Abstract
Hypertension is the leading remediable risk factor for cardiovascular disease, affecting more than 1 billion people worldwide, and is responsible for more than 10 million preventable deaths globally each year. While hypertension can be successfully diagnosed and treated, only one in seven persons with hypertension have controlled blood pressure. To meet the challenge of improving the control of hypertension, particularly in low‐ and middle‐income countries, the authors developed the Standardized Hypertension Treatment and Prevention Project, which involves a health systems–strengthening approach that advocates for standardized hypertension management using evidence‐based interventions. These interventions include the use of standardized treatment protocols, a core set of medications along with improved procurement mechanisms to increase the availability and affordability of these medications, registries for cohort monitoring and evaluation, patient empowerment, team‐based care (task shifting), and community engagement. With political will and strong partnerships, this approach provides the groundwork to reduce high blood pressure and cardiovascular disease‐related morbidity and mortality.
Noncommunicable diseases (NCDs), primarily cardiovascular disease (CVD), are responsible for approximately two thirds of all deaths worldwide, with 80% occurring in low‐ and middle‐income countries (LIMCs).1 Hypertension is the leading remediable risk factor for CVD.2 It affects more than 1 billion people worldwide3 and is responsible for more than ten million largely preventable deaths globally each year.4
With effective health systems in place, hypertension can be successfully diagnosed and treated with available inexpensive once‐daily regimens.5, 6 Among persons with hypertension, more than 47% are not aware of their condition and among those who are aware, only 35% are on pharmacologic treatment.7 Only one in seven people with hypertension worldwide have their blood pressure (BP) controlled (ie, at a clinical target <140/90 mm Hg).7, 8 The healthcare burden of uncontrolled hypertension is too expensive to ignore. In 2011, the annual global direct healthcare costs attributable to nonoptimal BP control (systolic BP >115 mm Hg) were estimated at US $372 billion, representing about 10% of the world's overall healthcare expenditures. The majority of these costs were attributed to ischemic heart disease and stroke, ranging from 85% to 97%, respectively.9 If BP levels remain unchanged, in 2016 the aggregate healthcare costs over a 10‐year period are estimated to be more than $1 trillion globally.9 A CVD risk–based approach may aid control by identifying persons who would benefit most from treatment, especially in settings with limited resources.10 Effective hypertension control for even half of the patients at medium to high CVD risk could avert 77 million deaths.11
The broad‐scale control of hypertension is challenging yet feasible. A major obstacle to BP control in some areas is the absence of comprehensive primary healthcare services, including limited access to medications,12 and lack of systems to effectively deliver prevention and treatment.13 However, building on lessons learned from the treatment of HIV/AIDS and tuberculosis in LMICs, as well as successful models of hypertension control in the United States and Canada,5, 6, 14, 15, 16, 17 we know that controlling hypertension is attainable using a health system–strengthening approach that involves standardized treatment protocols, effective drug procurement mechanisms using a core set of medications, accountability by tracking progress and control using registries, patient empowerment, team‐based care, and community engagement.18
In recognition of the need to meet the challenge of improving the prevention and control of hypertension in the Americas19 and worldwide, the Centers for Disease Control and Prevention (CDC) and the Pan American Health Organization (PAHO), in collaboration with other stakeholders, have launched the Standardized Hypertension Treatment and Prevention (SHTP) Project.20 The SHTP Project's goal is to improve CVD prevention and management, using hypertension as the entry point, by developing and implementing an approach for standardizing the management of hypertension and strengthening health systems at the primary care level. The SHTP Project design aims to be feasible and flexible for worldwide applicability and can be adapted to improve control of other NCDs.
Rationale for Strengthening Healthcare Delivery Systems for Hypertension Control
Strengthening of health systems can help address challenges to hypertension control by addressing a number of barriers to effective and sustained hypertension control.
Patient Barriers
Patient‐related barriers occur when a patient has limited access to a healthcare system, including medications and/or does not adhere to medical treatment. Limited access to treatment may be caused by multiple factors such as lack of an effective health insurance system, lack of a regular healthcare provider, difficulty in obtaining transportation to medical appointments, or other logistical challenges.21 Patients’ nonadherence to treatment may be related to a complicated medication regimen that is difficult to follow, poor communication between patient and provider, lack of knowledge or understanding about hypertension or the prescribed treatment regimen, lack of social support, cost of medications, and/or medication side effects.22 Many male patients tend to avoid seeking health care and are hard to reach in clinical settings. Differences in healthcare‐seeking behaviors by sex and other factors need to be addressed to improve health outcomes.23 In addition, a patient may experience other challenges, such as obesity, high sodium diet, and socioeconomic issues, which increase susceptibility to hypertension and make long‐term medical control difficult.22
Provider Barriers
Barriers to effective and sustained hypertension control related to the healthcare provider may include belief that a patient's BP tends to be higher when measured at the clinic than when measured at home; reluctance to treat an apparently asymptomatic condition; lack of time with the patient, including a lack of time for patient education; therapeutic inertia or reluctance to treat; and lack of adherence to current treatment guidelines because the healthcare provider is not familiar with the guidelines, does not agree with the guidelines, and/or does not have incentive to use the guidelines.22, 24
Healthcare System Barriers
Multiple barriers to effective healthcare delivery are well recognized, particularly related to process and the need to adapt a system that was established to address infectious diseases for the care of chronic conditions.21 In LIMCs, the capacity and resources to provide care are often limited as the clinical infrastructure is austere and there are limited healthcare workers trained to provide effective care. It is especially challenging to provide care in rural areas.21 If not overcome, they result in inadequate care in general, poor outcomes in management of chronic conditions overall, and failure to achieve successful long‐term control of hypertension in particular.
