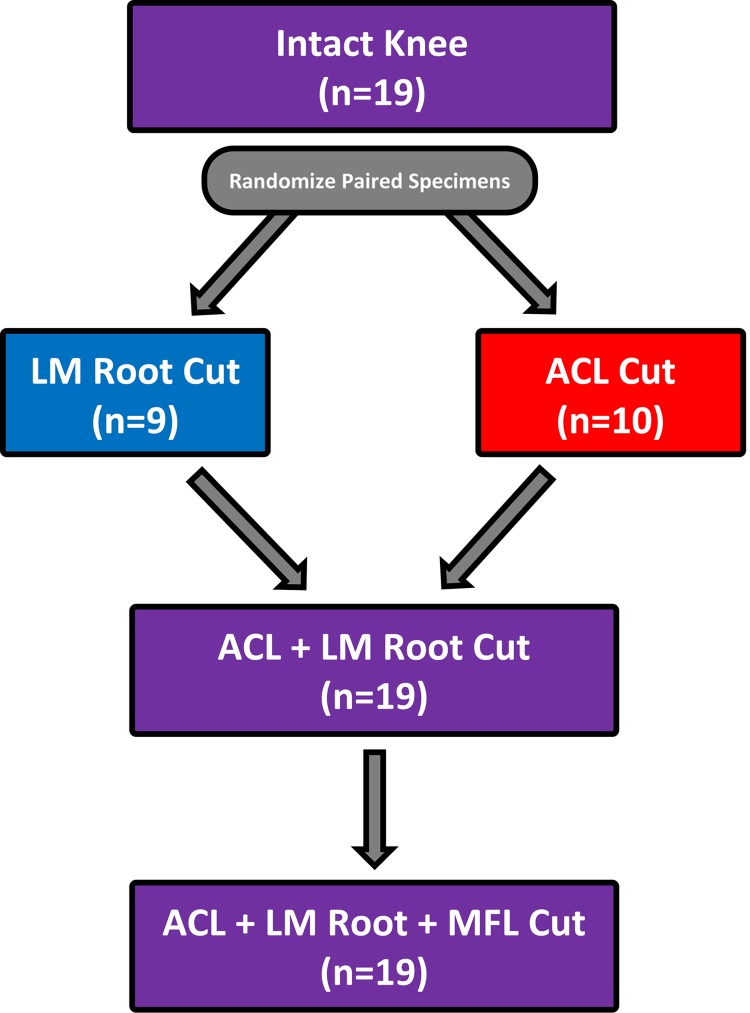
The specimens were divided into 2 groups, each undergoing a separate cutting sequence (Figure 1). The sectioning order for group 1 was (1) ACL, (2) LM posterior root, and (3) MFL. The sectioning order for group 2 was (1) LM posterior root, (2) ACL, and (3) MFL. Knees were tested at the following flexion angles: 0°, 20°, 30°, 60°, and 90° for pivot shift; 0°, 30°, 60°, and 90° for anterior drawer; and 0°, 30°, 60°, 75°, and 90° for internal rotation. Because the pivot shift is clinically relevant and elicited at lower flexion angles, smaller knee flexion increments were used at lower flexion angles for the provocative pivot maneuver. In addition, during pilot testing, rotational changes were observed at greater flexion angles, and smaller knee flexion angles increments were therefore utilized for the internal rotation test. For each flexion angle, knees were loaded to elicit a pivot shift consisting of a 10-N·m valgus torque with a 5-N·m internal rotation force.8,18 Additional testing included internal rotation (5 N·m)5 and an anterior drawer utilizing an 88-N anterior load.12 Displacements and rotations of the tibia were compared with the intact state and with the prior state.
Figure 1.
Flowchart illustrating the specimen testing states and cutting order. ACL, anterior cruciate ligament; LM, lateral meniscus; MFL, meniscofemoral ligaments.
