Abstract
We report a case of tonsillar histoplasmosis with hematogenous dissemination in a woman receiving infliximab for Crohn's disease. She also had a history of sarcoidosis. Due to the unusual location and confounding medical history, our case provided a diagnostic dilemma. Histoplasma infection was confirmed histologically, and the patient responded well to appropriate treatment.
Keywords: Histoplasmosis, Tonsil
1. Introduction
Histoplasma capsulatum (H. capsulatum) is a fungus that may infect the oral cavity, but rarely the tonsil. We describe a patient receiving infliximab who developed disseminated histoplasmosis with tonsillar involvement. Infection of the tonsil caused significant symptoms that led to the correct diagnosis.
2. Case report
A 51 year old woman presented with a one month history of progressive right sided neck swelling, throat and ear pain, and dysphagia. This was accompanied by worsening of a chronic cough, intermittent fevers and weight loss. Over these weeks, the patient received empiric courses of clindamycin, amoxicillin, penicillin VK, prednisone and acyclovir for presumed tonsillar cellulitis that were ineffective.
She had a history of Crohn's Disease diagnosed 6 years prior to presentation, for which she was receiving 6-mercaptopurine and infliximab for the past 3 years. She had been diagnosed with sarcoidosis based on cervical lymph node histology with sclerotic granulomas; lung nodules with mediastinal adenopathy; hypercalciuria and vitamin D dysregulation. She was a native of Germany, residing in upstate New York for the past 13 years. Her only travel outside New York was to Europe. Remote screening for latent tuberculosis had been negative. She was a current smoker and averaged about one pack per day for 34 years.
On physical examination, she was afebrile. Her right neck was tender to touch without a palpable mass. There was no cervical or supraclavicular adenopathy. Examination of the oropharynx revealed an enlarged necrotic right tonsil without odor. No lesions of the tongue, buccal mucosa or palate were identified. Chest auscultation was normal. There was no abdominal hepatosplenomegaly.
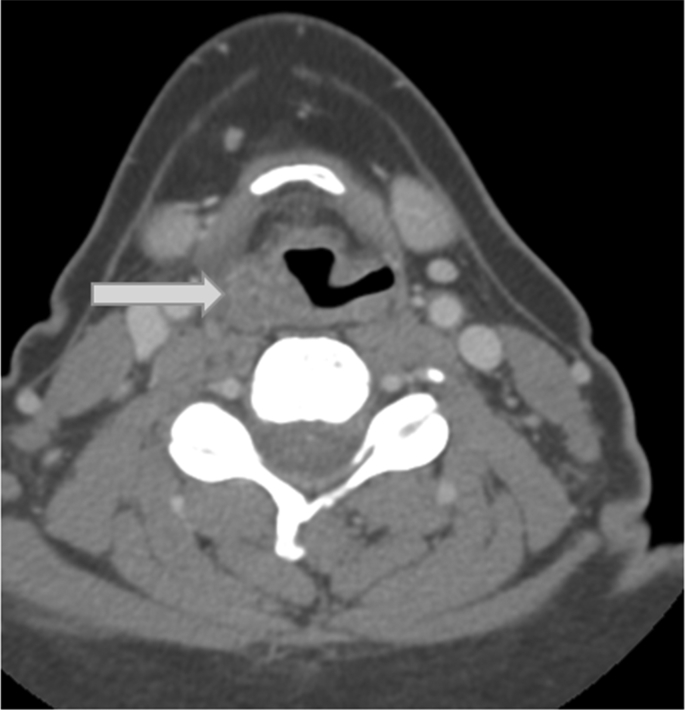
Complete blood count showed white blood cell count 4100/μL, hemoglobin 13.5 gm/dL and platelet count 167,000/μL. Computed tomography (CT) of the thorax showed bilateral diffuse micronodules. CT scan of the neck (Fig. 1) showed an enlarged right tonsil with asymmetric thickening of the aryepiglottic fold, the right side of the epiglottis, right tonsillar pillar, and right lingual tonsil.
Fig. 1.
Axial image from contrast-enhanced CT scan of the neck demonstrates asymmetric thickening of the right aryepiglottic fold (arrow).