Barriers to Medication Availability and Affordability
Barriers to the availability and affordability of antihypertensive medications vary from country to country and include policy, legal, institutional, behavioral, and financial factors. Examples of these may include lack of a national pharmaceutical policy, market authorization issues that preclude generic medications of high quality from becoming available, lack of knowledge among healthcare providers about medication costs and price regulations, prescribing habits of healthcare providers who equate low cost with low quality and effectiveness, and lack of authority and incentives among pharmacists to substitute generic drugs for expensive brand name drugs.25 As such, increasing the availability of the selected core medications on a worldwide scale will require attention to multiple factors. Solutions are likely best determined by country or region.
Description of Existing Healthcare Delivery Models
Two healthcare delivery models relevant to treatment for and long‐term control of hypertension are the Chronic Care Model (CCM) and an extension of CCM developed by the World Health Organization (WHO), the Innovative Care for Chronic Conditions Model. CCMs are comprehensive systems for chronic disease care within integrated health service delivery networks. CCMs are patient‐centered, evidence‐ and population‐based systems that were successfully established to improve care for patients with chronic conditions in all countries.26, 27, 28, 29 CCMs emphasize integrating preventive and treatment healthcare services, which can increase the effectiveness of treatment for chronic conditions, decrease the incidence of complications and preventable deaths, and increase the efficiency of primary and specialized care services. CCMs promote patient self‐care and redefine the roles and responsibilities of physicians, nursing staff, and community workers. Setting up a CCM can lead to more comprehensive and sustainable cardiovascular care, strengthen patient self‐care, and improve coordination of care.30 The WHO Innovative Care for Chronic Conditions model has all the elements of a CCM and incorporates the following elements into delivering treatment for NCDs in low‐resource settings: efficient use of limited healthcare resources; sustainable health‐financing mechanisms; access to basic diagnostic tools and essential medicines; organized medical information and referral systems; and long‐term care that is proactive, patient‐centered, community‐based, and sustainable.31 In addition to its Innovative Care for Chronic Conditions Model, WHO lists eight essential actions for improving care for chronic problems such as hypertension.21 CCMs were developed to address healthcare systems barriers to improve chronic illness management.26, 27, 28, 29, 30, 31 While we originally intended to identify care “models” for the effective treatment of hypertension, we concluded that focusing on key care delivery “elements” for hypertension control would be more appropriate because most countries already had invested in large care delivery models.
Key Elements of Healthcare Delivery Systems for Hypertension Control
Standardized hypertension management involves key elements of healthcare delivery system improvement for effective treatment and control of chronic diseases such as hypertension to help overcome the barriers discussed and to ensure successful implementation (Table 1). The rationale for the recommendations are discussed below.
Table 1.
Key Elements of Standardized Hypertension Management to Improve Hypertension Control
| Key Element | Recommendations |
|---|---|
| Guidelines‐based standardized treatment protocols |
Use nationally relevant, evidence‐based, patient‐oriented, clear, simple, and implementable treatment protocols that are endorsed by key stakeholders Integrate certain medication classes into guidelines‐based treatment protocols Consider potential barriers and mechanisms of support in implementation plan |
| Medications | |
| Identify a core set of widely available medications that are safe, high‐quality, and effective | |
| Ensure the quality and safety of the core set of medications | |
|
Implement and/or improve procurement mechanisms to ensure a consistent supply of the core set of medications Ensure adherence to treatment regimens |
|
| Registries for cohort monitoring and evaluation | |
| Develop hypertension registries to collect and store clinical information on all patients within the system with the condition | |
| Allows for the efficient management of “populations” of patients with hypertension within a care system by monitoring targets such as blood pressure control | |
| Data generated from these systems should be used to create indicators, set targets, and assess the impact of changes in the system and care delivery with an eye on improving quality of care | |
|
Use to track the care and outcomes of individual patients and ideally have the capacity to capture information from the community and other related systems such as pharmacies and hospitals Use data to evaluate the efficacy of the program and make adjustments accordingly |
|
| Patient empowerment | |
| Inform patients about their hypertension, involve them in decisions related to their treatment, and ensure they are comfortable expressing their concerns to their healthcare providers | |
| Create a relationship between patient and provider based on mutual respect | |
| Allow the patient to work with the provider to set the hypertension treatment goals, plan how to achieve these goals, and solve problems | |
| Use tools, education, and support systems that improve patients’ knowledge, attitudes, and medication‐taking behaviors such as educational materials and peer support groups | |
| Team‐based care system | |
| Provide patients with hypertension care and support from a multidisciplinary team of healthcare providers in the primary care setting who communicate with each other and coordinate their care delivery (task sharing) | |
| Focus on continuity of care is a high priority | |
| Check and address blood pressure at every visit | |
| Community engagement | |
| Increase awareness of hypertension as a public health priority | |
| Ground key‐related services in the community such as blood pressure checks and use of nontraditional care settings as venues for care advocacy and education as well as linkage to health care for newly diagnosed and complicated cases | |
| Engage community partners such as civil society organizations or representative organizations, technical communities, media, advertising, and other industries |
Guidelines‐Based Standardized Treatment Protocols
Numerous guidelines have been developed for hypertension management.22, 24 Such guidelines should be used to set standards of care for managing patients with high BP, including lifestyle recommendations for physical activity, smoking cessation, reduction of excessive use of alcohol, healthy and lower‐sodium diets, the presence of algorithms that address medication selection, frequency of BP monitoring, and strategies for improving patient medication and recommended lifestyle adherence. Guidelines may also specify decision points for referrals to specialty care or the need for communication with specialists via mobile technologies, telemedicine consultations, or review of medical records.32 To achieve optimal outcomes, guidelines must be actively integrated into clinical practice.25 Organizational context and resource constraints, including the availability and cost of recommended medications, laboratory services, and diagnostic equipment, must be considered in adapting guidelines to local contexts.21 In an evaluation of the Chronic Care Model, high‐performance organizations were more likely to have guidelines‐based decision support and employ other elements such as computerized reminders, registries, and self‐management support compared with lower performing organizations.33, 34 Standardized hypertension management promotes evidence‐based practice and the use of guidelines‐based standardized treatment protocols (Figure 1), which are valuable and effective as part of a multifactorial approach to improve BP control.35
Figure 1.
