Abstract
Background
Bleeding is the most common major complication following colonoscopic polypectomy. The purpose of this study is to evaluate whether submucosal epinephrine injections could prevent the occurrence of postpolypectomy bleeding.
Method
The dataset was defined by searching PubMed, EMBASE, Google Scholar, and the Cochrane database for appropriate randomized controlled studies published before April 2015. A meta-analysis was conducted to investigate the preventative effect of submucosal epinephrine injection for overall, early, and delayed postpolypectomy bleeding.
Results
The final analysis examined the findings of six studies, with data from 1388 patients. The results demonstrated that prophylactic treatment with epinephrine injection significantly reduced the occurrence of overall (OR = 0.38, 95% CI: 0.21, 0.66; p = 0.0006) and early bleeding (OR = 0.38, 95% CI: 0.20, 0.69; p = 0.002). However, for delayed bleeding complications, epinephrine injections were not found to be any more effective than treatment with saline injection or no injection (OR = 0.45, 95% CI: 0.11, 1.81; p = 0.26). Moreover, for patients with polyps larger than 20 mm, mechanical hemostasis devices (endoloops or clips) were found to be more effective than epinephrine injection in preventing overall bleeding (OR = 0.33, 95% CI: 0.13, 0.87; p = 0.03) and early bleeding (OR = 0.29, 95% CI: 0.08, 1.02; p = 0.05). This was not established for delayed bleeding.
Conclusion
The routine use of prophylaxis submucosal epinephrine injection is safe and beneficial preventing postpolypectomy bleeding.
Keywords: Colonic polyp, Colonoscopic polypectomy, Bleeding, Epinephrine, Meta-analysis
1. Introduction
Colonoscopic polypectomy is an effective technique that has been shown to reduce the incidence of colorectal cancer by 76–90% [1]. While colonoscopic polypectomy is a relatively safe procedure, it has nevertheless been associated with a number of complications, including bleeding, perforation, and postpolypectomy syndrome [2]. Postpolypectomy bleeding is the most common major complication following a colonoscopic polypectomy procedure, with an incidence rate ranging from 0.3 to 6.1% [3].
Precipitating risk factors for postpolypectomy bleeding in patients include old age (>65 years), comorbid diseases (cardiovascular disease, chronic renal disease, and hypertension), anticoagulant use, large polyp size (>10 mm), sessile polyps, pedunculated polyps with a stalk size > 5 mm, polyps located on the right side of the colon, malignant polyps, use of cutting mode in treatment and use of low-volume endoscopists in treatment [4], [5], [6], [7].
Various endoscopic techniques have been developed to prevent postpolypectomy bleeding; these include the administration of a submucosal injection with an epinephrine solution (1:10000) in the base of any polyps, argon plasma coagulation, or mechanical hemostasis (using a detachable snare and/or endoscopic clip) [8], [9], [10]. The hemostatic effect of epinephrine has been widely demonstrated and it is often used to prevent bleeding following colonic polypectomy and enhancing complete resection, especially in large sessile polyps [11], [12].
Although there is evidence from several studies that submucosal epinephrine injections may reduce the risk of postpolypectomy bleeding, the findings of these studies vary. The purpose of this meta-analysis was to analyze whether the routine administration of a submucosal epinephrine injection was effective in preventing the complications, by assessing the occurrence of overall, early, and delayed postpolypectommy bleeding for those who were treated with a prophylactic submucosal epinephrine injection and treated only with saline injections or with no injections at all (control group). We also compared the bleeding outcomes, of patients treated with prophylactic submucosal epinephrine injections with those treated with other mechanical hemostatic methods (mechanical group).
2. Method
2.1. Data sources and search strategies
An electronic search of PubMed, EMBASE, Google Scholar and the Cochrane database was undertaken. The search term “epinephrine injection,” “colonic polyp,” “prevention,” and “postpolypectomy bleeding” were used as keywords to identify all studies published in English before May 2017, that compared either (1) the postpolypectomy outcomes of patients treated with epinephrine injection with those treated with saline injections/no-injections or (2) studies that compared the postpolypectomy outcomes of patients treated with epinephrine injections with those treated with mechanical hemostatic methods.
2.2. Study selection and eligibility criteria
For inclusion in the meta-analysis, all studies had to (1) examine the effectiveness of colonic polypectomy in patients with colonic polyps, (2) use a randomized controlled study design to undertake the assessment, (3) compare the use of submucosal epinephrine injection prophylaxis by comparing a group of patients who had been treated with this method (epinephrine group) with a control group (either patients treated with non-injection/saline injection) or mechanical hemostasis method (mechanical group), (4) examine overall, early, and delayed postpolypectomy bleeding complication.
The following study types were excluded if: (1) non-randomized and non-comparative studies, (2) case reports, (3) letters to the editor, and (4) review articles. Articles that were only available in abstract form were also excluded. The meta-analysis was performed according to the guidelines of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2009 [13].
