Abstract
Purpose
To estimate the prevalence of women diagnosed with uterine fibroids and the associated symptom burden in the US.
Patients and methods
Responses of women aged 18–54 years, who completed an online survey, were analyzed. Data were weighted based on age, education, race, geographic region, income, and propensity score to derive national estimates of the prevalence of women diagnosed with uterine fibroids and associated symptom burden. Weighted means and percentages were reported. Prevalence across age and ethnic groups was examined. Symptom burden among women with and without uterine fibroids was compared using weighted logistic regressions.
Results
Of 59,411 respondents who met study inclusion criteria, 7.7% reported receiving a diagnosis of uterine fibroids. Of these, 5,670 women (1,402 in the uterine fibroid group and 4,268 in the control group) were excluded from analysis because they had a hysterectomy. Among the non-hysterectomized study participants, 3,031 self-reported a diagnosis of uterine fibroids (prevalence: 5.8%, 95% confidence interval [CI]: 5.5%–6.1%); prevalence increased as women aged and was greatest in the 50–54 age group (11.4%; 95% CI: 10.4%–12.4%). In addition, prevalence was greater in black vs white women (9.8%; 95% CI: 8.7%–11.0% vs 5.4%; 95% CI: 5.1%–5.7%). A greater percentage of women with uterine fibroids (vs those without) experienced severe heavy menstrual bleeding (16.7% vs 7.7%), severe constipation/bloating/diarrhea (7.7% vs 4.7%), severe passage of clots (6.7% vs 2.4%), severe spotting/bleeding between periods (1.7% vs 1.0%), and severe pelvic pressure (1.6% vs 0.6%). Among uterine fibroid patients with these typical uterine fibroid-related symptoms, 56.4%, 32.3%, 26.4%, 25.8%, and 20.4% reported heavy menstrual bleeding, passage of clots, spotting/bleeding between periods, constipation/bloating/diarrhea, and pelvic pressure, respectively, as extremely bothersome.
Conclusion
Uterine fibroids impose a heavy burden on women aged 18–54 years in the US.
Keywords: frequency, leiomyoma, signs and symptoms, questionnaire
Introduction
Uterine leiomyomata (fibroids), benign tumors of uterine smooth muscle, are one of the most prevalent tumors of the female reproductive system.1 Prevalence estimates of uterine fibroid disease vary ranging from 5.4% to 23.6% depending on the age group assessed, diagnostic methods used, and whether asymptomatic women were included in the analysis.2–6 Hysterectomy has been the most common intervention for uterine fibroids in the US.7,8
Many women who have uterine fibroids do not have symptoms and the condition may not be diagnosed.9,10 Among women who experience symptoms, abnormal bleeding (eg, heavy bleeding, prolonged bleeding, frequent periods, or irregular/unpredictable periods), pelvic pain, and dyspareunia are the most frequently reported symptoms.6,11–13 Several studies have documented how uterine fibroids and their associated symptoms may significantly impair a woman’s health-related quality of life (HRQL).2,14 Uterine fibroids are associated with a significant economic burden as well; total annual costs have been estimated to be $6 to $34 billion in the US.15,16
Uterine fibroids are more prevalent and develop at an earlier age with more severe symptoms in black/African American women than in white women.4,17–20 Although heavy menstrual bleeding and pelvic pain are often reported as the main symptoms,6,21 the total symptom burden associated with this disease has not been assessed for the general population of women in the US. Thus, the purpose of this study was to estimate the prevalence of uterine fibroids in women aged 18–54 years and the associated symptom burden among those women in the US, using a large nationally representative sample.
Material and methods
We conducted a cross-sectional survey of 59,411 women aged 18–54 years in the US from August 6, 2012, through September 14, 2012.22 The Harris Poll Online panel (Harris Interactive, New York, NY, US), Global Market Insite (GMI) respondents panel (Lightspeed Research, Warren, NJ, US), and E-rewards opinion panel (Research Now Group, Inc., Plano, TX, US) were used as the sampling frame for this analysis.14,18,23,24 All panel respondents were required to accept the site terms and privacy policy before opting into the panel. Recently published results from this survey focusing on the prevalence and symptom burden among patients with endometriosis used the same methodology and a similar analytic approach as outlined in the following paragraphs.22 A weighting algorithm with propensity score adjustment for distributions in age, education, race, region, and household income was used so that the survey sample would be representative of the general US population.25 Potential respondents received an email invitation, which described the study and directed the recipients to the survey website. Participants who met the study criteria and completed the survey received points and chances in a sweepstakes for cash prizes. The authors were not involved in the rewards program and had no contact with survey respondents. Only participants who provided electronic informed consent via an online form were permitted to complete the full survey. Women who were 18 to 54 years of age were eligible to participate in the survey if they had been diagnosed with uterine fibroids, or had symptoms associated with uterine fibroid disease, or were being treated for uterine fibroid disease, or had a hysterectomy. As part of the survey, respondents were asked “Has a doctor ever told you that you have or are suspected of having uterine fibroids (or leiomyomas)?” To identify women with symptoms of uterine fibroid disease, respondents were asked if they had ever experienced any of the following symptoms and to select all that applied: heavy bleeding during periods, spotting/bleeding between periods, passage of clots, pelvic pressure, and bloating. All data were reported by the respondents and were collected through an online survey.