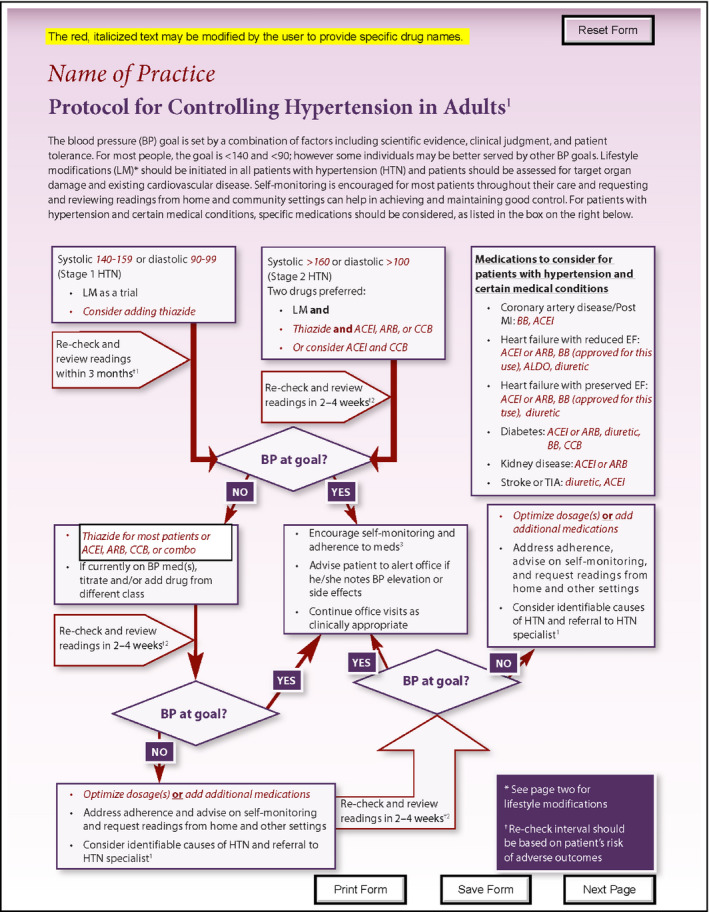
Example of guidelines‐based standardized treatment protocol. Available at: http://millionhearts.hhs.gov/files/Hypertension-Protocol.pdf.
Use of a Core Set of Medications and their Effective Procurement
Simplified Medication Protocol With Standardized Core Medications
Prioritization of the availability and affordability of a core set of quality‐assured drugs to treat hypertension is necessary. The use of a core set of medications for the standardized treatment of hypertension can improve patient access to high‐quality, effective medications that have been produced using safe manufacturing practices. Production of high‐quality core medications in large quantities for distribution throughout a country or region has the potential to greatly increase the availability and affordability of these medications both for the health system and for patients. Furthermore, the selection and adoption of a core set of medications allows for collaborative efforts and improved partnerships between nonprofit organizations, the pharmaceutical industry, healthcare systems, and government agencies to seek widespread high‐quality procurement mechanisms.
Ideal Characteristics of Selected Medications
Many antihypertensive medications are currently available. A group of regional experts that convened in 2013 to identify a core set of medications for use in the Americas identified ideal characteristics of medications to treat persons with hypertension (Table 2).36
Table 2.
Ideal Characteristics of Select Medications
| Characteristic | Priority Consideration |
|---|---|
| Efficacy (from a pharmacologic perspective) and safety | High |
| Evidence‐based clinical and effectiveness outcomes | High |
| Tolerability (few side effects) | High |
| Cost/affordability | High |
| Availability (inclusion on the WHO Model List of Essential Medicinesa , b) | High |
| Appropriate for regional considerations (eg, diversity of the population) | High |
| Once‐a‐day dosage (also including variability in dose) | Medium |
| Scored tablet with variety of doses available | Medium |
This was not an exclusionary criterion.
Hypertension medications included on the World Health Organization (WHO) Model List of Essential Medications: amlodipine, bisoprolol, enalapril, hydralazine, hydrochlorothiazide, methyldopa. Available at: http://www.who.int/medicines/publications/essentialmedicines/en/.
Selecting Medications Compatible With Current Guidelines
For most patients, thiazide diuretics; long‐acting calcium channel blockers (CCBs), particularly of the class of dihydropyridines; angiotensin‐converting enzyme (ACE) inhibitors; or angiotensin II receptor blockers (ARBs) are all recommended first‐line medications for treating hypertension, and were therefore all considered appropriate candidates for inclusion in a recommended set of core medications.37 Other classes of antihypertensive medications were included in the core set because they can be used in combination therapy, as one of a number of BP‐lowering medications combined in a single pill.