2.3. Definitions
Prophylaxis submucosal epinephrine injection prophylaxis treatment was defined as the administration of an injection of a 1: 10000 epinephrine solution into the base of a polyp or stalk to create tissue elevation sufficient to perform a polypectomy. Mechanical hemostasis treatment was defined as the use of either a detachable snare (endoloop) placed at the base of the stalk before polypectomy or an endoscopic clip placed at the residual stalk or the closure of the mucosal defect after polypectomy. Postpolypectomy bleeding was defined either as (1) early: occurring either during an endoscopic procedure or immediately after as hematochezia within 24 h or (2) delayed: any bleeding event that occurring between 24 h and 30 days following the polypectomy procedure.
2.4. Statistical analysis
The meta-analysis was performed using Review Manager Software (Revman version 5.2.6) provided by the Cochrane Collaboration (Nordic Cochrane Center, Cochrane Collaboration, Copenhagen, Denmark). Cochran's chi-square-based Q-statistic test was applied to assess between-study heterogeneity. I2 was generated to assess the percentage of variance in the meta-analysis attributable to heterogeneity between the included studies.
The pooled OR was calculated using the Mantel-Haenszel method, where ORs for outcomes of interest are combined. Dichotomous variables were analyzed by assessing the odds ratio (OR) of the postpolypectomy bleeding rate occurring in the epinephrine group compared to the control group or the mechanical group along with 95% confidence intervals (CIs). An OR that does not involve 1 when combined with the point estimate of the OR at the P < 0.05 level if the 95% CI did not include the value of 1 was considered to be statistically significant.
A random-effects model was used for analysis of the pool data which is a more conservative way to assume a high level of variation between studies and uses a weighted average of the effects reported in different studies to calculate levels of association. The risk of publication bias may have observed in the meta-analysis as we only selected randomized controlled studies, published in English in order to assess the pooled data. Thus, the evidence of publication bias was assessed by Egger's linear regression test and the rank correlation test (Begg's test) using the WINPEPI statistical software (Brixton Health).
3. Results
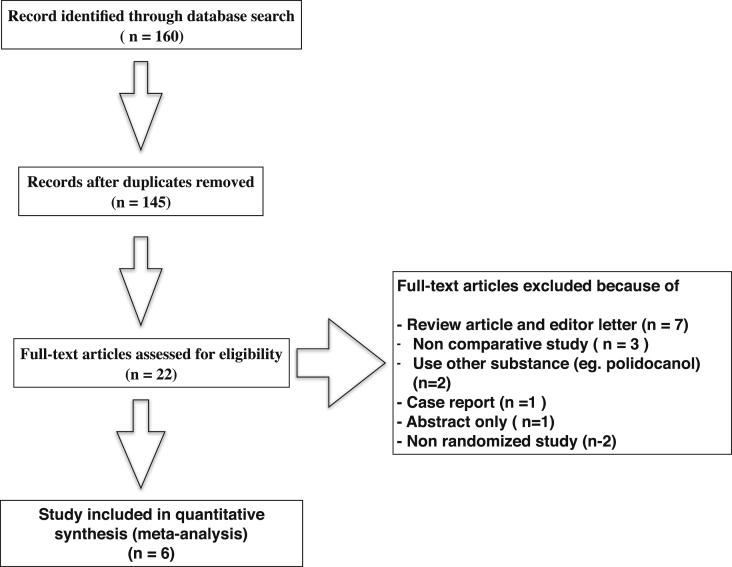
The initial search identified a total of 160 potential articles. After screening, six articles were deemed suitable for inclusion in the meta-analysis. An illustration of the search process is given in Fig. 1. The Modified Jadad scoring of the studies revealed moderate to good quality. Reviews of data extraction showed 100% agreement between the two reviewers. The pooled studies included data on 1523 polypectomy procedures in 1388 patients. Studies that included the patients with bleeding tendencies, abnormal coagulograms, or those undergoing anticoagulant therapy were excluded. An overview of the characteristics of the six studies [14], [15], [16], [17], [18], [19] is given in Table 1.
Fig. 1.
Study selection process.
Table 1.
Study characteristics.
