Abstract
Study Design:
Retrospective study.
Objective:
To compare 2 methods of selecting the lowest instrumented vertebra (LIV) on the rates of revision surgery for distal junctional kyphosis (DJK) following treatment for Scheuermann’s kyphosis (SK).
Methods:
A retrospective review of patients who have undergone surgical treatment for SK was performed. Forty-four patients were divided into 2 groups based on intervention: Group 1 (n = 26) included patients who had an LIV distal to or at the sagittal stable vertebrae (SSV), and Group 2 (n = 18) included patients who had an LIV proximal to the SSV. For each group, demographic, radiographic, and revision surgery data was analyzed.
Results:
The average follow-up was 3.1 years. There were no differences among demographic variables between the groups. Preoperative and postoperative thoracic kyphosis, lumbar lordosis, and sagittal balance were not different between groups. Postoperatively, Group 1 demonstrated a significantly greater average lordotic disc angle below the LIV compared with Group 2 (Group 1, −6.2 ± 4.3° vs Group 2, −2.9 ± 5.8°; P = .02). In a subgroup analysis, extending fusions to the sagittal stable vertebra rather than the first lordotic disc resulted in fewer distal LIV complications necessitating revision surgery compared with fusing short of the SSV (5% vs 36.3%, P = .04).
Conclusion:
The SSV method may reduce complications secondary to distal junctional failure, but at the expense of incorporating additional motion segments in a typically young population.
Keywords: Scheuermann’s kyphosis, distal fusion level, first lordotic disc, sagittal stable vertebra, distal junctional kyphosis
Introduction
When selecting fusion levels for the operative management of Scheuermann’s kyphosis (SK), the optimal distal level historically utilized the lordotic discs after the transitional segment.1–3 However, due to the often large kyphosis, patients have compensatory hyperlordosis in the lumbar spine making it difficult to truly determine the first lordotic disc (FLD) level. Such a scenario can result in shorter fusions than necessary, resulting in distal junctional kyphosis (DJK) and sagittal decompensation. Indeed, the incidence of DJK following operative management of SK ranges from 5% to 50%1,4–7 and has fueled debate regarding the optimal distal fusion level. Previously, Cho et al4 reported their results of utilizing the sagittal stable vertebrae (SSV) concept in distal fusion level selection for patients with SK. The sagittal stable vertebra was defined as the most proximal vertebra touched by a line drawn vertically from the posterior superior corner of the sacrum on the lateral radiograph. In their analysis of 29 patients with SK, the incidence of DJK was significantly less (4% vs 71%) when the distal fusion level extended to the SSV instead of the FLD, which is typically proximal to the SSV. However, more than 40% of these patients had hook instrumentation at the lowest instrumented vertebra (LIV), which is a potential cause of junctional failure.6 Recent studies of DJK after all-pedicle screw fixation at the LIV have reported mixed results regarding the superiority of fusion to the SSV compared to above the SSV.7,8 The aim our study is compare the incidence of DJK in SK when the distal fusion is at or below the SSV versus above the SSV in posterior-only approaches. We hypothesize that fusing at or below the SSV will result in less DJK compared to fusing above the SSV and therefore will result in lower rates of revision surgery following posterior spinal fusions (PSFs) for SK.
Materials and Methods
A retrospective review of patients who have undergone surgical treatment for SK by 2 surgeons from 2 institutions between 2002 and 2010 was performed. Institutional review board approval was obtained at both sites. The 2 surgeons performed an approximately equal number of surgeries (54.5% vs 45.5%). All patients who underwent PSFs with segmental instrumentation and pedicle screw-only constructs via a posterior approach only at the LIV were included. The selection of the distal fusion level at the time of surgery was determined by the transitional area between the thoracic hyperkyphosis and lumbar lordosis, assessing the magnitude of lumbar lordosis, and the effect of thoracic kyphosis on reciprocal lumbar lordosis, which can affect the levels of lordotic discs. However, during the study period the authors did not have a defined algorithm for selection distal fusion level. Exclusion criteria included patients who underwent a combined anterior/posterior approach, patients who had incomplete radiographic data, and less than 2 years of follow-up.