The survey was fielded in the US and globally; this manuscript focuses on the US data only. The survey consisted of two parts: the first part collected information that could be used to estimate the prevalence of uterine fibroids and the associated symptom burden, and the second part provided information that was more specific to HRQL, health-related productivity, surgery intentions, treatment history, and the cost burden associated with uterine fibroid disease. This study focused on information collected in the first part of the survey, which included questions on demographics, whether respondents had ever received a diagnosis of uterine fibroids, whether they had ever experienced any of a comprehensive list of gynecological and non-gynecological symptoms, whether they experienced symptoms during the 4 weeks before the survey was conducted, and whether they had any coexisting conditions. Among the symptoms queried, the following were considered to be typical uterine fibroid-related symptoms: heavy bleeding during periods, spotting/bleeding between periods, passage of clots, pelvic pressure, and constipation/bloating/diarrhea. Women who reported having symptoms were asked to indicate how bothersome and how severe they found their symptoms to be. Women with a diagnosis of uterine fibroids were also asked about the methods used to diagnose their uterine fibroids, and if they were receiving treatment for their uterine fibroids.
Women who reported having a hysterectomy were excluded from statistical analyses. Weighted means and percentages were used to summarize continuous and categorical variables. Because survey respondents were required to choose symptoms (that they were currently experiencing or had ever experienced) from a comprehensive list of symptoms, those who did not pick a certain symptom from the list were considered to have not experienced that symptom. This conservative approach was used to analyze data obtained in a recent cross-sectional survey examining the effect of endometriosis on the quality of life of women.26 Respondents were asked to rate the level of severity (mild, moderate, or severe) for any symptoms that they experienced in the month before completing the survey. Respondents who never experienced the symptom, as well as those who did not experience the symptom during the month before survey administration were assigned to the “no symptom” group.
Prevalence trends across age and ethnic groups were also examined. The Rao-Scott chi-square test27 was used to assess differences between women with uterine fibroids and controls (survey respondents without fibroids) in baseline comorbidities, symptoms experienced, severe symptoms experienced, and how bothersome women found their symptoms. Odds ratios of experiencing individual symptoms and their corresponding 95% confidence intervals (CIs) were derived from logistic regression analyses controlling for age and race. Similar logistic models were used to estimate the odds of experiencing the severe form of the symptoms. All data analyses were completed using SAS 9.2 (SAS Institute, Inc., Cary, NC, US).
This study was reviewed and approved by the Copernicus Group Institutional Review Board.
Results
Of the 382,797 potential respondents who were contacted, 59,411 (15.5%) were 18–54 years of age, met the study inclusion criteria, completed the survey, and 7.7% reported having uterine fibroids. Of these 59,411 women, 9.5% (5,670 women) had a hysterectomy; 32.1% (1,402 of 4,433) of women in the uterine fibroid group vs 7.4% (4,268 of 54,978) of women in the control group. Women who reported having a hysterectomy were excluded from the analysis. Of the 53,741 non-hysterectomized women, 3,031 (5.8%, 95% CI: 5.5%–6.1%) reported receiving a diagnosis of uterine fibroids (Table 1). The average age of patients with uterine fibroids at the time the survey was conducted was 43.4 years compared with 35.3 years in controls (P<0.0001), and the average age at the time of the diagnosis was 36.4 years. Most (84.1%) study participants had their diagnosis of uterine fibroids confirmed by surgical methods (laparoscopy, laparotomy, or other surgical procedure). More than half of the women in the uterine fibroid and control groups were white (62.6% and 67.0%, respectively). There was a fairly even distribution (20.1%–31.8%) of study respondents across the geographic regions of the US. A significantly (P<0.005) greater percentage of women with uterine fibroids vs controls reported gynecological conditions: endometriosis (16.5% vs 4.1%), infertility (8.6% vs 3.8%), polycystic ovarian syndrome (7.6% vs 4.1%), endometrial hyperplasia (5.7% vs 0.9%), adenomyosis (4.4% vs 0.5%), breast cancer (1.9% vs 1.0%), and ovarian cancer (1.2% vs 0.5%); as well as other medical conditions: anemia (35.0% vs 19.0%), obesity (28.9% vs 18.0%), depression (28.8% vs 25.4%), hypertension (24.4% vs 12.8%), high cholesterol (23.8% vs 13.5%), diabetes (8.5% vs 5.7%), and osteoporosis (3.9% vs 2.2%).
Table 1.