| Study | Country | Year of publication | Population | Number of patient | Number of polyp | Mean age (year) | Male sex | Size of polyp (Mean) | Type of polyp | Location of polyp | Comparision | Concentration of epinephrine solution | Polypectomy method | Outcome variable | Pathology | Post polypectomy bleeding (%) | Anticoaulant used or coagulopathy | Blood tranfusion | Modified Jadad score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lee SH. | South korea | 2007 | Multicenter | 486 | 561 | Epinephrine group: 51.6 ± 11.4, Controlled group: 56.8 ± 11.3 | 379 | Epinephrine group: 14.5 ± 5.7 mm, Controlled group:15.0 ± 6.8 mm. | Pedunculated: 128 Semipeduncul ated: 200 Sessile: 150 Superficial elevated type: 83 | Right colon (include transverse colon):99 Left colon:257 Both: 130 | Epinephrine versus Controlled (normal saline solution) | 0.01% (Total volume 2–25 ml) | Bipolar cauterization, blended current (30–40 Watts) | -Early bleeding (within 12 h) - Late bleeding (12 h.-30 days) | Nonneoplastic: 51 Dysplasia:362 High grade Dysplasia:95 Cancer: 53 | 8% | Excluded | – | 9 |
| Hsieh Yh. | Taiwan | 2001 | Single center | 122 | 151 | Epinephrine group 62.9 (59.8–62.1), Controlled group: 64.9 (62.1–67.8) | 80 | Epinephrine group: 8 (8–13) mm., Controlled group: 8 (8–11) mm. | Sessile | Ascending: 10 Transverse: 4 Descending:7 Sigmoid: 50 Rectum 16 | Epinephrine versus Controlled | 0.01% (Total volume 2–10 ml) | Coagulation current (25–30 Watts) | -Early bleeding (within 24 h) -Late bleeding (>24 h.-30 days) -Perforation -Mortality | Nonneoplastic: 12 Tubular: 59 Tubulovillus:13 Villus: 2 Carcinoid: 2 | 6.0% | Excluded | 2 | 6 |
| Dobrowolski S. | Poland | 2004 | Single center | 69 | 100 | 64.6 ± 10.5 | 44 | Epinephrine group: 16.3 ± 5.4 mm, Controlled group:16.1 ± 5.9 mm. | Pedunculated: 80 Sessile: 20 | Ascending: 6 Transverse: 10 Descending: 13 Sigmoid: 51 Rectum 20 | Epinephrine versus Controlled | 0.01% (Total volume 2–10 ml) | Endocut, effect 3 (output limit 120 W) and Soft coagulation (output limit 60 W) | -Early bleeding (within 24 h) -Late bleeding (>24 h.-30 days) | Nonneoplastic: 6 Tubular: 23 Tubulovillus:51 Adenocarcinim a: 20 | 9% | Excluded | 2 | 7 |
| Paspatis GA. | Greece | 2006 | Multicenter | 159 | 159 | Epinephrine group: 64.5 ± 11, Epinephrine + snare group: 61.7 ± 13.8 | 84 | Epinephrine group: 26.3 ± 8.1 mm, Epinephrine + snare group: 27.1 ± 8.9 mm. | Pedunculated | Right colon: 13 Left colon:130 Rectum: 16 | Epinephrine versus Epinephrine and Detachable snare | 0.01% (Total volume 2–3 ml) | Endocut mode (72 W) | -Early bleeding (within 24 h) -Late bleeding (>24 h.-30 days) - Blood transfusion - Operation need | – | 6% | Excluded | 1 | 7 |
| Kouklakis G. | Greece | 2009 | Single center | 64 | 64 | Epinephrine group: 58.8 ± 11.2, Endoloop + clip group: 57.9 ± 9.7 | 35 | Epinephrine group: 2.7 ± 1.1 cm. Endoloop + clip group: 2.56 ± 1.2 cm. | Pedunculated | Ascending: 3 Transverse: 4 Descending:8 Sigmoid: 35 Rectum 14 | Epinephrine versus Endoloop and hemoclip | 0.01% (Total volume 2–5 ml) | Monopolar coagulation in endocut function (72 W) | -Early bleeding (within 24 h) -Late bleeding (>24 h.-30 days) - Blood transfusion | Neoplastic:5 Severe dysplasis: 13 Mild-moderate dysplasia:46 | 8% | Excluded | 3 | 8 |
| Di Giorgio P. | Italy | 2004 | Single center | 488 | 488 | Epinephrine group: 63 ± 8.9, Controlled group: 62 ± 9.0, Snare group: 64 ± 9.2 | 267 | Epinephrine group: 24.72 ± 5.31 mm, Controlled group: 21.55 ± 4.77 mm, Snare group: 22.15 ± 5.92 mm. | Pedunculated | Right colon: 88 Left colon: 125 Rectosigmoid: 275 | Epinephrine versus Controlled versus Detachtable snare | 0.01% (Total volume 2 ml) | Bipolar cauterization, blended current (75 Watts) | -Early bleeding (within 24 h) -Late bleeding (>24 h.-30 days) | – | 4% | Excluded | – | 7 |
3.1. Prophylactic submucosal epinephrine injection versus saline injection or no injection
Four suitable studies with a total of 1062 patients were identified to examine the efficacy of treatment with submucosal epinephrine injection versus treatment with saline injection or no injection [14], [15], [16], [17]. All four studies compared the rate of postpolypectomy bleeding in patients with a polyp size larger than 10 mm.