Of the 50 patients who qualified for the study, 44 had at least 2 years of clinical and radiographic follow-up. The 44 patients were divided into 2 groups based on intervention: Group 1 (n = 26) included patients who had an LIV at or distal to the SSV (Figure 1), and Group 2 (n = 18) included patients who had an LIV above the SSV (Figure 2). For each group, the following characteristic data was analyzed: age, gender, fusion levels, instrumentation type, radiographic measurements, and duration of follow-up. Radiographic measurements were performed preoperatively, 4 to 8 weeks postoperatively, and at most recent follow-up and preoperative to most recent radiographs were utilized for analysis. The following radiographic parameters were collected: thoracic kyphosis (T2-T12), lumbar lordosis (L1-S1), sagittal balance, and disc angle. Sagittal balance was defined as the distance between the C7 plumb line (C7PL) and the posterosuperior endplate of S1 with a negative value indicating translation of the C7PL posteriorly to the sacrum. The disc angle was the angle subtended by a line paralleling the caudal endplate of the LIV and the cranial endplate of the subjacent vertebra. All radiographs were examined for DJK, which was the resultant angle between the caudal endplate of the LIV to the caudal endplate of the subjacent vertebra. DJK was confirmed (1) when the measured angle was greater than 10° and at least 10° greater than the preoperative measurement or (2) if the disk distal to the instrumentation changed from lordosis preoperatively to neutral or kyphosis postoperatively. All lateral radiographs were obtained on 36-inch-long cassettes in a standardized fashion with the patients’ hips and knees extended, arms positioned at a 45° angle in front of the body, and both hands resting on the clavicles. A comparison of demographics, pre- and postoperative radiographic parameters, and complications including revision surgery was performed between groups.
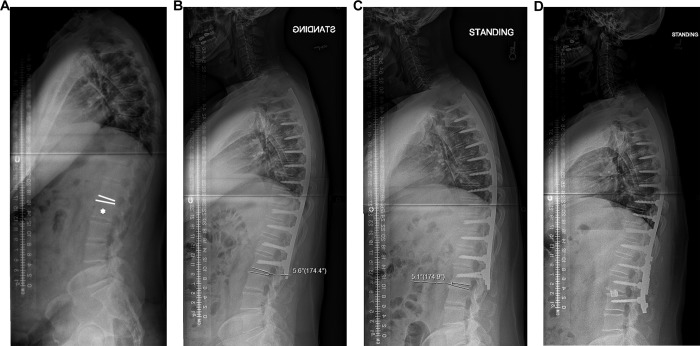
Figure 1.

Lateral standing radiograph of a 21-year-old male with Scheuermann’s kyphosis demonstrating the SSV as defined by a vertical line drawn from the posterosuperior corner of S1. L2 is marked by the “*” and represents the distal fusion level.
Figure 2.