When hypertension is not controlled by a single medication alone, three actions are available: increase the dosage of the current medication, add a second from another class of medication, or do both. The next steps should be implemented using guidelines‐based standardized protocols.
Recommended Medications
The proposed set of core medications identified by the SHTP Project for the Americas (Table 3) included one primary and one secondary choice for each of five medication classes (except for CCBs) reflected in current guidelines for hypertension management.22, 24 The secondary choices should be used under circumstances where the primary medication cannot be made broadly available. Single‐pill combinations of medications were also selected, because the combination of medications has additive or synergistic BP‐lowering efficacy, can simplify treatment regimens, may reduce side effects, and can improve adherence. Combination preparations that were considered ideal, although not currently or widely available, were also listed. For most patients without compelling health conditions (those conditions for which a particular class or medication is recommended, eg, diabetes mellitus, heart failure, CVD), thiazide diuretics, long‐acting CCBs, ACE inhibitors, or ARBs are all first‐line medications for treating hypertension, and therefore they were all considered good candidates for inclusion in a recommended set of core medications.22, 24 The proposed set of core medications is intended to be flexible, and can vary by country and clinic setting to include widely accessible medications to ensure consistent availability.
Table 3.
Example of Core Set of Medications
| Medication Classa | Primary | Backup |
|---|---|---|
| Diuretic | Chlorthalidone | HCTZ |
| ACE inhibitor | Lisinopril | Enalapril |
| ARB | Losartan | Valsartan |
| CCB | Amlodipine | None |
| β‐Blocker | Bisoprolol | Metoprolol SR |
| Other | Spironolactone | None |
| Fixed‐dose combinations (single pill)b | ||
| ARB + CCB | Losartan or valsartan + amlodipine | N/A |
| ACE inhibitor + CCB | Benazepril + amlodipine | N/A |
| ACE inhibitor + diuretic | Lisinopril + HCTZ | N/A |
| ARB + diuretic | Losartan + HCTZ | N/A |
| ARB + diuretic + CCB | Valsartan + HCTZ + amlodipine | N/A |
| Ideal fixed‐dose combinations (single pill)c | ||
| ARB + chlorthalidone + CCB | ARB + chlorthalidone + CCB | N/A |
| ACE inhibitor + CCB | Lisinopril + amlodipine | N/A |
| ACE inhibitor + diuretic | Lisinopril + chlorthalidone | N/A |
| ARB + CCB | Losartan + amlodipine | N/A |
| ARB + diuretic | Losartan + chlorthalidone | N/A |
Abbreviations: CCB, calcium channel blocker; HCTZ, hydrochlorothiazide; N/A, not applicable.
For most patients without compelling health conditions (those conditions for which a particular class or medication is recommended, eg, diabetes mellitus, heart failure, cardiovascular disease), thiazide diuretics, long‐acting calcium channel blockers, angiotensin‐converting enzyme (ACE) inhibitors, or angiotensin II receptor blockers (ARBs) are all first‐line medications for treating hypertension, and therefore they were all considered good candidates for inclusion in a recommended set of core medications.
Single‐pill combinations were not stratified into primary and backup choices; all combinations were equally recommended.
Recommended combination medications that, although desirable, are not yet available. Further investigation is needed for these ideal fixed‐dose single‐pill combinations.
Strategies for Increasing Medication Availability and Affordability
Achieving long‐term daily treatment for persons with hypertension worldwide is complex. Factors that can increase availability of medications in a country or region include a national pharmaceutical policy to promote the use of high‐quality generic drugs, sustainable financing, effective procurement systems, availability of qualified providers, coordination across multiple entities, simplified approaches free of administrative complexities, efficient national or regional medication distribution systems, and a regional mechanism to promote the acquisition of high‐quality medicines and essential public health supplies at affordable prices (Figure 2). The PAHO Strategic Fund (www.paho.org\strategicfund) represents a model that ensures access to a set of high‐quality core drugs at competitive prices.36, 38
Figure 2.
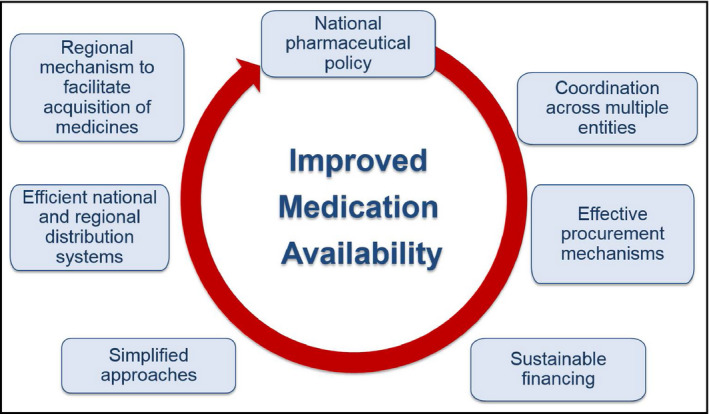
Strategies for improved medication availability and affordability.
