Abstract
Background
Adults aged 65 years and older account for more than 33% of annual visits to internal medicine (IM) generalists and specialists. Geriatrics experiences are not standardized for IM residents. Data are lacking on IM residents' continuity experiences with older adults and competencies relevant to their care.
Objective
To explore patient demographics and the prevalence of common geriatric conditions in IM residents' continuity clinics.
Methods
We collected data on age and sex for all IM residents' active clinic patients during 2011–2012. Academic site continuity panels for 351 IM residents were drawn from 4 academic medical center sites. Common geriatric conditions, defined by Assessing Care of Vulnerable Elders measures and the American Geriatrics Society IM geriatrics competencies, were identified through International Classification of Disease, ninth edition, coded electronic problem lists for residents' patients aged 65 years and older and cross-checked by audit of 20% of patients' charts across 1 year.
Results
Patient panels for 351 IM residents (of a possible 411, 85%) were reviewed. Older adults made up 21% of patients in IM residents' panels (range, 14%–28%); patients ≥ 75 (8%) or 85 (2%) years old were relatively rare. Concordance between electronic problem lists and chart audit was poor for most core geriatric conditions. On chart audit, active management of core geriatric conditions was variable: for example, memory loss (10%–25%), falls/gait abnormality (26%–42%), and osteoporosis (11%–35%).
Conclusions
The IM residents' exposure to core geriatric conditions and management of older adults was variable across 4 academic medical center sites and often lower than anticipated in community practice.
What was known and gap
A sizable portion of internists' practice is caring for older adults, yet little is known relevant to residents' experiences in their continuity clinics.
What is new
A study of internal medicine resident continuity clinics in 4 sites focusing on management of common geriatric conditions.
Limitations
All sites had existing funding to improve the care of older adults.
Bottom line
Internal medicine residents' exposure to core geriatric conditions and management of older adults is variable and is lower than what graduates will experience in community practice.
Introduction
The US population is aging rapidly, with the fastest growth in those aged 85 years and older.1 Older adults, by virtue of their higher incidence of chronic diseases, represent an even larger portion of those consuming health care. In 2012, adults aged 65 years and older represented approximately 14% of the population, and accounted for approximately 34% of health care costs.2 Internal medicine (IM) physicians provide much of this care, with those aged 65 years and older accounting for more than 32% of annual visits provided to adult patients by IM generalists and specialists.3 Adults over age 75 account for nearly 15% of primary care visits and 20% of medical specialty visits.3
In 2010, minimum competencies in geriatrics for IM (and family medicine) residents were developed and supported by the American Medical Association, the American Geriatrics Society, the American Board of Family Medicine, and the Society of General Internal Medicine.4 Although numerous studies document the positive impact of formal teaching of IM residents in geriatrics with an emphasis on competencies,5–9 the majority of studies in geriatrics education focus on curricula for subspecialty-specific experience silos such as long-term care10 or dedicated geriatrics rotations.11 Few studies have addressed the process of establishing competency in the care of older adults in IM residents' own longitudinal ambulatory experience. Residents' patient panels have a lower mean age compared with those of physicians in practice.12 To our knowledge, there has been no systematic characterization of IM residents' experiences caring for older patients in their own ambulatory primary care clinics, or whether residents apply geriatrics principles that are learned in specialty rotations to the clinic experiences in longitudinal practice.
We explored IM residents' exposure to older adult patients in their ambulatory primary care practice at 4 academic medical centers (AMCs), and their experience in managing core geriatric conditions in older patients.
Methods
Setting and Participants
We identified primary care patient panels for all categorical IM residents in the IM training programs at Duke University School of Medicine, Medical University of South Carolina, University of North Carolina School of Medicine, and Wake Forest School of Medicine, whose continuity patient panels were located at the AMC (N = 351). Of a possible 411 categorical IM residents at all sites, we excluded 60 residents whose continuity experience occurred in Veterans Affairs hospitals. We assessed demographics of active primary care patient panels (n = 15 139 patients) for all of the remaining 351 IM residents who completed the full academic year of 2011–2012. We also assessed the presence of core geriatric conditions for all IM resident active patients aged 65 years and older.