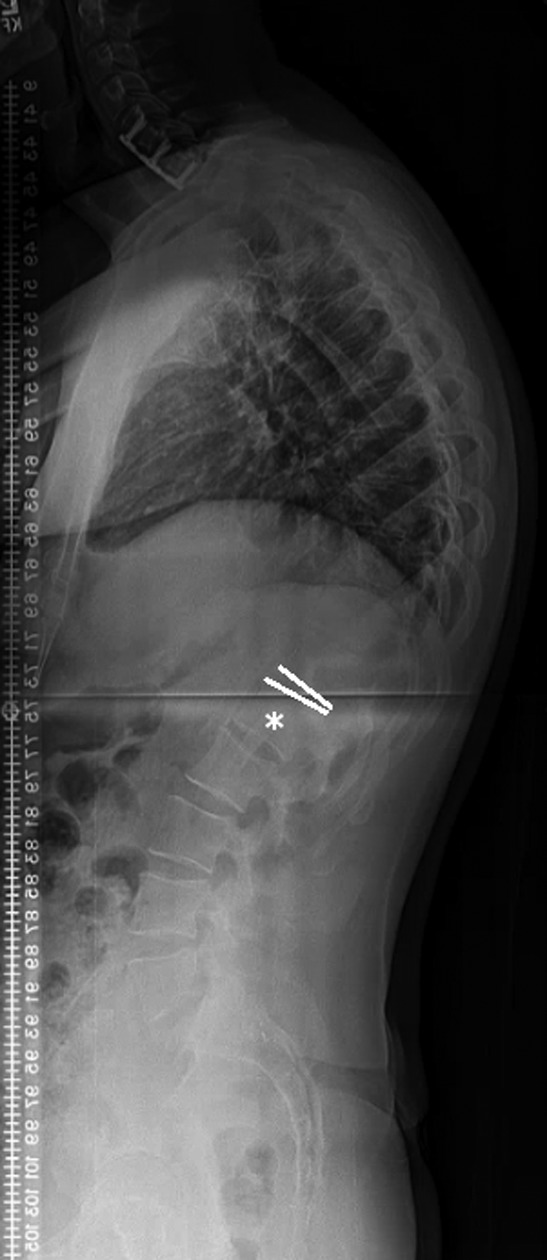
Lateral standing radiograph of a 33-year-old male with Scheuermann’s kyphosis. According to the first lordotic disc method, the distal fusion level (L1) is the vertebra subjacent to the FLD and marked by the “*” in this image.
A subgroup analysis was performed between patients who were fused at or below the SSV and patients whose LIV corresponded to the FLD. This analysis was performed in order to compare more distal (SSV) fusion levels to more proximal (FLD) fusion levels. Thus, for this analysis all patients in which the FLD and the SSV corresponded to the same level were excluded. Rates of DJK between patients whose fusion level was selected via the SSV method (Group A) versus the FLD method (Group B = LIV equal to the FLD) were compared. Complications between the different LIVs were compared with respect to requirement for revision surgery. The decision to perform revision surgery for DJK was based on clinical symptoms and progressive kyphosis. Comparisons between the 2 groups were performed by using the Fischer exact t test. Statistical significance was defined as a P < .05.
Results
Demographic Data
Demographic information is summarized in Table 1. Forty-four patients with SK underwent PSF with pedicle screw-only fixation at the LIV. Patients in Group 1 underwent surgery at an average age of 17.8 ± 4.8 years, and patients in Group 2 underwent surgery at an average age of 20.5 ± 9.6 years. The average follow-up was 3.1 years (range = 2.0-8.1). There were no statistically significant differences among demographic variables between the groups.
Table 1.
Demographic Data for Both Groups.
| Group 1 (n = 26) | Group 2 (n = 18) | P | |
|---|---|---|---|
| Age (years) | 17.8 ± 4.8 | 20.5 ± 9.6 | .26 |
| Gender | .35 | ||
| Male | 18 | 11 | |
| Female | 8 | 7 | |
| Follow-up (years) | 3.5 ± 1.5 | 3.16 ± 1.7 | .64 |
Abbreviations: LIV, lowest instrumented vertebra; SSV, sagittal stable vertebrae; Group 1, LIV distal to or at the SSV; Group 2, LIV proximal to the SSV.
Radiographic Results
Radiographic data is summarized in Table 2. Preoperative and postoperative thoracic kyphosis, lumbar lordosis, and sagittal balance were not significantly different between groups (P > .05). In Group 1, mean thoracic kyphosis improved from 82.5 ± 12.9° preoperatively to 49.6 ± 13.5° at most recent follow-up, representing a 39.9% curve correction. In Group 2, mean thoracic kyphosis improved from 80.6 ± 13.2° preoperatively to 45.8 ± 6.9° at most recent follow-up, representing a 43.2% curve correction. Posterior translation of C7 relative to the sacrum was observed in both groups. In Group 1, sagittal balance measured −2.8 mm prior to surgery and −8.2 mm at follow-up. In Group 2, sagittal balance changed from 11.1 mm prior to surgery to −5.8 mm at final follow-up. The average lordotic disc angle below the LIV was similar between groups preoperatively; however, disc angle between Groups 1 and 2 at most recent follow-up was significantly different. Postoperatively, Group 1 demonstrated a significantly greater average lordotic disc angle below the LIV compared to Group 2 (Group 1, −6.2 ± 4.3° vs Group 2, −2.9 ± 5.8°; P = .02; Table 2). One of 26 (3.8%) patients in Group 1 and 6 of 18 (33.3%) patients in Group 2 had radiographic evidence of DJK.
