Abstract
OBJECTIVE
The objective of the study was to compare pelvic floor symptom changes in patients who continue vs discontinue pessary use, and determine whether changes predict pessary continuation.
STUDY DESIGN
Women fitted with pessaries completed the Pelvic Floor Distress Inventory-20 (PFDI-20) before and after initiating pessary use. Scores were compared in women who continued vs discontinued pessaries. Analysis of covariance adjusted for baseline differences in scores. Logistic regression and receiver operating characteristic curves were used to find a score predicting pessary continuation.
RESULTS
Sixty-four women had complete follow up data; at 6–12 months, 36 of 64 (56%) continued pessary use, and 28 of 64 (44%) discontinued use. The continuation group’s final PFDI-20 total, bladder, and prolapse scale scores were better than the discontinuation group’s. A 2-month prolapse score that fell to 50% of baseline best predicted pessary continuation.
CONCLUSION
PFDI-20 scores improved most in women continuing pessary use. Pessaries effectively treated urinary symptoms, and most effectively treated prolapse symptoms. Prolapse score improvement best predicted continued pessary use.
Keywords: prolapse, urinary incontinence
Pelvic organ prolapse and urinary incontinence are common problems affecting women. The demand for health services for these problems is projected to increase 45% by the year 2030.1 It is important to understand nonsurgical treatments for these diagnoses, given the potential morbidity and cost of surgical interventions.
Pessaries have been used since ancient times to conservatively treat pelvic floor disorders. Few prospective studies have evaluated pessaries’ use and effectiveness.2–4 Greater understanding of pessaries’ effect on quality of life and specific aspects of pelvic floor dysfunction, including urinary, prolapse, and defecatory symptoms, will help guide clinicians in their use. We evaluated symptom changes in women who continued to use pessaries for urinary incontinence and/or pelvic organ prolapse and compared these changes with women who discontinued pessary use.
Materials and Methods
This was a prospective, observational, cohort study approved by the Human Research Review Committee of the University of New Mexico Health Sciences Center. Women successfully fitted with pessaries for treatment of prolapse and/or urinary incontinence were eligible for participation. Written consent was obtained from all study subjects. Women were excluded from the study if they were younger than 18 years old, pregnant, non–English speaking, or unable to answer questionnaires because of cognitive impairment.
Women were recruited from a clinic dedicated to pessary fitting and follow-up at the University of New Mexico. Successful pessary fitting was defined as comfortable pessary placement and retention without difficulty voiding. Pessary fitting occurred at the initial clinic visit. The pessary was ordered for the patient at that visit. Patients returned 1 month later to receive their pessaries and pessary care instructions. The choice of pessary was left to the discretion of the provider. If patients complained of stress urinary incontinence, they were fitted with incontinence pessaries. Generally, women with incontinence had incontinence rings placed. If the incontinence ring was not well maintained, an incontinence dish was placed.
After successful pessary fitting but prior to receiving pessaries, patients completed the short form of the Pelvic Floor Disorders Impact Questionnaire (PFDI-20). The PFDI-20 is a validated, condition-specific questionnaire designed for women with pelvic support disorders.5 It is comprised of 3 scales; prolapse, bladder, and bowel. The PFDI-20 total score is the sum of these 3 scales.
In the PFDI-20, lower scores represent fewer symptoms and higher scores represent more symptoms. A lower PFDI-20 score in follow-up is therefore more desirable than a higher score. Analysis of covariance (ANCOVA) was used to compare PFDI scores between the discontinuation and continuation groups.
Patient characteristics, medical and surgical history, and physical examination information were recorded. Pelvic exams were described using the Pelvic Organ Prolapse Quantitation (POP-Q) system, the standard adopted by the International Continence Society.6 Patients were administered the PFDI-20 at 2, 6, and 12 months following the pessary fitting. In addition to answering the PFDI-20 at follow-up, patients were also queried whether they continued pessary use, and if not, why not. In response to the question, “Why did you stop using your pessary?” patients were given a preset list of reasons for discontinuing pessary use, including the following: (1) “It was uncomfortable”; (2) “It did not stay in well”; (3) “It caused urinary problems”; (4) “It caused discharge”; (5) “It was too much trouble to use it”; or (6) “other (please explain).” Patients were allowed to give more than 1 answer.
