Abstract
SLE is a chronic inflammatory disease that affects the kidneys in about 50% of patients. Lupus nephritis is a major risk factor for overall morbidity and mortality in SLE, and despite potent anti-inflammatory and immunosuppressive therapies still ends in CKD or ESRD for too many patients. This review highlights recent updates in our understanding of disease epidemiology, genetics, pathogenesis, and treatment in an effort to establish a framework for lupus nephritis management that is patient-specific and oriented toward maintaining long-term kidney function in patients with lupus.
Keywords: systemic lupus erythematosus, Epidemiology and outcomes, glomerular disease, glomerulonephritis, immunosuppression, nephritis, humans, kidney, kidney failure, chronic, Lupus Erythematosus, Discoid, Lupus Erythematosus, Systemic, lupus nephritis, Renal Insufficiency, Chronic, risk factors
Epidemiology
SLE is a chronic inflammatory disease that can affect any organ, but very often injures the kidney. SLE is more prevalent in women than men across all age groups and populations; the female-to-male ratio is highest at reproductive age, ranging between 8:1 and 15:1, and is lowest in prepubertal children at about 4:3 (1–3). The prevalence of SLE and the chances of developing lupus nephritis (LN) vary considerably between different regions of the world and different races and ethnicities (Table 1) (2,4–14). In the United States, the higher frequency of LN in black populations persists after adjustment for socioeconomic factors (15). Additionally, black and Hispanic SLE patients develop LN earlier (16), and have worse outcomes than white patients with SLE, including death and ESRD (10). This might explain why black individuals account for nearly half of those with ESRD due to LN (17). The more aggressive disease course in black individuals might be the result of a higher incidence of diffuse proliferative LN, or the presence of more high-risk features within the same LN histologic class when compared with white individuals (18). Those differences may arise due to genetic predisposition as some “high-risk” genotypes and autoantibodies are more frequent in black patients (19–21). For example, black populations have a higher frequency of the Fcγ RIIA-R131 allele which is involved in mediating phagocytosis of IgG2 immune complexes (20). The APOL1 gene, which has been implicated in the development of ESRD in black patients, has also been associated with progression and development of ESRD in the LN population (22,23). In LN patients with two risk alleles for APOL1 the odds ratio (OR) for ESRD was 2.72 (95% confidence interval [95% CI], 1.76 to 4.19; P<6.2×10−6). An HLA-DR2 subtype (HLA-DRB181503), characteristic of black populations, was linked to worsening proteinuria (24). Black individuals are also more likely to have positive anti-Ro, anti-Sm, and anti-RNP antibodies, which have a high association with LN (25).
Table 1.
Prevalence of SLE and frequency of lupus nephritis
| Demographics | Prevalence, Per 100,000 | Frequency, % | References |
| SLE | |||
| Region | |||
| United States, Canada | 4.8–78.5 | Danchenko et al. (2) | |
| Europe (United Kingdom, Germany, France, Italy, Spain, Scandinavia) | 25–91 | Danchenko et al. (2) | |
| Australia | 19–63 | Danchenko et al. (2) | |
| China | 30–50 | Osio-Salido et al. (4) | |
| Japan | 8–18 | Osio-Salido et al. (4) | |
| Lupus nephritis | |||
| Race/ethnicity | |||
| Black | 69 | Bastian et al. (8) | |
| White | 29 | Bastian et al. (8) | |
| Asian | 40–82 | Jakes et al. (99) | |
| Hispanic | 61 | Bastian et al. (8) |
LN is a major risk factor for morbidity and mortality in SLE and 10% of patients with LN will develop ESRD (26). The risk of ESRD is higher in certain subsets of LN. For example, in class 4 LN the risk may be as high as 44% over 15 years (27). Patients with LN also have a higher standardized mortality ratio (6–6.8 versus 2.4) and die earlier than SLE patients without LN (28–31). Importantly, 10-year survival improves from 46% to 95% if disease remission can be achieved (32).
Genetics and Pathogenesis
A detailed discussion of the genetics and pathogenesis of LN is beyond the scope of this review, but can be found in Munroe and James (33). Here we will focus on recent findings that may be applicable to the clinical management of LN.
Systemic Lupus versus LN
Given the morbidity associated with LN, the ability to accurately identify SLE patients destined to develop LN could shift the current management paradigm from treatment to prevention. Although it is not likely that CKD and ESRD can be avoided completely, because many patients present with LN as the initial manifestation of their SLE, a preventative management strategy could significantly reduce CKD and ESRD. For example, SLE patients destined to develop LN could be followed much more closely, perhaps with home monitoring of the urine so kidney biopsy and treatment could be started without delay. Alternatively, such patients could be considered for pre-emptive therapy to attenuate autoimmunity before any clinical manifestations of kidney involvement are apparent. Although it is currently not possible to determine a priori who with SLE will develop LN, several investigations of lupus genetics have approached this question.
SLE arises in individuals with an appropriate genetic background exposed to certain environmental triggers. Several genes have been associated with SLE susceptibility, most prominently in the human HLA loci. A meta-analysis of HLA-DRB1 alleles in SLE concluded that carriers of HLA-DR4 and DR11 were protected against LN with ORs of 0.55 (95% CI, 0.39 to 0.79; P<0.01) and 0.6 (95% CI, 0.37 to 0.96; P<0.05), respectively (34). Conversely HLA-DR3 and DR15 conferred an increased risk of LN with ORs of 2.0 (95% CI, 1.49 to 2.7; P<0.05) and 1.6 (95% CI, 0.37 to 0.96; P<0.05). These associations were on the basis of 473 patients from five case-control studies, and included mainly white and Asian patients. Controls were healthy individuals. The mechanisms of HLA-based disease susceptibility and protection remain unknown. It has been suggested that this may be related to the degree of stability of the interaction between self-peptide and its HLA binding partner (35,36). More stable interactions may lead to protection as in other autoimmune diseases like rheumatoid arthritis.
In another approach, a meta-analysis of three genome-wide association studies was done to identify risk alleles for LN in patients already known to have SLE (37). All patients were women of European descent (n=2000) and 588 had LN. LN was defined by the American College of Rheumatology criteria of persistent proteinuria and abnormalities of the urine sediment. Here the most significant associations for LN mapped to the PDGF receptor A gene (OR, 3.41; 95% CI, 2.10 to 5.54; P=4.52×10−7) and the gene for the sodium-dependent glucose cotransporter SLC5A11 (OR, 2.85; 95% CI, 1.93 to 4.22; P=5.08×10−7). HLA loci were less strongly associated with LN in this analysis, possibly because the comparison group had lupus, and therefore was already linked strongly to HLA. In LN, PDGF may mediate kidney cell proliferation, matrix accumulation, and intrarenal inflammation. The link between SLC5A11 and LN is more convoluted. Several solute carrier (SLC) family genes have been associated with CKD (38). Variants in SLC5A11 may mediate a decrease in serum and an increase in urine myo-inositol, suggesting an active role of SLC5A11 in proximal tubule inositol reabsorption (38). Additionally, or through inositol regulation, SLC5A11 may mediate apoptosis through the programmed cell death and TNF-α pathways (39).
The limitations of these and other genetic association studies are the relatively small numbers of affected patients available for analysis, and the limited racial and ethnic diversity of the study cohorts, which to date have mainly focused on white and Asian patients.
Pathogenesis
Clues as to how LN develops in SLE patients were provided by a study of how the transcriptome of peripheral blood cells changed over time in a cohort of pediatric LN patients (40). LN occurred when the expression of neutrophil-associated genes increased. Neutrophil activation was preceded by an increase in IFN and plasmablast-related transcripts and was followed by upregulation of other myeloid cell and proinflammatory transcripts. These data were synthesized in a model of lupus in which the disease initiates preclinically with an IFN response and differentiation of B cells into plasmablasts, and progresses to tissue-specific (e.g., the kidney) and systemic inflammation as neutrophils and myeloid cells activate.
Neutrophils can contribute to the pathogenesis of SLE and LN even in death. When neutrophils die they often release neutrophil extracellular traps (NETs), which are composed of chromatin fibrils, histones, and neutrophil antibacterial and immunostimulatory proteins. This type of cell death, called NETosis, is normally a host defense mechanism to trap and kill microorganisms. However, NETs and NETing neutrophils can also be found in the kidneys of patients with SLE (41). NETs are a source of nuclear antigens in SLE and may help to maintain antigen-specific autoantibody production. NETS and NETing neutrophils facilitate inflammation, may cause endothelial damage, and can induce plasmacytoid dendritic cells to produce IFN-α (41), amplifying autoimmunity. Importantly, NET degradation is impaired in patients with SLE, and mainly in those with LN (42).
