Abstract
Background:
Capitellar osteochondritis dissecans (OCD) is a debilitating condition of unknown etiology for which various arthroscopic treatments are available. Prior data suggest that greater than 75% of the capitellum can be visualized arthroscopically through a dual lateral portal approach. However, there is no literature assessing arthroscopic visualization of the capitellum via alternative portals.
Purpose:
To determine the percentage of capitellum visualized using the dual lateral, distal ulnar and soft spot, and posterolateral and soft spot portal configurations in a cadaver model.
Study Design:
Descriptive laboratory study.
Methods:
Arthroscopy was performed on 12 fresh-frozen cadaver elbows, 4 for each of the following approaches: dual lateral, distal ulna, and posterolateral. Electrocautery was used to mark the most anterior, posterior, medial, and lateral points seen on the capitellum. The radiocapitellar joint was subsequently exposed through an extensile posterior dissection, and the surface anatomy was reconstructed using the Microscribe 3D digitizing system. Using Rhinoceros software, the percentage of capitellum surface area visualized by each approach was determined.
Results:
The mean percentage of capitellum visualized for the dual lateral, distal ulna, and posterolateral approaches was approximately 68.8%, 66.3%, and 63.5%, respectively. There was no significant difference between the percentage of capitellum seen among approaches (P = .68). On average, 66.5% of the capitellum was visible through these 3 arthroscopic approaches to the elbow.
Conclusion:
Approximately 66.5% of the capitellum is visualized through the popularized posterior arthroscopic portals, with no significant differences found between the 3 investigated approaches.
Clinical Relevance:
As determined in this cadaveric model investigation, each portal technique provides equivalent visualization for capitellar OCD pathology.
Keywords: elbow arthroscopy, capitellum visualization, portal selection
Capitellar osteochondritis dissecans (OCD) is an incapacitating condition characterized by noninflammatory degeneration of the subchondral bone.8,16,20,23 This pathology most commonly affects young athletes, such as throwers and gymnasts, engaged in valgus-producing, repetitive activities of the upper extremity.8,15,16,20,30 If left untreated, a capitellar OCD lesion can lead to an arthritic elbow, resulting in significant pain and functional limitations.8,24
Treatment algorithms for OCD of the capitellum are based on the stability of the lesion.3,5,7,31,32 Stable lesions are often managed conservatively with activity modification and rest.7,22,31 On the other hand, unstable lesions frequently require surgical intervention, and elbow arthroscopy is growing in popularity as both a diagnostic and definitive treatment tool.3,7,31,32 Arthroscopic or arthroscopic-assisted surgical options for the treatment of capitellar OCD include debridement and loose body removal, marrow stimulation, fragment fixation, and mosaicplasty.3,14,25,28,31,32
These arthroscopic techniques are challenging, and the importance of portal selection and placement is amplified when attempting to access capitellar OCD lesions at varying coronal and sagittal positions through a posterior approach.1,2,28 Prior literature suggests that greater than 75% of the capitellum can be accessed through a dual lateral approach.13 However, no studies have compared the accessibility of the capitellum from other popular posterior portals such as the posterolateral and distal ulnar portals. As techniques in elbow arthroscopy expand, it becomes of even greater importance to understand the most utilitarian approach to the radiocapitellar joint. The purpose of this study was to determine the percentage of capitellum that can be visualized using the dual lateral, distal ulnar, and posterolateral portals in a cadaver model. We hypothesized that there would be no significant advantage to any one approach due to the anatomic constraints inherent to the elbow, such as the congruity of the radiocapitellar joint.
Methods
Arthroscopy was performed on 12 fresh-frozen cadaver elbows (mean age, 69 years; range, 49-83 years) using a 4.0-mm 30° arthroscope. Cadavers and implants used in this study were provided by an educational grant from Arthrex Inc. The specimens were thawed overnight at room temperature prior to investigation. Each elbow specimen was mounted to simulate the lateral decubitus position. The appropriate landmarks and portals were identified. The elbow was insufflated with 20 mL of saline, and each specimen underwent standard diagnostic arthroscopy of the anterior compartment prior to experimentation.
