The flipped classroom learning model has become increasingly popular in undergraduate medical education.1 Influenced by overall trends for millennial learners who prefer digital resources and interfaces, many medical schools emphasize online prelecture materials over lecture-based curricula during the preclinical years.2–4 Many have also called for incorporating the flipped classroom into graduate medical education (GME).5 The limits on resident work hours make the flipped classroom model an attractive educational approach for program directors and curriculum developers under pressure to fit more content into shorter workdays. By leveraging technology for these time-limited learners, the flipped classroom paradigm is a logical solution.
While attractive, is the flipped classroom model practical within GME as currently structured, in light of residents' extensive clinical obligations? It has been implemented successfully in several residency programs5–7; however, outcomes focus on improved satisfaction rather than feasibility, which is essential.8
During their time as internal medicine residents, 3 of the authors performed a small feasibility assessment of a flipped classroom–based curriculum on an inpatient cardiology rotation. We developed a 10-minute Khan Academy–style video on intra-aortic balloon pumps. All residents attended a traditional lecture on the topic, and some were assigned to view the video before attending the lecture. We found that only a quarter of residents assigned to watch the video actually did so.
Our preliminary experience led us to question whether the flipped classroom model would be an effective backbone of GME curricula. For one, residents and preclinical medical students have different educational goals and philosophies (Table). Medical students, whose raison d'être is to learn and study without service obligations in the preclinical years, are accustomed to homework prior to teaching sessions. Residents balance service and learning obligations, but their primary role is to provide excellent patient care. While residents are expected to study independently, much of their learning happens on the job through real-world application. Residents also have fewer standardized tests for which to study.
Table.
Differences in Educational Milieu Between Preclinical Medical Students and Residents
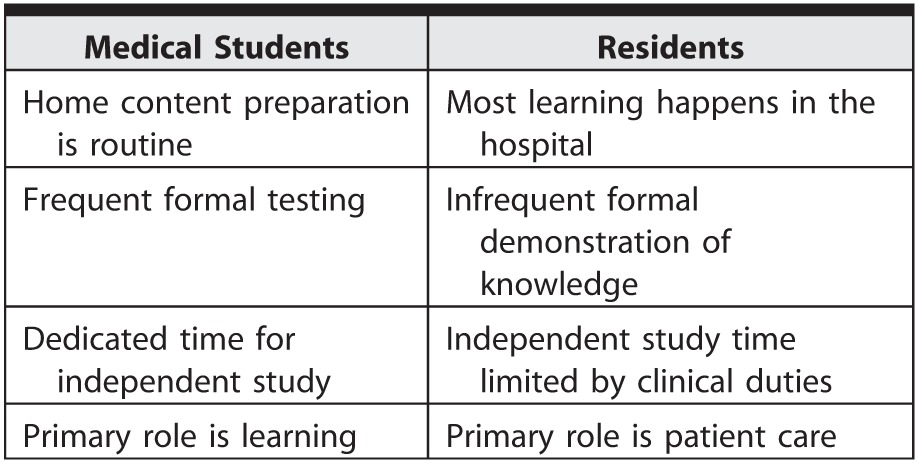
Second, time constraints differ for medical students and residents. While medical students must attend educational sessions, residents frequently miss or are pulled away from conferences out of clinical necessity and have heavy daily workloads, which may reduce their incentive to engage with prepared material (Table). As an intern who did not watch the module commented, “I was struggling with prioritizing my work flow. Checking and responding to [communications] was . . . low on my list of things to do.”
Incentives are important to consider when assessing the feasibility of any curricular innovation. In our intervention, residents received e-mails encouraging, but not requiring, them to watch the video modules. Without a concrete incentive or user tracking for flipped classroom modules, busy clinical residents seem unlikely to reliably access online content in their limited free time. Adequate adherence to a longitudinal, flipped classroom–based GME curriculum would likely require robust enforcement to drive resident use of the relevant online resources. We presume that busy residents would find this onerous.
Alternative flipped classroom implementation strategies may increase feasibility for GME by:
identifying effective incentives to encourage overall resident participation;
successfully implementing curricula among residents on elective/noncall blocks with more time for at-home learning;
incorporating dedicated presession time for independent review of resources, allowing residents to prepare without sacrificing their limited free time outside the hospital; and
incrementally increasing the use of flipped classroom–based learning over the academic year, allowing residents to adjust to new clinical roles at the beginning and consolidate knowledge at the end.
With any educational intervention, it is crucial to consider how the learning environment impacts feasibility. We want to emphasize that, given the time constraints and clinical requirements for GME learners, the flipped classroom model may not be well suited for large-scale implementation as the backbone of resident education.
References
- 1. Prober CG, Heath C. . Lecture halls without lectures—a proposal for medical education. N Engl J Med. 2012; 366 18: 1657– 1659. [DOI] [PubMed] [Google Scholar]
- 2. Khan Academy. http://www.khanacademy.org. Accessed March 30, 2017. [Google Scholar]
- 3. Desilets LD. . Are you ready for the net generation or the free agent learner? J Contin Educ Nurs. 2011; 42 8: 340– 341. [DOI] [PubMed] [Google Scholar]
- 4. Fu MY, Joung J. . Top medical schools react to Harvard's curriculum change. The Harvard Crimson. September 29, 2015. http://www.thecrimson.com/article/2015/9/29/schools-react-medical-curriculum. Accessed March 30, 2017. [Google Scholar]
- 5. Young TP, Bailey CJ, Guptill M, et al. . The flipped classroom: a modality for mixed asynchronous and synchronous learning in a residency program. West J Emerg Med. 2014; 15 7: 938– 944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Riddell JC, Sawtelle S, Jhun P, et al. . Low back pain in the emergency medicine department: a flipped classroom module. MedEdPORTAL Publications. 2016; 12: 10458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tainter CR, Wong NL, Cudemus-Deseda GA, et al. . The “flipped classroom” model for teaching in the intensive care unit. J Intensive Care Med. 2017; 32 3: 187– 196. [DOI] [PubMed] [Google Scholar]
- 8. Haspel RL, Ali AM, Huang GC. . Using a team-based learning approach at national meetings to teach residents genomic pathology. J Grad Med Educ. 2016; 8 1: 80– 84. [DOI] [PMC free article] [PubMed] [Google Scholar]