The C system is generally activated in LN and may directly mediate kidney injury through the terminal pathway, or indirectly increase renal inflammation by recruiting leukocytes to the kidney. Because C also helps clear apoptotic debris, it is important in reducing exposure to autoantigens. In this regard, autoantibodies to C components that are found in patients with lupus may be important in the development of LN. In a cohort of 114 lupus patients, 23% of patients had autoantibodies to C component C1q and to C3b (43). In these dual-antibody–positive patients who were prospectively followed, anti-C3b and anti-C1q levels tended to increase in the months leading up to renal flare. In vitro experiments have shown that anti-C1q binds C1q on early apoptotic cells and prevents their uptake by macrophages (44). Anti-C1q also blocks immune complex binding to red blood cells, a mechanism to safely clear immune complexes. These data suggest anti-C1q antibodies may enhance autoantigen exposure and may facilitate immune complex deposition in target organs like the kidneys. Consistent with this, it was shown that the absence of anti-C1q autoantibodies was qualitatively associated with protection against LN in a small cohort of lupus patients (45). Furthermore, C3b on immune complexes promotes immune complex binding to red blood cells for clearance. This may be blocked by anti-C3b, thereby augmenting the pro-LN effects of anti-C1q.
Finally, a recent investigation tied concepts important for viral immunity to autoimmunity, providing insights into relapsing autoimmune disease (46), a problem that is particularly relevant to LN. CD8 T cells become “exhausted” in the setting of persistent antigen exposure and the absence of CD4 T cell costimulation. These exhausted CD8 cells lose effector function and express inhibitory receptors at high levels. This leads to an inability to clear viral infections, but can be protective against relapsing autoimmune disease. In patients with SLE (not necessarily LN), a limited group of upregulated coinhibitory receptors characterized exhausted T cells, which translated to patients who had a nonrelapsing course of lupus. The upregulated genes were 4–1BB, CTLA4, PDCD1, LILRB4, and KLG1. The exhausted phenotype can be rescued by costimulation, and certain genes, like KAT2B, can facilitate this. KAT2B is antiapoptotic and mediates protection against metabolic stress. In this paradigm of disease relapse, yet to be tested in LN, therapeutic interventions to increase T cell exhaustion, perhaps by upregulating inhibitory receptor expression, or blocking costimulation to maintain the exhausted phenotype, may help prevent renal flares. It is intriguing to speculate that stable HLA presentation of self-antigens results in T cell exhaustion and protection in SLE, whereas unstable HLA associations with self-antigens result in intermittent T cell activation, enhanced costimulation, and suppression of the exhaustive (protective) T cell phenotype.
Clinicopathologic Correlations
The clinical manifestations of LN are often subtle and most commonly will be discovered by examination of the urine as opposed to physical examination (Table 2). Therefore, all patients with SLE should be evaluated for kidney involvement at initial diagnosis and at least yearly thereafter even if they do not have symptoms of kidney disease. It is also recommended that patients be re-evaluated for LN if SLE flares. Evaluation is straightforward and should include a urinalysis and measurement of kidney function, generally a serum creatinine concentration or eGFR. Because SLE patients often have several concomitant medical issues and may be on potentially nephrotoxic medications, it is important to exclude nonlupus causes of renal insufficiency, especially if the urinalysis does not show abnormal proteinuria and hematuria. If kidney involvement is suspected a kidney biopsy should be considered (see below). The clinical threshold for doing a kidney biopsy is not well defined, but we suggest performing a biopsy if proteinuria ≥500 mg/d, with or without other clinical abnormalities, or any level of proteinuria or hematuria with impaired kidney function that cannot be attributed to another cause. There is observational evidence that proteinuria of 500–1000 mg/d (or lower) may be associated with significant kidney pathology (47), and it has been well established that early diagnosis and treatment of LN improves prognosis (48).
Table 2.
Prevalence of clinical manifestations in patients with lupus nephritis
| Clinical Manifestation | Approximate Prevalence, % |
| Proteinuria | 100 |
| Nephrotic range proteinuria/nephrotic syndrome | 50 |
| Microscopic hematuria | 80 |
| Macroscopic hematuria | <5 |
| Urinary red blood cell casts | 30 |
| Other urinary cellular casts | 30 |
| Renal insufficiency | 60 |
| Rapid decline in kidney function | 15 |
| Hypertension | 30 |
| Tubular abnormalities | 70 |
The Kidney Biopsy in LN
Although the decision to perform a kidney biopsy in SLE patients when there is clinical evidence of renal involvement seems straightforward, it has become somewhat controversial because of a prevailing view that all forms of LN can be adequately treated with corticosteroids plus mycophenolate mofetil (MMF) (49). Nonetheless, the kidney biopsy is important to define the nature of renal involvement. Although immune-complex–mediated GN is the most common cause of kidney disease in SLE, there are other mechanisms that result in renal injury which can only be diagnosed with a biopsy, and require a different approach to management than immune-complex LN. Examples include thrombotic microangiopathy and lupus podocytopathy (defined as nephrotic syndrome in SLE that on kidney biopsy shows diffuse foot process effacement and no subendothelial or subepithelial immune deposits), which can be seen in up to 24% and 1.3% of LN patients, respectively (50,51). The finding of isolated tubulointerstitial nephritis is rare (52).
Immune-complex LN is described pathologically using the 2003 International Society of Nephrology/Renal Pathology Society (ISN/RPS) nomenclature (53). The ISN/RPS system classifies LN on the basis of where immune complexes accumulate in glomeruli, the presence or absence of mesangial or endocapillary proliferation, the overall extent of glomerular involvement (focal or diffuse) and glomerular injury (global or segmental), and whether glomerular injury is active (inflammatory) or chronic (sclerotic) (Table 3). In a general way, the ISN/RPS classes guide treatment decisions. Patients with disease limited to the mesangium (class 2) generally do not need specific therapy for their kidney disease but may need immunosuppressive treatment for extrarenal SLE manifestations. Patients with mainly chronic injury (any class) or end stage damage (class 6) also do not need immunosuppression for LN, but may benefit from antiproteinuric, renoprotective measures. The proliferative classes (3 and 4) are often treated with potent immunosuppression, whereas nonproliferative, membranous LN (class 5) may be managed conservatively (antiproteinuric therapy) if patients have subnephrotic proteinuria, or with immunosuppression if patients have nephrotic range proteinuria.
Table 3.
The histologic classification of lupus nephritis
| ISN/RPS Class | Histologic Findings | Modifications to Histology | Usual Clinical Findings |
| 1 | Normal light microscopy; mesangial immune complexes by immunofluorescence microscopy | None relevant to the kidney so rarely diagnosed or biopsied | |
| 2 | Mesangial immune complexes/mesangial cell proliferation | Hematuria, low-grade proteinuria; renal insufficiency, nephrotic syndrome not expected | |
| 3 | Mesangial and subendothelial immune complexes/segmental endocapillary proliferation in <50% of glomeruli | Lesions can be active, chronic, or have elements of both | Hematuria, proteinuria seen in most patients; renal insufficiency, nephrotic syndrome not unusual |
| 4 | Mesangial and subendothelial immune complexes/segmental or global endocapillary proliferation in ≥50% of glomeruli | Lesions can be active, chronic, or have elements of both | Hematuria, proteinuria seen in most patients; renal insufficiency, nephrotic syndrome not unusual |
| 5 | Numerous subepithelial immune complexes in >50% of glomerular capillaries | Proteinuria, often nephrotic range; hematuria possible; usually no renal insufficiency | |
| 6 | Glomerulosclerosis in >90% of glomeruli | Renal insufficiency; proteinuria and hematuria often present |
ISN/RPS, International Society of Nephrology/Renal Pathology Society.
