Abstract
Background
Studies report high burnout prevalence among resident physicians, with little consensus on methods to effectively reduce it.
Objective
This systematic literature review explores the efficacy of interventions in reducing resident burnout.
Methods
PubMed, Embase, and Web of Science were searched using these key words: burnout and resident, intern, or residency. We excluded review articles, editorials, letters, and non–English-language articles. We abstracted data on study characteristics, population, interventions, and outcomes. When appropriate, data were pooled using random effects meta-analysis to account for between-study heterogeneity. Study quality was assessed using Newcastle-Ottawa Scale (cohort studies) and Jadad scale (randomized control trials [RCTs]).
Results
Of 1294 retrieved articles, 19 (6 RCTs, 13 cohort studies) enrolling 2030 residents and examining 12 interventions met criteria, with 9 studying the 2003 and 2011 Accreditation Council for Graduate Medical Education (ACGME) duty hour restrictions. Work hour reductions were associated with score decrease (mean difference, −2.73; 95% confidence interval (CI) −4.12 to −1.34; P < .001) and lower odds ratio (OR) for residents reporting emotional exhaustion (42%; OR = 0.58; 95% CI 0.43–0.77; P < .001); a small, significant decrease in depersonalization score (−1.73; 95% CI −3.00 to −0.46; P = .008); and no effect on mean personal accomplishment score (0.93; 95% CI −0.19–2.06; P = .10) or for residents with high levels of personal accomplishment (OR = 1.01; 95% CI 0.67–1.54; P = .95). Among interventions, self-care workshops showed decreases in depersonalization scores, and a meditation intervention reduced emotional exhaustion.
Conclusions
The ACGME work hour limits were associated with improvement in emotional exhaustion and burnout.
Introduction
Burnout is a syndrome resulting from work-related stress and can be characterized by emotional exhaustion (feeling overwhelmed by job demands and depletion of emotional resources); depersonalization (feelings of cynicism and detachment toward patients); and reduced personal accomplishment (decline in feelings of work competence and achievement).1
The prevalence of burnout is greater among residents and fellows than it is among medical students, physicians, or college graduates of similar age.2 Combined estimates of burnout prevalence among residents range from 40% to 80%, depending on the specialty.2 Several stressors are associated with burnout, such as situational stressors (work hours, sleep deprivation, and staff conflicts); personal stressors (conflicts with family or friends, financial difficulties, or moving to a new city); and professional stressors (patient responsibilities, teaching or supervisory responsibilities, and information overload and other special situations).3
Medical educators struggle with determining appropriate methods to effectively address burnout among residents. While interventions have been implemented by some training programs to mitigate burnout, the medical education community would benefit from more evidence on the efficacy and generalizability of those interventions, and from the development of standardized methods for early identification of burnout and prompt intervention.
The most recent systematic review examining interventions for burnout among residents was limited by inclusion of few studies and a lack of pooling of the results.4 Our goal was to summarize current evidence and systematically review various interventions and their effect on burnout rates among residents.
Methods
We searched the PubMed (National Center for Biotechnology Information, Bethesda, MD), Embase (Elsevier, Amsterdam, the Netherlands), and Web of Science (Clarivate Analytics, New York, NY) databases from their inception using the following key words: burnout and (resident or intern or residency). Two reviewers independently evaluated and screened for relevant articles in 3 successive stages: review of titles, review of abstracts, and review of full-text articles (Figure 1). We included studies that presented original data, enrolled residents, had identifiable intervention with follow-up results, and were published in English-language, peer-reviewed medical journals. We excluded editorials, letters to the editor, and abstracts.
Figure 1.
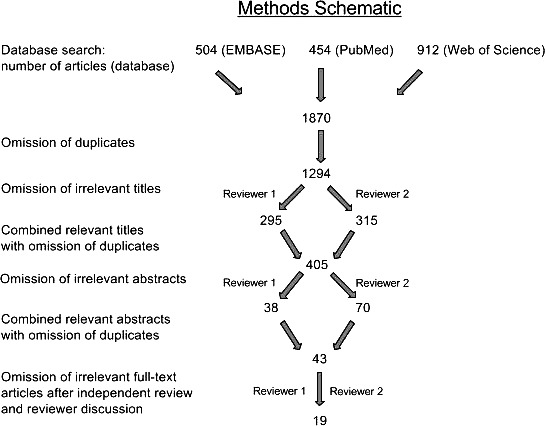
Flowchart of Literature Search
Data Extraction and Quality Assessment
We extracted data on study characteristics, characteristics of the enrolled population, intervention(s), extent of burnout, method of measuring burnout, and reported outcomes. The outcome of interest was change in the reported burnout rate or domains of burnout among residents in response to an intervention. Studies were grouped according to the intervention used to reduce resident burnout. Data were abstracted by 1 investigator (K.R.B.) and corroborated by a second investigator (J.A.M.). Disagreements between the 2 investigators were adjudicated by a third investigator (R.Q.).