Pelvic floor symptom changes in the group of women who continued pessary use at 6–12 months were compared with the group of women who discontinued use. Patients were defined as continuing pessary use if they answered “yes” to the question, “Are you still using your pessary,” at their 6 and/or 12 month follow-up. Patients were defined as discontinuing pessary use if they answered “no” to the question at 2, 6, or 12 month follow-up. The last answer given by patients determined whether they were in the continue or discontinuation groups.
In the pessary discontinuation group, the questionnaire at time of pessary discontinuation was used if later questionnaire data were unavailable using the last observation carried forward method. If patients discontinued pessary use at 2 months but 6 or 12 month questionnaires were available, the later questionnaires were used. If patients discontinued pessary use at 2 months, but later questionnaires were unavailable, then the 2-month questionnaires were used.
Follow-up results for the pessary continuation group were the answers to the 6 or 12 month questionnaires. Twelve month questionnaire data were used if available. If unavailable, 6-month questionnaire data were used. Patients were considered lost to follow-up if they answered the initial questionnaire but did not answer the subsequent questionnaires or if they continued pessary use at 2 months but were lost thereafter.
Power analysis was performed before study initiation. Assuming an initial mean score based on previously published scores,5 a 20% difference between the follow-up scores of the 2 groups and assuming a 30% dropout rate from the study to attain an 80% power with α = 0.05, approximately 80 patients were needed for enrollment.
Demographic, history, and physical examination data were analyzed using Fisher’s exact test, Wilcoxon rank sum test, or Student t tests where appropriate. The PFDI-20 total and prolapse, bowel, and bladder scale results were analyzed using ANCOVA. We used ANCOVA to compare the groups to account for chance imbalances in the groups’ baseline scores.7 The least squares mean method was used to calculate a summary follow-up mean score for the 2 groups using regression methods. Changes in answers to individual PFDI-20 questions between baseline and follow-up were analyzed using McNemar’s test of symmetry. Significance for all tests was set at P < .05. Based on models chosen using stepwise logistic regression, we created individual receiver operator characteristic (ROC) curves for 2-month total and prolapse/bladder/bowel scale PFDI-20 scores. These were used to determine scores that best predicted pessary continuation at 6–12 months. Statistical analysis was performed using SAS/STAT (v 9.1, SAS Institute, Cary, NC, 2004).
Results
Eighty women were enrolled in this study from September 2004–January 2006. Of these, 16 had incomplete follow-up data. Of the 64 women with complete follow-up data, 36 (56%) continued pessary use and 28 (44%) discontinued use (Figure). The 16 patients missing follow-up information did not differ in demographic, historical, POP-Q information, or initial PFDI-20 results from the discontinuation and continuation groups (all P > .05).
FIGURE.