As the therapy of LN moves beyond the currently available nontargeted immunosuppressive regimens of high-dose corticosteroids plus cyclophosphamide or MMF to interventions that focus on specific immune pathways, a more comprehensive picture of kidney pathology through molecular imaging of the kidney biopsy may be desirable. The immune pathways active in the kidney at the time of LN diagnosis vary considerably between patients. For example, when glomeruli were dissected from human LN biopsies and subject to transcriptomic analysis, patients segregated into groups showing dominant expression of B cell genes, myelomonocytic genes, IFN-inducible genes, or fibrosis-related genes (54). Similar pathways have been shown to be activated in the kidneys of lupus-prone mice (55). These molecular variations may reflect the intrinsic heterogeneity of LN or may occur because patients are biopsied at different points in the course of a disease that rapidly evolves. Regardless of how LN heterogeneity arises, these molecular differences suggest that a targeted therapy is not likely to work for all patients, but only those with activity in a specific autoimmune or inflammatory pathway. The applicability of molecular analyses of the kidney biopsy to LN treatment is illustrated by a recent survey of transcript expression of immune genes in kidney biopsies done at LN flare. Patients who had early complete clinical renal responses to standard-of-care induction therapies could be distinguished from nonresponders on the basis of transcript expression profiles (56). A similar approach could conceivably be applied to patients being treated with novel therapies to define which patients are likely to respond to a particular treatment.
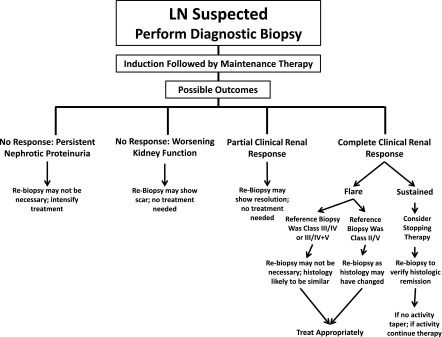
The role of protocol repeat kidney biopsies in LN is controversial, but emerging data suggest serial biopsies may inform ongoing treatment decisions and predict long-term renal prognosis. Repeat biopsies have demonstrated considerable discordance between clinically- and histologically-defined disease activity. After completing 6–8 months of immunosuppressive therapy, 20%–50% of complete clinical renal responders still had histologic evidence of ongoing active inflammation, and 40%–60% of patients with no histologic evidence of disease activity still had persistent, high-grade proteinuria (57,58). Even after several years of immunosuppressive treatment, histologic activity was found in about 20% of patients who had been in sustained clinical remission. Conversely, 40% of patients in complete histologic remission after long-term treatment had persistent clinical findings (59). These results suggest that an immediate application of repeat biopsies could be to evaluate a patient for withdrawal of maintenance immunosuppressive therapy. Presently there are no evidence-based guidelines concerning the duration of LN maintenance therapy (60).
The prognostic value of the diagnostic kidney biopsy for predicting long-term renal health in LN has been disappointing (61). However, repeat biopsies after at least 6 months of immunosuppressive therapy appear to provide better prognostic information. Persistent histologic evidence of glomerular and interstitial inflammation, glomerular capillary immune complexes, and macrophages in tubular lumens after completing induction therapy were risk factors for future doubling of the serum creatinine concentration (62,63). Increasing chronic damage on the postinduction biopsy also predicted long-term renal outcomes in some studies (57,58). The National Institutes of Health (NIH) activity and chronicity indices (64) were measured in repeat biopsies 12–18 months after starting treatment, while patients were on maintenance immunosuppression (65). After 10 years of follow-up, the probability of doubling serum creatinine was about 56% for patients whose second biopsy had persistent activity (an activity index >2), compared with 20% for patients who had an activity index ≤2 (P<0.001). Similarly, 10-year renal survival was >90% if the chronicity index of the repeat biopsy was <3, but 55% if the chronicity index was >6 (P=0.10).
Repeat kidney biopsies are also done in LN for clinical indications, with the assumption that the biopsy could support changes in therapy. Most of the time this is due to LN flare, persistent proteinuria, or declining kidney function (66–70). Considering these investigations together, some generalizations about clinically-indicated repeat biopsies may be drawn. Patients who originally had proliferative LN often show proliferative LN at flare, whereas many patients who originally had membranous LN often develop a proliferative component at flare. Similarly, in patients who had class 2 LN it is not unusual to find a more aggressive injury pattern at repeat biopsy. These findings suggest repeating a kidney biopsy for flare is most beneficial for patients with previous class 2 or 5 LN because there is a reasonable likelihood therapy may be intensified. Biopsies for persistent or worsening proteinuria or an increase in serum creatinine concentration do not necessarily reflect active LN; a biopsy diagnosis of chronic damage and inactive disease may allow a reduction in therapy.
On the basis of the current evidence of how a kidney biopsy may contribute to the management of LN, a suggested algorithm for initial and repeat kidney biopsies in lupus is provided in Figure 1.
Figure 1.
A proposed algorithm for when to perform a kidney biopsy in patients with lupus nephritis (LN).
The Treatment of LN
Management Strategy
The overarching goal of LN treatment is to prevent CKD and ESRD. As adverse kidney outcomes occur far more frequently in proliferative LN, we will focus on the treatment of classes 3 and 4. To prevent CKD and ESRD, short-term treatment strategies have focused on complete or partial reversal of the clinical signs of kidney injury discussed previously. By the time LN is clinically apparent the kidney is already modestly or severely inflamed due to the accumulation of autoantibody-containing immune complexes. Therefore, patients are treated with an anti-inflammatory agent to immediately attenuate intrarenal inflammation and allow healing to begin, coupled with a potent immunosuppressive agent to interrupt autoimmune pathways that could reignite renal immune complex formation and start the cycle of inflammatory injury again (renal flare). This induction phase of treatment generally lasts 3–6 months and is followed by a prolonged, but less intense maintenance phase, often lasting years. It is not clear when maintenance therapy can be withdrawn. A repeat kidney biopsy showing histologic remission during maintenance in patients who have achieved complete clinical remission, or who have stable but persistent proteinuria, may help in making a decision to taper off therapy. A randomized clinical trial is currently being done to address the question of duration of maintenance therapy (Clinicaltrials.gov identifier: NCT01946880).
The report card for this management strategy is mixed. Induction and maintenance therapies have improved overall patient survival to about 80% at 5 years, however, 12-month complete renal response rates are only 10%–40%, and as many as 30% of LN patients will still progress to ESRD (71–75). Furthermore, although there are no estimates of how many LN patients are left with CKD after treatment, the number is likely to be large. For example, kidney biopsies after induction therapy with high-dose corticosteroids and cyclophosphamide or MMF generally show an increase in chronic damage, even in those patients who achieved a complete clinical remission to induction alone (57). LN flare is also an important risk factor for CKD and CKD progression (76) and flares may occur in 25% of patients (77,78). These outcome statistics suggest there is considerable room for improvement in the treatment of LN.
Current Approaches to Treatment
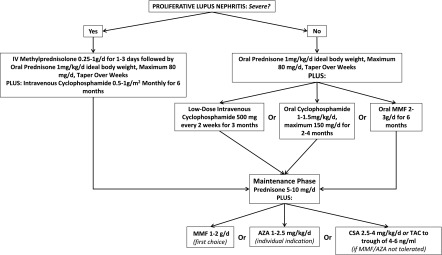
All current widely-accepted treatment regimens for LN (summarized in Figure 2) incorporate high-dose corticosteroids for rapid control of inflammation and either MMF or cyclophosphamide to control inflammation and autoimmunity (60,79). All patients (unless contraindicated) should be treated with an antimalarial given the evidence that lack of antimalarial use may be associated with an increase in LN treatment failures (80). Cyclophosphamide can be given orally or intravenously, and if intravenous in either standard-dose (designated the NIH regimen) or low-dose (called low-dose or Euro-lupus regimen). High intensity immunosuppression is given for the first 3–6 months and then replaced by MMF (or a lower dose of MMF if it was used for induction) or azathioprine to maintain suppression of autoimmunity and inflammation, and thereby prevent flare.
Figure 2.
Current induction and maintenance treatment choices for proliferative lupus nephritis. Patients are considered to have severe lupus nephritis if they have functional kidney injury with an elevated serum creatinine and/or heavy proteinuria, evidence that the loss of renal function occurred over a relatively short period of time and active histologic injury with glomerular crescents and necroses affecting several glomeruli. AZA, azathioprine; CSA, cyclosporine A; MMF, mycophenolate mofetil; TAC, tacrolimus.
