Abstract
Cryptogenic Organising Pneumonia (COP) is a relatively rare condition and can be difficult to differentiate from Community acquired pneumonia (CAP). We report two cases which demonstrate the importance of considering this differential diagnosis in patients with spontaneous pneumothorax who have raised inflammatory markers or lung infiltrates. Our report highlights the value of serum procalcitonin as a biomarker in differentiating between community acquired pneumonia and cryptogenic organising pneumonia especially in the context of a high serum C-reactive protein. Furthermore, the cases show early diagnosis and prompt treatment with corticosteroids may impact the clinical outcome.
1. Background
Cryptogenic organising pneumonia (COP), otherwise known as idiopathic bronchiolitis obliterans organising pneumonia (BOOP), was first described as a distinct clinico-pathological entity during the late 20th century [1]. Histologically, it is characterised by intraluminal filling of granulation tissue in secondary and tertiary airways typically associated with peribronchial infiltration of monocytes and foamy macrophages. Patients affected are more likely to be from the fourth to the sixth decade, mostly without any pre-existing co-morbidities. Clinically, patients usually present with non-specific symptoms including non-productive cough, dyspnoea, low-grade pyrexia and weight loss; less commonly pleuritic chest pain and haemoptysis. It is vital to note that patients with COP paint a similar clinical and radiological picture to bacterial pneumonia, marking COP as a rare but important differential diagnosis. Since being highlighted in the 1980's, the literature has described cases complicated by pneumothorax, solitary nodules and pleural effusion [2]. As such, there has been a growing interest in utilizing clinical investigations to differentiate infective and non-infective conditions, be it invasive or non-invasive. The serum biomarker, procalcitonin, has proven to be useful and may play an increasingly important role especially when the diagnosis is unclear [3], [4].
2. Case 1
PT is a 56-year-old gentleman who presented to emergency department with sudden onset of shortness of breath in Jan 2016. He smoked 5 cigarettes/day and previously smoked cannabis. He had no significant past medical history and wasn't on any regular medication. He works as a lorry driver. He was found to have right sided pneumothorax with tethering of the lung at the upper zone and a small pleural effusion on Chest X-ray (Fig. 1). His vital signs showed a respiratory rate (RR) of 16, oxygen saturations (SpO2) 95% on air, and temperature of 36.8° Celsius. White Blood Cell Count (WBC) was 20.2 × 103/ml; with a differential of Neutrophils 16.1 × 103/ml, and Eosinophils 0.0 × 103/ml. C - reactive protein (CRP) was incidentally found to be elevated at 231. The patient however denied any cough or fever and didn't have any signs of infection. Pleural fluid analysis revealed an exudate but fluid pH was normal. He was treated with oral co-amoxiclav 625 mg TDS for one week. A size 12 Seldinger chest drain was inserted and 500 ml of fluid was aspirated. The chest drain was later attached to a Pneumostat™ chest drain valve to facilitate early mobilisation. He remained well but the pneumothorax failed to heal. A CT scan of the chest (Fig. 2) was done which unexpectedly showed a right upper lobe mass lesion. Review of the initial CXR showed peripheral consolidation which was mistaken for an area of collapsed lung. Following discussion with the thoracic surgeon, this was investigated with a CT-PET scan (Fig. 3) on day 15. This showed moderate uptake (SUV max 4.9) in the peripheral right upper lobe lesion (presumed lung cancer) along with a small loculated effusion suggestive of early empyema. He was transferred to the tertiary hospital by the thoracic surgeons and underwent VATS on day 19 where wedge resection of the right upper lobe lesion and pleural decortication were performed. Intraoperative frozen section excluded malignancy and conventional histology of the lesion showed organising pneumonia. He had a prolonged air leak and fever post operatively and was eventually discharged home 20 days post operatively (Fig. 1, Fig. 2, Fig. 3).
Fig. 1.
Chest radiograph showing right sided pneumothorax.
Fig. 2.
CT thorax showing right peripheral nodule and pneumothorax.
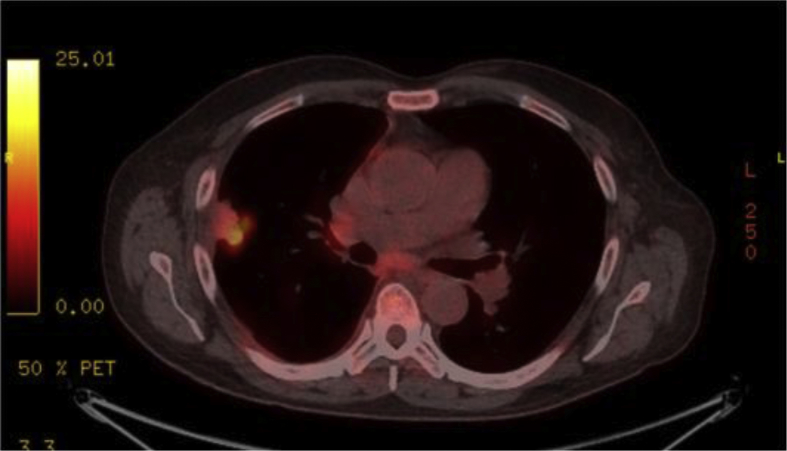
Fig. 3.