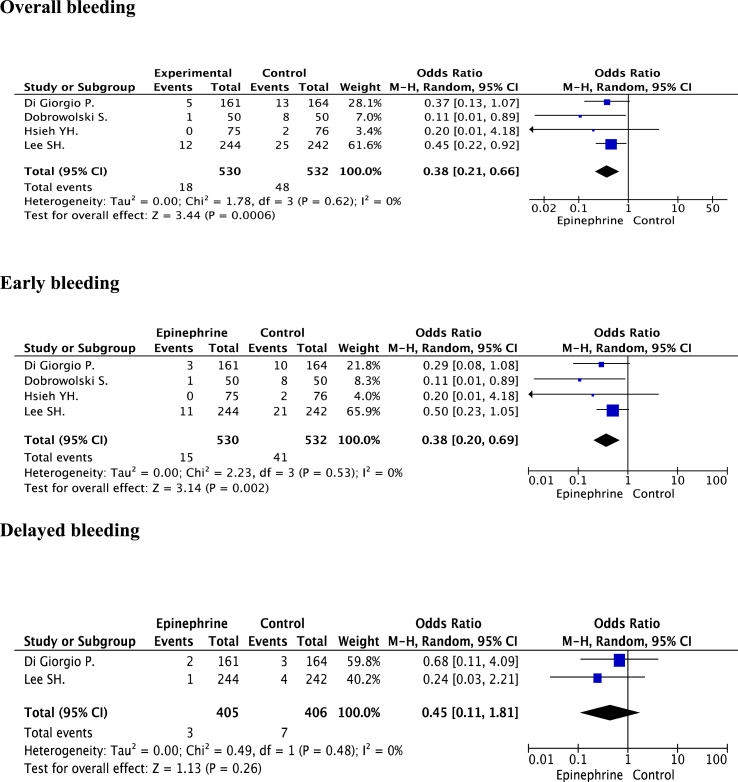
3.1.1. Overall bleeding complication
The analysis of the relevant studies [14], [15], [16], [17] found that the average rate of overall postpolypectomy bleeding complication was 6.2% (66/1062). The rate of overall postpolypectomy bleeding complication in the epinephrine group was 3.4% (% (18/530) and 9.0% (48/532) in the saline/no injection group. A pooled analysis of the ORs of these four studies indicated that prophylaxis with submucosal epinephrine injection significantly reduced the rate of overall bleeding (OR = 0.38, 95% CI: 0.21, 0.66; p = 0.0006). No evidence of heterogeneity was identified among the studies (P = 0.62, I2 = 0%). The poll analysis represented an absolute risk difference of 0.25 and number need to treat of 4. There was no evidence of publication bias observed by either Egger’s test (P = 0.108) or the rank correlation test (P = 0.174).
3.1.2. Early bleeding complication
The analysis of the relevant studies [14], [15], [16], [17] found that early postpolypectomy bleeding occurred in 2.8% of patients in the epinephrine group (15/530) and 7.7% of patients in the saline/no injection group (41/532). The polled ORs demonstrated that there was a significant reduction in the rate of early bleeding among those in the epinephrine group (OR = 0.38, 95% CI: 0.20, 0.69; p = 0.002). No significant heterogeneity between the studies was identified (P = 0.53, I2 = 0%). The poll analysis represented an absolute risk difference was 0.5 and number need to treat of 20. The evidence of publication was not observed by either Egger's test (P = 0.105) or the rank correlation test (P = 0.497).
3.1.3. Delayed bleeding complication
The analysis of the relevant studies [14], [17] demonstrated that delayed bleeding occurred in 0.7% of the epinephrine group (3/405) and 1.7% of the control group (7/406). No significant heterogeneity was identified between the studies (P = 0.48, I2 = 0%). The pooled analysis of the ORs indicated that prophylaxis submucosal epinephrine injection treatment did not reduce the risk of delayed postpolypectomy bleeding significantly (OR = 0.45, 95% CI: 0.11, 1.81; p = 0.26). The poll analysis represented an absolute risk difference was 0.01 and number need to treat of 100. The evidence of publication was not observed by either Egger's test (P = 0.247) or the rank correlation test (P = 0.467). Forest plots illustrating the rates of postpolypectomy bleeding in both the epinephrine and control group are given in Fig. 2.
Fig. 2.
Comparison of postpolypectomy bleeding in the epinephrine and control group.
3.2. Prophylactic submucosal epinephrine injection versus mechanical hemostasis
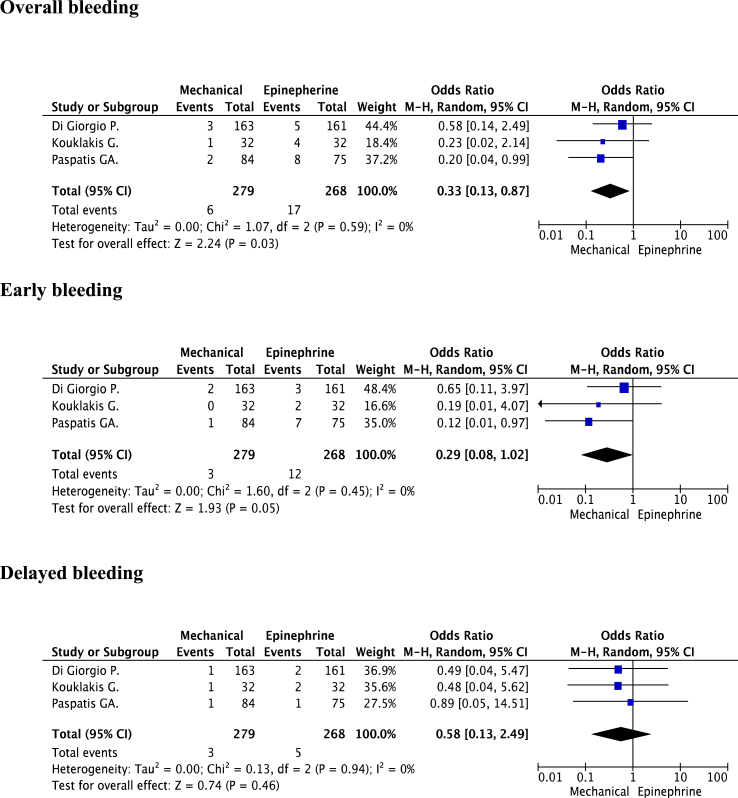
Three studies with a total of 565 patients were identified [17], [18], [19] that compared the rate of postpolypectomy bleeding between the patients being treated with epinephrine injection and those receiving mechanical hemostasis (such as treatment with an endoloop or clip). All three studies compared the rate of postpolypectomy bleeding in the patients with large pedunculated polyp (polyps larger than 20 mm).