Standard-dose cyclophosphamide (either oral or NIH) improved the long-term kidney survival compared with corticosteroids alone and set the standard-of-care for LN treatment (81). Because of toxicity concerns surrounding cyclophosphamide, MMF and NIH cyclophosphamide were directly compared in a large randomized controlled trial and found to be equivalent for the induction of renal responses after 6 months of treatment (73). Although the MMF arm had a similar number of adverse events as the cyclophosphamide arm, and its long-term ability to preserve renal function was not clear, MMF has replaced cyclophosphamide as first-line induction therapy for LN in many areas. The increased exposure of LN patients to MMF has raised some concerns as to whether it is equivalent to cyclophosphamide induction with respect to long-term kidney outcomes (77). A recent meta-analysis showed that between the 1970s and the 1990s the risk of ESRD from LN declined and plateaued, and this was coincident with cyclophosphamide treatment becoming routine (27). In the 2000s, as MMF was becoming a dominant induction drug for LN, the risk of ESRD increased, and was highest at 44% over 15 years in patients with diffuse proliferative LN.
In another attempt to reduce the long- and short-term toxicity of cyclophosphamide, low-dose, Euro-lupus cyclophosphamide was found to be equivalent to NIH cyclophosphamide for remission induction and preservation of renal function at 5 and 10 years, but with fewer adverse effects (78). The original Euro-lupus trial was done in a mainly white cohort with LN of mild-to-moderate severity, but recently, low-dose cyclophosphamide was found to be effective in a multiethnic/multiracial cohort with more severe LN (82).
The duration of corticosteroid administration in LN remains controversial and nonevidence-based. A small but interesting pilot study to assess the feasibility of doing a definitive trial on whether maintenance corticosteroids are needed in LN was done (83). The trial included 15 patients with proliferative (±membranous) LN induced with cyclophosphamide or MMF who achieved at least a partial response and had been tapered down to ≤20 mg of prednisone. After 3 weeks, prednisone was decreased to 5–7.5 mg/d in eight patients, and that dose was maintained. Prednisone was completely withdrawn in seven patients by week 17. Patients were followed for a median of 12 months, and the end point was renal or major nonrenal relapse. Relapse occurred in only one patient from the withdrawal group (14%; one renal flare), but in 50% of the low-dose prednisone patients (three renal and one major nonrenal flare). These data, although inconclusive, are provocative.
Opportunities in LN Management
To reduce the incidence of ESRD it will be necessary to prevent CKD. Preventing CKD will require more rapid and complete control of inflammatory kidney injury and minimization of LN flares. There are several opportunities to implement such a paradigm, which include developing methods for earlier diagnosis and treatment, improving patient compliance, and applying novel therapies. Here we will focus on creating opportunities with novel therapeutic approaches.
Controlling Renal Inflammation in LN
Historically, intrarenal inflammation has been controlled during induction by high-dose corticosteroids, which are effective but toxic (81). It is likely that many of the adverse outcomes that occur during the first year of LN treatment can be attributed to corticosteroids, and their side effects often challenge patient compliance. Borrowing existing therapies used for other diseases to treat renal inflammation may reduce or eliminate the need for corticosteroids. In this context, C inhibitors, quinolone immunomodulators, and proteasome inhibitors should be considered for LN clinical trials.
Several animal studies have demonstrated a beneficial effect of blocking the alternative C pathway in LN (84). Although little work has been done with C inhibition in human LN, effective inhibitors are available, including a monoclonal antibody against C5 (eculizumab) and a small molecule C5a receptor blocker (CCX168) (85). Interestingly, the ability of corticosteroids to attenuate intrarenal C activity in LN is not clear, but at least in some clinical settings, such as hemodialysis, they do not block C activation (86). Thus, C inhibitors may synergize with steroids to permit significant steroid dose reduction. Blocking the alternative C pathway can potentially attenuate renal inflammation and injury by inhibiting the chemotactic and leukocyte activating properties of C5a, and preventing the formation of C5b-9 (the membrane attack complex) which may directly injure renal cells.
Laquinimod, a quinolone, is a small molecule that blocks activation of NF-κB, a transcription factor important in the expression of proinflammatory cytokines that has been studied in human multiple sclerosis (87) and murine LN (88). A small phase 2 trial in LN showed improved kidney function and reduced proteinuria at 6 months when laquinimod was added to standard-of-care, including corticosteroids (89). These findings need to be replicated in a larger trial, but suggest synergy with steroids and offer the possibility of steroid dose reduction.
The proteasome inhibitors are used mainly to treat plasma cell malignancies, but their mechanism of action may offer efficacy at two steps in the pathogenesis of LN and kidney injury. The overall effect of the boronic acid proteasome inhibitors (for example, bortezomib and carfilzomib) is to kill plasma cells, so these drugs could immediately attenuate autoantibody production. This would be expected to halt or decrease immune complex production and thus ongoing immune complex–mediated renal injury. More directly relevant to inflammation, the proteasome inhibitors block activation of NF-κB, and so may also be anti-inflammatory. This class of drugs has successfully treated murine LN (90).
Minimizing LN Flares
In contrast to the many recent clinical trials of novel induction therapies in LN, flare prevention has received relatively little attention. However, several of these induction trials included follow-up and the effects of the experimental drugs on flare rate were determined. An interesting example is the abatacept and cyclophosphamide combination efficacy and safety study (ACCESS) trial which studied the effect of blocking the CD28/CD80 costimulatory pathway in LN with abatacept, a CTLA4-Ig construct. Although abatacept did not offer any benefit for induction of remission when added to low-dose cyclophosphamide, patients in the abatacept arm that reached a complete renal remission at 6 months were followed for another 6 months without any maintenance immunosuppressive therapy. At 12 months the patients in the abatacept arm had fewer SLE flares than patients in the placebo arm who did receive maintenance azathioprine. This study was not powered to test abatacept in maintenance of remission, and the flare rates were not significantly different, but the results suggest that abatacept may be worth investigating as a maintenance agent to prevent flares. Importantly, no important safety signal for abatacept was detected in the ACCESS trial.
Similarly, a post hoc analysis of belimumab, a monoclonal antibody directed against the B cell survival factor BLyS, trials in nonrenal lupus showed a dose-dependent trend toward a decreased rate of renal flares in patients who had received belimumab (91). This analysis suggested that belimumab may be effective in preventing renal flares in patients who have inactive or stable LN. In contrast, another anti-BLyS monoclonal antibody, tabalumab, also trialed in nonrenal SLE, did not prevent renal flares (92). The effects of BLyS blockade in LN are being directly tested in an ongoing trial (NCT0139330), so resolution of these conflicting results may need to wait until the trial is finished.
Other Emerging Therapies
IFN-α seems to be a central regulatory cytokine in SLE and especially in LN, and may promote development of autoreactive plasma cells, helper and memory T cells, and several proinflammatory cytokines (93–95). Blocking the effects of IFN-α may therefore ameliorate inflammation and attenuate autoimmunity and prevent future LN flares. Anifrolumab, a monoclonal antibody against the IFN-α type 1 receptor, was found to be effective in nonrenal lupus and is currently under evaluation in a randomized clinical trial in LN (NCT02547922).
The calcineurin inhibitors (CNIs) cyclosporine A and tacrolimus have been tested extensively in LN, especially in Asia, with very encouraging results. CNIs attenuate inflammation by preventing release of inflammatory cytokines from leukocytes, and also block T cell activation (96), and therefore could have an effect to maintain remission. CNIs have been used as part of a multitarget approach to treating LN, added to a regimen of MMF and corticosteroids, and have been shown to be superior to cyclophosphamide in inducing remission by 6 months (97). A multitarget approach is appealing as the pathogenesis of SLE involves several immune pathways. CNIs plus corticosteroids alone have also been used for LN induction and found to be as effective as MMF for proliferative LN (98). At this time, CNI studies need to be viewed cautiously. Unexpectedly, in the multitarget study patient withdrawals due to adverse events were higher in the CNI arm than the cyclophosphamide arm (97). The effects of CNIs in more racially and ethnically diverse cohorts must be studied. Additionally, most of the studies to date are fairly short-term, and long-term preservation of kidney function needs to be verified. Finally, because proteinuria is the major contributor to current criteria of LN response, and CNIs can affect proteinuria by mechanisms unrelated to immune modulation, it is not clear that proteinuria is an appropriate end point for comparing CNIs to drugs with different mechanisms of action. In this setting a kidney biopsy should be considered to verify histologic improvement/resolution.