CT – PET scan showing moderate uptake in the right peripheral nodule.
3. Case 2
AT is an 82-year-old lady who presented with a 5-day history of shortness of breath and productive cough. There was no evidence of haemoptysis, pyrexia or weight loss. Her past medical history includes Chronic Obstructive Pulmonary Disease (COPD), hypothyroidism, hypertension, mitral regurgitation and previous varicose veins. She had a 21 pack-year history of smoking. Her previous occupation was a clerk, and occasionally enjoys volunteer work for charity. Her current medication includes regular Seretide 500 accuhaler, Levothyroxine, Ramipril, Bisoprolol and Amlodipine, with Salbutamol inhalers on as required basis.
On examination, positive findings included bilateral expiratory wheeze with scattered crackles throughout. Her vital signs showed a respiratory rate (RR) of 20, oxygen saturations (SpO2) 95% on 28% oxygen, and temperature of 36.9° Celsius. Her blood results revealed a White Blood Cell Count (WBC) of 10.9 × 103/ml; with a differential of Neutrophils 9.8 × 103/ml and Eosinophils 0.0 × 103/ml, and CRP of 161 mg/l. Her arterial blood gas on room air revealed a pH of 7.5, pO2 6.1 kPa, pCO2 4.8 kPa and HCO3 28 mmol/l. Sputum cultures were negative. Her immunology including Anti-nuclear Antibodies, ANCA and Rheumatoid Factor were negative. Her chest radiograph revealed right sided upper to mid zone infiltrates (Fig. 4). She was further investigated with a Computed Tomography (CT) of the Chest, which depicted consolidation, mild volume loss and some ground glass opacification in the right upper lobe, associated with small to moderate right anterior pneumothorax (Fig. 5). On admission, she was initially started on Amoxicillin and Clarithromycin but remained hypoxaemic. On Day 2 a procalcitonin level was found to be normal at 0.13 ng/ml (reference range 0.00–0.25) and she was then commenced on oral prednisolone 40 mg once a day and antibiotics were downgraded to oral amoxicillin 500 mg TDS for five days. She improved rapidly and was successfully weaned off oxygen by day 3 and her repeat blood test on day 6 revealed a WCC and CRP counts within the normal range. CXR showed complete resolution of the pneumothorax. She was discharged on long term corticosteroid therapy after 6 days in hospital following satisfactory progress.
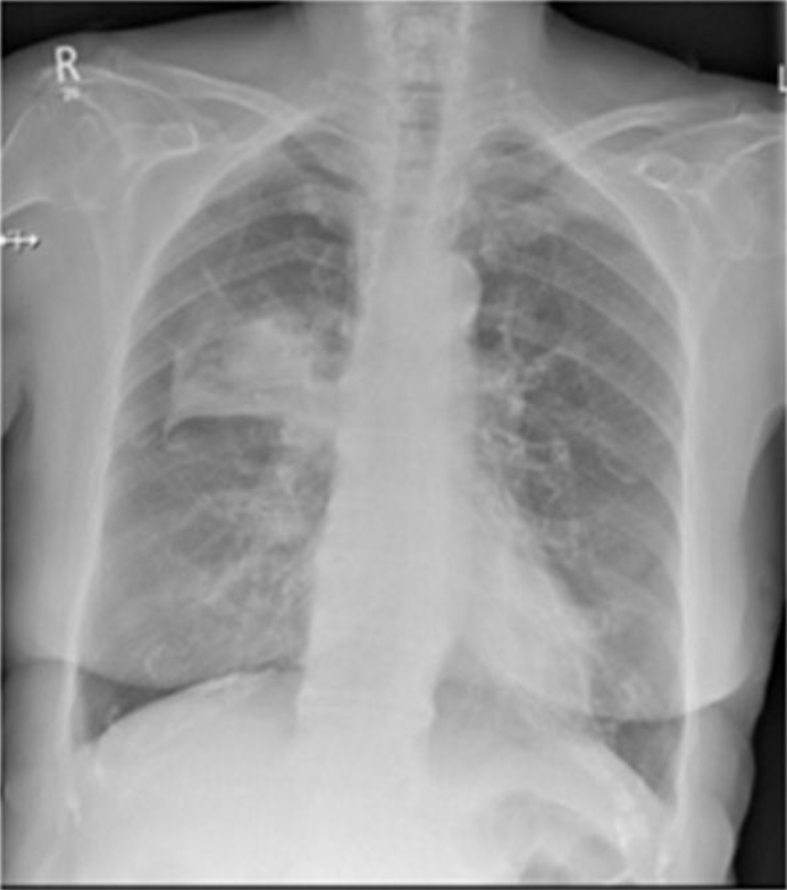
Fig. 4.