Study quality was assessed using the Newcastle-Ottawa Scale (NOS; Ottawa Hospital, Ottawa, ON) for cohort studies and the Jadad scale (University of Oxford, Oxford, England) for randomized, controlled trials; that scoring was not used to exclude the articles.5,6 The NOS uses 2 tools for case control and cohort studies and encompasses 3 quality parameters: selection, comparability, and exposure/outcome assessment. It assigns a maximum of 4 points for selection, 2 points for comparability, and 3 points for exposure or outcome (for a total of up to 9 points). The NOS scores of 7 or higher were considered high-quality studies, and scores of 5 to 6 denoted moderate quality.6 The Jadad scale bases the quality of studies on descriptions of randomization, blinding, and dropouts (withdrawals). The Jadad scale ranges from 0 to 5 points, with a score of 2 or less indicating a low-quality report and a score of 3 or more indicating a high-quality report.5
Data Synthesis
Of the 1870 articles identified through our search strategy, 19 studies (6 randomized control trials [RCTs] and 13 cohort studies) fulfilled our inclusion and exclusion criteria (Figure 1). Most studies were from the United States (n = 16); 1 study each was from Canada,7 Belgium,8 and Israel.9
We pooled data from the 9 studies that examined the effect of work hour limits on burnout rates using random effects meta-analysis that accounted for between-study heterogeneity.7,10–17 The studies reported data in different forms; when studies reported data on the number (or percentage) of residents with high levels of burnout, we pooled their odds ratios (ORs), and when studies reported mean burnout scores, we pooled their mean differences. Six of the 9 studies reported data on all or some components of the Maslach Burnout Inventory (MBI; Mind Garden, Menlo Park, CA), and data were pooled within those components. The components were emotional exhaustion, depersonalization, and personal accomplishment. The personal accomplishment component is a reverse scale, with higher scores indicating less burnout. Two studies reported data for overall burnout only, and data from those studies were pooled separately. One study reported data using the Universal Tedium Index (Mediocre Laboratories, Carrollton, TX).