Sectioning of the Structures
The ACL was sectioned at its tibial insertion with care to avoid injury to the anterior meniscal root attachments. An LM posterior root tear was created by performing a footprint tear through sectioning the accessory fibers of the LM between the posterior root attachment and the medial tibial eminence14 and the posterior root attachment on the tibia, and then released from the tibial attachment as described in anatomic studies. The aMFL was sectioned at its femoral and meniscal attachments. The pMFL was sectioned at its lateral meniscal attachment through the posterior arthrotomy, taking care not to damage the meniscus or the PCL.
Statistical Analysis
All measurement variables were reasonably normally distributed, so paired t tests were used to make all comparisons among knee conditions. The Holm method was used to control the familywise alpha level to 0.05 within each separate simulated biomechanical test, and Holm-adjusted P values were reported. Eight comparisons of interest were chosen before conducting the analysis: (1) intact versus LM root cut, (2) intact versus ACL cut, (3) intact versus ACL + LM root cut, (4) intact versus ACL + LM root + MFL cut, (5) ACL cut versus ACL + LM root cut, (6) LM root cut versus ACL cut, (7) ACL + LM root cut versus ACL + LM root + MFL cut, and (8) ACL cut versus ACL + LM root + MFL cut.
A priori power calculations were made for paired comparisons. Assuming 2-tailed testing, α = 0.05, and requiring 80% power, 10 matched pairs of knees was sufficient to detect effect sizes of d = 1 and d = 0.66 for the comparisons utilizing 10 and 20 knees, respectively. One specimen that underwent cutting order 1 was removed from all analyses because of a robotic position offset, leaving 19 specimens. Thus, some comparisons involved 10 knees (or 9 for cutting order 1) assigned to a single cutting order, while other comparisons were able to use all 19 specimens.
Adjusted P values less than .05 were deemed statistically significant. The statistical software R was used for all analyses (R; R Foundation for Statistical Computing with ggplot2).
Results
Results are presented as means ± standard deviations. The most important clinically relevant results are presented below, with the remainder of the data presented in the figures and tables.
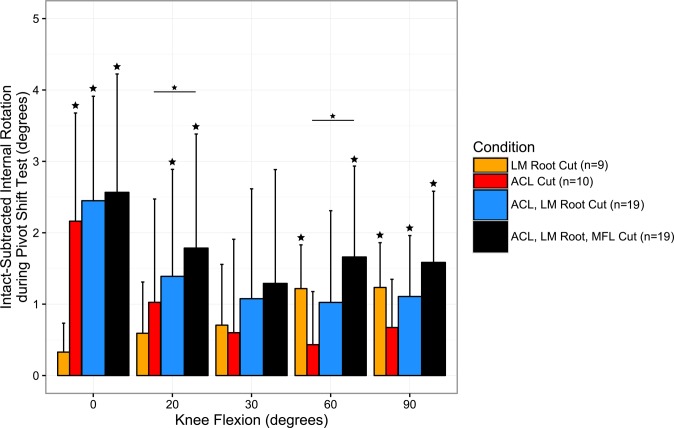
Internal Rotation During a Simulated Pivot Shift
At 60° and 90°, there was an identical significant increase in internal rotation of 1.2° ± 0.6° during a simulated pivot-shift test when the LM posterior root was cut compared with ACL-intact knees (P = .012). When the LM root was cut in ACL-deficient knees, there was no significant change in internal rotation during a simulated pivot-shift test (all mean differences ≤0.3°, all Ps > .6). Combined sectioning of the LM posterior root and the MFLs in ACL-deficient knees produced a significant increase in internal rotation when compared with the ACL-cut state at 20° and 60° (both Ps < .05) (Table 1 and Figure 2).
TABLE 1.