Design Overview
Identifying IM Resident Primary Care Panels:
All patients included were assigned to an IM resident physician or resident physician team (in 3+1 or 4+1 schedules) as primary care physician during the academic year 2011–2012. Resident primary care schedules were then reviewed using each site's electronic health record (EHR). We excluded urgent care schedules, where a resident may see a faculty primary care physician's patient. An active resident primary care patient was defined as assigned to an IM resident and seen by a resident at that practice site at least once during 2011–2012. Patient demographics (age as of July 1, 2011, and sex) were extracted from each EHR.
Management of Core Geriatrics Conditions:
We listed core geriatric conditions and syndromes from the Assessing Care of Vulnerable Elders list and the Minimum Geriatric Competencies for IM residents.4 The conditions were dementia or any memory loss/cognitive impairment, depression, urinary incontinence, falls or any gait abnormality, weight loss or malnutrition, hearing loss, vision impairment, chronic pain, pressure ulcers, osteoporosis, and osteoarthritis. Residents' management of each core geriatric condition was explored by querying the EHR, using International Classification of Diseases, ninth edition (ICD-9), codes, for core geriatric conditions in patients aged 65 years and older. If relevant ICD-9 codes were found in the documented problem list, this was defined as active management of that condition. Problem lists at each site were customarily maintained and updated by physicians and other clinicians, primarily (but not exclusively) primary care physicians. As several sites used paper-based billing, visit diagnoses were not available from all sites and, therefore, not included.
Chart Audit:
To check the accuracy of EHR problem lists, we developed a chart audit tool (using the American Geriatrics Society Minimum Geriatrics Competencies for IM Residents) for reviewing clinic visits to document management of core geriatric conditions (provided as online supplemental material). The tool listed synonyms and descriptors for core geriatric conditions as well as a comprehensive list of medications used and/or relevant interventions for these conditions. Audited charts were selected using a weighted random selection. Charts selected for review included all patients aged 85 years and older, plus a random selection of patients aged 65 to 85 years, with a minimum audit at each site of 20% of active charts for patients aged 65 years and older. Deidentified identification numbers were used to enter patient information; these data were managed using research electronic data capture (REDCap).13 The chart audit encompassed documentation of all primary care visits that occurred during the target year for the selected resident's primary care patients. Specialty visits (eg, memory assessment clinic) were not included.
This project was approved by the Institutional Review Board of each participating institution.
Analysis
Demographics are reported using descriptive statistics for continuous (t test) and categorical (chi-square) variables. Patients with core geriatric conditions based on EHR or chart audit are reported as percentages of total patients aged 65 years and older who were reviewed.
Results
Demographics
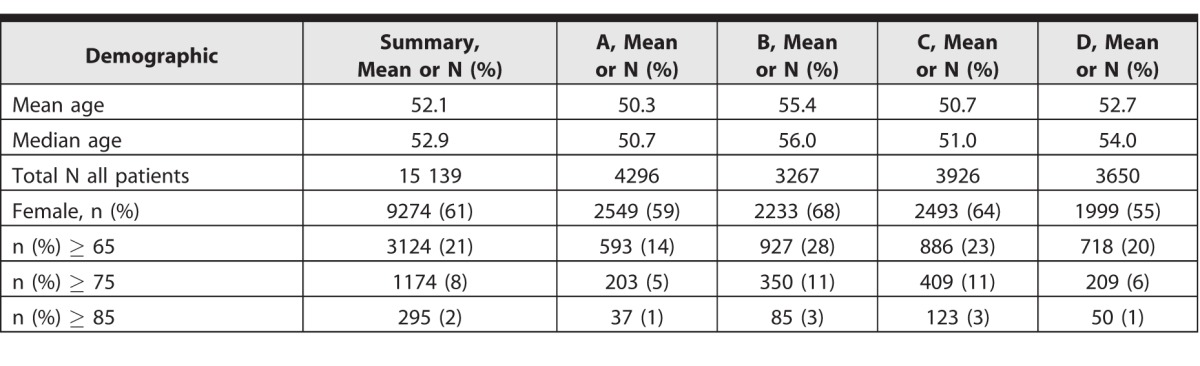
Data were reviewed for 85% of categorical IM residents for 2011–2012 (N = 351 of a possible 411). Of the 15 139 patients identified for the 351 residents, the majority were female, both overall and at each site (Table 1). The proportion of residents' active primary care patients who were aged 65 years and older varied across sites, from 14% to 28%, with an average of 21%. Those aged 75 years and older made up from 5% to 11%, with an average of 8%. Data on race and ethnicity for these patients were not consistently available.
Table 1.