Conclusions
LN continues to be a major source of morbidity and mortality for SLE patients. Most patients develop LN during the prime of their lives, and this adversely affects their livelihoods and families, affecting all of society. An improved understanding of disease pathogenesis has not yet resulted in major therapeutic advances. However, the availability of a variety of novel drugs to modify the immune system, coupled with a thoughtful approach to clinical trial design, is anticipated to overcome this slow progress in advancing LN management.
Disclosures
B.H.R. has consultancy agreements and has received honoraria from Lilly, Genentech-Roche, and Mallinckrodt, and has received research funding from the National Institute of Diabetes, Digestive Diseases and Kidney Diseases (NIDDK), Mallinckrodt, and Genentech.
This work was supported in part by NIDDK U01 DK096927 (to B.H.R.)
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Schwartzman-Morris J, Putterman C: Gender differences in the pathogenesis and outcome of lupus and of lupus nephritis. Clin Dev Immunol 2012: 604892, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Danchenko N, Satia JA, Anthony MS: Epidemiology of systemic lupus erythematosus: a comparison of worldwide disease burden. Lupus 15: 308–318, 2006 [DOI] [PubMed] [Google Scholar]
- 3.Mina R, Brunner HI: Pediatric lupus--are there differences in presentation, genetics, response to therapy, and damage accrual compared with adult lupus? Rheum Dis Clin North Am 36: 53–80, vii–viii, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Osio-Salido E, Manapat-Reyes H: Epidemiology of systemic lupus erythematosus in Asia. Lupus 19: 1365–1373, 2010 [DOI] [PubMed] [Google Scholar]
- 5.Symmons DPM: Frequency of lupus in people of African origin. Lupus 4: 176–178, 1995 [DOI] [PubMed] [Google Scholar]
- 6.Tiffin N, Hodkinson B, Okpechi I: Lupus in Africa: can we dispel the myths and face the challenges? Lupus 23: 102–111, 2014 [DOI] [PubMed] [Google Scholar]
- 7.Pons-Estel GJ, Alarcón GS, Scofield L, Reinlib L, Cooper GS: Understanding the epidemiology and progression of systemic lupus erythematosus. Semin Arthritis Rheum 39: 257–268, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bastian HM, Roseman JM, McGwin G Jr, Alarcón GS, Friedman AW, Fessler BJ, Baethge BA, Reveille JD; LUMINA Study Group. LUpus in MInority populations: NAture vs nurture: Systemic lupus erythematosus in three ethnic groups. XII. Risk factors for lupus nephritis after diagnosis. Lupus 11: 152–160, 2002 [DOI] [PubMed] [Google Scholar]
- 9.Hanly JG, O’Keeffe AG, Su L, Urowitz MB, Romero-Diaz J, Gordon C, Bae S-C, Bernatsky S, Clarke AE, Wallace DJ, Merrill JT, Isenberg DA, Rahman A, Ginzler EM, Fortin P, Gladman DD, Sanchez-Guerrero J, Petri M, Bruce IN, Dooley MA, Ramsey-Goldman R, Aranow C, Alarcón GS, Fessler BJ, Steinsson K, Nived O, Sturfelt GK, Manzi S, Khamashta MA, van Vollenhoven RF, Zoma AA, Ramos-Casals M, Ruiz-Irastorza G, Lim SS, Stoll T, Inanc M, Kalunian KC, Kamen DL, Maddison P, Peschken CA, Jacobsen S, Askanase A, Theriault C, Thompson K, Farewell V: The frequency and outcome of lupus nephritis: results from an international inception cohort study. Rheumatology (Oxford) 55: 252–262, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Contreras G, Lenz O, Pardo V, Borja E, Cely C, Iqbal K, Nahar N, de La Cuesta C, Hurtado A, Fornoni A, Beltran-Garcia L, Asif A, Young L, Diego J, Zachariah M, Smith-Norwood B: Outcomes in African Americans and Hispanics with lupus nephritis. Kidney Int 69: 1846–1851, 2006 [DOI] [PubMed] [Google Scholar]
- 11.O’Shaughnessy MM, Montez-Rath ME, Lafayette RA, Winkelmayer WC: Patient characteristics and outcomes by GN subtype in ESRD. Clin J Am Soc Nephrol 10: 1170–1178, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hopkinson ND, Jenkinson C, Muir KR, Doherty M, Powell RJ: Racial group: Racial group, socioeconomic status, and the development of persistent proteinuria in systemic lupus erythematosus. Ann Rheum Dis 59: 116–119, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huong DL, Papo T, Beaufils H, Wechsler B, Blétry O, Baumelou A, Godeau P, Piette J-C: Renal involvement in systemic lupus erythematosus. A study of 180 patients from a single center. Medicine (Baltimore) 78: 148–166, 1999 [DOI] [PubMed] [Google Scholar]
- 14.Pons-Estel GJ, Catoggio LJ, Cardiel MH, Bonfa E, Caeiro F, Sato E, Massardo L, Molina-Restrepo JF, Toledano MG, Barile-Fabris LA, Amigo MC, Acevedo-Vásquez EM, Abadi I, Wojdyla D, Alarcón-Riquelme ME, Alarcón GS, Pons-Estel BA; GLADEL: Lupus in Latin-American patients: lessons from the GLADEL cohort. Lupus 24: 536–545, 2015 [DOI] [PubMed] [Google Scholar]
- 15.Feldman CH, Hiraki LT, Liu J, Fischer MA, Solomon DH, Alarcón GS, Winkelmayer WC, Costenbader KH: Epidemiology and sociodemographics of systemic lupus erythematosus and lupus nephritis among US adults with Medicaid coverage, 2000-2004. Arthritis Rheum 65: 753–763, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burgos PI, McGwin G, Pons-Estel GJ, Reveille JD, Alarcón GS, Vilá LM: US patients of Hispanic and African ancestry develop lupus nephritis early in the disease course: Data from LUMINA, a multiethnic US cohort (LUMINA LXXIV). Ann Rheum Dis 70: 393–394, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nee R, Martinez-Osorio J, Yuan CM, Little DJ, Watson MA, Agodoa L, Abbott KC: Survival Disparity of African American Versus Non-African American Patients With ESRD Due to SLE. Am J Kidney Dis 66: 630–637, 2015 [DOI] [PubMed] [Google Scholar]
- 18.Austin HA 3rd, Boumpas DT, Vaughan EM, Balow JE: High-risk features of lupus nephritis: importance of race and clinical and histological factors in 166 patients. Nephrol Dial Transplant 10: 1620–1628, 1995 [PubMed] [Google Scholar]
- 19.Reveille JD, Moulds JM, Ahn C, Friedman AW, Baethge B, Roseman J, Straaton KV, Alarcón GS: Systemic lupus erythematosus in three ethnic groups: I. The effects of HLA class II, C4, and CR1 alleles, socioeconomic factors, and ethnicity at disease onset. LUMINA Study Group. Lupus in minority populations, nature versus nurture. Arthritis Rheum 41: 1161–1172, 1998 [DOI] [PubMed] [Google Scholar]
- 20.Salmon JE, Millard S, Schachter LA, Arnett FC, Ginzler EM, Gourley MF, Ramsey-Goldman R, Peterson MG, Kimberly RP: Fc gamma RIIA alleles are heritable risk factors for lupus nephritis in African Americans. J Clin Invest 97: 1348–1354, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Korbet SM, Schwartz MM, Evans J, Lewis EJ; Collaborative Study Group: Severe lupus nephritis: racial differences in presentation and outcome. J Am Soc Nephrol 18: 244–254, 2007 [DOI] [PubMed] [Google Scholar]