Table 2.
Preoperative and Postoperative Radiographic Parameters.a
| Group 1 | Group 2 | P | |
|---|---|---|---|
| Preoperative | |||
| Thoracic kyphosis (°) | 82.5 ± 12.9 | 80.6 ± 13.2 | .7 |
| Lumbar lordosis (°) | 75.0 ± 15.8 | 70.0 ± 19.6 | .52 |
| Sagittal balance (mm) | −2.8 | 11.1 | .41 |
| Disc angle below LIV (°) | −9.9 ± 6.0 | −8.6 ± 5.1 | .44 |
| Postoperative | |||
| Thoracic kyphosis (°) | 49.6 ± 13.5 | 45.8 ± 6.9 | .41 |
| Curve correction (%) | 39.9 | 43.2 | |
| Lumbar lordosis (°) | 61.7 ± 14.0 | 55.0 ± 16.2 | .21 |
| Sagittal balance (mm) | −8.2 | −5.8 | .82 |
| Disc angle below LIV (°) | −6.2 ± 4.3 | −2.9 ± 5.8 | .02 |
Abbreviation: LIV, lowest instrumented vertebra.
aSignificant values (P < .05) are in bold.
For purposes of evaluating differences in revision rates secondary to DJK, a subgroup analysis of the lordotic disc method (when the lordotic disc was the distal fusion level) and the SSV method (extension of fusion to the stable vertebra) was performed (Table 3). Of the original cohort of 44 patients (26 from Group 1 and 18 from Group 2), 13 patients were excluded because the SSV and FLD corresponded to the same vertebral level. Of the remaining 31 patients, 20 had an LIV equal to the SSV (Group A) and 11 had an LIV equal to the FLD (Group B). Five of 31 patients in the subgroup analysis underwent revision surgery because of DJK: 5% in Group A and 36.3% in Group B (P = .04). Five of 28 (17.9%) patients in Group 1 had radiographic evidence of proximal junctional kyphosis (PJK), compared to 1 of 16 (6.3%) in Group 2 (P = .02).
Table 3.
Rates of Revision Surgery for Distal Junctional Kyphosis.
| Total, n (%) | Group A, n (%) | Group B, n (%) | P | |
|---|---|---|---|---|
| DJK | 5 (16.1) | 1 (5.0) | 4 (36.3) | .04 |
Abbreviations: DJK, distal junctional kyphosis; Group A, distal fusion level equal to sagittal stable vertebrae (n = 20); Group B, distal fusion level equal to first lordotic disc (n = 11).
Discussion
Fusing at or below the SSV results in a lower incidence of DJK compared to fusing above the SSV. Additionally, our subgroup analysis demonstrates that extending the distal fusion level to the SSV, rather than fusing to the FLD, resulted in a significantly lower incidence of distal junctional failure requiring revision surgery (5% vs 36.3%, P = .04) in SK patients who underwent PSF with modern techniques. The difference in distal fusion level did not affect the degree of kyphosis correction, which should not exceed 50% of the initial deformity because of an increased risk of proximal and distal junctional failure.1 Additionally, fusion at or below the SSV resulted in the maintenance of a greater lordotic disc angle at an average follow-up of more than 3 years. Previous studies on distal fusion levels for SK patients have reported rates of DJK as high as 50%1,4–7; however, other studies have included anterior-posterior approaches,4–7,9 non-pedicle screw instrumentation techniques,4–6,9 postoperative cast immobilization,5 LIVs proximal to the FLD,6 mixed etiologies of hyperkyphosis,4,7 and patients with less than 2 years of follow-up.2,7 Our study reflects a homogeneous sample of SK patients who underwent posterior-only surgery, all-pedicle screw instrumentation at the LIV, fusion to the FLD or distally, and a minimum follow-up of 2 years.