Demographics of the Resident Practices (Labeled A–D)
Management of Core Geriatric Conditions
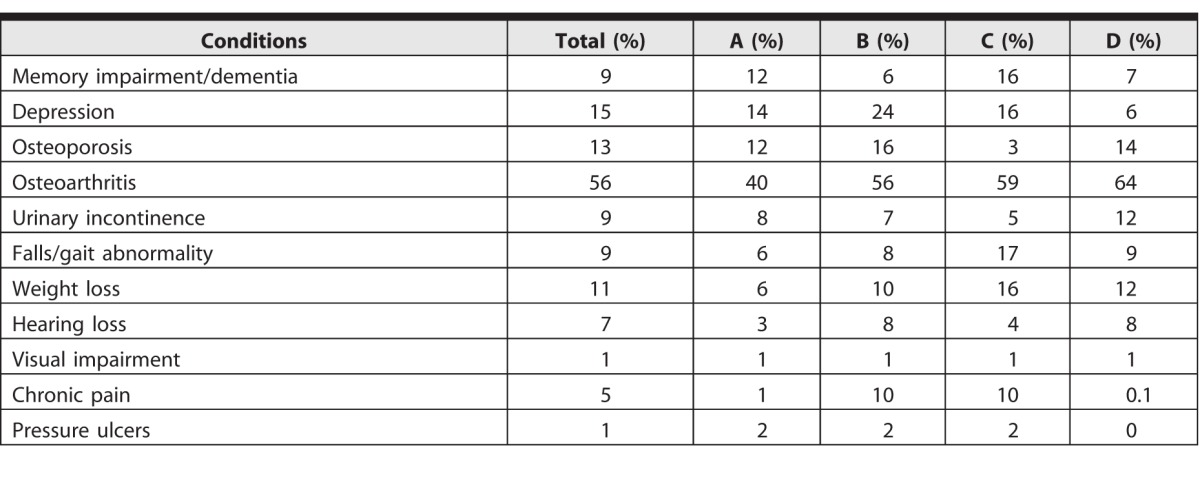
The EHR problem lists rarely documented core geriatric conditions for older patients, with prevalence percentages varying across sites for different diagnoses (Table 2a). Osteoarthritis showed the highest prevalence (56%; range, 40%–64%).
Table 2a.
Electronic Health Record Prevalence of Common Geriatric Conditions for Older Adults by Site (Labeled A–D; n = 3124)
We completed 1224 patient chart audits for resident primary care patients aged 65 years and older, who experienced a median of 3 visits to the residency practices across the year (mean range across sites, 3.5–3.8; full range, 1–15 visits across sites). All primary care visits to resident physicians were reviewed. Residents were more likely to document active management of core geriatric conditions than record them in the EHR problem list. Concordance between conditions on the EHR problem list and chart audit was low across all conditions and all sites (Table 2b). The 3 conditions with greatest concordance were osteoarthritis (72%), pressure ulcers (64%), and dementia/memory loss (51%). The 3 lowest concordances were for visual impairment (3%), pain (5%), and falls/gait instability (15%).
Table 2b.
Concordance Between Chart Audit–Identified and Electronic Health Record (EHR) Problem List–Identified Prevalence of Core Geriatric Conditions (n = 1224)a
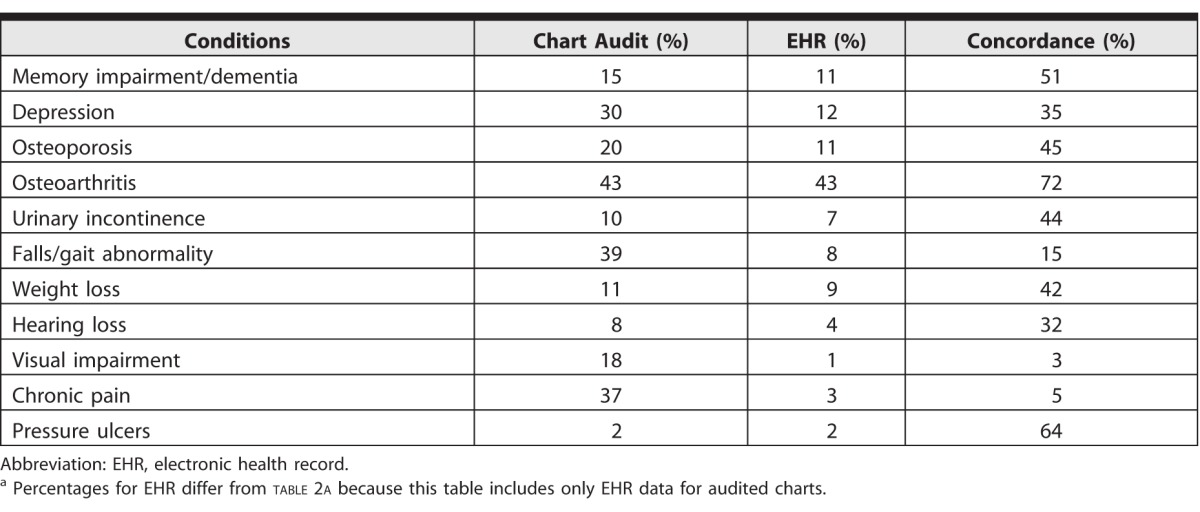
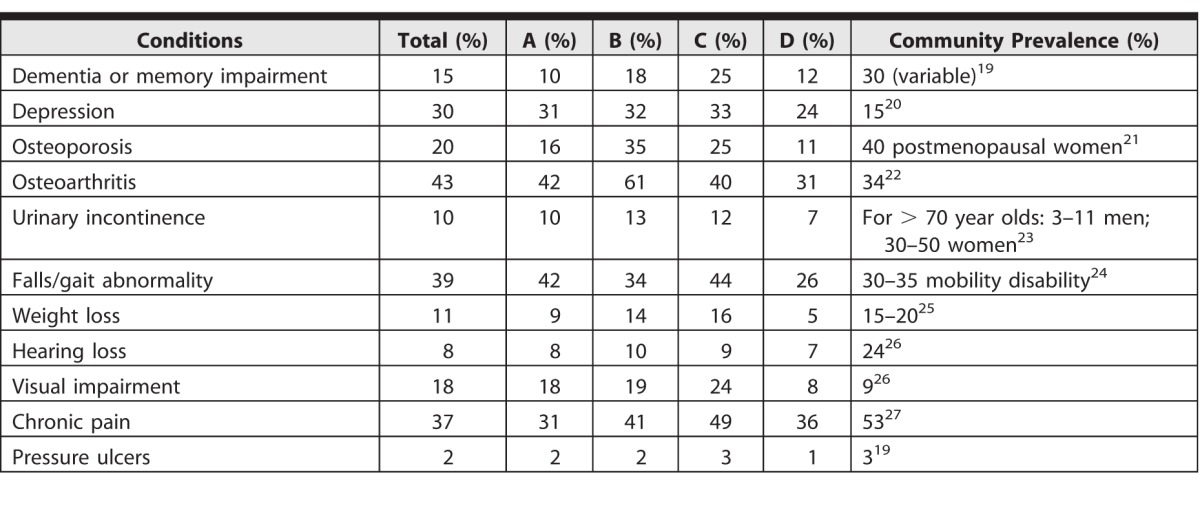
Chart audit demonstrated discrepancies across the 4 sites in prevalence of documented management of core geriatric conditions (Table 3). The widest variability was in osteoarthritis, osteoporosis, and falls/gait abnormality; the least variability was for hearing loss, urinary incontinence, and depression. Active management of some core geriatric conditions was less common than would be anticipated based on published community prevalence (Table 3).