Strategies for Medication Adherence
Nonadherence to medication regimens is common and can increase morbidity and mortality related to hypertension. Reducing the number of daily doses should be a first‐line strategy.39 Additionally, fixed‐dose combination pills should be made available as most patients require one or more medications for hypertension control.40
Registries or Clinical Information Systems for Cohort Monitoring and Evaluation
Clinical information systems, also referred to as registries, are important components of effective chronic care models. Specifically, registries of patients with hypertension can be created retrospectively from diagnoses on insurance claims and medical charts, or prospectively as patients visit their primary care provider.32 From a population perspective, registries can be used to monitor how well guidelines are implemented and to track trends in individual and population health outcomes, such as the proportion of patients whose hypertension is controlled.33 Information systems can also be structured to give feedback on performance at the healthcare provider, team, or clinic level. This feedback serves as a benchmark for quality of care.28 Registries can also be used to support clinical decision making41; to allow providers to be proactive rather than reactive,21 for example, by setting up patient reminders about needed services or follow‐up visits32 and to share data throughout a practice, among practices, and potentially throughout an entire healthcare system. Such a system decreases duplication, increases coordination, decreases costs, improves quality of care, and ultimately improves health outcomes.35 Although computer‐based or electronic records would be the ideal approach, if they are not available, registries and feedback systems for monitoring or evaluation can and should be done manually by creating a line‐listing of patients in the cohort.
Significant effects on provider performance were documented by a systematic review of computerized clinical decision supports, including some studies that targeted hypertension‐related care as the performance indicator of interest.42 Outcomes were positive across a range of support types, including diagnostic, disease management, and drug‐dosing or ‐prescribing systems. A more recent review confirmed these positive effects on preventive care services for NCDs, including hypertension, and prescribing behaviors.43 Therefore, the use of hypertension registries to collect and store clinical information on all patients within the system with the condition for cohort monitoring and quality assurance/improvement is beneficial.
Patient Empowerment and Self‐Management Support
Managing chronic diseases such as hypertension successfully requires the patient to be actively informed and engaged. Patient behaviors, including healthy eating and being physically active, adherence to medication regimens, and making and keeping medical appointments play a major role in hypertension control.43, 44, 45 A patient‐centered healthcare system focuses on preventing disease rather than on alleviating or curing symptoms and complications.21 In such a system, the patient‐provider relationship is based on mutual respect.41 This approach to health care requires a multidisciplinary team and culturally appropriate communication.41, 44
Self‐management support is central to empowering the patient. Managing hypertension successfully over the long term requires that patients have the skill, motivation, and confidence to adhere to proper diet and exercise and medication regimens, as well as, in some cases, measure their own BP.45, 46, 47 Self‐management support is no longer based on didactic patient education but has instead shifted to collaboration between patients, their families, and healthcare providers28, 29, 34, 48 Support for self‐management can be offered through primary care settings or through referral to community‐based programs.
Successful standardized hypertension management requires that patient empowerment be made a priority. Patients should be informed about their hypertension, involved in decisions related to their treatment, and comfortable expressing their concerns to their healthcare providers reflecting mutual respect.
Team‐Based Care System
A system for the effective delivery of hypertension treatment should be led and managed in the primary care setting where patients receive most of their health care, including preventive medicine and referral to specialty medicine.44, 45, 48 For patients with hypertension, a focus on continued care is essential. BP should be checked and addressed at every visit,49 and care and support should be provided by a multidisciplinary team according to the individual needs of each patient.21 Treatment coordination can be improved when patients are assigned a “care coordinator” who assumes responsibility for coordination of care across all levels of care.21 Primary care can also link to nontraditional care settings and leverage relationships with community organizations to coordinate systematic screening, messaging, advocacy, and other interventions.
In terms of standardizing the management of hypertension, the effective delivery of hypertension treatment involves providing patients with hypertension care and support from a multidisciplinary team of healthcare providers in the primary care setting who communicate with each other and coordinate their care delivery (task sharing).
Community Engagement
Links between healthcare systems and the community can strengthen programs to prevent, treat, and control hypertension. Existing chronic care models include a community component that calls for increased access to complementary community programs that offer related services (eg, self‐management training and nutrition counseling)36, 37; healthcare providers to partner with nontraditional organizations or businesses, or pharmacies to promote screening for hypertension and offer guidance on self‐management and medication adherence;50 and community healthcare workers to improve hypertension prevention and control by offering, for example, educational services through home visits.51 Such links between the healthcare system and community organizations are cost‐effective alternatives to offering self‐management programs within the primary care setting. Establishing health‐promoting public policies, creating cost‐supportive environments, and strengthening community action have also been suggested.52 Broader community engagement in hypertension control acknowledges the importance of social determinants in disease prevention and self‐management.41
Standardized hypertension management encourages community engagement to increase awareness and to address hypertension as a public health priority, which should be systematically supported by clinical systems.
Strategy for Effective Implementation
To effectively reduce the burden of hypertension within a care delivery system, it is essential to develop and implement a multipronged strategy based on strong political will. This strategy should create an environment where hypertension control is a priority and specific stakeholders, as well as leaders and champions, are identified with clearly defined roles and responsibilities. Involved parties should include patients, clinicians, pharmacists, and social service workers, as well as others to comprise a multidisciplinary team. Concrete targets and goals and an accountability mechanism should be established at all levels with a plan to conduct monitoring and evaluation. Financial resources, including funding sources and procurement mechanisms, should be considered and mobilized. Furthermore, a formative assessment should be conducted prior to implementation to inform the needs for the program's success (Table 4).
Table 4.