Resultant Mean Internal Rotation (in degrees) for All Knees When Subjected to a Simulated Pivot-Shift Test (5-N·m Internal Rotation Torque + 10-N·m Valgus Torque)a
| Flexion Angle | ||||||
|---|---|---|---|---|---|---|
| n | 0° | 20° | 30° | 60° | 90° | |
| Internal rotation, deg | ||||||
| Intact | 19 | 8.9 ± 2.3 | 15.7 ± 4.8 | 18.4 ± 9.0 | 14.0 ± 7.1 | 12.8 ± 6.0 |
| LM root cut | 9 | 9.0 ± 2.5 | 17.5 ± 3.2 | 17.1 ± 6.0 | 12.1 ± 1.7 | 13.9 ± 6.1 |
| ACL cut | 10 | 11.3 ± 2.5 | 15.7 ± 6.3 | 20.8 ± 10.0 | 17.2 ± 8.8 | 13.6 ± 5.9 |
| LM root + ACL cut | 19 | 11.4 ± 2.3 | 17.1 ± 5.3 | 19.5 ± 8.3 | 15.0 ± 6.6 | 13.9 ± 5.7 |
| LM root + ACL + MFL cut | 19 | 11.5 ± 2.2 | 17.5 ± 5.4 | 19.7 ± 8.3 | 15.6 ± 7.0 | 14.4 ± 5.6 |
aACL, anterior cruciate ligament; LM root, lateral meniscus root; MFL, meniscofemoral ligament.
Figure 2.
Changes in mean internal rotation (in degrees) for all knees when subjected to a simulated pivot-shift test (5-N·m internal rotation torque + 10-N·m valgus torque). Error bars represent 1 SD. Large stars above error bars indicate significance (P < .05) compared with the intact condition. Horizontal lines with small stars connect bars that are significantly different. ACL, anterior cruciate ligament; LM root, lateral meniscus root; MFL, meniscofemoral ligaments.
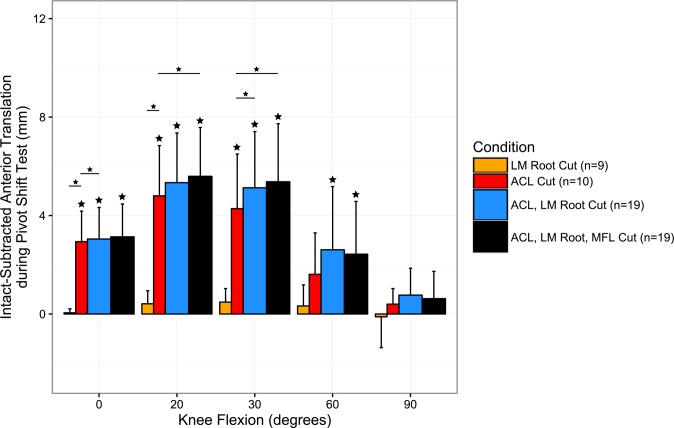
Anterior Tibial Translation During a Simulated Pivot-Shift Test
Cutting the LM root in ACL-intact knees did not produce any significant changes in ATT (all Ps > .4) compared with the intact state for a simulated pivot-shift test. Cutting the LM root in ACL-deficient knees increased ATT by between 0.2 ± 0.1 mm at 0° and 1.3 ± 1.3 mm at 60°; these changes were significant at 0° and 30° (both Ps < .05). Combined cutting of the LM posterior root and MFLs in ACL-deficient knees significantly increased ATT during simulated pivot-shift testing at 20° and 30° (both Ps < .05) but not at 0°, 60°, or 90° (all Ps > .05) compared with the ACL-cut state (Table 2 and Figure 3).
TABLE 2.