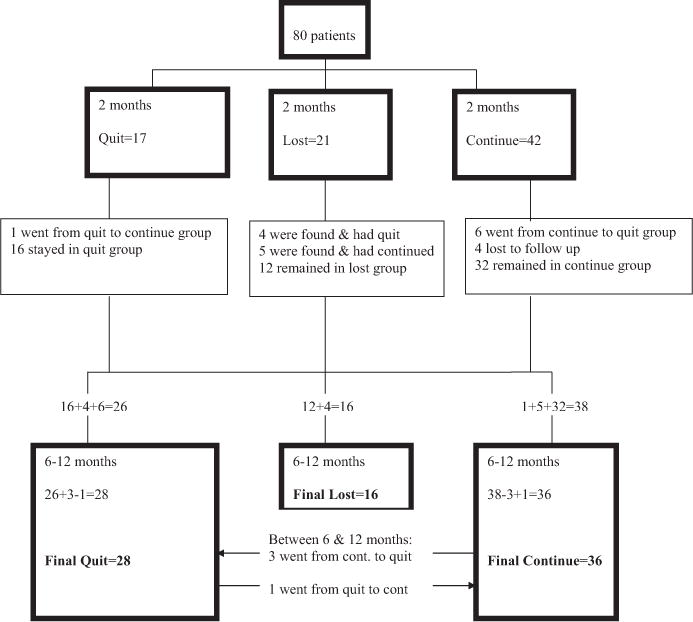
Study cohort
The 28 women who discontinued pessary use gave 51 reasons for pessary discontinuation. Most women discontinued pessary use because “it did not stay in well” (11 of 51 responses, 22%) or because “it was uncomfortable” (11 of 51 responses, 22%). Only 2 women who discontinued pessary use went on to have surgery.
The majority of women required only 1 pessary fitting (51 of 80, 66%), whereas a minority used 2 or three different pessaries (23 of 80, 34%). Having more than 1 pessary fitting was not associated with pessary continuation or discontinuation (P = .34), nor was it associated with final PFDI-20 scores using ANCOVA (P = .5). The most commonly used pessaries at final follow-up were ring pessaries (19 of 64, 30%) and incontinence dishes (20 of 64, 31%). The other pessaries used included incontinence rings (11 of 64, 17%), shaatz (4 of 64, 6%), gelhorns (4 of 64, 6%), rings with knobs (4 of 64, 6%), cubes (1 of 64, 2%), and gehrung pessaries (1 of 64, 2%). There was no difference between the pessaries used by the continuation and discontinuation groups (P = .124).
There were no differences between the histories of the 2 groups with regard to sexual activity, menopausal status, hormone replacement therapy, previous surgery, or other patient characteristics (Table 1). There were also no differences between the POP-Q examinations of the 2 groups using the Wilcoxon rank sum test (P > .05). The majority of patients in both groups had stage I prolapse of the apex and stage II prolapse of the anterior and posterior compartments. The majority of the women in both the pessary continuation and the discontinuation groups had stage II prolapse overall, with a mean POP-Q stage of 2.1 for the continuation group and 1.9 for the discontinuation groups (Table 1).
TABLE 1.
Patient characteristics and medical and surgical history
| Discontinued use (n = 28) | Continued use (n = 36) | P value | |
|---|---|---|---|
| Age ± SD (y) | 50.9 ± 11.1 | 53.1 ± 12.0 | .45* |
| Mean BMI ± SD (kg/cm2) | 30.3 ± 6.8 | 27.5 ± 5.3 | .09* |
| Parity (rank score) [mean] | (31.0) [mean, 2.2] | (34.5) [mean, 2.0] | .43† |
| Ethnicity (%) | .66‡ | ||
| White | 17 (61) | 25 (69) | |
| Hispanic | 8 (29) | 8 (22) | |
| Other | 3 (11) | 2 (6) | |
| Postmenopausal (%) | 15 (54) | 16 (44) | .61‡ |
| No hormone treatment | 10 (67) | 10 (63) | 1.0‡ |
| Sexually active (%) | 15 (54) | 23 (64) | .44‡ |
| Previous surgery (%) | |||
| Hysterectomy | 7 (25) | 9 (25) | All = 1.0‡ |
| Prolapse surgery | 1 (4) | 1 (3) | |
| Urinary incontinence | 1 (4) | 1 (3) | |
| POP-Q stage by compartment rank score [mean stage] | |||
| Anterior | 29.3 [mean, 1.8 ± 2.0] | 34.0 [mean, 2.0 ± 0.8] | .3† |
| Apex | 30.6 [mean, 1.3 ± 1.0] | 30.4 [mean, 1.2 ± 0.7] | 1.0† |
| Posterior | 27.6 [mean, 1.1 ± 0.9] | 33.7 [mean, 1.4 ± 0.8] | .1† |
| Overall POP-Q | 29.5 [mean, 1.9 ± 0.8] | 33.8 [mean, 2.1 ± 0.8] | .3† |
Two-sample t test (Satterthwaite unpaired t test).