Suggested Areas of Focus for Formative Assessment
| Area of focus | |
|---|---|
| Description of hypertension care and control | Basic epidemiology—awareness, treatment, control (national vs subnational) |
| Provider knowledge, attitudes, and behavior | |
Healthcare system coverage
|
|
Healthcare system features
|
|
| Inventory available tools | |
|
Survey data (eg, the World Health Organization's STEPwise approach to Surveillance [WHO STEPS]) Surveillance data Other—specific projects (regional, local, site‐specific) |
|
| Review existing data | |
|
Relevant data elements
|
|
| Collect specific data for review of current practices | |
|
Clinic process
|
|
|
Drug/pharmacy processes
Quality data collection systems
|
|
| Identify and fill in data gaps | |
| Design necessary surveys and studies | |
| Identify barriers | Devise solutions to meet challenges |
Conclusions
This standardized hypertension management approach comes at an unprecedented time of global attention to NCDs. Hypertension is responsible for more deaths than any other single NCD risk factor, and improved control at the population level could have substantial positive impact. The WHO and its global membership recognized this when they created a set of global NCD indicators and targets that included a focus on improved hypertension control. Standardized hypertension management complements population approaches to primary prevention, particularly healthy diet and specifically salt reduction. A dynamic set of related tools and resources are available online (http://www.cdc.gov/globalhealth/ncd/hypertension-toolkit.htm). A technical package is being developed to facilitate widespread implementation and pilots are underway in Malawi and Barbados.
In May 2013, the World Health Assembly, as part of a Global Monitoring Framework, endorsed a set of targets and indicators to be achieved by 2025, including five that the SHTP Project addresses: (1) a 25% reduction in the relative risk of mortality caused by CVDs, cancer, diabetes, and chronic respiratory diseases, (2) a 25% relative reduction of raised BP, (3) at least a 50% rate of eligible people receive drug therapy and counselling (including glycemic control) to prevent heart attacks and strokes, (4) 80% availability of the affordable basic technologies and essential medicines, including generics, required to treat major NCDs in both public and private facilities, and (5) a 30% reduction in salt and sodium intake.53 In addition, this approach, which is inherently flexible, fully supports the primary prevention of CVD and can be expanded to include other chronic diseases. It can be adapted to align with the availability of resources in a specific country and is consistent with and can enhance WHO's essential interventions for primary care.31 Furthermore, this approach is aligned with the World Heart Federation's road map on hypertension and secondary prevention, an initiative that requires collaborative efforts between different institutions for success.54, 55 With political will and strong partnerships, the SHTP Project will facilitate global hypertension control and thus reduce CVD‐related morbidity and mortality worldwide.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the US Centers for Disease Control and Prevention and the Pan American Health Organization.
Acknowledgements
The Standardized Hypertension Treatment and Prevention Network: Alma Adler, World Heart Federation; Sonia Y. Angell, New York City Department of Health and Mental Hygiene; Samira Asma, CDC; Michele Bashin, Public Health Institute; Rafael Bengoa, Minister of Health, Basque Region; Ana Isabel Barrientos Castro, Sociedad Interamericana de Cardiología and Sociedad Centroamericana de Cardiología; Barbara Bowman, CDC; Francis Burnett, Organization of Eastern Caribbean States; Jose Castro, PAHO; Norman Campbell, World Hypertension League; Beatriz Marcet Champagne, InterAmerican Heart Foundation; Kenneth Connell, University of West Indies; Jose De Gracia, Martin Didier, Caribbean Cardiac Society; Donald DiPette, University of South Carolina; Maria Cristina Escobar, Chile Ministry of Health; Daniel Ferrante, Argentina Ministry of Health; Thomas Gaziano, Harvard School of Public Health; Marino Gonzalez, Universidad Simon Bolivar; Sir Trevor Hassell, Health Caribbean Coalition; Anselm Hennis, PAHO; Rafael Hernandez, Universidad Centroccidental Lisandro Alvarado, Venezuela; Maryam Hinds, Barbados Drug Service; Marc Jaffe, Kaiser Permenante; Fernando Lanas, Universidad de La Frontera, Chile; Patricio Lopez‐Jaramillo, Latin American Society of Hypertension; Fleetwood Loustalot, CDC; Ben Lumley, Public Health England; Javier Maldonado, Colombia Ministry of Health; Thelma Nelson, National Health Fund; Jose Miguel do Nascimento Junior, Brazil Ministry of Health; Pedro Ordunez, PAHO; Marcelo Orias, Latin American Society of Nephrology and Hypertension; Jose Ortellado, Latin American Society of Internal Medicine; Pragna Patel, CDC; Jacqueline Poselli, Venezuela Foro Farmaceutico de Las Américas; Agustin Ramirez, International Society of Hypertension; Lynn Silver, Public Health Institute; Donald Simeon, Caribbean Cardiac Society; Valerie Steinmetz, Public Health Institute; Kathryn Taubert; Honorable Alvina Reynolds, St. Lucia Ministry of Health; Hilary Wall, CDC; Jamie Waterall, Public Health England; Fernando Wyss, Interamerican Society of Cardiology; Amy Valderrama, CDC; Jose Fernando Valderrama, Colombia Ministry of Health; and Fernando Lanas Zanetti, Interamerican Society of Cardiology.
J Clin Hypertens (Greenwich). 2016;18:1284–1294. DOI: 10.1111/jch.12861. © 2016 Wiley Periodicals, Inc.