Resultant Mean Anterior Tibial Translation for All Knees (in mm) When Subjected to a Simulated Pivot-Shift Test (5-N·m Internal Rotation Torque + 10-N·m Valgus Torque)a
| Flexion Angle | ||||||
|---|---|---|---|---|---|---|
| n | 0° | 20° | 30° | 60° | 90° | |
| ATT, mm | ||||||
| Intact | 19 | 0.4 ± 0.6 | 1.5 ± 1.7 | 1.5 ± 1.4 | 0.2 ± 1.5 | –0.2 ± 1.2 |
| LM root cut | 9 | 0.5 ± 0.5 | 1.9 ± 1.5 | 1.7 ± 1.1 | 0.5 ± 1.9 | –0.2 ± 2.0 |
| ACL cut | 10 | 3.3 ± 1.6 | 6.3 ± 2.8 | 6.0 ± 2.8 | 1.9 ± 2.6 | 0 ± 1.4 |
| LM root + ACL cut | 19 | 3.4 ± 1.5 | 6.8 ± 2.7 | 6.6 ± 2.6 | 2.8 ± 3.4 | 0.5 ± 1.9 |
| LM root + ACL + MFL cut | 19 | 3.5 ± 1.6 | 7.1 ± 2.6 | 6.8 ± 2.6 | 2.7 ± 3.0 | 0.4 ± 1.8 |
aACL, anterior cruciate ligament; ATT, anterior tibial translation; LM root, lateral meniscus posterior root; MFL, meniscofemoral ligament.
Figure 3.
Changes in mean anterior tibial translation during a simulated pivot-shift test (5-N·m internal rotation torque + 10-N·m valgus torque). Error bars represent 1 SD. Large stars above error bars indicate significance (P < .05) compared with the intact condition. Horizontal lines with small stars connect bars that are significantly different. ACL, anterior cruciate ligament; LM root, lateral meniscus root; MFL, meniscofemoral ligaments.
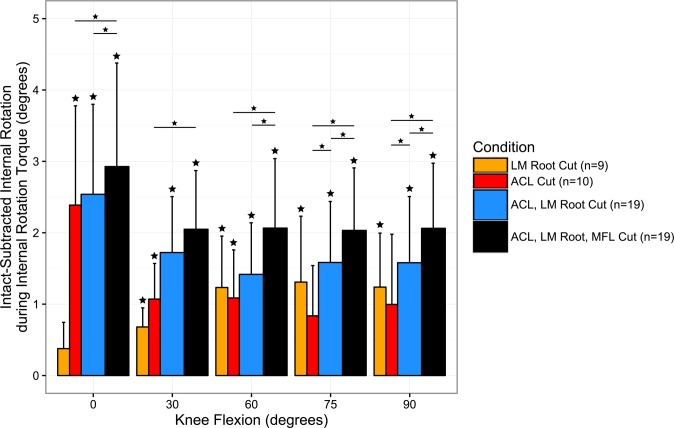
Internal Rotation During a 5-N·m Internal Rotation Torque
Cutting the LM root in ACL-intact knees significantly increased internal rotation by between 0.7° ± 0.3° and 1.3° ± 0.9° (all Ps < .05) during an internal rotation torque, except at 0° (P = .136). Cutting the LM posterior root in ACL-deficient knees significantly increased internal rotation at higher flexion angles (75° and 90°; both Ps < .05) but not between 0° and 60° (all Ps > .2) (Table 3 and Figure 4). Combined cutting of the LM posterior root and the MFLs significantly increased internal rotation when compared with the ACL-cut state for all flexion angles (all Ps < .05). The additional effect of cutting the MFLs in the ACL + LM root cut state was significant for all flexion angles (P < .05) except at 30° (P = .100).
TABLE 3.
Resultant Mean Internal Rotation of the Tibia (in Degrees) When Subjected to a 5-N·m Internal Rotation Torquea
| Flexion Angle | ||||||
|---|---|---|---|---|---|---|
| n | 0° | 20° | 30° | 60° | 90° | |
| Internal rotation, deg | ||||||
| Intact | 19 | 9.3 ± 2.8 | 18.6 ± 9.0 | 14.1 ± 7.3 | 14.9 ± 8.0 | 13.1 ± 6.7 |
| LM root cut | 9 | 9.3 ± 2.6 | 17.1 ± 7.0 | 12.4 ± 2.4 | 14.8 ± 7.6 | 14.2 ± 6.7 |
| ACL cut | 10 | 12.1 ± 3.6 | 21.6 ± 10.6 | 17.8 ± 9.4 | 16.9 ± 8.0 | 14.1 ± 6.5 |
| LM root + ACL cut | 19 | 11.9 ± 3.0 | 20.3 ± 9.0 | 15.5 ± 7.3 | 16.4 ± 7.6 | 14.6 ± 6.5 |
| LM root + ACL + MFL cut | 19 | 12.3 ± 3.1 | 20.7 ± 8.9 | 16.2 ± 7.2 | 16.9 ± 7.6 | 15.1 ± 6.4 |
aACL, anterior cruciate ligament; LM root, lateral meniscus root; MFL, meniscofemoral ligament.