The ideal distal fusion level is controversial in coronal and sagittal plane deformities.4,8,10 The stable vertebra in scoliosis, which is the most cranial vertebra bisected by the central sacral vertical line, is often designated as the LIV unless the presumed end level is kyphotic or degenerative. In primary kyphotic deformities, the SSV concept can be important for determining the LIV as well. In 2009, Cho et al4 published their results of 29 patients with SK who were fused to either the FLD or SSV. The authors recommended inclusion of the SSV in the fusion because patients whose fusions ended at the FLD developed significantly higher rates of distal junction problems (8% vs 71%, P < .05) including DJK and implant loosening. However, distal junctional complications occurred in 38% of hook and only 11% of pedicle screw constructs, limiting the applicability of their results to patients who are treated with pedicle screws-only at the LIV. An analysis of risk factors for PJK and DJK has suggested that hooks predispose the spine to junctional kyphosis as a result of disruption of the ligamentum flavum.6 Another criticism of the study by Cho et al4 is that they did not include a group in which the LIV and the FLD were the same level.8 Our article includes patients in whom the LIV and FLD correspond to the same level and confirms the findings of Cho et al4 with current-day instrumentation techniques and a larger patient cohort.
Lundine et al7 assessed the incidence of DJK in 22 SK patients who underwent anterior release and posterior instrumentation to either the SSV or FLD with all-pedicle screw constructs in the distal segments. In their study, DJK was defined as any disk distal to the instrumentation that was lordotic prior to surgery and became neutral or kyphotic after surgery. In 12 patients, the SSV was distal to the FLD; the SSV and FLD corresponded to the same level in the remaining 10 patients. The rate of DJK was greater in patients who were fused to the FLD compared to the SSV (38% vs 11%) and even greater if the LIV was proximal to the FLD or SSV (83% vs 71%, respectively). According to logistic regression analysis, fusion to the FLD rather than the SSV was 4 times more likely to result in DJK. However, the primary outcome of Lundine et al7 was DJK, which is a radiographic diagnosis and may not accurately represent distal junctional failure, which is the clinical corollary and often necessitates revision surgery. For instance, 7 (63.6%) patients with DJK were clinically asymptomatic and did not require revision surgery in the study by Lundine et al.7 In our study, we included a subgroup analysis regarding the rate of revision surgery because many patients with DJK do not require surgical intervention,6–8,11 and we found a significantly higher requirement for revision surgery when the LIV was proximal to the SSV (Figure 3).
Figure 3.
A 50-year-old male with Scheuermann’s kyphosis who underwent fusion to L2, the first lordotic disc (*) and had 5.6° lordosis of disc angle postoperatively (A and B). At 6 months postoperatively, the patient developed significant pain located at the L2-3 level, which severely limited his daily activities. A radiograph at that time demonstrated 5° of kyphosis at the L2-3 interspace (C), representing a 10° change of disc angle from “B.” He underwent extension of fusion to L3 (D).