Demographics of study population
| Parameter | Patients with uterine fibroids (n=3,031) | Controls (n=50,710) | P-value |
|---|---|---|---|
| Average age (years) | 43.4 | 35.3 | <0.0001 |
| Age groups (years), n (%) | <0.0001 | ||
| 18–29 | 127 (4.9) | 14,447 (34.0) | |
| 30–34 | 243 (10.0) | 7,998 (15.9) | |
| 35–39 | 391 (13.9) | 6,677 (12.9) | |
| 40–44 | 590 (21.0) | 6,753 (12.9) | |
| 45–49 | 745 (25.4) | 6,967 (12.4) | |
| 50–54 | 935 (24.9) | 7,868 (11.8) | |
| Average age at diagnosis (years) | 36.4 | – | |
| Experiencing symptoms before diagnosis, n (%) | 1,977 (73.1) | – | |
| Diagnostic method, n (%) | |||
| Surgical | 2,537 (84.1) | – | |
| Physician-suspecteda | 199 (7.2) | – | |
| Otherb | 295 (8.7) | – | |
| Ethnicity, n (%) | <0.0001 | ||
| White | 2,169 (62.6) | 38,413 (67.0) | |
| Black/African American | 460 (23.2) | 4,108 (13.1) | |
| Other | 402 (14.2) | 8,189 (19.9) | |
| Geographic regions, n (%) | 0.0183 | ||
| East | 779 (24.5) | 11,546 (21.6) | |
| Midwest | 680 (20.1) | 12,440 (21.7) | |
| South | 906 (31.8) | 15,353 (32.4) | |
| West | 609 (21.9) | 10,744 (23.2) | |
| Unknown | 57 (1.7) | 627 (1.1) | |
| Type of insurance, n (%)c | <0.0001 | ||
| Public | 180 (12.0) | 979 (13.9) | |
| Private | 922 (66.6) | 3,977 (54.8) | |
| Other | 145 (8.8) | 1,008 (13.5) | |
| None | 189 (12.6) | 1,287 (17.8) | |
| Education level, n (%) | <0.0001 | ||
| High school or less | 365 (18.6) | 9,511 (28.6) | |
| Some college/college | 2,023 (66.9) | 32,792 (61.6) | |
| Graduate education | 643 (14.5) | 8,407 (9.9) | |
Notes:
Physician-suspected responses reported included: ultrasound/sonogram or other imaging test (eg, magnetic resonance imaging) results; physical or pelvic examination results; patient’s description of the heavy or irregular bleeding; patient’s family history; blood test indicating the patient was anemic; patient had a hysterectomy; or patient was infertile.
Response of “other” or “not sure” or the respondent declined to answer.
Total number of respondents providing an answer for question on type of insurance was 1,436 women in the uterine fibroid group and 7,251 women in the control group.
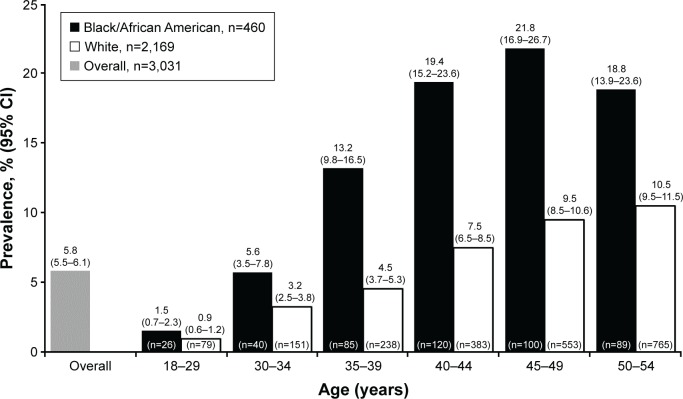
When examined across different age groups, the prevalence of uterine fibroids increased as women aged and was greatest in the 50–54 age group (11.4%; 95% CI: 10.4%–12.4%). Prevalence was 0.9% (95% CI: 0.7%–1.1%), 3.7% (95% CI: 3.1%–4.3%), 6.2% (95% CI: 5.3%–7.0%), 9.0% (95% CI: 0.7%–1.1%), and 11.1% (95% CI: 10.1%–12.2%) in the 18–29, 30–34, 35–39, 40–44, and 50–54 age groups, respectively. The prevalence of uterine fibroids was greater in black/African American women than in white women (9.8%; 95% CI: 8.7%–11.0% vs 5.4%; 95% CI: 5.1%–5.7%). As in the overall population, the prevalence of uterine fibroids in both black/African American and white women increased with increasing age (Figure 1).
Figure 1.
Prevalence of uterine fibroids across different age groups in black/African American and white women.
Abbreviation: CI, confidence interval.
Typical uterine fibroid symptoms of spotting/bleeding between periods, heavy menstrual bleeding, constipation/bloating/diarrhea, passage of clots, and pelvic pressure were reported by 74.9%, 73.4%, 63.3%, 56.9%, and 22.4% of women with uterine fibroids at some time in the past (Table 2). Among the women who experienced these symptoms at some time in the past, 23.1%, 44.2%, 53.9%, 33.6%, and 16.4%, respectively, were still experiencing these symptoms during the month before the survey was conducted (Table 3).
Table 2.
Distribution of uterine fibroid-related symptoms ever experienced in patients with uterine fibroids and controls
| Symptom | Patients with uterine fibroids (n=3,031) | Controls (n=50,710) | Odds ratio (95% CI)a |
|---|---|---|---|
| Menstrual pelvic pain/cramping | 2,277 (74.9) | 28,994 (59.0) | 2.8 (2.5, 3.2) |
| Non-menstrual pelvic pain/cramping | 984 (33.2) | 9,089 (19.3) | 2.9 (2.5, 3.2) |
| Pain during sex | 851 (29.3) | 10,277 (21.0) | 2.1 (1.9, 2.4) |
| Heavy menstrual bleeding | 2,147 (73.4) | 22,240 (45.7) | 3.5 (3.1, 3.9) |
| Spotting/bleeding between periods | 1,342 (45.0) | 12,295 (25.0) | 3.0 (2.6, 3.3) |
| Passage of clots | 1,690 (56.9) | 13,202 (26.4) | 3.3 (2.9, 3.6) |
| Irregular periods | 1,698 (57.8) | 20,919 (42.0) | 2.4 (2.1, 2.6) |
| Pelvic pressure | 654 (22.4) | 4,782 (10.3) | 2.9 (2.6, 3.4) |
| Lower back pain | 2,090 (68.4) | 27,774 (56.2) | 1.9 (1.7, 2.1) |
| General abdominal pain | 1,019 (35.0) | 11,770 (24.4) | 2.1 (1.9, 2.3) |
| Constipation/bloating/diarrhea | 1,859 (63.3) | 24,124 (50.0) | 2.2 (2.0, 2.5) |
| Difficulty having a bowel movement | 1,140 (38.9) | 14,880 (30.6) | 1.6 (1.5, 1.8) |
| Fatigue/weariness/anemia | 2,069 (68.3) | 24,734 (50.0) | 2.4 (2.1, 2.7) |
| Infertility | 384 (12.0) | 2,980 (5.8) | 1.9 (1.6, 2.3) |
Notes:
Controlling for age and race. Data presented as n (weighted %) unless stated otherwise.