Figure 4.
Changes in mean internal rotation of the tibia (in degrees) when the knees were subjected to a 5-N·m internal rotation torque. Error bars represent 1 SD. Large stars above error bars indicate statistical significance (P < .05) compared with the intact condition. Horizontal lines with small stars connect bars that are significantly different. ACL, anterior cruciate ligament; LM root, lateral meniscus root; MFL, meniscofemoral ligaments.
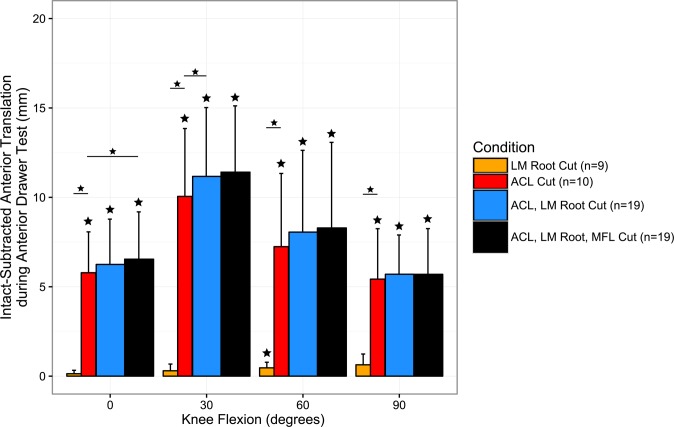
Anterior Tibial Translation to an Anteriorly Applied Load
When the LM root was cut prior to the ACL, the only significant ATT increase was of 0.5 ± 0.3 mm at 60° (P = .029). In ACL-deficient knees, cutting the LM posterior root significantly increased ATT at 30° by 1.1 ± 0.6 mm (P < .007), and combined cutting of LM posterior roots and MFLs only produced a significant increase compared with the ACL cut state at 0° (P = .019) (Table 4 and Figure 5).
TABLE 4.
Resultant Mean Anterior Tibial Translation (in mm) for All Knees Subjected to an 88-N Anterior Load Forcea
| Flexion Angle | ||||||
|---|---|---|---|---|---|---|
| n | 0° | 30° | 60° | 90° | ||
| ATT, mm | ||||||
| Intact | 19 | 3.5 ± 0.8 | 4.7 ± 1.2 | 4.3 ± 1.5 | 4.0 ± 1.4 | |
| LM root cut | 9 | 3.8 ± 1.2 | 4.9 ± 1.7 | 4.9 ± 1.8 | 4.9 ± 1.9 | |
| ACL cut | 10 | 9.1 ± 2.4 | 14.9 ± 4.2 | 11.5 ± 4.0 | 9.2 ± 2.6 | |
| LM root + ACL cut | 19 | 9.7 ± 2.6 | 15.9 ± 4.0 | 12.4 ± 4.7 | 9.7 ± 2.7 | |
| LM root + ACL + MFL cut | 19 | 10 ± 2.7 | 16.1 ± 3.9 | 12.6 ± 4.9 | 9.7 ± 2.8 | |
aACL, anterior cruciate ligament; ATT, anterior tibial translation; LM root, lateral meniscus posterior root; MFL, meniscofemoral ligament.
Figure 5.
Changes in anterior tibial translation when the knees were subjected to an 88-N anterior drawer. Error bars represent 1 SD. Large stars above error bars indicate statistical significance (P < .05) compared with the intact condition. Horizontal lines with small stars connect bars that are significantly different. ACL, anterior cruciate ligament; LM root, lateral meniscus root; MFL, meniscofemoral ligaments.