3.2.1. Overall bleeding complication
The average rate of overall postpolypectomy bleeding complication was 4.1% (23/565). The rate of overall postpolypectomy bleeding complication in the epinephrine group was 6.3% (17/268) and 2.2% (6/279) in the mechanical group. A pooled analysis of the ORs of these four studies indicated that treatment with mechanical hemostasis significantly reduced the rate of overall bleeding (OR = 0.33, 95% CI: 0.13, 0.87; p = 0.03). No evidence of heterogeneity was identified among the studies (P = 0.59, I2 = 0%). The poll analysis represented an absolute risk difference was 0.04 and number need to treat of 25. The evidence of publication bias was not observed by either Egger's test (P = 0.634) or the rank correlation test (P = 0.602).
3.2.2. Early bleeding complication
The early postpolypectomy bleeding occurred in 4.5% of patients in the epinephrine group (12/268) and 1.1% of patients in the mechanical group (3/279). The polled ORs demonstrated that there was a significant reduction in the rate of early bleeding among those in the mechanical group (OR = 0.29, 95% CI: 0.08, 1.02; p = 0.05) without a significant heterogeneity between the studies (P = 0.45, I2 = 0%). The poll analysis represented an absolute risk difference was 0.03 and number need to treat of 33. The evidence of publication bias was not observed by either Egger's test (P = 0.491) or the rank correlation test (P = 0.602).
3.2.3. Delayed bleeding complication
The delayed postpolypectomy bleeding occurred in the epinephrine group was 1.9% and 1.1% in the mechanical group respectively. This treatment was not found to significantly affect the rate of delayed postpolypectomy bleeding (OR = 0.58, 95% CI: 0.13, 2.49; p = 0.46) without a significant heterogeneity between the studies (P = 0.94, I2 = 0%). The poll analysis represented an absolute risk difference was 0.01 and number need to treat of 100. The evidence of publication bias was not observed by either Egger's test (P = 0.403) or the rank correlation test (P = 0.602). Forest plots illustrating the rates of postpolypectomy bleeding in both the epinephrine and mechanical hemostasis group are shown in Fig. 3 and the summarized results of the meta-analysis was illustrated in Table 2.
Fig. 3.
Comparison of postpolypectomy bleeding in the mechanical and epinephrine group.
Table 2.
Summarized of the results of the meta-analysis.
| Comparison | No. of studies | n | OR | 95% CI | p-value | Heterogeneity |
Eager's test | Rank correlation test | Absolute risk differences | Number need to treat | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| I2 | P | ||||||||||
| Control vs. Epinephrine group | |||||||||||
| Overall postpolypectomy bleeding | 4 | 1062 | 0.38 | 0.21–0.66 | 0.0006a | 0% | 0.62 | 0.108 | 0.174 | 0.25 | 4 |
| Early postplypectomy bleeding | 4 | 1062 | 0.38 | 0.20–0.69 | 0.002a | 0% | 0.53 | 0.105 | 0.497 | 0.05 | 20 |
| Delayed postpolypectomy bleeding | 2 | 811 | 0.45 | 0.11–1.81 | 0.26 | 0% | 0.26 | 0.247 | 0.467 | 0.01 | 100 |
| Mechanical vs. Epinephrine group | |||||||||||
| Overall postpolypectomy bleeding | 3 | 547 | 0.33 | 0.13–0.87 | 0.03a | 0% | 0.59 | 0.634 | 0.602 | 0.04 | 25 |
| Early postplypectomy bleeding | 3 | 547 | 0.29 | 0.08–1.02 | 0.05a | 0% | 0.45 | 0.491 | 0.602 | 0.03 | 33 |
| Delayed postpolypectomy bleeding | 3 | 547 | 0.58 | 0.13–2.49 | 0.46 | 0% | 0.94 | 0.403 | 0.602 | 0.01 | 100 |
OR = Odds ratio, 95%CI = 95% Confidential interval.
Statistical significant.
4. Discussion
Submucosal epinephrine injections inhibit blood flow into the polyp stalk, which provokes vasoconstriction and compression of the polyp vessels [20]. However, until now, the effectiveness of routine submucosal epinephrine injection has not been clearly demonstrated. This meta-analysis, evaluated the preventative effect of the prophylaxis epinephrine injections for overall, early, and delayed postpolypectomy bleeding complications. The routine used of local epinephrine injection significantly reduced the occurrence of overall (3.4% vs. 9.0%) and early (2.8% vs. 7.7%) postpolypectomy bleeding in comparison with saline injection or non-injection.