Abbreviation: CI, confidence interval.
Table 3.
Distribution of uterine fibroid-related symptoms during the 4 weeks before survey administration in patients with uterine fibroids and controls
| Symptom | Patients with uterine fibroids (n=3,031) | Controls (n=50,710) | Odds ratio (95% CI)a |
|---|---|---|---|
| Overall population | |||
| Menstrual pelvic pain/cramping | 1,492 (51.4) | 20,643 (43.7) | 2.1 (1.9, 2.3) |
| Non-menstrual pelvic pain/cramping | 683 (23.6) | 6,355 (14.1) | 2.7 (2.4, 3.1) |
| Pain during sex | 485 (16.9) | 6,130 (13.2) | 1.8 (1.6, 2.2) |
| Heavy menstrual bleeding | 1,238 (44.2) | 14,045 (30.5) | 2.2 (1.9, 2.4) |
| Spotting/bleeding between periods | 664 (23.0) | 6,130 (13.3) | 2.7 (2.4, 3.0) |
| Passage of clots | 961 (33.6) | 7,913 (16.6) | 2.5 (2.2, 2.8) |
| Irregular periods | 948 (33.3) | 11,997 (25.4) | 2.0 (1.7, 2.2) |
| Pelvic pressure | 467 (16.4) | 3,307 (7.4) | 3.0 (2.6, 3.5) |
| Lower back pain | 1,768 (58.2) | 23,849 (49.1) | 1.6 (1.5, 1.8) |
| General abdominal pain | 772 (26.3) | 8,567 (18.6) | 2.0 (1.8, 2.3) |
| Constipation/bloating/diarrhea | 1,572 (53.9) | 19,875 (42.2) | 2.1 (1.9, 2.3) |
| Difficulty having a bowel movement | 909 (31.6) | 11,515 (24.1) | 1.6 (1.5, 1.8) |
| Fatigue/weariness/anemia | 1,827 (60.5) | 22,014 (44.7) | 2.1 (1.9, 2.4) |
| Infertility | 212 (6.7) | 1,615 (3.4) | 2.1 (1.7, 2.6) |
| Patients with severe symptoms | |||
| Menstrual pelvic pain/cramping | 302 (11.8) | 3,238 (7.6) | 2.3 (1.9, 2.8) |
| Non-menstrual pelvic pain/cramping | 65 (2.3) | 558 (1.4) | 2.7 (1.8, 3.8) |
| Pain during sex | 56 (1.9) | 546 (1.3) | 1.9 (1.2, 2.8) |
| Heavy menstrual bleeding | 461 (16.7) | 3,354 (7.7) | 2.5 (2.1, 2.9) |
| Spotting/bleeding between periods | 59 (1.7) | 416 (1.0) | 2.6 (1.7, 3.9) |
| Passage of clots | 199 (6.7) | 1,087 (2.4) | 2.5 (2.0, 3.2) |
| Irregular periods | 221 (8.2) | 2,348 (5.3) | 2.3 (1.9, 2.9) |
| Pelvic pressure | 43 (1.6) | 270 (0.6) | 3.8 (2.3, 6.1) |
| Lower back pain | 307 (10.4) | 3,608 (8.4) | 1.4 (1.2, 1.7) |
| General abdominal pain | 70 (2.4) | 645 (1.6) | 1.9 (1.3, 2.7) |
| Constipation/bloating/diarrhea | 207 (7.7) | 1,992 (4.7) | 2.1 (1.7, 2.7) |
| Difficulty having a bowel movement | 122 (4.5) | 1,459 (3.5) | 1.5 (1.2, 2.0) |
| Fatigue/weariness/anemia | 407 (13.8) | 3,644 (7.8) | 2.1 (1.8, 2.5) |
| Infertility | 131 (3.9) | 969 (2.0) | 1.8 (1.4, 2.4) |
Notes:
Controlling for age and race. Data presented as n (weighted %) unless stated otherwise.
Abbreviation: CI, confidence interval.
Women with uterine fibroids were more likely to have severe heavy menstrual bleeding (16.7% vs 7.7%), severe constipation/bloating/diarrhea (7.7% vs 4.7%), severe passage of clots (6.7% vs 2.4%), severe spotting/bleeding between periods (1.7% vs 1.0%), and severe pelvic pressure (1.6% vs 0.6%) compared with women in the control group (Table 3). Among study respondents with typical uterine fibroid-related symptoms, 59.3%, 58.3%, 52.8%, 46.7%, and 35.5% reported constipation/bloating/diarrhea, pelvic pressure, spotting/bleeding between periods, passage of clots, and heavy menstrual bleeding, respectively, as somewhat bothersome (Table 4). The percentage of women who reported heavy menstrual bleeding, passage of clots, spotting/bleeding between periods, constipation/bloating/diarrhea, and pelvic pressure as extremely bothersome was 56.4%, 32.3%, 26.4%, 25.8%, and 20.4%, respectively.