References
- 1. WHO . Global status report on noncommunicable diseases 2014. Geneva: World Health Organization, 2015. [DOI] [PubMed] [Google Scholar]
- 2. WHO . Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization, 2009. [Google Scholar]
- 3. Causes of Death 2008: data sources and methods . Geneva; World Health Organization; http://www.who.int/healthinfo/global-burden-disease/cod-2008-sources-methods.pdf. Accessed September 10, 2013. [Google Scholar]
- 4. GBD 2013 Risk Factors Collaborators . Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks and clusters of risks in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015; 386: 2287–2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jaffe MG, Lee GA, Young JD, et al. Improved blood pressure control associated with a large‐scale hypertension program. JAMA. 2013;310:699–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McAlister FA, Wilkins K, Joffres M, et al. Changes in the rates of awareness, treatment and control of hypertension in Canada over the past two decades. CMAJ. 2011;183:1007–1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pereira M, Lunet N, Azavedo A, Barros H. Differences in prevalence, awareness, treatment and control of hypertension between developing and developed countries. J Hypertens. 2009;27:963–975. [DOI] [PubMed] [Google Scholar]
- 8. Chow CK, Teo KK, Rangarajan S, et al; and the PURE (Prospective Urban Rural Epidemiology) Study investigators . Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high‐, middle‐, and low‐income countries. JAMA. 2013; 310: 959–968. [DOI] [PubMed] [Google Scholar]
- 9. Gaziano TA, Bitton A, Weinstein AS, for the International Society of Hypertension. The global cost of nonoptimal blood pressure. J Hypertens. 2009;27:1472–1477. [DOI] [PubMed] [Google Scholar]
- 10. Jackson R, Lawes CMM, Bennett DA, et al. Treatment with drugs to lower blood pressure and blood cholesterol based on an individual's absolute cardiovascular risk. Lancet. 2005;365:434–441. [DOI] [PubMed] [Google Scholar]
- 11. Nugent R. Benefits and Costs of the Noncommunicable Disease Targets for the Post‐2015 Development Agenda. Copenhagen Consensus Center. Perspective Paper. 2015.
- 12. MacMahon S, Alderman MH, Lindholm LH, et al. Blood‐pressure‐related disease is a global health priority. Lancet. 2008;371:1480–1482. [DOI] [PubMed] [Google Scholar]
- 13. Ikeda N, Sapienza D, Guerrero R, et al. Control of hypertension with medication: a comparative analysis of national surveys in 20 countries. Bull World Health Organ. 2014;92:10–19C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Allain TJ, van Oosterhout JJ, Douglas GP, et al. Applying lessons learnt for ‘DOTS’ Tuberculosis Model to monitoring and evaluating persons with diabetes mellitus in Blantyre, Malawi. Tropical Med Int Health. 2011;16:1077–1084. [DOI] [PubMed] [Google Scholar]
- 15. Harries AD, Zachariah R, Jahn A, et al. Scaling up antiretroviral therapy in Malawi – implications for managing other chronic diseases in resource‐limited countries. J Acquired Immune Deficiency Syndrome. 2009;52:S14–S16. [DOI] [PubMed] [Google Scholar]
- 16. Mullins J. Cohort reporting improves hypertension care for refugees. Lancet. 2012;380:552. [DOI] [PubMed] [Google Scholar]
- 17. Seita A, Harries AD. All we need to know if public health we can learn from tuberculosis care: lessons for non‐communicable disease. Int J Tuberculosis Lung Dis. 2013;17:429–430. [DOI] [PubMed] [Google Scholar]
- 18. Angell SY, DeCock KM, Frieden TR. A public health approach to global management of hypertension. Lancet. 2015;385:825–827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ordunez P, Martines R, Niebylski ML, Campbell NR. Hypertension prevention and control in Latin America and the Caribbean. J Clin Hypertens (Greenwich). 2015;17:499–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Patel P, DiPette DJ. Hypertension‐related congestive heart failure in West Africa: a framework for global blood pressure control. J Clin Hypertens (Greenwich). 2015;17:260–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. WHO . Innovative care for chronic conditions: building blocks for action: global report. Geneva, Switzerland: World Health Organization; 2002. Available at: http://www.who.int/chp/knowledge/publications/icccglobalreport.pdf. Accessed April 1, 2015. [Google Scholar]
- 22. Chobanian AV, Bakris GL, Black HR, Cushman WC. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 Report. JAMA. 2003;289:2560. [DOI] [PubMed] [Google Scholar]
- 23. Thompson AE, Anisimowicz Y, Miedema B, et al. The influence of gender and other patient characteristics on health care‐seeking behaviour: a QUALICOPC study. BMC Family Practice. 2016;17:38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community. A statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich). 2014;32:3–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kaplan WA, Ritz LS, Vitello M, Wirtz VJ. Policies to promote use of generic medicines in low and middle income countries: a review of published literature, 2000–2010. Health Policy. 2012;106:211–224. [DOI] [PubMed] [Google Scholar]
- 26. Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Effective Clinical Practice. 1998;1:2–4. [PubMed] [Google Scholar]
- 27. Ham C. The ten characteristics of the high‐performing chronic care system. Health Economics, Policy Law. 2010;5:71–90. doi: 10.1017/S1744133109990120. [DOI] [PubMed] [Google Scholar]
- 28. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288:1775–1779. [DOI] [PubMed] [Google Scholar]
- 29. Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self‐management of chronic disease in primary care. JAMA. 2002;288:2469–2475. [DOI] [PubMed] [Google Scholar]