The posterolateral compartment was approached through 3 techniques: (1) dual lateral, (2) soft spot and posterolateral, or (3) soft spot and distal ulnar technique. The dual lateral portals were made radial and ulnar to the point of insufflation at the soft spot, approximately 1 cm apart.13 The posterolateral portal can be established just lateral to the triceps tendon and anywhere from the tip of the olecranon to 3 cm proximal to the olecranon.2 To maintain uniformity, a portal approximately 1 cm proximal to the olecranon tip along the lateral border of the triceps was chosen for this study. The distal ulnar portal was made approximately 3 cm distal to the posterior aspect of the radiocapitellar joint and just lateral to the palpable posterior edge of the ulna.34 The soft spot portal was located in the center of the triangle formed by the lateral epicondyle, olecranon tip, and radial head (Figure 1).2 Each 2-portal approach was assigned to 4 cadavers. The viewing and working portals were alternated during the marking process according to surgeon preference. Synovium debridement was performed to enhance visualization of the radiocapitellar joint. An arthroscopic electrocautery device was used to mark the most anterior, posterior, medial, and lateral points seen on the capitellum for each specimen (Figure 2). Elbow flexion and extension was allowed during arthroscopy. Once complete, the visualized capitellar surface area was recorded.
Figure 1.
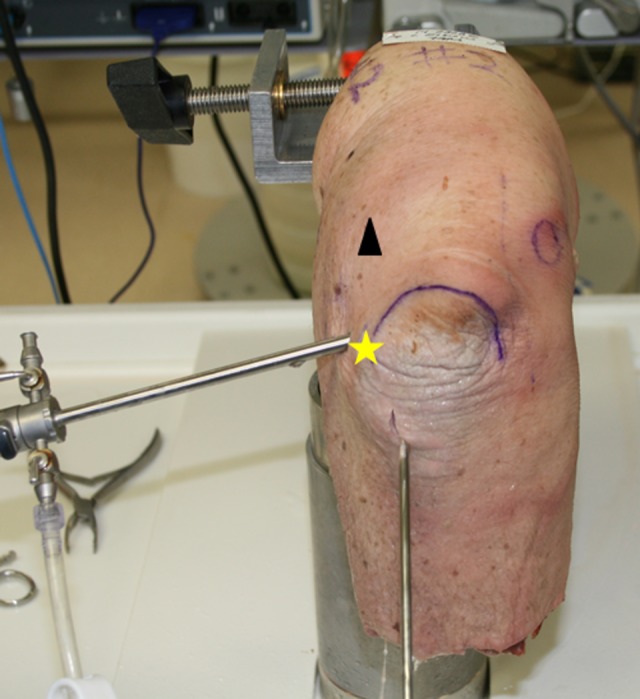
Portal location. The posterolateral compartment was approached using 3 different techniques. The dual lateral technique is represented by a portal just radial to the arthroscope and the yellow star. The soft spot and distal ulnar technique are represented by the arthroscope and distal working instrument. Finally, the soft spot and posterolateral technique are represented by the arthroscope and black triangle.
Figure 2.

Specimen marking. An arthroscopic electrocautery device was used to mark the most anterior, posterior, medial, and lateral points visualized on the capitellum for each specimen.
An extensile posterior approach with transection of the lateral collateral ligament complex was then used to disarticulate the radiocapitellar joint. This technique allowed full access to the capitellum and radial head articular surfaces. The surface area of the entire capitellum, the capitellum visualized arthroscopically, and the radial head were reconstructed using the Microscribe 3D digitizing system (Revware Inc). A point-to-point probe was used to outline these areas, and each surgeon repeated these measurements twice, documenting a total of 4 dimensions for every end point. Inter- and intraobserver reliability were assessed by calculating the intraclass correlation coefficient (ICC). The interobserver ICC was 0.51, representing moderate agreement17; the intraobserver ICC was 0.59 and 0.79 for the 2 individual observers, representing moderate and substantial agreement, respectively. These measurements were used to create digitized images that were then analyzed using Rhinoceros 3D modeler software (McNeel North America). The percentage of capitellum surface area visualized by each approach was calculated for every specimen. An example is shown in Figure 3.