- 22.Lin CP, Adrianto I, Lessard CJ, Kelly JA, Kaufman KM, Guthridge JM, Freedman BI, Anaya JM, Alarcón-Riquelme ME, Pons-Estel BA, Martin J, Glenn S, Adler A, Bae SC, Park SY, Bang SY, Song YW, Boackle SA, Brown EE, Edberg JC, Alarcón GS, Petri MA, Criswell LA, Ramsey-Goldman R, Reveille JD, Vila LM, Gilkeson GS, Kamen DL, Ziegler J, Jacob CO, Rasmussen A, James JA, Kimberly RP, Merrill JT, Niewold TB, Scofield RH, Stevens AM, Tsao BP, Vyse TJ, Langefeld CD, Moser KL, Harley JB, Gaffney PM, Montgomery CG; BIOLUPUS and GENLES Networks: Role of MYH9 and APOL1 in African and non-African populations with lupus nephritis. Genes Immun 13: 232–238, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Freedman BI, Langefeld CD, Andringa KK, Croker JA, Williams AH, Garner NE, Birmingham DJ, Hebert LA, Hicks PJ, Segal MS, Edberg JC, Brown EE, Alarcón GS, Costenbader KH, Comeau ME, Criswell LA, Harley JB, James JA, Kamen DL, Lim SS, Merrill JT, Sivils KL, Niewold TB, Patel NM, Petri M, Ramsey-Goldman R, Reveille JD, Salmon JE, Tsao BP, Gibson KL, Byers JR, Vinnikova AK, Lea JP, Julian BA, Kimberly RP; Lupus Nephritis–End‐Stage Renal Disease Consortium: End-stage renal disease in African Americans with lupus nephritis is associated with APOL1. Arthritis Rheumatol 66: 390–396, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bastian HM, Alarcón GS, Roseman JM, McGwin G Jr, Vilá LM, Fessler BJ, Reveille JD; LUMINA Study Group: Systemic lupus erythematosus in a multiethnic US cohort (LUMINA) XL II: factors predictive of new or worsening proteinuria. Rheumatology (Oxford) 46: 683–689, 2007 [DOI] [PubMed] [Google Scholar]
- 25.McCarty GA, Harley JB, Reichlin M: A distinctive autoantibody profile in black female patients with lupus nephritis. Arthritis Rheum 36: 1560–1565, 1993 [DOI] [PubMed] [Google Scholar]
- 26.Alarcón GS: Multiethnic lupus cohorts: what have they taught us? Reumatol Clin 7: 3–6, 2011 [DOI] [PubMed] [Google Scholar]
- 27.Tektonidou M, Dasgupta A, Ward M: Risk of end-stage renal disease in patients with lupus nephritis, 1970-2015: A systematic review and Bayesian meta-analysis. Arthritis Rheumatol 68:1432– 1441, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yap DYH, Tang CSO, Ma MKM, Lam MF, Chan TM: Survival analysis and causes of mortality in patients with lupus nephritis. Nephrol Dial Transplant 27: 3248–3254, 2012 [DOI] [PubMed] [Google Scholar]
- 29.Lerang K, Gilboe I-M, Steinar Thelle D, Gran JT: Mortality and years of potential life loss in systemic lupus erythematosus: a population-based cohort study. Lupus 23: 1546–1552, 2014 [DOI] [PubMed] [Google Scholar]
- 30.Bernatsky S, Boivin JF, Joseph L, Manzi S, Ginzler E, Gladman DD, Urowitz M, Fortin PR, Petri M, Barr S, Gordon C, Bae SC, Isenberg D, Zoma A, Aranow C, Dooley MA, Nived O, Sturfelt G, Steinsson K, Alarcón G, Senécal JL, Zummer M, Hanly J, Ensworth S, Pope J, Edworthy S, Rahman A, Sibley J, El-Gabalawy H, McCarthy T, St Pierre Y, Clarke A, Ramsey-Goldman R: Mortality in systemic lupus erythematosus. Arthritis Rheum 54: 2550–2557, 2006 [DOI] [PubMed] [Google Scholar]
- 31.Faurschou M, Dreyer L, Kamper AL, Starklint H, Jacobsen S: Long-term mortality and renal outcome in a cohort of 100 patients with lupus nephritis. Arthritis Care Res (Hoboken) 62: 873–880, 2010 [DOI] [PubMed] [Google Scholar]
- 32.Chen YE, Korbet SM, Katz RS, Schwartz MM, Lewis EJ; Collaborative Study Group: Value of a complete or partial remission in severe lupus nephritis. Clin J Am Soc Nephrol 3: 46–53, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Munroe ME, James JA: Genetics of Lupus Nephritis: Clinical Implications. Semin Nephrol 35: 396–409, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Niu Z, Zhang P, Tong Y: Value of HLA-DR genotype in systemic lupus erythematosus and lupus nephritis: a meta-analysis. Int J Rheum Dis 18: 17–28, 2015 [DOI] [PubMed] [Google Scholar]
- 35.Miyadera H, Ohashi J, Lernmark Å, Kitamura T, Tokunaga K: Cell-surface MHC density profiling reveals instability of autoimmunity-associated HLA. J Clin Invest 125: 275–291, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Miyadera H, Tokunaga K: Associations of human leukocyte antigens with autoimmune diseases: challenges in identifying the mechanism. J Hum Genet 60: 697–702, 2015 [DOI] [PubMed] [Google Scholar]
- 37.Chung SA, Brown EE, Williams AH, Ramos PS, Berthier CC, Bhangale T, Alarcon-Riquelme ME, Behrens TW, Criswell LA, Graham DC, Demirci FY, Edberg JC, Gaffney PM, Harley JB, Jacob CO, Kamboh MI, Kelly JA, Manzi S, Moser-Sivils KL, Russell LP, Petri M, Tsao BP, Vyse TJ, Zidovetzki R, Kretzler M, Kimberly RP, Freedman BI, Graham RR, Langefeld CD; International Consortium for Systemic Lupus Erythematosus Genetics: Lupus nephritis susceptibility loci in women with systemic lupus erythematosus. J Am Soc Nephrol 25: 2859–2870, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Raffler J, Friedrich N, Arnold M, Kacprowski T, Rueedi R, Altmaier E, Bergmann S, Budde K, Gieger C, Homuth G, Pietzner M, Römisch-Margl W, Strauch K, Völzke H, Waldenberger M, Wallaschofski H, Nauck M, Völker U, Kastenmüller G, Suhre K: Genome-Wide Association Study with Targeted and Non-targeted NMR Metabolomics Identifies 15 Novel Loci of Urinary Human Metabolic Individuality. PLoS Genet 11: e1005487, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tsai LJ, Hsiao SH, Tsai LM, Lin CY, Tsai JJ, Liou DM, Lan JL: The sodium-dependent glucose cotransporter SLC5A11 as an autoimmune modifier gene in SLE. Tissue Antigens 71: 114–126, 2008 [DOI] [PubMed] [Google Scholar]
- 40.Banchereau R, Hong S, Cantarel B, Baldwin N, Baisch J, Edens M, Cepika AM, Acs P, Turner J, Anguiano E, Vinod P, Kahn S, Obermoser G, Blankenship D, Wakeland E, Nassi L, Gotte A, Punaro M, Liu YJ, Banchereau J, Rossello-Urgell J, Wright T, Pascual V: Personalized Immunomonitoring Uncovers Molecular Networks that Stratify Lupus Patients. Cell 165: 551–565, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Villanueva E, Yalavarthi S, Berthier CC, Hodgin JB, Khandpur R, Lin AM, Rubin CJ, Zhao W, Olsen SH, Klinker M, Shealy D, Denny MF, Plumas J, Chaperot L, Kretzler M, Bruce AT, Kaplan MJ: Netting neutrophils induce endothelial damage, infiltrate tissues, and expose immunostimulatory molecules in systemic lupus erythematosus. J Immunol 187: 538–552, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hakkim A, Fürnrohr BG, Amann K, Laube B, Abed UA, Brinkmann V, Herrmann M, Voll RE, Zychlinsky A: Impairment of neutrophil extracellular trap degradation is associated with lupus nephritis. Proc Natl Acad Sci U S A 107: 9813–9818, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Birmingham DJ, Bitter JE, Ndukwe EG, Dials S, Gullo TR, Conroy S, Nagaraja HN, Rovin BH, Hebert LA: Relationship of Circulating Anti-C3b and Anti-C1q IgG to Lupus Nephritis and Its Flare. Clin J Am Soc Nephrol 11: 47–53, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pang Y, Yang XW, Song Y, Yu F, Zhao MH: Anti-C1q autoantibodies from active lupus nephritis patients could inhibit the clearance of apoptotic cells and complement classical pathway activation mediated by C1q in vitro. Immunobiology 219: 980–989, 2014 [DOI] [PubMed] [Google Scholar]
- 45.Gargiulo ML, Gómez G, Khoury M, Collado MV, Suárez L, Álvarez C, Sarano J: Association between the presence of anti-C1q antibodies and active nephritis in patients with systemic lupus erythematosus. Medicina (B Aires) 75: 23–28, 2015 [PubMed] [Google Scholar]