Table 4.
Symptoms’ bothersomeness among uterine fibroid patients
| Symptom | Not at all bothersome | Somewhat bothersome | Extremely bothersome |
|---|---|---|---|
| Menstrual pelvic pain/cramping | 179 (10.1) | 878 (57.3) | 435 (32.6) |
| Non-menstrual pelvic pain/cramping | 115 (17.0) | 430 (58.6) | 138 (24.4) |
| Pain during sex | 54 (10.5) | 269 (54.3) | 162 (35.2) |
| Heavy menstrual bleeding | 106 (8.0) | 451 (35.5) | 681 (56.4) |
| Spotting/bleeding between periods | 131 (20.8) | 366 (52.8) | 167 (26.4) |
| Passage of clots | 221 (21.2) | 434 (46.7) | 306 (32.2) |
| Irregular periods | 194 (18.2) | 447 (46.6) | 307 (35.2) |
| Pelvic pressure | 96 (21.2) | 287 (58.3) | 84 (20.4) |
| Lower back pain | 174 (9.4) | 1,097 (59.0) | 497 (31.5) |
| General abdominal pain | 115 (15.0) | 516 (63.3) | 141 (21.8) |
| Constipation/bloating/diarrhea | 240 (15.0) | 970 (59.3) | 362 (25.8) |
| Difficulty having a bowel movement | 104 (9.8) | 541 (58.4) | 264 (31.7) |
| Fatigue/weariness/anemia | 148 (7.0) | 1,016 (56.0) | 663 (37.0) |
| Infertility | 63 (26.6) | 47 (23.5) | 102 (49.9) |
Note: Data presented as n (weighted %) unless stated otherwise.
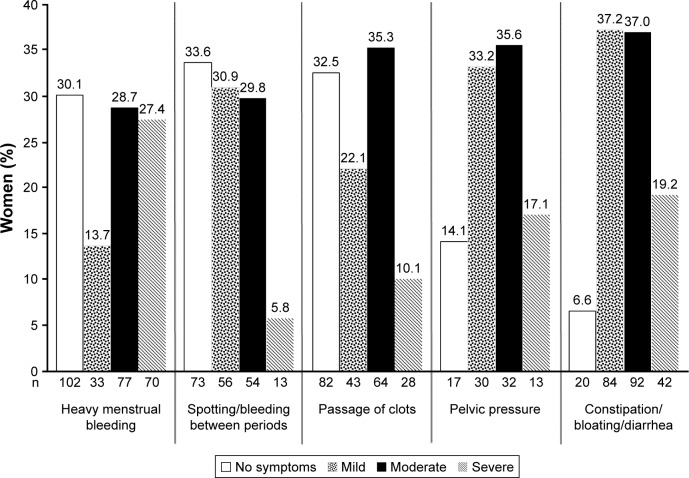
Among the women currently being treated for uterine fibroid disease, 56.2%, 56.1%, 52.7%, 45.4%, and 35.6% were experiencing moderate or severe constipation/bloating diarrhea, heavy menstrual bleeding, pelvic pressure, passage of clots, and spotting/bleeding between periods, respectively (Figure 2).
Figure 2.
Severity of typical uterine fibroid-related symptoms among respondents who were being treated for uterine fibroids at the time of the survey.
Discussion
This study is among the first to provide a comprehensive assessment of the symptom experience of women diagnosed with uterine fibroids in terms of past history, current experience, severity of uterine fibroid-related symptoms and the degree to which survey respondents were bothered by their symptoms. The prevalence of uterine fibroids and the symptom distribution by age and race were also assessed.
Direct comparisons of results across studies evaluating the prevalence or incidence of uterine fibroid disease are difficult to make because of differences in the study sample size, populations, and methodology.2–6 For example in our study, the prevalence of uterine fibroids was 5.8%, which is lower than the prevalence of 6.9% for women in the US reported by Zimmerman et al.6 Although both studies were online surveys and recruited study participants via an online-panel, the prevalence estimates may be different because the inclusion criteria in our study were more flexible in terms of age (18–54 years) and were not limited to patients who are currently symptomatic. Broadening the inclusion criteria enabled a more generalized estimate of uterine fibroid prevalence and burden among the US female population. Other differences between the two studies were the inclusion/exclusion of hysterectomized patients and total number of patients surveyed. Prevalence estimates from an internet-based survey2 conducted in Western European countries (including France, Germany, Italy, Spain, and the United Kingdom) ranged from 11.7% to 23.6%; these estimates are higher than prevalence estimates in our study and Zimmerman’s study,6 and may be due to the smaller sample size analyzed (a total of 1,756 women, evenly distributed across the five countries) or may result from differences in how it was ascertained that women had uterine fibroids. In our study, most participants (84.1%) had their diagnosis confirmed by surgical methods. In Zimmerman’s study,6 participants were told by a doctor or health care professional that they had uterine fibroid disease. In Downes’s study,2 results were reported for women with a diagnosis of uterine fibroids, those who had surgery to treat uterine fibroids, those actively taking prescription medication or an over-the-counter product to treat uterine fibroids as well as those experiencing uterine fibroid-related symptoms or inter-menstrual bleeding.2
In our study, a 13-fold increase in the prevalence of uterine fibroids was seen as age increased (0.9% vs 11.4% in the 18–29 and 50–54 age groups, respectively). This increase may be attributed to multiple factors, among which are variable levels of hormones among different age groups, increased rate of screening and/or diagnosis as age increases, and potential change in fibroid size that may be linked to aging.11,28–32 We found that the prevalence of uterine fibroids was 1.8 times greater in black/African American women than in white women (9.8% vs 5.4%). These results are consistent with other studies documenting higher prevalence of the disease, more severe disease, and a greater symptom burden among African American women.4,17–20
Our analysis also shows that women with uterine fibroids were 2.5 times more likely to have severe heavy menstrual bleeding than women who did not have uterine fibroids. Anemia, a possible consequence of severe menstrual bleeding, was 2.3 times greater in women with uterine fibroids compared with controls. The higher rate of anemia is not unexpected because heavy menstrual bleeding is one of the hallmark symptoms of uterine fibroids.6,21 Similar trends were observed for other bleeding symptoms; women with uterine fibroids were 2 to 3 times more likely to experience severe spotting/bleeding between periods or passage of clots than women without uterine fibroids. Although these findings agree with other studies evaluating bleeding symptoms in women with uterine fibroids,6,12 we took our analysis a step further and assessed bleeding and non-bleeding symptoms from a historical perspective as well as from a current perspective. We found that 73.4% of respondents with uterine fibroids in our study reported that they had experienced heavy menstrual bleeding at some time in the past, 44.2% were currently experiencing heavy menstrual bleeding, and of those currently being treated, 16.7% were still experiencing severe heavy menstrual bleeding with 56.4% of these women rating heavy menstrual bleeding as an extremely bothersome symptom.