Recently, Yanik et al8 found that extension to the SSV is unnecessary. Rather, the authors proposed that fusion to the FLD results in comparable rates of DJK and has the advantage of saving fusion levels. In their study, 3 groups were compared based on the distal fusion level (LIV = SSV, LIV = FLD, and SSV = FLD). Sagittal balance, lumbar lordosis, pelvic parameters, and SF-36 scores were similar between groups before and after surgery. Eleven of 54 patients developed DJK, and the incidence was similar in all groups (P > .05). None of the patients required revision surgery. The authors hypothesized that one of the reasons for the similar outcomes between groups was the preservation of lumbar lordosis within physiologic range, citing the risk of distal junctional failure in the setting of hypolordosis after SK correction. We report contrasting findings even in the presence of similar postoperative lordosis between groups despite that our study and that of Yanik et al8 analyzed similar patient cohorts who were treated by similar techniques. Yanik et al8 stated that fusing to the first lordotic vertebra (FLV), if proximal to the SSV, has the advantage of saving fusion levels. Although PSFs extending to L4 or L5 may cause adjacent segment degenerative disc disease,12–14 minimal degeneration occurs with fusions ending more proximally.15,16 Green et al15 reviewed magnetic resonance imaging scans of 20 scoliosis patients who were followed for an average of 11.8 years after PSF. Comparison of subgroups between LIV = T12 or L1 and LIV = L3 found no significant differences in Pfirrmann scores (a reliable measure of disc degeneration using magnetic resonance imaging17) at any caudal disc level, SRS-22R, or Oswestry Disability Index scores. Therefore, the benefit of fusing short of the SSV may not outweigh the risk of DJK and risk for revision surgery.
Limitations of our study include small patient sample and retrospective design. Although only 44 patients were included, this is more than4,7,9 or similar to8 prior studies. Another weakness is our average follow-up of only 3.1 years. Additional patients may develop DJK at longer follow-up, but prior studies have reported substantial rates of DJK after only a minimum of 2 years,4,7,8,11 which indicates that DJK occurs early in the postoperative period. A further limitation of our study is the lack of measurements pertaining to spinopelvic parameters, which would provide additional information for the evaluation of spinal alignment. Last, our study did not include analyses of the surgical techniques of the 2 surgeons who performed all of the operations; surgical strategies may have affected DJK rates. Despite these limitations, our study is strengthened by the use of modern, consistent surgical techniques (all-pedicle screw instrumentation and posterior-only fusion); analysis of revisions secondary to DJK, thereby avoiding the inclusion of clinically asymptomatic kyphosis; and reporting of the lordotic disc angle below the LIV, which was significantly different between groups and may be a harbinger for distal junctional failure.
Conclusion
The importance of the SSV for LIV selection specific to SK lies in the compensatory measures that the other regions of the spine take in order to maintain sagittal balance in the setting of hyperkyphosis. Specifically, the lumbar and cervical spine will become hyperlordotic in order to compensate for the thoracic hyperkyphosis.18,19 This can result in a false sense of the true “lordotic” disc level because the lordosis is exaggerated, thus making an otherwise parallel level or even slightly kyphotic disc level appear to be lordotic. Ultimately, this can lead to the suboptimal selection of the distal fusion level and an overall short fusion, thereby causing DJK, screw pullout, loss of fixation, and/or decompensation necessitating revision surgery. Indeed, when fusions were extended to the SSV rather than the more proximal FLD, the number of revision surgeries for DJK was significantly less (5% vs 36.3%, P = .04). The SSV method may reduce complications secondary to distal junctional failure, but at the expense of incorporating additional motion segments in a typically young population.