Between-study heterogeneity was assessed by standard χ2 tests and the I2 statistic. The influence of individual studies on the overall prevalence estimate was examined by serially excluding each study in a sensitivity analysis. Publication bias was assessed by visual examination of the funnel plots. All statistical tests were 2-sided, and a P < .05 was considered significant.
Results
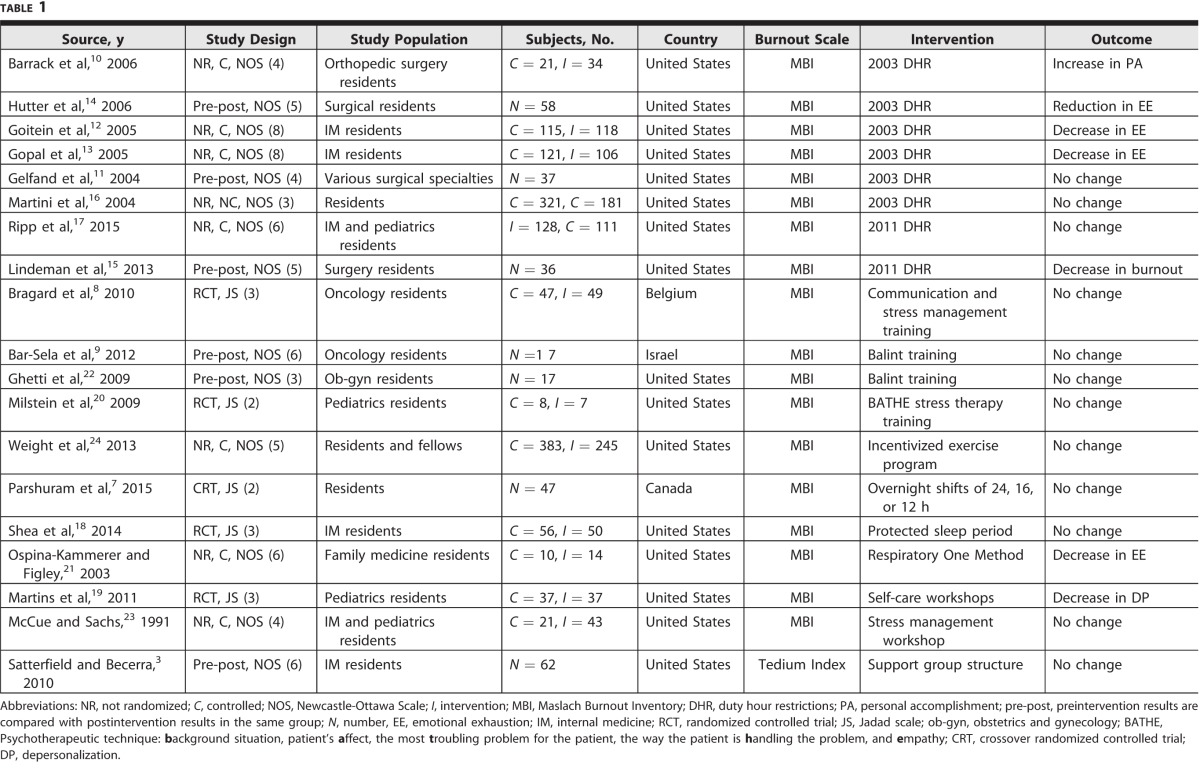
Of the 1870 articles identified through our search, 19 studies (6 RCTs and 13 cohort studies) met the inclusion criteria (Figure 1). The interrater reliability between the 2 raters was good (κ = 0.79 for titles and 0.66 for abstracts). Most studies were from the United States (n = 16), and 1 study each was from Canada,7 Belgium,8 and Israel.9 Internal medicine residents were the subject 4 studies3,12,13,18; 1 study of orthopedic residents10; 2 studies of pediatrics residents19,20; 1 study of family medicine residents21; 1 study of obstetrics and gynecology residents22; 3 studies of surgical specialty residents11,14,15; 2 studies of oncology residents8,9; and 5 studies enrolled residents from a combination of residency programs.7,16,17,23,24 The studies included enrolled 2030 residents, and examined the effect of 12 different strategies on resident burnout (Table 1).
Table 1.
Characteristics of Studies Included in the Systematic Review
Work hour limits, particularly the Accreditation Council for Graduate Medical Education (ACGME) 2003 and 2011 duty hour restrictions, was the most commonly studied intervention (9 studies). To measure resident burnout, 18 studies used the MBI, and 1 used the Tedium Index. Of the 14 observational studies that were assessed using the NOS (provided as online supplemental material), 2 were rated high quality,12,13 and 7 were rated as being of moderate quality.3,9,14,15,17,21,24 Of the 5 RCTs that were assessed using the Jadad scale (Table 1), 3 were rated high quality8,18,19 (score ≥ 3), and the remaining 2 were rated to be of moderate quality.
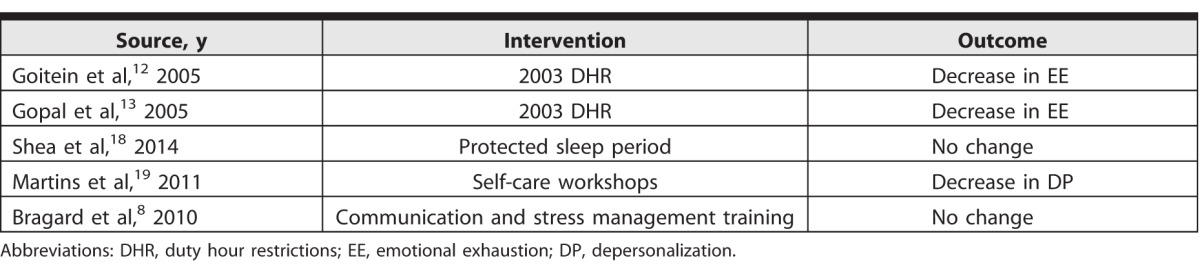
Two high-quality studies, as judged by the NOS, showed that the 2003 work hour limits did not affect burnout rates for internal medicine residents.9,10 For 3 high-quality RCTs, as judged by the Jadad scale, protected sleep periods18 and communication and stress management8 had no effect on burnout rates. Self-care workshops resulted in a decrease in the depersonalization component of burnout.19 The outcomes for high-quality studies are summarized in Table 2.