Figure 3.
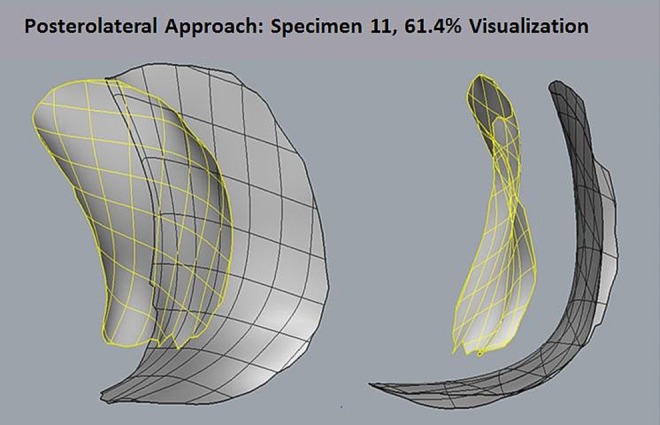
Rendering of the surface area of the capitellum, visualized arthroscopically, over the entire capitellum surface area for specimen 11. The point-to-point probe was used to collect data that were translated into digitized images that could be analyzed using Rhinoceros 3D modeler software. In this example, 61.4% of the capitellum was accessed and visualized.
Statistical analyses were performed using GraphPad Prism version 6.0e (GraphPad Software) and R 3.1.2. Statistical significance was determined using a Student 2-tailed t test and analysis of variance (ANOVA) when comparing the means of 2 or more groups, respectively.
Results
Prior to arthroscopy, the elbow flexion of each cadaveric specimen was recorded. The mean elbow flexion found was 129.2° (range, 125.0°-135.3°). During arthroscopy, all posterior approaches provided complete access to the lateral-, medial-, and posterior-most aspects of the capitellum. Variability was related to visualization of the anterior capitellum. Specimens 1 through 4 were assigned the dual lateral approach to the radiocapitellar joint. The mean percentage of capitellum visualized was 68.8% ± 6.5%. Specimens 5 through 8 were assigned the distal ulnar approach to the radiocapitellar joint. The mean percentage of capitellum visualized was 66.3% ± 8.2%. Specimens 9 through 12 were assigned the posterolateral technique to the radiocapitellar joint. The mean percentage of capitellum visualized was 63.5% ± 5.2% (Table 1). There was no significant difference noted between the mean percentage of capitellum visualized between the dual lateral and distal ulnar (P = .66) or posterolateral approaches (P = .34). Similarly, there was no significant difference between the distal ulnar and posterolateral visualization (P = .72). No difference was found between the mean percentages of capitellum visualized between the 3 approaches (ANOVA; P = .68). On average, 66.5% of the capitellum was visualized through a 2-portal posterior technique.
TABLE 1.