Footnotes
Authors’ Note: Institutional review board approval was obtained for this study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Lowe TG, Kasten MD. An analysis of sagittal curves and balance after Cotrel-Dubousset instrumentation for kyphosis secondary to Scheuermann’s disease. A review of 32 patients. Spine (Phila Pa 1976). 1994;19:1680–1685. [DOI] [PubMed] [Google Scholar]
- 2. Taylor TC, Wenger DR, Stephen J, Gillespie R, Bobechko WP. Surgical management of thoracic kyphosis in adolescents. J Bone Joint Surg Am. 1979;61:496–503. [PubMed] [Google Scholar]
- 3. Otsuka NY, Hall JE, Mah JY. Posterior fusion for Scheuermann’s kyphosis. Clin Orthop Relat Res. 1990;(251):134–139. [PubMed] [Google Scholar]
- 4. Cho KJ, Lenke LG, Bridwell KH, Kamiya M, Sides B. Selection of the optimal distal fusion level in posterior instrumentation and fusion for thoracic hyperkyphosis: the sagittal stable vertebra concept. Spine (Phila Pa 1976). 2009;34:765–770. [DOI] [PubMed] [Google Scholar]
- 5. Bradford DS, Ahmed KB, Moe JH, Winter RB, Lonstein JE. The surgical management of patients with Scheuermann’s disease: a review of twenty-four cases managed by combined anterior and posterior spine fusion. J Bone Joint Surg Am. 1980;62:705–712. [PubMed] [Google Scholar]
- 6. Denis F, Sun EC, Winter RB. Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: minimum five-year follow-up. Spine (Phila Pa 1976). 2009;34:E729–E734. [DOI] [PubMed] [Google Scholar]
- 7. Lundine K, Turner P, Johnson M. Thoracic hyperkyphosis: assessment of the distal fusion level. Global Spine J. 2012;2:65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Yanik HS, Ketenci IE, Coskun T, Ulusoy A, Erdem S. Selection of distal fusion level in posterior instrumentation and fusion of Scheuermann kyphosis: is fusion to sagittal stable vertebra necessary? Eur Spine J. 2016;25:583–589. [DOI] [PubMed] [Google Scholar]
- 9. Mikhaylovskiy MV, Sorokin AN, Novikov VV, Vasyura AS. Selection of the optimal level of distal fixation for correction of scheuermann’s hyperkyphosis. Folia Med. 2015;57:29–36. [DOI] [PubMed] [Google Scholar]
- 10. Trobisch PD, Ducoffe AR, Lonner BS, Errico TJ. Choosing fusion levels in adolescent idiopathic scoliosis. J Am Acad Orthop Surg. 2013;21:519–528. [DOI] [PubMed] [Google Scholar]
- 11. Lonner BS, Newton P, Betz R, et al. Operative management of Scheuermann’s kyphosis in 78 patients: radiographic outcomes, complications, and technique. Spine (Phila Pa 1976). 2007;32:2644–2652. [DOI] [PubMed] [Google Scholar]
- 12. Edwards CC, 2nd, Bridwell KH, Patel A, et al. Thoracolumbar deformity arthrodesis to L5 in adults: the fate of the L5-S1 disc. Spine (Phila Pa 1976). 2003;28:2122–2131. [DOI] [PubMed] [Google Scholar]
- 13. Kuhns CA, Bridwell KH, Lenke LG, et al. Thoracolumbar deformity arthrodesis stopping at L5: fate of the L5-S1 disc, minimum 5-year follow-up. Spine (Phila Pa 1976). 2007;32:2771–2776. [DOI] [PubMed] [Google Scholar]
- 14. Harding IJ, Charosky S, Vialle R, Chopin DH. Lumbar disc degeneration below a long arthrodesis (performed for scoliosis in adults) to L4 or L5. Eur Spine J. 2008;17:250–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Green DW, Lawhorne TW, 3rd, Widmann RF, et al. Long-term magnetic resonance imaging follow-up demonstrates minimal transitional level lumbar disc degeneration after posterior spine fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2011;36:1948–1954. [DOI] [PubMed] [Google Scholar]
- 16. Rinella A, Bridwell K, Kim Y, et al. Late complications of adult idiopathic scoliosis primary fusions to L4 and above: the effect of age and distal fusion level. Spine (Phila Pa 1976). 2004;29:318–325. [DOI] [PubMed] [Google Scholar]
- 17. Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976). 2001;26:1873–1878. [DOI] [PubMed] [Google Scholar]
- 18. Jansen RC, van Rhijn LW, van Ooij A. Predictable correction of the unfused lumbar lordosis after thoracic correction and fusion in Scheuermann kyphosis. Spine (Phila Pa 1976). 2006;31:1227–1231. [DOI] [PubMed] [Google Scholar]
- 19. Wood KB, Melikian R, Villamil F. Adult Scheuermann kyphosis: evaluation, management, and new developments. J Am Acad Orthop Surg. 2012;20:113–121. [DOI] [PubMed] [Google Scholar]