Non-bleeding symptoms are also commonly experienced by patients with uterine fibroids. Both Zimmermann et al,6 and Lippman et al,13 reported that women with uterine fibroids experienced more severe forms of dyspareunia and non-cyclical pelvic pain compared to those without uterine fibroids. Also, Zimmermann et al,6 reported that women were more likely to experience pain-related symptoms compared with controls. Nonetheless, the prevalence and severity of these symptoms in uterine fibroids remains an understudied area in assessing the overall uterine fibroid-related symptomatic burden. We found that more than 60% of women with uterine fibroids reported lower back pain and constipation/bloating/diarrhea; approximately one-third reported general abdominal pain, non-menstrual pelvic pain, and pain during sex at some point in the past. Approximately half of the women with uterine fibroids reported lower back pain and constipation/bloating/diarrhea; 22% reported general abdominal pain, non-menstrual pelvic pain, and pain during sex at the time the survey was conducted; and ~28% rated these symptoms as extremely bothersome. These results indicate that in addition to typical bleeding symptoms, non-bleeding symptoms are a substantial burden among women with uterine fibroids.
Recently, notable research efforts have been directed to evaluating the symptom burden of uterine fibroids in the US using national surveys.14,18 Although our study and the aforementioned studies highlight the substantial burden of uterine fibroid disease, our study offers some unique perspectives. First, we captured the symptom burden in a much younger population of women (18–54 years of age), which allowed us to examine disease experience among women who have disease onset during adolescence. Second, by comparing women with and without uterine fibroids, we were able to assess how women experience the disease and quantify differences between those who have the disease and those who do not. Third, we excluded women who had a hysterectomy from our analysis to eliminate the effect of hysterectomy on symptom burden. Finally, our sampling frame included asymptomatic patients. Thus, our assessment of the disease burden captured a woman’s experience with uterine fibroids across the various stages of the disease rather than just at the time symptoms were experienced.
Multiple cross-sectional studies have evaluated the management of uterine fibroid disease recently.6,14,33 Treatment can vary depending on the country because of health care system differences and cultural attitudes toward treatments. A recent study examining treatment patterns in eight different countries found that the number of women with uterine fibroids who received medical treatment after diagnosis ranged from 18.5% in Germany to 55.8% in Brazil.6 A second study, which was conducted in the US, investigated women’s concerns about treatment options for uterine fibroid disease and found that 79% of the women surveyed wanted to have non-invasive treatment options.14 In this study, we found that approximately half of the women currently being treated for typical uterine fibroid-related symptoms were still experiencing moderate or severe symptoms. This proportion may be even higher if past treatment history is taken into account. Future studies need to evaluate how effective current treatments are, how satisfied patients are with their current treatment, and why so many women are not receiving treatment to alleviate their symptoms. A few other issues remain to be examined in future research. For instance, several studies have documented the negative impact of uterine fibroid on various aspects of a woman’s HRQL,6,14,34,35 but more comprehensive studies are needed to determine how the full spectrum of bleeding and non-bleeding symptoms adversely affects HRQL and work productivity among affected women.
A noteworthy strength of this study is its sample size; this study is among the largest, in terms of the number of study participants, to explore the prevalence and symptom experience of uterine fibroids among women in the US. Also, the study participants were equally distributed across the US, which makes the findings more applicable to the general population. One limitation of our study is that more than 50% of the study sample was non-African American women although uterine fibroid disease is known to be more prevalent among African American women; a finding that was corroborated by our study as well. In addition, when interpreting the results of this study, several possible sources of bias summarized in previous reports should be kept in mind.22 For example, this study includes data from individuals who responded to the survey and excludes individuals who were not members of the three respondent panels. Finally, uterine fibroid diagnosis in our study was self-reported. Thus, our analysis could not control for the extent of the disease (size, location, and number of fibroid tumors) which could influence the overall uterine fibroid symptomatic burden.