Mean Percentage of Capitellum Visualized for Each Approach
| Approach | Mean Percentage of Capitellum Visualized (SD) |
|---|---|
| Dual lateral | 68.8 (6.5) |
| Distal ulnar | 66.3 (8.2) |
| Posterolateral | 63.5 (5.2) |
Discussion
OCD of the elbow is a debilitating condition for young athletes. While the exact etiology remains unknown, it is likely multifactorial, with potential causes including patient genetics, a tenuous vascular supply to the capitellum, biomechanical mismatch, and repetitive stresses placed onto the radiocapitellar joint by specific athletic populations.12 While long-term results are lacking, promising intermediate outcomes have helped arthroscopy become the treatment of choice for many OCD lesions of the capitellum.3,6,9–11,14,18,19,26,27 Options for surgical treatment include arthroscopic removal of loose bodies, chondroplasty, microfracture, retrograde drilling, fragment fixation, and osteochondral autograft transplantation.4,29,33,35
As new techniques for treatment continue to develop, it is important to determine the best strategy for arthroscopic capitellar visualization. In 2007, Davis et al13 conducted a cadaveric study demonstrating the safety of the dual lateral approach in relation to the lateral ligamentous structures. Using a mathematical formula, the authors also determined that approximately 78% of the capitellar surface was visualized through the dual lateral portals; however, they did not compare the dual lateral approach to other portal configurations.13
The current investigation sought to improve upon that initial study. As such, our purpose was to calculate the percentage of capitellar surface area visualized via 3 arthroscopic approaches to optimize potential treatment strategies. Furthermore, a strength of this study is the utilization of a digitized system to accurately map the surface anatomy of the capitellum and calculate the exact amount that was accessible arthroscopically. For the dual lateral, distal ulna, and posterolateral approaches, the mean percentage of capitellum visualized was approximately 68.8%, 66.3%, and 63.5%, respectively. While this degree of visualization is adequate for most clinically significant OCD lesions of the capitellum, which lie approximately 45° to 60° anterior to the humeral shaft, these percentages are more than 10% less than were found in the analysis by Davis et al13 of the visualization possible via the dual lateral approach.13,21 This disparity is most likely due to the different methods of calculating the capitellar surface area in both studies. For example, Davis et al13 estimated capitellar surface area by multiplying the calculated surface area of a cylinder by a coefficient representing the percentage that comprised the capitellar articular surface. Another factor that may have affected our respective results is that the mean elbow flexion in the current investigation was 129.2°, which is lower than that found by Davis et al13 (142°). Finally, it should also be mentioned that Davis et al13 positioned patients supine while the lateral decubitus position was utilized in the current investigation, although this is unlikely to have played a large role in the differences noted between the amount of capitellum visualized.
In a review of treating OCD of the capitellum via the distal ulnar approach, van den Ende et al34 described the disadvantages for the dual lateral and posterolateral approaches. The authors argue that the dual lateral approach requires close placement of the portals, which increases the chance of competition between the instruments and arthroscope (referred to as “sword fighting”), while the posterolateral approach is awkward as the arthroscope must be pointed toward the surgeon to visualize the capitellum. On the other hand, the distal ulnar portal allows for a more ergonomic approach to the posterolateral capitellum due to the orientation of the portal in relation to the capitellum that allows the arthroscope to be pointed away from the surgeon. Despite this advantage, the distal ulnar portal did not provide any substantial difference in visualization compared with the other approaches investigated in the current study.
The limitation of this study is that it is an observational, cadaveric investigation confined by the number of specimens available. In addition, while capitellar OCD is most commonly a pediatric disease, the specimens used averaged approximately 70 years of age and likely had some degree of osteoarthritis given that the mean elbow flexion was 129.2°, which may have limited capitellar visualization. On the other hand, pediatric elbows are smaller, which may further limit access to the anterior aspects of the capitellum. Finally, the authors only used a 4.0-mm, 30° arthroscope in this investigation. Future similar studies may incorporate different instrumentation such as a smaller diameter or a 70° arthroscope, which may improve visualization. Despite these limitations, the results presented have simple and practical clinical applications. The findings suggest that the dual lateral, distal ulnar, and posterolateral approaches are equally effective with regard to visualization of the capitellum. As a result, surgeons have the ability to select their preferred approach without compromising their ability to identify pathology.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: C.S.A. is a consultant for Arthrex and Acumed and receives research support from Arthrex, Stryker, and Major League Baseball. This project was funded by an educational grant from Arthrex Inc. Cadavers and implants for this study were provided by Arthrex. Arthrex and the granting agency had no influence over the design of the study or the analysis and interpretation of the study data.
Ethical approval was not sought for the present study.