Wilcoxon rank sum test.
Fisher’s exact test.
The 2 groups did manifest important differences in the total PFDI-20 scores. Although the scores of both groups fell at follow-up, the pessary continuation group’s PFDI-20 scores were significantly lower and had greater decline than the discontinuation group, indicating greater improvement in the continuation group (P < .001). The least squares mean final score for the pessary discontinuation group was 77.6 (95% confidence interval [CI], 64.4–90.9), representing a follow-up score that was 75% of baseline, whereas the continuation group’s score was 35.2 (95% CI, 24–46.5), representing a follow-up score that was 24% of baseline. The final PFDI-20 questionnaires used in the analysis for the 2 groups are summarized in Table 2.
TABLE 2.
Final (follow-up) PFDI-20 used for analysis
| Discontinue group (n = 28) |
Continue group (n = 36) |
|
|---|---|---|
| PFDI-20, 2 mo | 11 | 0 |
| PFDI-20, 6 mo | 11 | 17 |
| PFDI-20, 12 mo | 6 | 19 |
The groups differed in the PFDI-20 prolapse and bladder scales. Although both groups showed improvement in follow-up prolapse scores, compared with baseline, the continuation group had greater improvement than the discontinuation group (P < .001). In the discontinuation group, the prolapse follow-up score fell to 77% of baseline, whereas the continuation group’s follow-up score fell to 15% of baseline. The least squares mean follow-up prolapse score was 31.7 (95% CI, 25.5–37.8) for the pessary discontinuation group and 6.5 (95% CI, 1.3–11.8) for the continuation group, indicating a superior follow-up score for the continuation group.
Similarly, whereas the PFDI-20 bladder scores for both groups fell, the continuation group showed greater improvement than the discontinuation group. The continuation group’s least squares mean follow-up score was 17.5 (95% CI, 10.3–24.6), representing a follow-up score 24% of baseline, and the discontinuation group’s follow-up score was 34.5 (95% CI, 25.9–43.1), approximately 67% of baseline. Again, this indicates a superior follow-up score for the continuation group.
The bowel follow-up scores improved in both the pessary continuation and discontinuation groups falling to approximately 40% of the baseline scores. However, unlike the prolapse and bladder scales, there was no difference in improvement between the pessary continuation and the discontinuation groups’ follow-up bowel scores (P = .86).
Lastly, the discontinuation and continuation groups also differed in “yes” or “no” responses to individual questions (Table 3). Responses to 8 questions (4 prolapse, 1 bowel, and 3 bladder questions) improved at follow-up in the pessary continuation group. Two of the bladder questions that improved were stress related; the other was urge related or irritative.8 None of these 8 questions improved in the discontinuation group. In the discontinuation group, symptoms improved in response to only 1 question, a bowel question.
TABLE 3.