Table 2.
Results of High-Quality Studies
Qualitative Synthesis of Data
Of the 9 studies that examined the effect of work hour limits, 8 studied the effect of the ACGME standards, and 1 randomized residents in an intensive care setting to 24-hour rotations versus a limit of 12 or 16 hours.7 Seven studies reported on emotional exhaustion and depersonalization,7,10–14,17 6 on personal accomplishment,7,10–14 and 2 on overall burnout.15,16 Several studies reported on more than 1 dimension of the MBI. Improvement in emotional exhaustion was reported in 4 studies,12–14,21 improvement in depersonalization was reported in 1 study,19 and improvements in personal achievement was reported in 1 study.10 Only 1 of the 2 studies reported the overall burnout score and significant improvement, although the direction of the effect was the same in both studies.15,16
Three studies examined the effect of stress management workshops on resident burnout, with 2 studies reporting that it did not result in reduction in the burnout components.8,20 The third study did not provide sufficient data to detect whether the results were significantly different than one would see by chance.23 A stress therapy training did not show a significant decrease in burnout as physicians were too busy to implement the entire tool systematically, and the sample size (n = 7) also was too small to allow significance testing of results.20 In another study, the lack of a positive effect on burnout rates after communication and stress management training may be because it takes longer to analyze the effects of such training than the time accounted for in the study.8 Two studies examined the effect of Balint-type case discussion groups (designed to improve physician communication skills with a focus on patient-physician interactions).9,22 Both studies were limited by small sample sizes (n = 17), and the positive effect of Balint training on burnout rates may be related to resident bonding during training, which contrasted with the intervention itself.9,22
The effect of meditation (the Respiratory One Method) on the emotional exhaustion component of the MBI was examined in 1 study, and found a statistically significant decrease in the emotional exhaustion domain of the treatment group compared with that of the control group (−2.71 versus 3.8, P < .05).21 Another study qualitatively assessed the role of the monthly support group meetings on resident burnout, finding improvement in burnout with training and noting the critical importance of peer relationships as a source of support during training.3 An incentivized, 12-week exercise program was examined with 1060 participants that resulted in a decrease in resident and fellow burnout rates in all 3 components of the MBI, although the changes were not statistically significant.24
Quantitative Synthesis of Data
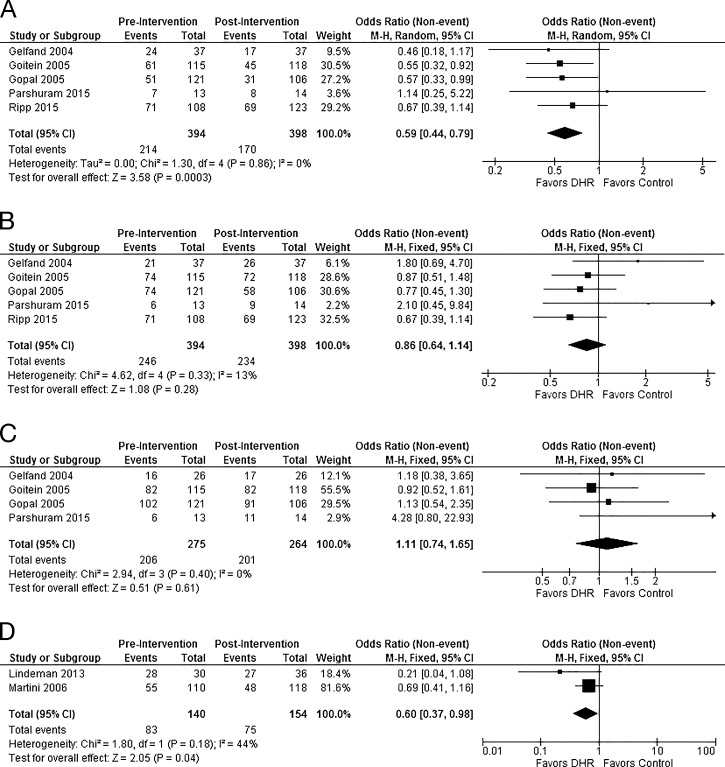
We pooled the 9 studies that examined the effect of work hour limits on resident burnout. The reduction of resident hours was associated with a 42% lower odds of the percentage of residents reporting high levels of the emotional exhaustion component (OR = 0.59; 95% confidence interval [CI] 0.45–0.79; P < .001; Figure 2A) and a decrease in the mean burnout score (mean difference, −2.70; 95 CI −3.98 to −1.41; P < .001; provided as online supplemental material). Work hour limits had no effect on the number of residents with a high level of depersonalization (OR = 0.86; 95% CI 0.64–1.14; P = .28; Figure 2B), although there was a small, but statistically significant, decrease in mean depersonalization score (mean difference, −1.43; 95% CI −2.54 to −0.31; P = .010; provided as online supplemental material). There was no effect of the limits of the mean personal accomplishment score (mean difference, 0.99; 95% CI −0.04–2.02; P = .06) or on the number of residents with high levels of personal accomplishment (OR = 1.11; 95% CI 0.74–1.65; P = .61; Figure 2C and provided as online supplemental material). Pooling the results from the 2 studies that examined the overall MBI scores found that work hour limits were associated with a 40% lower odds of residents reporting high levels of overall burnout (OR = 0.60; 95% CI 0.37–0.98; P = .040; Figure 2D). The I2 statistic for heterogeneity between the studies varied from 0%, for some outcomes, to up to 45% (Figure 2 and provided as online supplemental material). We did not find evidence of a publication bias on visual examination of funnel plots.