Discussion
The most important finding of this study was that the LM posterior root stabilized the knee for both ATT and internal rotation during a simulated pivot-shift test at 20° and 30° in ACL-deficient knees. Lateral meniscal posterior root tears significantly increased knee translation and rotation in ACL-deficient knees, and this implies that it may result in a higher grade pivot shift in these knees. In addition, the LM posterior root was important in controlling internal rotation at higher flexion angles in both ACL-intact and ACL-deficient knees. Lateral meniscal posterior root tears increased internal rotation in ACL-intact knees, which demonstrates a significant role of the LM posterior root for controlling internal rotation. The MFLs were found to contribute to increased stability in internal rotation; cutting the MFLs in ACL-deficient knees with LM posterior root tear further increased internal rotation during a simulated internal rotation torque. These findings have important implications on the treatment of ACL tears because of the relatively high percentage of patients who have LM posterior root tears associated with an ACL tear.4,10,17
ATT during a simulated pivot-shift test significantly increased by an additional 1.0 mm at 30° when the LM root was cut when compared with the ACL-cut state, and by 1.2 mm when both the LM root and MFLs were cut compared with the ACL-cut state. This finding suggests that the LM root and the MFLs combined to stabilize the knee during proactive pivot test in ACL-deficient knees but that the LM root had the most important significant effect on coupled ATT changes during the pivot shift when compared with the ACL-cut state. The stabilizing effect of the LM root has been reported by previous studies.11,15 Shybut et al24 reported 2.1 mm of additional ATT during a simulated pivot shift when an LM posterior root and MFL disruption was added to an isolated ACL tear. In the present study, the LM posterior root and the MFLs were sectioned sequentially to determine the effect of each structure, whereas in the study by Shybut et al,24 the LM posterior root was sectioned together with the MFLs. Lateral meniscal posterior root injuries with or without concomitant MFLs injuries have been reported,17 and thus, evaluating these injuries separately is clinically relevant. Obtaining somewhat similar results in anatomic function, Musahl et al19 noted an additional 6 mm of ATT of the lateral compartment after a subtotal lateral meniscectomy in an ACL-deficient state. However, the methods of eliciting a pivot shift in these 2 other studies varied from our study, and this may have contributed to the differences in results.20 Musahl et al19 performed a pivot shift using a continuous passive motion machine, foot plate, and Velcro strap,19 while Shybut et al24 utilized various iliotibial band forces and internal rotation and valgus moments. In addition, Musahl et al19 performed a complete lateral meniscectomy versus an isolated root disruption as in our study, possibly aggravating the destabilizing effects. However, the overall concordance between these varying studies is that the LM posterior root attachment has a significant role in stabilizing against increased ATT in an ACL-deficient knee during pivoting activities.
In addition to increased ATT during a pivot shift, ATT during an 88-N anterior tibial applied force significantly increased by 1.1 mm when the LM posterior root was cut in ACL-deficient knees at 30° and 60°. Cutting the LM posterior root and MFLs in ACL-deficient knees increased ATT by 1.1 and 1.4 mm at 30° and 60°, respectively. A 3-mm side-to-side difference in ATT has been reported to be pathologic when evaluating the function of the ACL.6 Thus, a concurrent deficiency of the LM posterior root and the MFLs could result in up to half of the recognized side-to-side objective ATT differences seen with an ACL tear. In contrast, Shybut et al24 reported no significant difference in ATT during a simulated anterior stability test between the ACL-deficient and ACL-deficient with LM root avulsion groups. Musahl et al19 also reported no significant difference in ATT in knees with an ACL tear and a subtotal lateral meniscectomy when compared with ACL-deficient knees.