The effectiveness of mechanical hemostasis devices (such as endoloops or endoscopic clips) for preventing postpolypectomy bleeding by securing of the polyp stalks or closing mucosal defect has been well established. However, previous randomized controlled studies failed to demonstrate the efficacy of the routine use of the clips to prevent delayed postpolypectomy bleeding (possibly due to small sample sizes and the fact that the mean diameter of the polyps in the study was only 7.8 mm) [21].
To attempt to clarify the effectiveness of this treatment, the study analyzed data from three randomized studies that compared the efficacy of epinephrine injection and mechanical hemostasis in postpolypectomy bleeding examined in the patients with polyp sizes > 20 mm. The results demonstrated that prophylactic treatment with mechanical hemostasis is more effective than epinephrine injection for preventing of overall postpolypectomy bleeding (2.2% vs. 6.3%) and early postpolypectomy bleeding (1.1% vs. 4.5%) postpolypectomy bleeding.
The application of submucosal epinephrine injection and mechanical hemostasis device (in the polyps’ size larger than 20 mm.) as a routine procedure is helpful to reduce the occurrence of postpolypectomy bleeding. Both preventative methods are safe and establish hemostasis of the polyp stumps following a polypectomy as well as reduce the risk of bleeding, which contributes to the encouragement of the patient safety, reduce cost and avoid unnecessary intervention to correct the postpolypectomy bleeding (such as blood transfusion, endoscopic intervention, embolization and surgery) [22].
Nonetheless, neither prophylaxis methods were found to significantly reduce the risk of delayed postpolypectomy bleeding. However, this may reflect aspects of our analysis, rather than the inefficiency of the methods in preventing delayed bleeding. For instance, only a few examples of delayed bleeding were included in our study; most of the patients were treated with cutting modes or blend currents that are associated with a lower risk of delayed bleeding and patients who were more likely to suffer from delayed bleeding (such as those with coagulopathy or taking the anticoagulants) were excluded [23], [24], [25], [26].
While the findings of the meta-analysis help clarify the effectiveness of these treatments, the study is subject to several limitations. For instance, in order to the data set that was as appropriate for comparison as possible, only a limited number of randomized controlled studies were included in the meta-analysis. In addition, differences in the electrical current used in the polypectomy procedures, as well as variations in the types and pathologic features of the polyp in each study may have led to an increase in the heterogeneity between the studies.
Moreover, in the studies comparing the prophylaxis effect of epinephrine injections with that of mechanical methods, patients taking anticoagulants, those with abnormal coagulation, and those with pedunculated polyp sizes smaller than 20 mm and non-English studies were excluded from the data, which may have resulted in some level of publication bias in the meta-analysis. However, the statistical tests did not identify heterogeneity between the studies nor publication bias.
Established in the result of the meta-analysis, the occurrence of delayed postpolypectomy bleeding was less than 0.01% and there was a limited number of randomized controlled studies in this meta-analysis. Thus, the negative results in a small sample size may contribute to non-significant difference in bleeding outcomes. Thus, a power calculation with 0.05% significance level and 80% power was used. Future RCTs will need to enroll 1275 polypectomy procedures in each arm to rule out a 50% relative risk reduction (1% absolute risk reduction) in routine use of submucosal epinephrine injection and application of hemostasis device for the prevention of delayed postpolypectomy bleeding.
Given the study focused exclusively on studies where the mean polyp size was larger than 15 mm, it may be beneficial for future randomized controlled studies to examine the efficacy of prophylaxis submucosal epinephrine injections in the smaller sized polyps. Further research on the effectiveness of routine use of these treatments in patients at high risk of postpolypectomy bleeding patients (such as those undergoing antiplatelet and anticoagulant therapy) may also be beneficial.
5. Conclusion
This study demonstrates the benefit of prophylaxis submucosal epinephrine injections and mechanical hemostasis devices for the prevention of postpolypectomy bleeding. On the basis of this findings; the use of epinephrine injection as a routine procedure before the performance of a polypectomy were recommended. In cases where polyps are larger than 20 mm, a combination treatment, where treatment with epinephrine injection is combined with the placing of mechanical hemostasis devices, may be more effective in significantly decreasing the occurrence of bleeding.
Ethical approval
This research is not a study in humans or animals.
Funding
The study was supported by grants from Faculty of Medicine, Srinakharinwirot University (240/2559), Thailand.
Author contribution
The Corresponding author of this manuscript is Dr. Thawatchai Tullavardhana and contribution of the authors as mentioned below with their responsibility in the research.
1. Dr.Prinya Akkranurakul: working as a reviewer of all relevant potential selected articles.
2. Dr.Thammanit Rookkachart: working on data analysis and manuscripts prove reading.
Conflicts of interest
The authors have no conflicts of interest or financial ties to disclose.