Figure 2.
Effect of Work Hour Limits on Resident Burnout: (A) Emotional Exhaustion (Number of Residents Reporting High Levels); (B) Depersonalization (Number of Residents Reporting High Levels); (C) Personal Accomplishment (Number of Residents Reporting High Levels); (D) Overall Burnout Rate (Number of Residents Reporting High Levels)
Note: The square data markers indicate odds ratios (ORs) from primary studies, with sizes reflecting the statistical weight of the study using random-effects meta-analysis. The horizontal lines indicate 95% confidence intervals (CIs). The diamond data markers represent the subtotal and overall OR and 95% CI. The vertical line shows the line of no effect (OR = 1). Abbreviations: CHI2, chi-square; df, degrees of freedom; Z, test of overall effect; P, probability value; DHR, duty hour restrictions.
Discussion
In this systematic review and meta-analysis of 19 studies enrolling 2030 residents, we found that 1 intervention, limiting resident hours, was consistently associated with a decreased emotional exhaustion component of burnout12–14,21 and lower overall burnout rates.15 Other interventions were examined in a few studies that enrolled small numbers of residents. Overall, those studies did not find any decrease in resident burnout rates, except for 2 studies, which used meditation and self-care workshops as interventions.19,21
In our analysis, we observed that the main limitations of studies on the effect of interventions on resident burnout were small sample size and research being conducted within a single residency program. Those limitations make generalizability among varying specialties and residency work environments difficult. Further, the outcome of the studies was complicated by the inherently subjective nature of postintervention surveys.
Our analysis found that the 2003 ACGME work hour standards were associated with significant reductions in emotional exhaustion scores for surgical and internal medicine residents12–14 and an improvement in personal accomplishment scores for orthopedic residents.10 The 2011 standards were associated with significant decreases in burnout rates for surgery residents but not for internal medicine residents.17 However, the 2011 standards also were associated with interns reporting a decreased sense of readiness for more senior roles and with reported added burdens and reduced quality of life for senior residents.25 A recent systemic review demonstrated that focusing on duty hours alone did not result in improvements in patient care or resident well-being and may have had a negative effect on resident education.26
While work hour limits appear to be effective in reducing burnout rates among resident physicians, further restrictions in work hours may result in the inadequate training of physicians or the lengthening of an already long training period. Some other interventions to address burnout have been suggested, including supportive interventions for internal medicine residents.3 Identifying challenges faced by trainees at different levels and across different specialties may assist in improved, effective tailoring of interventions. For example, 1 study found a significant correlation among burnout rates, peer relationships, and interventions aimed at improving peer relationships, which may reduce burnout in resident physicians.27
One high-quality RCT study, which examined this aspect using self-care workshops, centered around the discussion of the negative effects of burnout on professional activity, the recognition of risk factors for burnout, and tools to cope with burnout. While it resulted in significant improvement in depersonalization, other MBI subcategories were not affected.19
Conditions for burnout may be more related to the characteristics of the learning environment along with those of individuals.28 Interventions may involve such factors as removing excessively burdensome work schedules, increasing trainees' sense of control over their work, increasing recognition of their work contribution, ensuring a clear division of roles, and creating a sense of justice.29
Other strategies examined in this review showed little evidence of effectiveness. This may be related to the fact that interventions may be perceived as “adding” burden to residents' lives. There may be benefit found in interventions that remove certain tasks and burdens from resident work, particularly nonclinical and non–educationally relevant tasks.