Table 3.
Prevalence of Common Geriatric Conditions for Older Adults by Site (Labeled A–D) in Chart Audits (n = 1224)
Discussion
The proportion of older adults in IM residents' primary care patient panels varied across 4 AMCs; some numbers were lower than expected given the aging population. We also assessed the prevalence of core geriatric conditions in IM residents' older primary care patients, examining both EHR problem lists and a chart audit of approximately 20% of their older adult patients' visits across 1 year. We noted discordance between EHR problem lists and chart audit. We found a variable and lower than expected prevalence of care related to common conditions of aging compared with community practice. This raised a concern that some IM residents' experience in ambulatory care for older adults may not align with future anticipated ambulatory practice needs of the US population. These data are consistent with studies reporting that resident patients are younger and less likely to receive geriatric quality metrics than those of physicians in practice.12
The discordance between EHR problem lists and chart audit may stem from the duration of the problem, the focus of the visit on comorbidities, or the overall underuse of EHR problem lists by IM residents. However, it could reflect IM residents' lower recognition of core geriatric conditions (even when actively managed) as notable or billable conditions to record in the EHR. The poor concordance between chart audit and EHR problem lists serves as a caution in assessment of graduate trainees: while milestones motivate educators to conduct workplace assessment, this disconnect adds to the evidence of limitations of the EHR as an assessment tool.