The importance of the ACL as a primary knee stabilizer for internal rotation at lower flexion angles has been reported in earlier biomechanical studies,24 but the role of the LM posterior root as a primary stabilizer of the knee to internal rotation at higher flexion angles is new information. The increase in internal rotation after sectioning the LM root in the ACL-deficient knee was comparable to that reported in ACL-deficient noncopers, which further highlights the important role of the LM root attachment in ACL-deficient knees. In a recent in vivo 3-dimensional gait kinematics analysis study by Shabani et al,22 ACL-deficient noncoper knees had a significant increase of 1.4° ± 0.2° in internal rotation compared with the ACL-intact group, which essentially matches the amount of increased internal rotation seen in our study for an LM posterior root tear.
It is acknowledged that this study has some limitations. As a time-zero cadaveric study, it is inherent that the results of this study did not take into account the dynamic stabilizers of the knee. Internal and external rotation, as well as pivoting mechanisms of the knee, are controlled by an intricate interplay of many structures, including muscles and the anterolateral corner structures. The effect of these other structures was not a subject of this study. For consistency, the same surgeon performed all cuts. To avoid testing bias, the testing angles were randomized and the paired knees were randomized to cutting order.
Conclusion
In the current study, the LM posterior root was a significant stabilizer of the knee for ATT during a simulated pivot-shift test at lower flexion angles and internal rotation at higher flexion angles. Increased knee instability due to lateral meniscal root deficiency may contribute to increased functional limitations in patients and potentially to increased loads on ACL reconstruction grafts.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: Smith & Nephew provided funding for this study and an in-kind donation of surgical supplies. R.F.L. is a consultant for Arthrex, Ossur, and Smith & Nephew; receives royalties from Arthrex and Smith & Nephew; receives research support from Arthrex and Smith & Nephew; has received grants from Health East, Norway and an NIH R-13 grant for biologics; has patents pending with Ossur and Smith & Nephew; and patents with royalties paid from Ossur, Smith & Nephew, and Arthrex. G.M. has received grants from Health South East (Helse Sør-Øst) Norway and Arthrex.
Ethical approval was not sought for the present study.
References
- 1. Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90:1922–1931. [DOI] [PubMed] [Google Scholar]
- 2. Amis AA, Gupte CM, Bull AM, Edwards A. Anatomy of the posterior cruciate ligament and the meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2006;14:257–263. [DOI] [PubMed] [Google Scholar]
- 3. Anderson CJ, Ziegler CG, Wijdicks CA, Engebretsen L, LaPrade RF. Arthroscopically pertinent anatomy of the anterolateral and posteromedial bundles of the posterior cruciate ligament. J Bone Joint Surg Am. 2012;94:1936–1945. [DOI] [PubMed] [Google Scholar]
- 4. Brody JM, Lin HM, Hulstyn MJ, Tung GA. Lateral meniscus root tear and meniscus extrusion with anterior cruciate ligament tear. Radiology. 2006;239:805–810. [DOI] [PubMed] [Google Scholar]
- 5. Coobs BR, Wijdicks CA, Armitage BM, et al. An in vitro analysis of an anatomical medial knee reconstruction. Am J Sports Med. 2010;38:339–347. [DOI] [PubMed] [Google Scholar]
- 6. Daniel DM, Stone ML, Sachs R, Malcom L. Instrumented measurement of anterior knee laxity in patients with acute anterior cruciate ligament disruption. Am J Sports Med. 1985;13:401–407. [DOI] [PubMed] [Google Scholar]
- 7. De Smet AA, Blankenbaker DG, Kijowski R, Graf BK, Shinki K. MR diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. AJR Am J Roentgenol. 2009;192:480–486. [DOI] [PubMed] [Google Scholar]