Research registration unique identifying number (UIN)
Reviewregistry239.
Guarantor
Dr. Thawatchai Tullavardhana.
Acknowledgments
The study was supported by grants from Faculty of Medicine, Srinakharinwirot University, Thailand.
References
- 1.Winawer S.J., Zauber A.G., Ho M.N., O'Brien M.J., Gottlieb L.S., Sternberg S.S. Prevention of colorectal cancer by colonoscopic polypectomy. The national polyp study workgroup. N. Engl. J. Med. 1993;329(27):1977–1981. doi: 10.1056/NEJM199312303292701. [DOI] [PubMed] [Google Scholar]
- 2.Rogers B.H., Silvis S.E., Nebel O.T., Sugawa C., Mandelstam P. Complications of flexible fiberoptic colonoscopy and polypectomy. Gastrointest. Endosc. 1975;22(2):73–77. doi: 10.1016/s0016-5107(75)73705-7. [DOI] [PubMed] [Google Scholar]
- 3.Rosen L., Bub D.S., Reed J.F., 3rd, Nastasee S.A. Hemorrhage following colonoscopic polypectomy. Dis. colon rectum. 1993;36(12):1126–1131. doi: 10.1007/BF02052261. [DOI] [PubMed] [Google Scholar]
- 4.Choo W.K., Subhani J. Complication rates of colonic polypectomy in relation to polyp characteristics and techniques: a district hospital experience. J. interv. gastroenterol. 2012;2(1):8–11. doi: 10.4161/jig.20126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim H.S., Kim T.I., Kim W.H., Kim Y.H., Kim H.J., Yang S.K., Myung S.J., Byeon J.S., Lee M.S., Chung I.K., Jung S.A., Jeen Y.T., Choi J.H., Choi K.Y., Choi H., Han D.S., Song J.S. Risk factors for immediate postpolypectomy bleeding of the colon: a multicenter study. Am. J. gastroenterol. 2006;101(6):1333–1341. doi: 10.1111/j.1572-0241.2006.00638.x. [DOI] [PubMed] [Google Scholar]
- 6.Lorenzo-Zúñiga V., Moreno de Vega V., Doménech E., Mañosa M., Planas R., Boix J. Endoscopist experience as a risk factor for colonoscopic complications. Colorectal Dis. Off. J. Assoc. Coloproctol. G. B. Irel. 2010;12(10 Online):e273–e277. doi: 10.1111/j.1463-1318.2009.02146.x. [DOI] [PubMed] [Google Scholar]
- 7.Dobrowolski S., Dobosz M., Babicki A., Głowacki J., Nałecz A. Blood supply of colorectal polyps correlates with risk of bleeding after colonoscopic polypectomy. Gastrointest. Endosc. 2006;63(7):1004–1009. doi: 10.1016/j.gie.2005.11.063. [DOI] [PubMed] [Google Scholar]
- 8.Iida Y., Miura S., Munemoto Y., Kasahara Y., Asada Y., Toya D., Fujisawa M. Endoscopic resection of large colorectal polyps using a clipping method. Dis. colon rectum. 1994;37(2):179–180. doi: 10.1007/BF02047544. [DOI] [PubMed] [Google Scholar]
- 9.Luigiano C., Ferrara F., Ghersi S., Fabbri C., Cennamo V., Landi P., Polifemo A.M., Billi P., Bassi M., Consolo P., Alibrandi A., D'Imperio N. Endoclip-assisted resection of large pedunculated colorectal polyps: technical aspects and outcome. Dig. Dis. Sci. 2010;55(6):1726–1731. doi: 10.1007/s10620-009-0905-2. [DOI] [PubMed] [Google Scholar]
- 10.Lee Chang Kyun, Lee Suck-Ho, Park Ji-Young, Lee Tae Hoon, Chung Il-Kwun, Park Sang-Heum, Kim Hong-Soo, Kim Sun-Joo. Prophylactic argon plasma coagulation ablation does not decrease delayed postpolypectomy bleeding. Gastrointest. Endosc. 2009;70(2):353–361. doi: 10.1016/j.gie.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 11.Iishi H., Tatsuta M., Kitamura S., Narahara H., Iseki K., Ishiguro S. Endoscopic resection of large sessile colorectal polyps using a submucosal saline injection technique. Hepato Gastroenterol. 1997 May-Jun;44(15):698–702. [PubMed] [Google Scholar]
- 12.Chung S.S., Lau J.Y., Sung J.J., Chan A.C., Lai C.W., Ng E.K., Chan F.K., Yung M.Y., Li A.K. Randomised comparison between adrenaline injection alone and adrenaline injection plus heat probe treatment for actively bleeding ulcers. BMJ Clin. Res. Ed.) 1997;314(7090):1307–1311. doi: 10.1136/bmj.314.7090.1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J. Clin. Epidemiol. 2009;62(10):e1–34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 14.Lee S.H., Chung I.K., Kim S.J., Kim J.O., Ko B.M., Kim W.H., Kim H.S., Park D.I., Kim H.J., Byeon J.S., Yang S.K., Jang B.I., Jung S.A., Jeen Y.T., Choi J.H., Choi H., Han D.S., Song J.S. Comparison of postpolypectomy bleeding between epinephrine and saline submucosal injection for large colon polyps by conventional polypectomy: a prospective randomized, multicenter study. World J. gastroenterol. 2007;13(21):2973–2977. doi: 10.3748/wjg.v13.i21.2973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsieh Y.H., Lin H.J., Tseng G.Y., Perng C.L., Li A.F., Chang F.Y., Lee S.D. Is submucosal epinephrine injection necessary before polypectomy? A prospective, comparative study. Hepato Gastroenterol. 2001 Sep-Oct;48(41):1379–1382. [PubMed] [Google Scholar]