- 30. Barcelo A, Luciani S, Agurto I, et al. Improving chronic illness care through integrated health service delivery networks. Editors. Washington, DC: Pan American Health Organization; 2012. Available at: http://new.paho.org/hq/index.php?option=com-docman&task=-doc-view&gid=17652&Itemid==. [Google Scholar]
- 31. WHO . Package of Essential Noncommunicable (PEN) Disease Interventions for Primary Health Care in Low‐Resource Settings. Geneva: World Health Organization, 2010. [Google Scholar]
- 32. Wagner E, Austin B, Davis C, et al. Improving chronic illness care: translating evidence into action. Health Aff. 2001;20:64–78. [DOI] [PubMed] [Google Scholar]
- 33. Parchman ML, Zeber JE, Romero RR, Pugh JA. Risk of coronary artery disease in type 2 diabetes and the delivery of care consistent with the chronic care model in primary care settings: a STARNet study. Med Care. 2007;45:1129–1134. [DOI] [PubMed] [Google Scholar]
- 34. Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the Chronic Care Model in the new millennium. Health Aff. 2009;28:75–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Go AS, Bauman MA, Coleman King SM, et al; American Heart Association; American College of Cardiology; Centers for Disease Control and Prevention . An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension. 2014; 63:878–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. CDC . Global Standardized Hypertension Treatment Project: identification of a core set of medications & care delivery models for the medical treatment of hypertension. Atlanta: Centers for Disease Control and Prevention, 2013. http://www.cdc.gov/globalhealth/ncd/pdf/GSHTPp-march2013.pdf. Accessed May 1, 2015. [Google Scholar]
- 37. U.S. Department of Health and Human Services, National Institutes of Health . The seventh report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure. Washington, DC: Government Printing Office; 2003. NIH Publication No. 03‐5233.29. [Google Scholar]
- 38. Ordunez P, Luciani S, Barojas A, et al. A public health approach to hypertension. Lancet. 2015;385:1833. [DOI] [PubMed] [Google Scholar]
- 39. Schroeder K, Fahey T, Ebrahim S. Interventions for improving adherence to treatment in patients with high blood pressure in ambulatory setting. Cochrane Database Syst Rev. 2004;(2):CD004804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Frank J. Managing hypertension using combination therapy. Am Fam Physician. 2008;77:1279–1286. [PubMed] [Google Scholar]
- 41. Pan American Health Organization (PAHO) . Improving Chronic Illness Care through Integrated Health Service Delivery Networks. Washington DC: PAHO; 2012. Available at: http://new.paho.org/hq/index.php?option=com-docman&task=-doc-view&gid=17652&Itemid==. Accessed April 1, 2015. [Google Scholar]
- 42. Garg A, Adhikari N, McDonald H, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA. 2005;293:1223–1238. [DOI] [PubMed] [Google Scholar]
- 43. Bright TJ, Wong A, Dhurjati R, et al. Effect of clinical decision‐support systems: a systematic review. Ann Inter Med. 2012;157:29–43. [DOI] [PubMed] [Google Scholar]
- 44. Rittenhouse D, Shortell S. The patient‐centered medical home. Will it stand the test of health reform? [Commentary]. JAMA. 2009;301:2038–2040. [DOI] [PubMed] [Google Scholar]
- 45. Institute of Medicine . Promoting cardiovascular health in the developing world: a critical challenge to achieve global health. Washington, DC: The National Academies Press; 2010. [PubMed] [Google Scholar]
- 46. Arnett DK, Goodman RA, Halperin JL, et al. AHA/ACC/HHS/ Strategies to enhance application of clinical practice guidelines in patients with cardiovascular disease and comorbid conditions. Circulation. 2014;130:1662–1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Centers for Disease Control and Prevention (CDC) . Self‐Measured Blood Pressure Monitoring: Actions Steps for Public Health Practitioners. Atlanta, Georgia: CDC; 2013. [Google Scholar]
- 48. Lorig K, Sobel D, Ritter P, et al. Effect of a self‐management program on patients with chronic diseases. Effective Clin Practice. 2001;4:256–262. [PubMed] [Google Scholar]
- 49. CDC . Vital signs: awareness and treatment of uncontrolled hypertension among adults—United States, 2003–2010. MMWR. 2012;61:703–709. [PubMed] [Google Scholar]
- 50. Sookaneknun P, Saramunee K, Rattarom R, et al. Economic analysis of the diabetes and hypertension screening collaboration between community pharmacies and a Thai government primary care unit. Primary Care Diabetes. 2010;4:155–164. [DOI] [PubMed] [Google Scholar]
- 51. Jafar HT, Hatcher J, Poulter N, et al. Community‐based interventions to promote blood pressure control in a developing country. Ann Intern Med. 2009;151:593–601. [DOI] [PubMed] [Google Scholar]
- 52. Barr V, Robinson S, Marin‐Link B, et al. The expanded Chronic Care Model: an integration of concerns and strategies from population health promotion and the Chronic Care Model. Hospital Quarterly. 2003;71:73–78. [DOI] [PubMed] [Google Scholar]
- 53. WHO . Global action plan for the prevention and control of noncommunicable diseases 2013–2020. Geneva: World Health Organization, 2013. [Google Scholar]
- 54. Adler AJ, Prabhakaran D, Bovet P, et al. Reducing cardiovascular mortality through prevention and management of raised blood pressure: a World Heart Federation roadmap. Glob Heart. 2015;10:111–122. [DOI] [PubMed] [Google Scholar]
- 55. Perel P, Avezum A, Huffman M, et al. Reducing premature cardiovascular morbidity and mortality in people with atherosclerotic vascular disease: the World Heart Federation roadmap for secondary prevention of cardiovascular disease. Glob Heart. 2015;10:99–110. [DOI] [PubMed] [Google Scholar]