- 46.McKinney EF, Lee JC, Jayne DR, Lyons PA, Smith KG: T-cell exhaustion, co-stimulation and clinical outcome in autoimmunity and infection. Nature 523: 612–616, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Christopher-Stine L, Siedner M, Lin J, Haas M, Parekh H, Petri M, Fine DM: Renal biopsy in lupus patients with low levels of proteinuria. J Rheumatol 34: 332–335, 2007 [PubMed] [Google Scholar]
- 48.Fiehn C, Hajjar Y, Mueller K, Waldherr R, Ho AD, Andrassy K: Improved clinical outcome of lupus nephritis during the past decade: importance of early diagnosis and treatment. Ann Rheum Dis 62: 435–439, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rovin BH: Glomerular disease: Lupus nephritis treatment: are we beyond cyclophosphamide? Nat Rev Nephrol 5: 492–494, 2009 [DOI] [PubMed] [Google Scholar]
- 50.Song D, Wu LH, Wang FM, Yang XW, Zhu D, Chen M, Yu F, Liu G, Zhao MH: The spectrum of renal thrombotic microangiopathy in lupus nephritis. Arthritis Res Ther 15: R12, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hu W, Chen Y, Wang S, Chen H, Liu Z, Zeng C, Zhang H, Liu Z: Clinical-Morphological Features and Outcomes of Lupus Podocytopathy. Clin J Am Soc Nephrol 11: 585–592, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Singh AK, Ucci A, Madias NE: Predominant tubulointerstitial lupus nephritis. Am J Kidney Dis 27: 273–278, 1996 [DOI] [PubMed] [Google Scholar]
- 53.Weening JJ, D’Agati VD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, Balow JE, Bruijn JA, Cook T, Ferrario F, Fogo AB, Ginzler EM, Hebert L, Hill G, Hill P, Jennette JC, Kong NC, Lesavre P, Lockshin M, Looi L-M, Makino H, Moura LA, Nagata M: The classification of glomerulonephritis in systemic lupus erythematosus revisited. J Am Soc Nephrol 15: 241–250, 2004 [DOI] [PubMed] [Google Scholar]
- 54.Peterson KS, Huang JF, Zhu J, D’Agati V, Liu X, Miller N, Erlander MG, Jackson MR, Winchester RJ: Characterization of heterogeneity in the molecular pathogenesis of lupus nephritis from transcriptional profiles of laser-captured glomeruli. J Clin Invest 113: 1722–1733, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bethunaickan R, Berthier CC, Zhang W, Kretzler M, Davidson A: Comparative transcriptional profiling of 3 murine models of SLE nephritis reveals both unique and shared regulatory networks. PLoS One 8: e77489, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Parikh SV, Malvar A, Song H, Alberton V, Lococo B, Vance J, Zhang J, Yu L, Rovin BH: Characterising the immune profile of the kidney biopsy at lupus nephritis flare differentiates early treatment responders from non-responders. Lupus Sci Med 2: e000112, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Malvar A, Pirruccio P, Alberton V, Lococo B, Recalde C, Fazini B, Nagaraja H, Indrakanti D, Rovin BH: Histologic versus clinical remission in proliferative lupus nephritis [published online ahead of print August 6, 2015]. Nephrol Dial Transplant doi:10.1093/ndt/gfv296, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zickert A, Sundelin B, Svenungsson E, Gunnarsson I: Role of early repeated renal biopsies in lupus nephritis. Lupus Sci Med 1: e000018, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Alvarado AS, Malvar A, Lococo B, Alberton V, Toniolo F, Nagaraja HN, Rovin BH: The value of repeat kidney biopsy in quiescent Argentinian lupus nephritis patients. Lupus 23: 840–847, 2014 [DOI] [PubMed] [Google Scholar]
- 60.Kidney Disease Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group: Kidney Int Suppl 2: 139–274, 2012 [Google Scholar]
- 61.Parikh SV, Alvarado A, Malvar A, Rovin BH: The Kidney Biopsy in Lupus Nephritis: Past, Present, and Future. Semin Nephrol 35: 465–477, 2015 [DOI] [PubMed] [Google Scholar]
- 62.Hill GS, Delahousse M, Nochy D, Rémy P, Mignon F, Méry JP, Bariéty J: Predictive power of the second renal biopsy in lupus nephritis: significance of macrophages. Kidney Int 59: 304–316, 2001 [DOI] [PubMed] [Google Scholar]
- 63.Hill GS, Delahousse M, Nochy D, Tomkiewicz E, Rémy P, Mignon F, Méry JP: A new morphologic index for the evaluation of renal biopsies in lupus nephritis. Kidney Int 58: 1160–1173, 2000 [DOI] [PubMed] [Google Scholar]
- 64.Austin HA 3rd, Muenz LR, Joyce KM, Antonovych TA, Kullick ME, Klippel JH, Decker JL, Balow JE: Prognostic factors in lupus nephritis. Contribution of renal histologic data. Am J Med 75: 382–391, 1983 [DOI] [PubMed] [Google Scholar]
- 65.Alsuwaida A, Husain S, Alghonaim M, AlOudah N, Alwakeel J, ullah A, Kfoury H: Strategy for second kidney biopsy in patients with lupus nephritis. Nephrol Dial Transplant 27: 1472–1478, 2012 [DOI] [PubMed] [Google Scholar]
- 66.Bajaj S, Albert L, Gladman DD, Urowitz MB, Hallett DC, Ritchie S: Serial renal biopsy in systemic lupus erythematosus. J Rheumatol 27: 2822–2826, 2000 [PubMed] [Google Scholar]
- 67.Daleboudt GM, Bajema IM, Goemaere NN, van Laar JM, Bruijn JA, Berger SP: The clinical relevance of a repeat biopsy in lupus nephritis flares. Nephrol Dial Transplant 24: 3712–3717, 2009 [DOI] [PubMed] [Google Scholar]
- 68.Greloni G, Scolnik M, Marin J, Lancioni E, Quiroz C, Zacariaz J, De la Iglesia Niveyro P, Christiansen S, Pierangelo MA, Varela CF, Rosa-Diez GJ, Catoggio LJ, Soriano ER: Value of repeat biopsy in lupus nephritis flares. Lupus Sci Med 1: e000004, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Moroni G, Pasquali S, Quaglini S, Banfi G, Casanova S, Maccario M, Zucchelli P, Ponticelli C: Clinical and prognostic value of serial renal biopsies in lupus nephritis. Am J Kidney Dis 34: 530–539, 1999 [DOI] [PubMed] [Google Scholar]
- 70.Pagni F, Galimberti S, Goffredo P, Basciu M, Malachina S, Pilla D, Galbiati E, Ferrario F: The value of repeat biopsy in the management of lupus nephritis: an international multicentre study in a large cohort of patients. Nephrol Dial Transplant 28: 3014–3023, 2013 [DOI] [PubMed] [Google Scholar]
- 71.Ginzler EM, Bollet AJ, Friedman EA: The natural history and response to therapy of lupus nephritis. Annu Rev Med 31: 463–487, 1980 [DOI] [PubMed] [Google Scholar]
- 72.Costenbader KH, Desai A, Alarcón GS, Hiraki LT, Shaykevich T, Brookhart MA, Massarotti E, Lu B, Solomon DH, Winkelmayer WC: Trends in the incidence, demographics, and outcomes of end-stage renal disease due to lupus nephritis in the US from 1995 to 2006. Arthritis Rheum 63: 1681–1688, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Appel GB, Contreras G, Dooley MA, Ginzler EM, Isenberg D, Jayne D, Li L-S, Mysler E, Sánchez-Guerrero J, Solomons N, Wofsy D; Aspreva Lupus Management Study Group: Mycophenolate mofetil versus cyclophosphamide for induction treatment of lupus nephritis. J Am Soc Nephrol 20: 1103–1112, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Houssiau FA, Vasconcelos C, D’Cruz D, Sebastiani GD, Garrido Ed ER, Danieli MG, Abramovicz D, Blockmans D, Mathieu A, Direskeneli H, Galeazzi M, Gül A, Levy Y, Petera P, Popovic R, Petrovic R, Sinico RA, Cattaneo R, Font J, Depresseux G, Cosyns JP, Cervera R: Immunosuppressive therapy in lupus nephritis: the Euro-Lupus Nephritis Trial, a randomized trial of low-dose versus high-dose intravenous cyclophosphamide. Arthritis Rheum 46: 2121–2131, 2002 [DOI] [PubMed] [Google Scholar]