PFDI Individual questions that resolved on follow-up
| Question in PFDI-20 | Discontinued (n = 25)* or continued group (n = 34)* |
“Yes” at initial | “Yes” at 6–12 month follow-up |
P value† |
|---|---|---|---|---|
| Symptoms improved in pessary continuation group | ||||
|
| ||||
| 1. Do you usually experience pressure in the lower abdomen?‡ | Discontinued (%) | 14 (56) | 13 (52) | 1.00 |
| Continued (%) | 16 (47) | 3 (9) | < .01 | |
|
| ||||
| 2. Do you usually experience heaviness or dullness in the pelvic area?‡ | Discontinued (%) | 14 (56) | 11 (44) | .38 |
| Continued (%) | 16 (47) | 1 (3) | < .001 | |
|
| ||||
| 3. Do you usually have a bulge or something falling out that you can see or feel in the vaginal area?‡ | Discontinued (%) | 10 (40) | 10 (40) | 1.00 |
| Continued (%) | 23 (68) | 5 (15) | < .001 | |
|
| ||||
| 5. Do you usually experience a feeling of incomplete bladder emptying?‡ | Discontinued (%) | 17 (68) | 14 (56) | .38 |
| Continued (%) | 18 (53) | 5 (15) | < .001 | |
|
| ||||
| 11. Do you usually lose gas from your rectum beyond your control? | Discontinued (%) | 13 (52) | 10 (40) | .44 |
| Continued (%) | 20 (59) | 13 (38) | .04 | |
|
| ||||
| 15. Do you usually experience frequent urination?§(irritative) | Discontinued (%) | 20 (80) | 15 (60) | .06 |
| Continued (%) | 17 (50) | 9 (26) | .04 | |
|
| ||||
| 17. Do you usually experience urine leakage related to coughing, sneezing, or laughing?§(stress) | Discontinued (%) | 22 (88) | 20 (80) | .50 |
| Continued (%) | 22 (65) | 12 (35) | .01 | |
|
| ||||
| 18. Do you usually experience small amounts of urine leakage (ie, droops)?§(stress) | Discontinued (%) | 20 (80) | 17 (68) | .51 |
| Continued (%) | 20 (59) | 11 (32) | .01 | |
|
| ||||
| Symptoms improved in pessary discontinuation group | ||||
|
| ||||
| 12. Do you usually have pain when you pass your stool?‖ | Discontinued (%) | 7 (28) | 1 (4) | .03 |
| Continued (%) | 2 (6) | 1 (3) | 1.00 | |
Not all patients answered all baseline and follow-up questions.
McNemar’s test of symmetry.
Prolapse scale.
Bladder scale (stress, irritative).
Bowel scale.
Step-wise logistic regression and ROC curves identified the 2 month prolapse scale result to be the best predictor of pessary continuation. A prolapse score on 2-month follow-up, which was less than 50% of the baseline score, had an estimated area under an ROC curve equal to 0.77. This fall in the prolapse score predicted pessary continuation with 77% sensitivity and 73% specificity.
Comment
In our study, women who continued pessary use had greater than 70% improvement in their symptom questionnaire scores, significantly more improvement than women who discontinued pessary use. Although women who discontinued pessary use also had improvement in their scores, this improvement was more modest, possibly because of placebo effect or because of conservative interventions such as dietary change and pelvic floor exercise.
The improvement in pelvic floor symptom scores in women who continued to use pessaries in our study was in part because of improvement in the bladder scale scores. Symptoms in the PFDI-20 bladder scale can be classified as either stress or irritative.8 When individual questions were analyzed, we found that women who continued pessary use had improvement in both irritative and stress urinary questions, whereas women who discontinued use did not (Table 3). This contrasts with the findings of Fernando et al,4 who described improvement in irritative symptoms but not stress symptoms in pessary users. This difference may be partly explained by the different pessaries used in the studies. Fernando et al used ring, gelhorn, and cube pessaries. In contrast, our patients were also fitted with incontinence pessaries (those with knobs abutting the urethra) when appropriate. The incontinence pessaries may be more effective in treating stress urinary symptoms.
In addition to the improvement in bladder scale scores, the decline in the overall PFDI-20 scores among pessary users was driven by improvement in prolapse symptoms. The greatest difference between the scores in the continuation and discontinuation groups was in the prolapse scale. This scale, not the bladder scale, is the best predictor of pessary continuation. This finding is consistent with that of others who reported that prolapse is more commonly associated with pessary continuation than urinary incontinence.9 In our patients, we found that a 50% decline (improvement) in prolapse scale scores at 2 month follow-up is associated with pessary continuation. Thus, women who experience significant improvement in prolapse symptoms are much more likely to continue to use their pessaries.