Conclusion
Uterine fibroids impose a heavy clinical burden on women aged 18–54 years in the US. The current analyses showed that women suffering from uterine fibroids are more prone to experiencing a plethora of gynecological bleeding and non-bleeding symptoms than women without fibroids. More research is needed to assess the quality of life implications of such a clinical burden in this population and how it affects the overall societal burden.
Acknowledgments
Medical writing assistance was provided by Joann Hettasch, PhD, of Arbor Communications, Inc., a member of the Fishawack Group of Companies, Conshohocken, Pennsylvania, and was funded by AbbVie. The authors would like to dedicate this manuscript to the memory of Dr Craig Alan Winkel, MD, MBA (1945–2016) for his significant contribution to the development of the manuscript.
Footnotes
Disclosure
Financial support for this study and for medical writing/editing services was provided by AbbVie, Inc. AbbVie participated in developing the study design; data collection, analysis and interpretation; writing, review, and approval of the manuscript, and the decision to submit the manuscript for publication. M Fuldeore and A Soliman are employees of AbbVie and may own stock in AbbVie.
References
- 1.Bulun SE. Uterine fibroids. N Engl J Med. 2013;369(14):1344–1355. doi: 10.1056/NEJMra1209993. [DOI] [PubMed] [Google Scholar]
- 2.Downes E, Sikirica V, Gilabert-Estelles J, et al. The burden of uterine fibroids in five European countries. Eur J Obstet Gynecol Reprod Biol. 2010;152(1):96–102. doi: 10.1016/j.ejogrb.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 3.Marino JL, Eskenazi B, Warner BM, et al. Uterine leiomyoma and menstrual cycle characteristics in a population-based cohort study. Hum Reprod. 2004;19(10):2350–2355. doi: 10.1093/humrep/deh407. [DOI] [PubMed] [Google Scholar]
- 4.Baird DD, Dunson DB, Hill MC, Cousins D, Schectman JM. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188(1):100–107. doi: 10.1067/mob.2003.99. [DOI] [PubMed] [Google Scholar]
- 5.Borgfeldt C, Andolf E. Transvaginal ultrasonographic findings in the uterus and the endometrium: low prevalence of leiomyoma in a random sample of women age 25–40 years. Acta Obstet Gynecol Scand. 2000;79(3):202–207. [PubMed] [Google Scholar]
- 6.Zimmermann A, Bernuit D, Gerlinger C, Schaefers M, Geppert K. Prevalence, symptoms and management of uterine fibroids: an international internet-based survey of 21,746 women. BMC Womens Health. 2012;12:6. doi: 10.1186/1472-6874-12-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Whiteman MK, Hillis SD, Jamieson DJ, et al. Inpatient hysterectomy surveillance in the United States, 2000–2004. Am J Obstet Gynecol. 2008;198(1):34.e1–e7. doi: 10.1016/j.ajog.2007.05.039. [DOI] [PubMed] [Google Scholar]
- 8.Wu JM, Wechter ME, Geller EJ, Nguyen TV, Visco AG. Hysterectomy rates in the United States, 2003. Obstet Gynecol. 2007;110(5):1091–1095. doi: 10.1097/01.AOG.0000285997.38553.4b. [DOI] [PubMed] [Google Scholar]
- 9.Okolo S. Incidence, aetiology and epidemiology of uterine fibroids. Best Pract Res Clin Obstet Gynaecol. 2008;22(4):571–588. doi: 10.1016/j.bpobgyn.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz SM, Marshall LM, Baird DD. Epidemiologic contributions to understanding the etiology of uterine leiomyomata. Environ Health Perspect. 2000;108(Suppl 5):821–827. doi: 10.1289/ehp.00108s5821. [DOI] [PubMed] [Google Scholar]
- 11.Ryan GL, Syrop CH, Van Voorhis BJ. Role, epidemiology, and natural history of benign uterine mass lesions. Clin Obstet Gynecol. 2005;48(2):312–324. doi: 10.1097/01.grf.0000159538.27221.8c. [DOI] [PubMed] [Google Scholar]
- 12.Wegienka G, Baird DD, Hertz-Picciotto I, et al. Self-reported heavy bleeding associated with uterine leiomyomata. Obstet Gynecol. 2003;101(3):431–437. doi: 10.1016/s0029-7844(02)03121-6. [DOI] [PubMed] [Google Scholar]
- 13.Lippman SA, Warner M, Samuels S, Olive D, Vercellini P, Eskenazi B. Uterine fibroids and gynecologic pain symptoms in a population-based study. Fertil Steril. 2003;80(6):1488–1494. doi: 10.1016/s0015-0282(03)02207-6. [DOI] [PubMed] [Google Scholar]
- 14.Borah BJ, Nicholson WK, Bradley L, Stewart EA. The impact of uterine leiomyomas: a national survey of affected women. Am J Obstet Gynecol. 2013;209(4):319.e1–e20. doi: 10.1016/j.ajog.2013.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Soliman AM, Yang H, Du EX, Kelkar SS, Winkel C. The direct and indirect costs of uterine fibroid tumors: a systematic review of the literature between 2000 and 2013. Am J Obstet Gynecol. 2015;213(2):141–160. doi: 10.1016/j.ajog.2015.03.019. [DOI] [PubMed] [Google Scholar]