- 75.Rovin BH, Furie R, Latinis K, Looney RJ, Fervenza FC, Sanchez-Guerrero J, Maciuca R, Zhang D, Garg JP, Brunetta P, Appel G; LUNAR Investigator Group: Efficacy and safety of rituximab in patients with active proliferative lupus nephritis: the Lupus Nephritis Assessment with Rituximab study. Arthritis Rheum 64: 1215–1226, 2012 [DOI] [PubMed] [Google Scholar]
- 76.Parikh SV, Nagaraja HN, Hebert L, Rovin BH: Renal flare as a predictor of incident and progressive CKD in patients with lupus nephritis. Clin J Am Soc Nephrol 9: 279–284, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dooley MA, Jayne D, Ginzler EM, Isenberg D, Olsen NJ, Wofsy D, Eitner F, Appel GB, Contreras G, Lisk L, Solomons N; ALMS Group: Mycophenolate versus azathioprine as maintenance therapy for lupus nephritis. N Engl J Med 365: 1886–1895, 2011 [DOI] [PubMed] [Google Scholar]
- 78.Houssiau FA, Vasconcelos C, D’Cruz D, Sebastiani GD, de Ramon Garrido E, Danieli MG, Abramovicz D, Blockmans D, Cauli A, Direskeneli H, Galeazzi M, Gül A, Levy Y, Petera P, Popovic R, Petrovic R, Sinico RA, Cattaneo R, Font J, Depresseux G, Cosyns J-P, Cervera R: The 10-year follow-up data of the Euro-Lupus Nephritis Trial comparing low-dose and high-dose intravenous cyclophosphamide. Ann Rheum Dis 69: 61–64, 2010 [DOI] [PubMed] [Google Scholar]
- 79. Parikh SV, Rovin BH: Current and Emerging Therapies for Lupus Nephritis [published online ahead of print June 9, 2016]. J Am Soc Nephrol doi:10.1681/ASN.2016040415, 2016. [DOI] [PMC free article] [PubMed]
- 80.Dall’Era M, Levesque V, Solomons N, Truman M, Wofsy D: Identification of clinical and serological factors during induction treatment of lupus nephritis that are associated with renal outcome. Lupus Sci Med 2: e000089, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Austin HAI 3rd, Klippel JH, Balow JE, le Riche NGH, Steinberg AD, Plotz PH, Decker JL: Therapy of lupus nephritis. Controlled trial of prednisone and cytotoxic drugs. N Engl J Med 314: 614–619, 1986 [DOI] [PubMed] [Google Scholar]
- 82.ACCESS Trial Group: Treatment of lupus nephritis with abatacept: the Abatacept and Cyclophosphamide Combination Efficacy and Safety Study. Arthritis Rheumatol 66: 3096–3104, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Galbraith L, Manns B, Hemmelgarn B, Walsh M: The Steroids In the Maintenance of remission of Proliferative Lupus nephritis (SIMPL) pilot trial. Can J Kidney Health Dis 1: 30, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Naik A, Sharma S, Quigg RJ: Complement regulation in renal disease models. Semin Nephrol 33: 575–585, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Xiao H, Dairaghi DJ, Powers JP, Ertl LS, Baumgart T, Wang Y, Seitz LC, Penfold ME, Gan L, Hu P, Lu B, Gerard NP, Gerard C, Schall TJ, Jaen JC, Falk RJ, Jennette JC: C5a receptor (CD88) blockade protects against MPO-ANCA GN. J Am Soc Nephrol 25: 225–231, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Enia G, Catalano C, Misefari V, Salnitro F, Mundo N, Tetta C, Maggiore Q: Complement activated leucopenia during hemodialysis: effect of pulse methyl-prednisolone. Int J Artif Organs 13: 98–102, 1990 [PubMed] [Google Scholar]
- 87.Vollmer TL, Sorensen PS, Selmaj K, Zipp F, Havrdova E, Cohen JA, Sasson N, Gilgun-Sherki Y, Arnold DL; BRAVO Study Group: A randomized placebo-controlled phase III trial of oral laquinimod for multiple sclerosis. J Neurol 261: 773–783, 2014 [DOI] [PubMed] [Google Scholar]
- 88.Lourenço EV, Wong M, Hahn BH, Palma-Diaz MF, Skaggs BJ: Laquinimod delays and suppresses nephritis in lupus-prone mice and affects both myeloid and lymphoid immune cells. Arthritis Rheumatol 66: 674–685, 2014 [DOI] [PubMed] [Google Scholar]
- 89.Jayne D, Appel G, Chan TM, Mimrod D, Spiegelstein O, Barkay H, Weiss R, Wofsy D: The pharmacokinetics of laquinimod and mycophenolate mofetil during treatment of active lupus nephritis. Presented at the 2013 American Society of Nephrology Annual Meeting, Atlanta, GA, November 5–10, 2013 [Google Scholar]
- 90.Weng J, Lai P, Lv M, Lin S, Ling W, Geng S, Luo C, Liu X, Du X: Bortezomib modulates regulatory T cell subpopulations in the process of acute graft-versus-host disease. Clin Lab 59: 51–58, 2013 [DOI] [PubMed] [Google Scholar]
- 91.Dooley MA, Houssiau F, Aranow C, D’Cruz DP, Askanase A, Roth DA, Zhong ZJ, Cooper S, Freimuth WW, Ginzler EM; BLISS-52 and -76 Study Groups: Effect of belimumab treatment on renal outcomes: results from the phase 3 belimumab clinical trials in patients with SLE. Lupus 22: 63–72, 2013 [DOI] [PubMed] [Google Scholar]
- 92.Rovin BH, Dooley MA, Radhakrishnan J, Ginzler EM, Forrester TD, Anderson PW: The impact of tabalumab on the kidney in systemic lupus erythematosus: results from two phase 3 randomized, clinical trials [published online ahead of print, may 24, 2016]. Lupus doi:10.1177/0961203316650734, 2016 [DOI] [PubMed] [Google Scholar]
- 93.Gallagher KM, Lauder S, Rees IW, Gallimore AM, Godkin AJ: Type I interferon (IFN alpha) acts directly on human memory CD4+ T cells altering their response to antigen. J Immunol 183: 2915–2920, 2009 [DOI] [PubMed] [Google Scholar]
- 94.Jego G, Palucka AK, Blanck JP, Chalouni C, Pascual V, Banchereau J: Plasmacytoid dendritic cells induce plasma cell differentiation through type I interferon and interleukin 6. Immunity 19: 225–234, 2003 [DOI] [PubMed] [Google Scholar]
- 95.Rönnblom L, Alm GV, Eloranta ML: The type I interferon system in the development of lupus. Semin Immunol 23: 113–121, 2011 [DOI] [PubMed] [Google Scholar]
- 96.Tsuda K, Yamanaka K, Kitagawa H, Akeda T, Naka M, Niwa K, Nakanishi T, Kakeda M, Gabazza EC, Mizutani H: Calcineurin inhibitors suppress cytokine production from memory T cells and differentiation of naïve T cells into cytokine-producing mature T cells. PLoS One 7: e31465, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Liu Z, Zhang H, Liu Z, Xing C, Fu P, Ni Z, Chen J, Lin H, Liu F, He Y, He Y, Miao L, Chen N, Li Y, Gu Y, Shi W, Hu W, Liu Z, Bao H, Zeng C, Zhou M: Multitarget Therapy for Induction Treatment of Lupus Nephritis: A Randomized Trial. Ann Intern Med 162: 18–26, 2015 [DOI] [PubMed] [Google Scholar]
- 98.Mok CC, Ying KY, Yim CW, Siu YP, Tong KH, To CH, Ng WL: Tacrolimus versus mycophenolate mofetil for induction therapy of lupus nephritis: a randomised controlled trial and long-term follow-up. Ann Rheum Dis 75: 30–36, 2016 [DOI] [PubMed] [Google Scholar]
- 99.Jakes RW, Bae S-C, Louthrenoo W, Mok C-C, Navarra SV, Kwon N: Systematic review of the epidemiology of systemic lupus erythematosus in the Asia-Pacific region: prevalence, incidence, clinical features, and mortality. Arthritis Care Res (Hoboken) 64: 159–168, 2012 [DOI] [PubMed] [Google Scholar]