Chest radiograph (left) revealing right upper lobe consolidation/collapse.
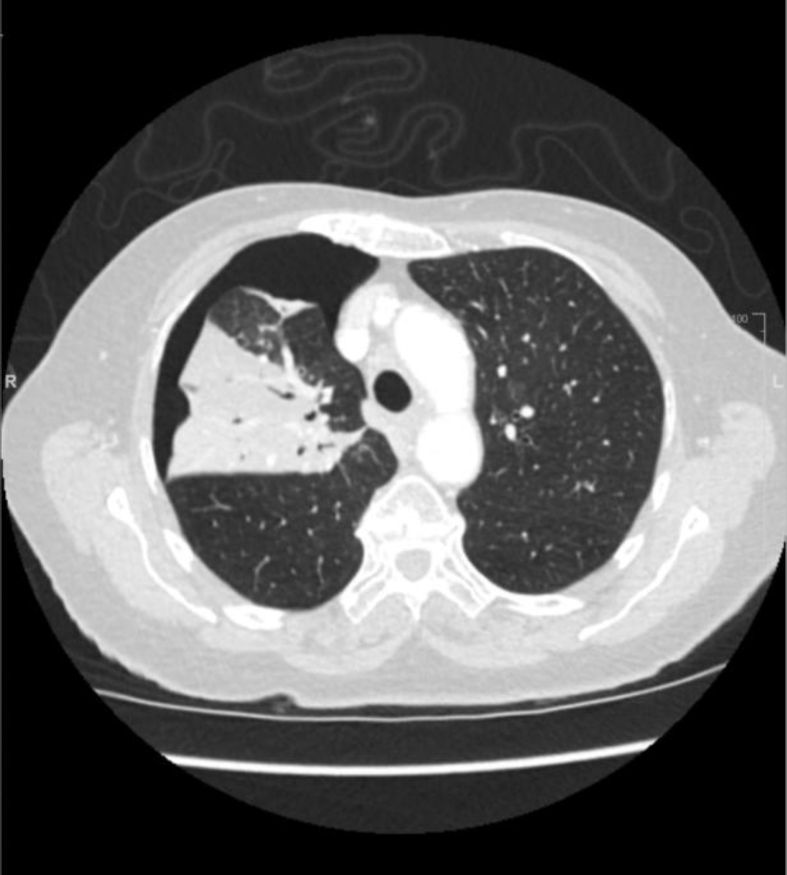
Fig. 5.
CT chest (right) showing right upper lobe consolidation and pneumothorax.
4. Discussion
COP has been recognised as an infrequent but important entity in respiratory medicine, often being a diagnosis of exclusion when patients do not respond to high dose intravenous antibiotics for pneumonia. It has been illustrated as a spectrum disorder based on clinical and radiological findings: acute (potentially fatal), sub-acute and progressive [5]. There does not seem to be a gender predominance in this disease. The majority of cases described commonly present with dyspnoea, cough, pyrexia, malaise and hypoxia; uncommon presentations including pleuritic chest pain, haemoptysis and arthralgia and night sweats have also been highlighted. Imaging including chest radiographs and CT chest provide crucial clues to diagnosis, often showing characteristic patterns in typical cases. By far, the most common abnormality observed is bilateral patchy alveolar opacities; less commonly diffuse interstitial patterns, localised consolidation, unilateral patchy alveolar infiltrates and occasionally solitary nodular densities are seen [5].
Since its recognition, it remains a diagnostic conundrum for clinicians, as it usually requires a triad of pathological, clinico-radiological findings with an idiopathic cause for the disease. The pathological hallmark of organising pneumonia includes the presence of granulation buds affecting adjacent alveoli and bronchi, which results in mechanical obstruction of the smaller airways [1]. Inflammation and recruitment of foamy macrophages then occurs, especially in alveoli that are not filled with granulation tissue. It is thought that these inflammatory plugs provides a ball-valve effect mechanism as they cause localised and peripheral obstruction, leading to over-distension of the distal airspaces which subsequently causing alveoli to burst. However, spontaneous pneumothorax remains a rare complication of COP, only gaining its first recognition in the early 20th century. Fatal and complicated recovery has been reported in cases describing COP and spontaneous pneumothorax [6], [7]. Furthermore, it has also been recognised as a presenting feature as well as complication of the condition.