In auditing charts across 1 year, prevalence of core geriatric conditions varied across institutions, and conditions occurred less than published community averages (Table 3). The IM residents could be managing geriatric conditions but not documenting them; they may be focused on medical comorbidities, or these conditions may not be active. However, the conditions drawn from Assessing Care of Vulnerable Elders measures and Association of American Medical Colleges competencies reflect a baseline standard of care; one would expect these to be assessed for an older adult at least once across a year. Indeed, each institution in the study has incorporated quality improvement (QI) initiatives targeting the care of older adults, and differences across the 4 sites in documentation and management may relate to active QI interventions focused on different geriatric conditions across sites.
Work hour limitations and curricular competition may challenge the duration, quality, and continuity of residents' ambulatory experiences.14,15 Residents reported feeling unprepared to manage patients in an ambulatory setting upon graduation,16 and practicing general internists have expressed frustration in caring for older adults and their complex conditions.17 These views may stem in part from the mismatch described here between residents' ambulatory practice experiences and the older patients who they will see in practice.12,15,18 Recognition and management of geriatric conditions such as mobility disability and cognitive impairment may improve the training experience while improving patient care, and are critical to postgraduate success in our changing health care environment. Our findings suggest that if residents are unable to devote time or focus on important geriatric conditions during continuity clinic, dedicated geriatrics exposure during other experiences remains critical to training.
Our study has limitations. In the EHR data pull and chart audit, we were unable to consistently obtain visit diagnoses or billing codes; these may have better demonstrated active clinical decision making compared with problem lists. We did not include core medical conditions such as diabetes or hypertension, which could have allowed for comparison with core geriatric conditions. Although 4 different AMCs were used, they are in the same geographic region; each also received Donald W. Reynolds Foundation funding to promote geriatrics education. Also, 3 of the 4 AMCs have geriatrics fellowships, and geriatrics faculty and fellows at each AMC may have siphoned some older adults from the residency practices. Non-AMC resident practice sites, such as the Veterans Affairs hospitals, were not included; IM residents there may have a broader exposure to continuity care of geriatrics patients. Each institution has geriatrics rotations, yet with the modest number of geriatricians, an educational goal would be that residents extrapolate best practices from geriatrics rotations to actively manage their primary care patients.
We observed differences among the 4 sites with regard to the prevalence of core geriatric conditions. Future directions would include examining and describing current differences in curricula at each site, including traditional clinic structures versus 3+1 or 4+1 rotations; and potentially testing curricular innovations, such as comparing geriatrics rotations with an embedded geriatrician preceptor, or initiating QI projects related to the care of older adults within IM resident clinics.
Conclusion
IM residents' exposure to core geriatric conditions and management of older adults was variable across 4 AMC sites and often lower than anticipated in community practice.
Supplementary Material
References
- 1. Ortman JM, Velkoff VA. . An aging nation: the older population in the United States. Population estimates and projections. Current Population Reports. United States Census Bureau. 2014. https://www.census.gov/prod/2014pubs/p25-1140.pdf. Accessed March 6, 2017. [Google Scholar]
- 2. Centers for Medicare and Medicaid Services. National Health Expenditure Fact Sheet, 2014. https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nhe-fact-sheet.html. Accessed March 6, 2017. [Google Scholar]
- 3. Schappert SM, Rechsteiner EA. . Ambulatory medical care utilization estimates for 2007. Vital Health Stat 13. 2011; 169: 1– 38. [PubMed] [Google Scholar]
- 4. Williams BC, Warshaw G, Fabiny AR, et al. Medicine in the 21st century: recommended essential geriatrics competencies for internal medicine and family medicine residents. J Grad Med Educ. 2010; 2 3: 373– 383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Caton C, Wiley MK, Zhao Y, et al. Improving internal medicine residents' falls assessment and evaluation: an interdisciplinary, multistrategy program. J Am Geriatr Soc. 2011; 59 10: 1941– 1946. [DOI] [PubMed] [Google Scholar]