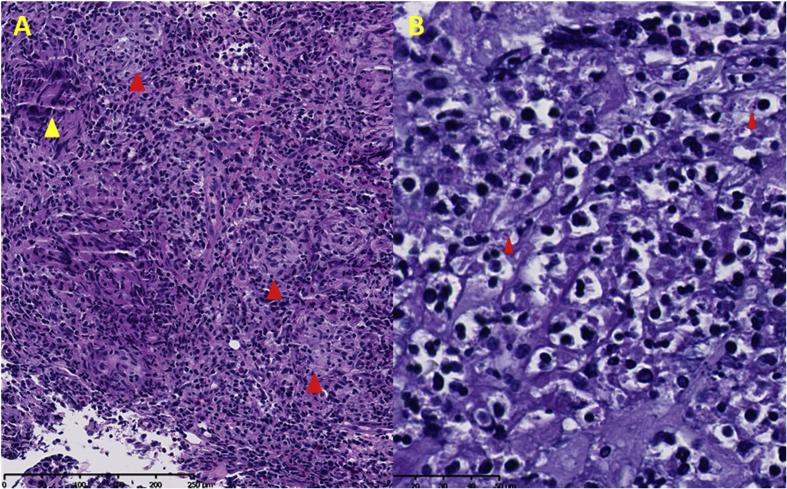
Infliximab was discontinued with her most recent dose being three weeks prior to presentation. One week later, bronchoalveolar lavage (BAL) and transbronchial biopsy were performed, but histology and microbiology were non-diagnostic. BAL cytology and flow cytometry did not suggest lymphoma or malignancy. Tonsillar biopsy (Fig. 2A) demonstrated granulomas and multinucleated giant cells with suppurative inflammation. Diastase-resistant periodic acid Schiff (DPAS) stain showed intracytoplasmic yeast forms, consistent with histoplasmosis (Fig. 2B). Two weeks after the biopsy, the urine Histoplasma antigen was negative. Serum Histoplasma antibody quantitative immunodiffusion analysis was obtained an additional two weeks later, and was positive for M antigen with a titer of 1:128, but was negative for H antigen. The formalin fixed tonsillar biopsy tissue was sent to the Mycology Laboratory, Wadsworth Center, Albany, NY, which was confirmed to contain H. capsulatum DNA with a cycle threshold (Ct) of 35.5 (positive <40) by real-time polymerase chain reaction (rt-PCR) assay.
Fig. 2.
A: Tonsil biopsy demonstrating numerous granulomas (large red arrowheads) associated with inflammation and multinucleated giant cells (yellow arrowhead) B: DPAS stain highlights numerous intracytoplasmic yeasts, consistent with histoplasmosis (small red arrowheads).(For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Itraconazole was administered at a dose of 200mg three times daily for three days and continued at 200mg twice daily. Within two weeks of starting therapy, her throat pain and cough greatly improved. Within one month of therapy, her tonsil had healed, and follow up CT of the chest at 3 months was normal.
3. Discussion
We report a case of tonsillar histoplasmosis. A biopsy of the tonsil demonstrated intracytoplasmic yeast forms on DPAS staining. These results were further confirmed by real-time PCR where tissue biopsy was positive for H. capsulatum DNA. The real-time PCR assay targeting MSP gene that codes for M antigen is highly specific for the diagnosis of histoplasmosis, as it can differentiate H. capsulatum from other fungi such as Candida, Aspergillus, Cryptococcus and others [1], [2]. Additionally, the patient's serum was positive for H. capsulatum specific M antigen. While the majority of histoplasmosis cases occur along the Ohio and Mississippi river regions, a small percentage have been identified along the St. Lawrence Seaway, including upstate New York where our patient resided [3].
Involvement of the oral cavity is fairly common with histoplasmosis, especially the tongue [4], [5]. Tonsillar histoplasmosis, however, is rare with only two prior cases reported [6], [7]. One earlier reported case, like our patient, was receiving a TNF-alpha inhibitor [6]. In our case and the prior reports, the diagnosis was delayed because the oral lesions were attributed to alternative etiologies including, bacterial and viral infections [6], tuberculosis [7] and malignancy [7].