As such, clinical awareness is essential for effective management of COP. Lung biopsy remains the preferred choice of investigation for establishing diagnosis. Among the various types of procedures, video-assisted thoracoscopy is preferred compared to cytologic bronchoalveolar lavage and trans-bronchial lung biopsy, since large specimens are required for diagnosis to be made in sufficient confidence [8]. However, invasive investigations like lung biopsies mandate careful patient selection and consideration of cost and risks. The increasing interest in the value of utilizing serum biomarkers, especially procalcitonin, has offered a valuable alternative to invasive investigations in suspected COP. This is especially useful considering the similarity in clinical and radiological presentations between infective pneumonia and COP, both which can also present with high levels of WBC and CRP counts. It has been shown to be a sensitive and specific biomarker in differentiating between COP and community-acquired pneumonia (CAP). Yet, there have been limited large scale studies in stratifying the accuracy of procalcitonin in the diagnosis of COP, mostly because of its rarity as a distinct clinical entity.
To the best of our knowledge, this is the first case of COP, presenting with spontaneous pneumothorax, where the serum biomarker procalcitonin has been utilised to guide diagnosis and management, subsequently achieving excellent clinical outcome without the need of invasive investigations. In case 1, lack of clinical suspicion resulted in a non-healing pneumothorax and the patient required surgery. However, the lessons learnt whilst managing case 1 helped us in identifying the proximate cause quite early on in the management of case 2. Even though no surgical biopsy was done in case 2, the clinical presentation and rapidity of response to corticosteroids on a background of normal procalcitonin levels clearly points to COP as the most probable diagnosis. Minimal antibiotic therapy was continued due to worry about very high CRP but wasn't necessary. Our case also highlights the importance of early steroid therapy in achieving adequate healing without invasive interventions.
There has not been an agreed guideline on the ideal dose and duration of steroids for COP, but initial doses of 0.75 mg/kg/day to 1.5 mg/kg/day have been suggested, followed by weaning doses over a period of weeks to months. As relapse in COP is common, long term steroid therapy is sometimes required [9].
References
- 1.Epler G. Broncholitis obliterans organizing pneumonia. N. Eng. J. Med. 1985;312:152–158. doi: 10.1056/NEJM198501173120304. [DOI] [PubMed] [Google Scholar]
- 2.Yang Idiopathic broncholitis obliterans with organizing pneumonia presenting with spontaneous hydropneumothorax and solitary pulmonary nodule. Respirology. 1999;4:267–270. doi: 10.1046/j.1440-1843.1999.00187.x. [DOI] [PubMed] [Google Scholar]
- 3.Takeda Satoshi. Clinical utility of procalcitonin for differentiating between cryptogenic organizing pneumonia and community-acquired pneumonia. Int. J. Clin. Med. 2015;6:372–376. [Google Scholar]
- 4.Limper The diagnostic role of procalcitonin and other biomarkers in discriminating infectious from non-infectious fever. J. Infect. 2010;60(6):409–416. doi: 10.1016/j.jinf.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 5.Cordier J.-F. Cryptogenic organising pneumonia. Eur. Respir. J. 2006;28:422–446. doi: 10.1183/09031936.06.00013505. [DOI] [PubMed] [Google Scholar]
- 6.Lee P.C. Spontaneous pneumothorax after steroid treatment in a patient with bronchiolitis obliterans organizing pneumonia. J. Formos. Med. Assoc. 2005;104(3):190–193. [PubMed] [Google Scholar]
- 7.Chakravorty Rapidly progressive bronchiolitis obliterans organising pneumonia presenting with pneumothorax, persistent air leak, acute respiratory distress syndrome and multi-organ dysfunction: a case report. J. Med. Case Rep. Jan 2008;2(145):1752–1947. doi: 10.1186/1752-1947-2-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yebra M. Percutaneous lung biopsy in the diagnosis of bronchiolitis obliterans organizing pneumonia. Chest. 1994 March;105(3):972–973. doi: 10.1378/chest.105.3.972b. [DOI] [PubMed] [Google Scholar]
- 9.Lazor R. Cryptogenic organizing pneumonia. Characteristics of relapses in a series of 48 patients. Am. J. Respir. Crit. Care Med. 2000;162:571–577. doi: 10.1164/ajrccm.162.2.9909015. [DOI] [PubMed] [Google Scholar]