- 8. Engebretsen L, Wijdicks CA, Anderson CJ, Westerhaus B, LaPrade RF. Evaluation of a simulated pivot shift test: a biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2012;20:698–702. [DOI] [PubMed] [Google Scholar]
- 9. Forkel P, Herbort M, Schulze M, et al. Biomechanical consequences of a posterior root tear of the lateral meniscus: stabilizing effect of the meniscofemoral ligament. Arch Orthop Trauma Surg. 2013;133:621–626. [DOI] [PubMed] [Google Scholar]
- 10. Forkel P, Reuter S, Sprenker F, et al. Different patterns of lateral meniscus root tears in ACL injuries: application of a differentiated classification system. Knee Surg Sports Traumatol Arthrosc. 2015;23:112–118. [DOI] [PubMed] [Google Scholar]
- 11. Geeslin AG, Civitarese D, Turnbull TL, Dornan GJ, Fuso FA, LaPrade RF. Influence of lateral meniscal posterior root avulsions and the meniscofemoral ligaments on tibiofemoral contact mechanics. Knee Surg Sports Traumatol Arthrosc. 2016;24:1469–1477. [DOI] [PubMed] [Google Scholar]
- 12. Goldsmith MT, Jansson KS, Smith SD, Engebretsen L, LaPrade RF, Wijdicks CA. Biomechanical comparison of anatomic single- and double-bundle anterior cruciate ligament reconstructions: an in vitro study. Am J Sports Med. 2013;41:1595–1604. [DOI] [PubMed] [Google Scholar]
- 13. Grood ES, Suntay WJ. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105:136–144. [DOI] [PubMed] [Google Scholar]
- 14. Johannsen AM, Civitarese DM, Padalecki JR, Goldsmith MT, Wijdicks CA, LaPrade RF. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med. 2012;40:2342–2347. [DOI] [PubMed] [Google Scholar]
- 15. LaPrade CM, Jansson KS, Dornan G, Smith SD, Wijdicks CA, LaPrade RF. Altered tibiofemoral contact mechanics due to lateral meniscus posterior horn root avulsions and radial tears can be restored with in situ pull-out suture repairs. J Bone Joint Surg Am. 2014;96:471–479. [DOI] [PubMed] [Google Scholar]
- 16. Levy IM, Torzilli PA, Warren RF. The effect of medial meniscectomy on anterior-posterior motion of the knee. J Bone Joint Surg Am. 1982;64:883–888. [PubMed] [Google Scholar]
- 17. Matheny LM, Ockuly AC, Steadman JR, LaPrade RF. Posterior meniscus root tears: associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc. 2015;23:3127–3131. [DOI] [PubMed] [Google Scholar]
- 18. McCulloch PC, Shybut TB, Isamaily SK, et al. The effect of progressive degrees of medial meniscal loss on stability after anterior cruciate ligament reconstruction. J Knee Surg. 2013;26:363–369. [DOI] [PubMed] [Google Scholar]
- 19. Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010;38:1591–1597. [DOI] [PubMed] [Google Scholar]
- 20. Musahl V, Voos J, O’Loughlin PF, Stueber V, Kendoff D, Pearle AD. Mechanized pivot shift test achieves greater accuracy than manual pivot shift test. Knee Surg Sports Traumatol Arthrosc. 2010;18:1208–1213. [DOI] [PubMed] [Google Scholar]
- 21. Noyes FR, Bassett RW, Grood ES, Butler DL. Arthroscopy in acute traumatic hemarthrosis of the knee. Incidence of anterior cruciate tears and other injuries. J Bone Joint Surg Am. 1980;62:687–695, 757. [PubMed] [Google Scholar]
- 22. Shabani B, Bytyqi D, Lustig S, Cheze L, Bytyqi C, Neyret P. Gait changes of the ACL-deficient knee 3D kinematic assessment. Knee Surg Sports Traumatol Arthrosc. 2015;23:3259–3265. [DOI] [PubMed] [Google Scholar]
- 23. Shelbourne KD, Roberson TA, Gray T. Long-term evaluation of posterior lateral meniscus root tears left in situ at the time of anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:1439–1443. [DOI] [PubMed] [Google Scholar]
- 24. Shybut TB, Vega CE, Haddad J, et al. Effect of lateral meniscal root tear on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2015;43:905–911. [DOI] [PubMed] [Google Scholar]
- 25. Wu G, Cavanagh PR. ISB recommendations for standardization in the reporting of kinematic data. J Biomech. 1995;28:1257–1261. [DOI] [PubMed] [Google Scholar]