References
- 1. Adams JE, King GJ, Steinmann SP, Cohen MS. Elbow arthroscopy: indications, techniques, outcomes, and complications. J Am Acad Orthop Surg. 2014;22:810–818. [DOI] [PubMed] [Google Scholar]
- 2. Ahmad CS, Vitale MA. Elbow arthroscopy: setup, portal placement, and simple procedures. Instr Course Lect. 2011;60:171–180. [PubMed] [Google Scholar]
- 3. Ahmad CS, Vitale MA, ElAttrache NS. Elbow arthroscopy: capitellar osteochondritis dissecans and radiocapitellar plica. Instr Course Lect. 2011;60:181–190. [PubMed] [Google Scholar]
- 4. Baker CL, 3rd, Baker CL, Jr, Romeo AA. Osteochondritis dissecans of the capitellum. J Shoulder Elbow Surg. 2010;19:76–82. [DOI] [PubMed] [Google Scholar]
- 5. Baumgarten TE, Andrews JR, Satterwhite YE. The arthroscopic classification and treatment of osteochondritis dissecans of the capitellum. Am J Sports Med. 1998;26:520–523. [DOI] [PubMed] [Google Scholar]
- 6. Bojanic I, Ivkovic A, Boric I. Arthroscopy and microfracture technique in the treatment of osteochondritis dissecans of the humeral capitellum: report of three adolescent gymnasts. Knee Surg Sports Traumatol Arthrosc. 2006;14:491–496. [DOI] [PubMed] [Google Scholar]
- 7. Bradley JP, Petrie RS. Osteochondritis dissecans of the humeral capitellum. Diagnosis and treatment. Clin Sports Med. 2001;20:565–590. [DOI] [PubMed] [Google Scholar]
- 8. Brown R, Blazina ME, Kerlan RK, Carter VS, Jobe FW, Carlson GJ. Osteochondritis of the capitellum. J Sports Med. 1974;2:27–46. [DOI] [PubMed] [Google Scholar]
- 9. Brownlow HC, O’Connor-Read LM, Perko M. Arthroscopic treatment of osteochondritis dissecans of the capitellum. Knee Surg Sports Traumatol Arthrosc. 2006;14:198–202. [DOI] [PubMed] [Google Scholar]
- 10. Byrd JW, Elrod BF, Jones KS. Elbow arthroscopy for neglected osteochondritis dissecans of the capitellum. J South Orthop Assoc. 2001;10:12–16. [PubMed] [Google Scholar]
- 11. Byrd JW, Jones KS. Arthroscopic surgery for isolated capitellar osteochondritis dissecans in adolescent baseball players: minimum three-year follow-up. Am J Sports Med. 2002;30:474–478. [DOI] [PubMed] [Google Scholar]
- 12. Churchill RW, Munoz J, Ahmad CS. Osteochondritis dissecans of the elbow. Curr Rev Musculoskelet Med. 2016;9:232–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Davis JT, Idjadi JA, Siskosky MJ, ElAttrache NS. Dual direct lateral portals for treatment of osteochondritis dissecans of the capitellum: an anatomic study. Arthroscopy. 2007;23:723–728. [DOI] [PubMed] [Google Scholar]
- 14. de Graaff F, Krijnen MR, Poolman RW, Willems WJ. Arthroscopic surgery in athletes with osteochondritis dissecans of the elbow. Arthroscopy. 2011;27:986–993. [DOI] [PubMed] [Google Scholar]
- 15. Douglas G, Rang M. The role of trauma in the pathogenesis of the osteochondroses. Clin Orthop Relat Res. 1981;158:28–32. [PubMed] [Google Scholar]
- 16. Duthie RB, Houghton GR. Constitutional aspects of the osteochondroses. Clin Orthop Relat Res. 1981;158:19–27. [PubMed] [Google Scholar]
- 17. Fleiss J. The equivalence of weighted kappa and the intraclass correlation coefficient as measures of reliability. Educ Psychol Meas. 1973;33:613–619. [Google Scholar]
- 18. Jones KJ, Wiesel BB, Sankar WN, Ganley TJ. Arthroscopic management of osteochondritis dissecans of the capitellum: mid-term results in adolescent athletes. J Pediatr Orthop. 2010;30:8–13. [DOI] [PubMed] [Google Scholar]