- 16.Dobrowolski S., Dobosz M., Babicki A., Dymecki D., Hać S. Prophylactic submucosal saline-adrenaline injection in colonoscopic polypectomy: prospective randomized study. Surg. Endosc. 2004;18(6):990–993. doi: 10.1007/s00464-003-9214-6. [DOI] [PubMed] [Google Scholar]
- 17.Di Giorgio P., De Luca L., Calcagno G., Rivellini G., Mandato M., De Luca B. Detachable snare versus epinephrine injection in the prevention of postpolypectomy bleeding: a randomized and controlled study. Endoscopy. 2004;36(10):860–863. doi: 10.1055/s-2004-825801. [DOI] [PubMed] [Google Scholar]
- 18.Paspatis Gregorios A., Paraskeva Konstantina, Theodoropoulou Angeliki, Mathou Nikoletta, Vardas Emmanouil, Oustamanolakis Pantelis, Chlouverakis Gregorios, Karagiannis Ioannis. A prospective, randomized comparison of adrenaline injection in combination with detachable snare versus adrenaline injection alone in the prevention of postpolypectomy bleeding in large colonic polyps. Am. J. Gastroenterol. 2006;101(12):2805–2809. doi: 10.1111/j.1572-0241.2006.00855.x. [DOI] [PubMed] [Google Scholar]
- 19.Kouklakis G., Mpoumponaris A., Gatopoulou A., Efraimidou E., Manolas K., Lirantzopoulos N. Endoscopic resection of large pedunculated colonic polyps and risk of postpolypectomy bleeding with adrenaline injection versus endoloop and hemoclip: a prospective, randomized study. Surg. Endosc. 2009;23(12):2732–2737. doi: 10.1007/s00464-009-0478-3. [DOI] [PubMed] [Google Scholar]
- 20.Shirai M., Nakamura T., Matsuura A., Ito Y., Kobayashi S. Safer colonoscopic polypectomy with local submucosal injection of hypertonic saline-epinephrine solution. Am. J. gastroenterol. 1994;89(3):334–338. [PubMed] [Google Scholar]
- 21.Shioji Kazuhiko, Suzuki Yutaka, Kobayashi Masaaki, Nakamura Atsuo, Azumaya Masaki, Takeuchi Manabu, Baba Youichiro, Honma Terasu, Narisawa Rintaro. Prophylactic clip application does not decrease delayed bleeding after colonoscopic polypectomy. Gastrointest. Endosc. 2003;57(6):691–694. doi: 10.1067/mge.2003.193. [DOI] [PubMed] [Google Scholar]
- 22.Gibbs D.H., Opelka F.G., Beck D.E., Hicks T.C., Timmcke A.E., Gathright J.B., Jr. Postpolypectomy colonic hemorrhage. Dis. colon rectum. 1996;39(7):806–810. doi: 10.1007/BF02054448. [DOI] [PubMed] [Google Scholar]
- 23.Van Gossum A., Cozzoli A., Adler M., Taton G., Cremer M. Colonoscopic snare polypectomy: analysis of 1485 resections comparing two types of current. Gastrointest. Endosc. 1992 Jul-Aug;38(4):472–475. doi: 10.1016/s0016-5107(92)70479-9. [DOI] [PubMed] [Google Scholar]
- 24.Matsumoto M., Fukunaga S., Saito Y., Matsuda T., Nakajima T., Sakamoto T., Tamai N., Kikuchi T. Risk factors for delayed bleeding after endoscopic resection for large colorectal tumors. Jpn. J. Clin. Oncol. 2012;42(11):1028–1034. doi: 10.1093/jjco/hys131. [DOI] [PubMed] [Google Scholar]
- 25.Watabe H., Yamaji Y., Okamoto M., Kondo S., Ohta M., Ikenoue T., Kato J., Togo G., Matsumura M., Yoshida H., Kawabe T., Omata M. Risk assessment for delayed hemorrhagic complication of colonic polypectomy: polyp-related factors and patient-related factors. Gastrointest. Endosc. 2006;64(1):73–78. doi: 10.1016/j.gie.2006.02.054. [DOI] [PubMed] [Google Scholar]
- 26.Sawhney M.S., Salfiti N., Nelson D.B., Lederle F.A., Bond J.H. Risk factors for severe delayed postpolypectomy bleeding. Endoscopy. 2008;40(2):115–119. doi: 10.1055/s-2007-966959. [DOI] [PubMed] [Google Scholar]