A recent systematic review and meta-analysis found that individual-focused and structural and organizational strategies were effective in reducing burnout among physicians.30 However, the optimum combination of individual- and organization-focused interventions to improve physician well-being remains to be investigated.
Our study has some limitations. While we performed an extensive search of peer-reviewed literature, it is possible that our search missed some articles. Although we did not find any evidence of publication bias, it remains a possibility.
Further research is needed to assess efforts to improve residents' learning climate, as well the benefits of physical activity, meditation, and other wellness interventions.
Research is also needed to identify optimal ways to equip residents with the proper tools for managing workload and personal and professional stressors, and to effectively identify and mitigate burnout. Finally, several prospective, randomized trials currently underway of different work hour limits may shed additional light onto the relationship between resident hours and burnout.
Conclusion
The ACGME work hour limits were consistently associated with improvement in the domains of emotional exhaustion and overall burnout. There is insufficient information available to draw conclusions about studies involving other interventions aimed at the reduction of burnout.
Supplementary Material
References
- 1. Maslach C. . Burnout: a multidimensional perspective. : Schaufeli W, Maslach C, Marek, T, . Professional Burnout: Recent Developments in Theory and Research. Abingdon, UK: Taylor & Francis Group; 1993: 19– 32. [Google Scholar]
- 2. Dyrbye LN, West CP, Satele D, et al. Burnout among US medical students, residents, and early career physicians relative to the general US population. Acad Med. 2014; 89 3: 443– 451. [DOI] [PubMed] [Google Scholar]
- 3. Satterfield JM, Becerra C. . Developmental challenges, stressors, and coping strategies in medical residents: a qualitative analysis of support groups. Med Educ. 2010; 44 9: 908– 916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Williams D, Tricomi G, Gupta J, et al. Efficacy of burnout interventions in the medical education pipeline. Acad Psychiatry. 2015; 39 1: 47– 54. [DOI] [PubMed] [Google Scholar]
- 5. Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996; 17 1: 1– 12. [DOI] [PubMed] [Google Scholar]
- 6. Wells GA, Shea B, O'Connell J, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analysis. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed March 23, 2017. [Google Scholar]
- 7. Parshuram CS, Amaral AC, Ferguson ND, . et al; Canadian Clinical Care Trials Group. Patient safety, resident well-being, and continuity of care with different resident duty schedules in the intensive care unit: a randomized trial. CMAJ. 2015; 187 5: 321– 329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bragard I, Etienne AM, Merckaert I, et al. Efficacy of a communication and stress management training on medical residents' self-efficacy, stress to communicate, and burnout: a randomized controlled study. J Health Psychol. 2010; 15 7: 1075– 1081. [DOI] [PubMed] [Google Scholar]
- 9. Bar-Sela G, Lulav-Grinwald D, Mitnik I. . “Balint group” meetings for oncology residents as a tool to improve therapeutic communication skills and reduce burnout level. J Cancer Educ. 2012; 27 4: 786– 789. [DOI] [PubMed] [Google Scholar]
- 10. Barrack RL, Miller LS, Sotile WM, et al. Effect of duty hour standards on burnout among orthopaedic surgery residents. Clin Orthop Relat Res. 2006; 449: 134– 137. [DOI] [PubMed] [Google Scholar]
- 11. Gelfand DV, Podnos YD, Carmichael JC, et al. Effect of the 80-hour workweek on resident burnout. Arch Surg. 2004; 139 9: 933– 938; discussion 938–940. [DOI] [PubMed] [Google Scholar]
- 12. Goitein L, Shanafelt TD, Wipf JE, et al. The effects of work-hour limitations on resident well-being, patient care, and education in an internal medicine residency program. Arch Intern Med. 2005; 165 22: 2601– 2606. [DOI] [PubMed] [Google Scholar]