- 19. Krijnen MR, Lim L, Willems WJ. Arthroscopic treatment of osteochondritis dissecans of the capitellum: report of 5 female athletes. Arthroscopy. 2003;19:210–214. [DOI] [PubMed] [Google Scholar]
- 20. Kusumi T, Ishibashi Y, Tsuda E, et al. Osteochondritis dissecans of the elbow: histopathological assessment of the articular cartilage and subchondral bone with emphasis on their damage and repair. Pathol Int. 2006;56:604–612. [DOI] [PubMed] [Google Scholar]
- 21. Maesawa S. Roentgenologic evaluation of etiology of osteochondritis dissecans of the elbow. Rinshoseikeigeka. 1985;20:1157–1163. [Google Scholar]
- 22. Mihara K, Tsutsui H, Nishinaka N, Yamaguchi K. Nonoperative treatment for osteochondritis dissecans of the capitellum. Am J Sports Med. 2009;37:298–304. [DOI] [PubMed] [Google Scholar]
- 23. Nagura S. The so-called osteochondritis dissecans of Konig. Clin Orthop Relat Res. 1960;18:100–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nakagawa Y, Matsusue Y, Ikeda N, Asada Y, Nakamura T. Osteochondral grafting and arthroplasty for end-stage osteochondritis dissecans of the capitellum. A case report and review of the literature. Am J Sports Med. 2001;29:650–655. [DOI] [PubMed] [Google Scholar]
- 25. Pill SG, Ganley TJ, Flynn JM, Gregg JR. Osteochondritis dissecans of the capitellum: arthroscopic-assisted treatment of large, full-thickness defects in young patients. Arthroscopy. 2003;19:222–225. [DOI] [PubMed] [Google Scholar]
- 26. Rahusen FT, Brinkman JM, Eygendaal D. Results of arthroscopic debridement for osteochondritis dissecans of the elbow. Br J Sports Med. 2006;40:966–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ruch DS, Cory JW, Poehling GG. The arthroscopic management of osteochondritis dissecans of the adolescent elbow. Arthroscopy. 1998;14:797–803. [DOI] [PubMed] [Google Scholar]
- 28. Savoie FH., 3rd Guidelines to becoming an expert elbow arthroscopist. Arthroscopy. 2007;23:1237–1240. [DOI] [PubMed] [Google Scholar]
- 29. Shimada K, Tanaka H, Matsumoto T, et al. Cylindrical costal osteochondral autograft for reconstruction of large defects of the capitellum due to osteochondritis dissecans. J Bone Joint Surg Am. 2012;94:992–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Singer KM, Roy SP. Osteochondrosis of the humeral capitellum. Am J Sports Med. 1984;12:351–360. [DOI] [PubMed] [Google Scholar]
- 31. Takahara M, Mura N, Sasaki J, Harada M, Ogino T. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. J Bone Joint Surg Am. 2007;89:1205–1214. [DOI] [PubMed] [Google Scholar]
- 32. Takahara M, Mura N, Sasaki J, Harada M, Ogino T. Classification, treatment, and outcome of osteochondritis dissecans of the humeral capitellum. Surgical technique. J Bone Joint Surg Am. 2008;90(suppl 2 pt 1):47–62. [DOI] [PubMed] [Google Scholar]
- 33. Uchida S, Utsunomiya H, Taketa T, et al. Arthroscopic fragment fixation using hydroxyapatite/poly-l-lactate acid thread pins for treating elbow osteochondritis dissecans. Am J Sports Med. 2015;43:1057–1065. [DOI] [PubMed] [Google Scholar]
- 34. van den Ende KI, McIntosh AL, Adams JE, Steinmann SP. Osteochondritis dissecans of the capitellum: a review of the literature and a distal ulnar portal. Arthroscopy. 2011;27:122–128. [DOI] [PubMed] [Google Scholar]
- 35. Zlotolow DA, Bae DS. Osteochondral autograft transplantation in the elbow. J Hand Surg Am. 2014;39:368–372. [DOI] [PubMed] [Google Scholar]