- 6. Ahmed NN, Farnie M, Dyer CB. . The effect of geriatric and palliative medicine education on the knowledge and attitudes of internal medicine residents. J Am Geriatr Soc. 2011; 59 1: 143– 147. [DOI] [PubMed] [Google Scholar]
- 7. Kostas T, Zimmerman K, Salow M, et al. Improving medication management competency of clinical trainees in geriatrics. J Am Geriatr Soc. 2014; 62 8: 1568– 1574. [DOI] [PubMed] [Google Scholar]
- 8. Schlaudecker JD, Lewis TJ, Moore I, et al. Teaching resident physicians chronic disease management: simulating a 10-year longitudinal clinical experience with a standardized dementia patient and caregiver. J Grad Med Educ. 2013; 5 3: 468– 475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wilkerson LM, Iwata I, Wilkerson MD, et al. An educational intervention to improve internal medicine interns' awareness of hazards of hospitalization in acutely ill older adults. J Am Geriatr Soc. 2014; 62 4: 727– 733. [DOI] [PubMed] [Google Scholar]
- 10. Baum EE, Nelson KM. . The effect of a 12-month longitudinal long-term care rotation on knowledge and attitudes of internal medicine residents about geriatrics. J Am Med Dir Assoc. 2007; 8 2: 105– 109. [DOI] [PubMed] [Google Scholar]
- 11. Karani R, Callahan EH, Thomas DC. . An unfolding case with a linked OSCE: a curriculum in inpatient geriatric medicine. Acad Med. 2002; 77 9: 938. [DOI] [PubMed] [Google Scholar]
- 12. Lynn LA, Hess BJ, Conforti LN, et al. Clinic systems and the quality of care for older adults in residency clinics and in physician practices. Acad Med. 2009; 84 12: 1732– 1740. [DOI] [PubMed] [Google Scholar]
- 13. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42 2: 377– 381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wieland ML, Jaeger TM, Bundrick JB, et al. Resident physician perspectives on outpatient continuity of care. J Grad Med Educ. 2013; 5 4: 668– 673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Warshaw GA, Bragg EJ, Thomas DC, et al. Are internal medicine residency programs adequately preparing physicians to care for the baby boomers? A national survey from the Association of Directors of Geriatric Academic Programs Status of Geriatrics Workforce Study. J Am Geriatr Soc. 2006; 54 10: 1603– 1609. [DOI] [PubMed] [Google Scholar]
- 16. Mladenovic J, Shea JA, Duffy FD, et al. Variation in internal medicine residency clinic practices: assessing practice environments and quality of care. J Gen Intern Med. 2008; 23 7: 914– 920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tanner CE, Eckstrom E, Desai SS, et al. Uncovering frustrations. A qualitative needs assessment of academic general internists as geriatric care providers and teachers. J Gen Intern Med. 2006; 21 1: 51– 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Boult C, Counsell SR, Leipzig RM, et al. The urgency of preparing primary care physicians to care for older people with chronic illnesses. Health Aff (Millwood). 2010; 29 5: 811– 818. [DOI] [PubMed] [Google Scholar]
- 19. Kane RL, Talley KMC, Shamliyan T, et al. Common syndromes in older adults related to primary and secondary prevention. Report No 11-05157-EF-1. Rockville, MD: Agency for Healthcare Research and Quality; 2011. [PubMed] [Google Scholar]
- 20. Blazer DG. . Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003; 58 3: 249– 265. [DOI] [PubMed] [Google Scholar]
- 21. Ray NF, Chan JK, Thamer M, et al. Medical expenditures for the treatment of osteoporotic fractures in the United States in 1995: report from the National Osteoporosis Foundation. J Bone Miner Res. 1997; 12 1: 24– 35. [DOI] [PubMed] [Google Scholar]
- 22. Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 2008; 58 1: 26– 35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nitti VW. . The prevalence of urinary incontinence. Rev Urol. 2001; 3 suppl 1: 2– 6. [PMC free article] [PubMed] [Google Scholar]
- 24. Pahor M, Guralnik JM, Ambrosius WT, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA. 2014; 311 23: 2387– 2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gaddey HL, Holder K. . Unintentional weight loss in older adults. Am Fam Physician. 2014; 89 9: 718– 722. [PubMed] [Google Scholar]
- 26. Crews JE, Campbell VA. . Vision impairment and hearing loss among community-dwelling older Americans: implications for health and functioning. Am J Public Health. 2004; 94 5: 823– 829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Patel KV, Guralnik JM, Dansie EJ, et al. Prevalence and impact of pain among older adults in the United States: findings from the 2011 National Health and Aging Trends Study. Pain. 2013; 154 12: 2649– 2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