- 13. Gopal R, Glasheen JJ, Miyoshi TJ, et al. Burnout and internal medicine resident work-hour restrictions. Arch Intern Med. 2005; 165 22: 2595– 2600. [DOI] [PubMed] [Google Scholar]
- 14. Hutter MM, Kellogg KC, Ferguson CM, et al. The impact of the 80-hour resident workweek on surgical residents and attending surgeons. Ann Surg. 2006; 243 6: 864– 871; discussion 871–865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lindeman BM, Sacks BC, Hirose K, et al. Multifaceted longitudinal study of surgical resident education, quality of life, and patient care before and after July 2011. J Surg Educ. 2013; 70 6: 769– 776. [DOI] [PubMed] [Google Scholar]
- 16. Martini S, Arfken CL, Churchill A, et al. Burnout comparison among residents in different medical specialties. Acad Psychiatry. 2004; 28 3: 240– 242. [DOI] [PubMed] [Google Scholar]
- 17. Ripp JA, Bellini L, Fallar R, et al. The impact of duty hours restrictions on job burnout in internal medicine residents: a 3-institution comparison study. Acad Med. 2015; 90 4: 494– 499. [DOI] [PubMed] [Google Scholar]
- 18. Shea JA, Bellini LM, Dinges DF, et al. Impact of protected sleep period for internal medicine interns on overnight call on depression, burnout, and empathy. J Grad Med Educ. 2014; 6 2: 256– 263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Martins AE, Davenport MC, Del Valle MP, et al. Impact of a brief intervention on the burnout levels of pediatric residents. J Pediatr (Rio J). 2011; 87 6: 493– 498. [DOI] [PubMed] [Google Scholar]
- 20. Milstein JM, Raingruber BJ, Bennett SH, et al. Burnout assessment in house officers: Evaluation of an intervention to reduce stress. Med Teach. 2009; 31 4: 375– 378. [DOI] [PubMed] [Google Scholar]
- 21. Ospina-Kammerer V, Figley CR. . An evaluation of the Respiratory One Method (ROM) in reducing emotional exhaustion among family physician residents. Int J Emerg Ment Health. 2003; 5 1: 29– 32. [PubMed] [Google Scholar]
- 22. Ghetti C, Chang J, Gosman G. . Burnout, psychological skills, and empathy: Balint training in obstetrics and gynecology residents. J Grad Med Educ. 2009; 1 2: 231– 235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McCue JD, Sachs CL. . A stress management workshop improves residents' coping skills. Arch Intern Med. 1991; 151 11: 2273– 2277. [PubMed] [Google Scholar]
- 24. Weight CJ, Sellon JL, Lessard-Anderson CR, et al. Physical activity, quality of life, and burnout among physician trainees: the effect of a team-based, incentivized exercise program. Mayo Clin Proc. 2013; 88 12: 1435– 1442. [DOI] [PubMed] [Google Scholar]
- 25. Antiel RM, Reed DA, Van Arendonk KJ, et al. Effects of duty hour restrictions on core competencies, education, quality of life, and burnout among general surgery interns. JAMA Surg. 2013; 148 5: 448– 455. [DOI] [PubMed] [Google Scholar]
- 26. Bolster L, Rourke L. . The effect of restricting residents' duty hours on patient safety, resident well-being, and resident education: an updated systematic review. J Grad Med Educ. 2015; 7 3: 349– 363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. van Vendeloo SN, Brand PL, Verheyen CC. . Burnout and quality of life among orthopaedic trainees in a modern educational programme. Bone Joint J. 2014; 96-B 8: 1133– 1138. [DOI] [PubMed] [Google Scholar]
- 28. Merecz D, Andysz A. . Relationship between person-organization fit and objective and subjective health status (person-organization fit and health). Int J Occup Med Environ Health. 2012; 25 2: 166– 177. [DOI] [PubMed] [Google Scholar]
- 29. Maslach C, Leiter MP. . Early predictors of job burnout and engagement. J Appl Psychol. 2008; 93 3: 498– 512. [DOI] [PubMed] [Google Scholar]
- 30. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016; 388 10057: 2272– 2281. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.