Treatment of disseminated histoplasma is indicated regardless of severity. Infectious Diseases Society of America (IDSA) guidelines [8] recommend one to two weeks of liposomal Amphotericin B for severe disease. Upon stabilization, a loading dose of 200mg three times a day of itraconazole for three days followed by maintenance dosing of 200mg twice daily for one year is indicated. For mild to moderate disease, the itraconazole loading dose and maintenance dosing remains the same, and at least one year of therapy is recommended. It is believed that resuming immunosuppression is reasonable after one year of therapy with close follow-up to monitor for recurrence [9]. It is important to note that patients who require continued immunosuppression may require suppressive therapy for as long as they are immunocompromised.
4. Conclusion
This case highlights that the tonsil is a potential site of H. capsulatum infection. The pathogen should be considered in immunocompromised patients with tonsillar complaints who have lived in areas endemic for this fungus. Although histological examination of the tonsil with appropriate fungal staining is usually adequate to confirm the diagnosis of tonsillar Histoplasma infection, the highly specific and sensitive H. capsulatum rt-PCR may aid in the diagnosis.
Conflict of interest
MAJ is a consultant for Biogen. No other author has a conflict of interest to disclose.
References
- 1.de Matos Guedes Herbert Leonel, Guimaraes Allan Jefferson, de Medeiros Muniz Mauro, Pizzini Claudia Vera, Hamilton Andrew John, Peralta Jose Mauro, Deepe George S., Jr., Zancope-Oliveira Rosely M. PCR assay for identification of Histoplasma capsulatum based on the nucleotide sequence of the M Antigen. J. Clin. Microbiol. Feb. 2003:535–539. doi: 10.1128/JCM.41.2.535-539.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Histologic and molecular identification of disseminated Histoplasma capsulatum in a captive brown bear (Ursus arctos). Margaret A.Highland, SudhaChaturvedi, MichaelPerez, HowardSteinberg, RobertaWallace. J. Veterinary Diagn. Investig.. 23(4) 764–769 [DOI] [PubMed]
- 3.Chu Jaclyn H., Feudtner Chris, Heydon Kateri, Walsh Thomas J., Zaouti Theoklis E. Hospitalizations for endemic mycoses: a population-based national study. Clin. Infect. Dis. 2006;42(6):822–825. doi: 10.1086/500405. [DOI] [PubMed] [Google Scholar]
- 4.Hernández S.L., López De Blanc S.A., Sambuelli R.H., Roland H., Cornelli C., Lattanzi V., Carnelli M.A. Oral histoplasmosis associated with HIV infection: a comparative study. J. Oral Pathol. Med. 2004 Sep;33(8):445–450. doi: 10.1111/j.1600-0714.2004.00183.x. [DOI] [PubMed] [Google Scholar]
- 5.Antonello V.S., Zaltron V.F., Vial M., Oliveira F.M., Severo L.C. Oropharyngeal histoplasmosis: report of eleven cases and review of the literature. Rev. Soc. Bras. Med. Trop. 2011 Jan-Feb;44(1):26–29. doi: 10.1590/s0037-86822011000100007. [DOI] [PubMed] [Google Scholar]
- 6.Durand M.L., Lin D.T., Juliano A.F., Sadow P.M. Case records of the Massachusetts General Hospital. Case 32-2014. A 78-year-old woman with chronic sore throat and a tonsillar mass. N. Engl. J. Med. 2014 Oct 16;371(16):1535–1543. doi: 10.1056/NEJMcpc1406191. [DOI] [PubMed] [Google Scholar]
- 7.Clyti E., Aznar C., Couppie P., Sainte-Marie D., Lemoine C., Huerre M., Carme B., Pradinaud R. Disseminated histoplasmosis detected by lingual and tonsillar erosions in an immunocompetent patient. Ann. Dermatol. Venereol. 1999 Oct;126(10):709–711. [PubMed] [Google Scholar]
- 8.Joseph Wheat L., Freifeld Alison G., Kleiman Martin B., Baddley John W., McKinsey David S., Loyd James E., Kauffman Carol A. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the infectious diseases society of America. Clin. Infect. Dis. 2007;45(7):807–825. doi: 10.1086/521259. [DOI] [PubMed] [Google Scholar]
- 9.Vergidis, P., Avery, R. K., Wheat, L. J., Dotson, J. L., Assi, M. A., Antoun, S. A.,... HageC. A. Histoplasmosis complicating tumor necrosis factor-α blocker therapy: a retrospective analysis of 98 cases. Clin. Infect. Dis., 61(3), 409–417. [DOI] [PMC free article] [PubMed]