- 16.Cardozo ER, Clark AD, Banks NK, Henne MB, Stegmann BJ, Segars JH. The estimated annual cost of uterine leiomyomata in the United States. Am J Obstet Gynecol. 2012;206(3):211.e1–e9. doi: 10.1016/j.ajog.2011.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eltoukhi HM, Modi MN, Weston M, Armstrong AY, Stewart EA. The health disparities of uterine fibroid tumors for African American women: a public health issue. Am J Obstet Gynecol. 2014;210(3):194–199. doi: 10.1016/j.ajog.2013.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stewart EA, Nicholson W, Bradley L, Borah B. The burden of uterine fibroids for African-American women: results of a national survey. J Womens Health (Larchmt) 2013;22(10):807–816. doi: 10.1089/jwh.2013.4334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jacoby VL, Fujimoto VY, Giudice LC, Kuppermann M, Washington AE. Racial and ethnic disparities in benign gynecologic conditions and associated surgeries. Am J Obstet Gynecol. 2010;202(6):514–521. doi: 10.1016/j.ajog.2010.02.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Weiss G, Noorhasan D, Schott LL, Powell L, Randolph JF, Jr, Johnston JM. Racial differences in women who have a hysterectomy for benign conditions. Womens Health Issues. 2009;19(3):202–210. doi: 10.1016/j.whi.2009.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stewart E. Uterine fibroids. Lancet. 2001;357(9252):293–298. doi: 10.1016/S0140-6736(00)03622-9. [DOI] [PubMed] [Google Scholar]
- 22.Fuldeore MJ, Soliman AM. Prevalence and symptomatic burden of diagnosed endometriosis in the United States: National estimates from a cross-sectional survey of 59,411 women. Gynecol Obstet Invest. 2016 Nov 8; doi: 10.1159/000452660. Epub. [DOI] [PubMed] [Google Scholar]
- 23.Work SS, Colamonico JA, Bradley WG, Kaye RE. Pseudobulbar affect: an under-recognized and under-treated neurological disorder. Adv Ther. 2011;28(7):586–601. doi: 10.1007/s12325-011-0031-3. [DOI] [PubMed] [Google Scholar]
- 24.Mosca L, Mochari-Greenberger H, Dolor RJ, Newby LK, Robb KJ. Twelve-year follow-up of American women’s awareness of cardiovascular disease risk and barriers to heart health. Circ Cardiovasc Qual Outcomes. 2010;3(2):120–127. doi: 10.1161/CIRCOUTCOMES.109.915538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kalton G, Flores-Cervantes I. Weighting Measures. J Off Stat. 2003;19(2):81–97. [Google Scholar]
- 26.De Graff AA, D’Hooghe TM, Dunselman GA, Dirksen CD, Hummelshoj L. WERF EndoCost Consortium, Simoens S. The significant effect of endometriosis on physical, mental and social wellbeing: results from an international cross-sectional survey. Hum Reprod. 2013;28(10):2677–2685. doi: 10.1093/humrep/det284. [DOI] [PubMed] [Google Scholar]
- 27.Rao JN, Scott AJ. The analysis of categorical data from complex sample surveys: chi-squared tests for goodness of fit and independence in two-way tables. J Am Stat Assoc. 1981;76(374):221–230. [Google Scholar]
- 28.Peddada SD, Laughlin SK, Miner K, et al. Growth of uterine leiomyomata among premenopausal black and white women. Proc Natl Acad Sci USA. 2008;105(50):19887–19892. doi: 10.1073/pnas.0808188105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wallach EE, Vlahos NF. Uterine myomas: an overview of development, clinical features, and management. Obstet Gynecol. 2004;104(2):393–406. doi: 10.1097/01.AOG.0000136079.62513.39. [DOI] [PubMed] [Google Scholar]
- 30.Fields KR, Neinstein LS. Uterine myomas in adolescents: case reports and a review of the literature. J Pediatr Adolesc Gynecol. 1996;9(4):195–198. doi: 10.1016/s1083-3188(96)70030-x. [DOI] [PubMed] [Google Scholar]
- 31.Andersen J. Growth factors and cytokines in uterine leiomyomas. Semin Reprod Endocrinol. 1996;14(3):269–282. doi: 10.1055/s-2007-1016336. [DOI] [PubMed] [Google Scholar]
- 32.Rein MS, Barbieri RL, Friedman AJ. Progesterone: a critical role in the pathogenesis of uterine myomas. Am J Obstet Gynecol. 1995;172(1 Pt 1):14–18. doi: 10.1016/0002-9378(95)90077-2. [DOI] [PubMed] [Google Scholar]
- 33.Gliklich RE, Leavy MB, Velentgas P, et al. Identification of future research needs in the comparative management of uterine fibroid disease. A report on the priority-setting process, preliminary data analysis, and research plan. Rockville, MD: Agency for Healthcare Research and Quality; 2011. [Accessed September 8, 2016]. (Effective Healthcare Research Report No. 31. AHRQ Publication No. 11-EHC023-EF). Available from: http://effectivehealthcare.ahrq.gov/reports/final.cfm. [Google Scholar]
- 34.Lerner D, Mirza F, Chang H, Renzulli K, Perch K, Chelmow D. Impaired work performance among women with symptomatic uterine fibroids. J Occup Environ Med. 2008;50(10):1149–1157. doi: 10.1097/JOM.0b013e3181895e10. [DOI] [PubMed] [Google Scholar]
- 35.Liu Z, Doan QV, Blumenthal P, Dubois RW. A systematic review evaluating health-related quality of life, work impairment, and healthcare costs and utilization in abnormal uterine bleeding. Value Health. 2007;10(3):183–194. doi: 10.1111/j.1524-4733.2007.00168.x. [DOI] [PubMed] [Google Scholar]