Our findings are largely consistent with prior reports that found improvement in both prolapse and bladder symptoms with pessary use.3,4,10,11 Fernando et al4 also reported an improvement in bowel symptoms. However, that study did not include a comparison group of patients discontinuing pessary use. In our work we also compared PDFI-20 bowel scores of patients continuing to use pessaries with those who discontinued use. Whereas the scores in both groups improved, pessary use did not confer a significant advantage. This suggests that pessaries improve prolapse and bladder symptoms but have little effect on bowel symptoms. This underscores the importance of using a comparison group when interpreting quality-of-life data.
There were several limitations to this study. Despite multiple attempts by investigators to contact patients missing follow-up questionnaires, 20% of the patients were missing follow-up data. We attribute this follow-up rate to the mobile and socioeconomically disadvantaged nature of the population served by the University of New Mexico Health Sciences Center.
Obtaining follow-up data in our cohort was challenging. Because either 6 or 12 month data were missing in a number of subjects in the continuation group, we combined 6 to 12 month data as noted previously. Long-term follow-up was particularly difficult among patients who discontinued pessary use. Many of these patients were unwilling to answer questionnaires at 6 to 12 month follow-up because they were no longer using pessaries. We suspect, however, that the 6 and 12 month data in this group would show a rise in PFDI-20 scores toward baseline (a deterioration in quality of life), further accentuating the difference between the groups.
Additionally, the potential for selection bias exists in our study. Although the majority of women in our clinic are offered pessaries because the majority of women in our study had stage II prolapse, it is possible that women with more advanced prolapse are underrepresented in this study. Lastly, although we believe our identification of a predictor score for continued pessary use is potentially useful, this score was not applied to an independent patient group for validation.
This study’s strength is its success in demonstrating clinical utility of quality-of-life scores. It is a prospective, cohort study that offers a unique opportunity to correlate quality-of-life scores with an objective outcome, pessary continuation. This links quality-of-life measurements to an objective behavior, rather than relying on subjective measures.
In summary, total PFDI-20 symptom questionnaire scores improved most in women who continued pessary use. Pessaries were effective in treating urinary stress symptoms and were most effective in treating prolapse symptoms. Women who had PFDI-20 prolapse scores that declined by 50% at 2-month follow-up were most likely to continue pessary use at 6–12 months. Although it awaits validation, this last finding promises to aid decision making when treating patients with pessaries and is an example of how quality-of-life and symptom questionnaires might help shape clinical practice in the future.
Acknowledgments
We thank Dr. Ronald Schrader (University of New Mexico General Clinical Research Center) for his invaluable statistical support.
Supported in part by the Department of Health and Human Services, National Institutes of Health, and Grant 5M01 RR00997 from the Graduate Clinical Research Center, University of New Mexico.
Footnotes
Presented at the 33rd Annual Scientific Meeting of the Society of Gynecologic Surgeons, Orlando, FL, Apr. 12–14, 2007.
Reprints not available from the authors.
References
- 1.Luber KM, Boero S, Choe JY. The demographics of pelvic floor disorders: current observations and future projections. Am J Obstet Gynecol. 2001;184:1496–1503. doi: 10.1067/mob.2001.114868. [DOI] [PubMed] [Google Scholar]
- 2.Clemons JL, Aguilar VC, Sokol ER, Jackson ND, Myers DL. Patient characteristics that are associated with continued pessary use versus surgery after 1 year. Am J Obstet Gynecol. 2004;191:159–64. doi: 10.1016/j.ajog.2004.04.048. [DOI] [PubMed] [Google Scholar]
- 3.Barber MD, Walters MD, Cundiff GW. Responsiveness of the Pelvic Floor Distress Inventory (PFDI) and Pelvic Floor Impact Questionnaire (PFIQ) in women undergoing vaginal surgery and pessary treatment for pelvic organ prolapse. Am J Obstet Gynecol. 2006;194:1492–8. doi: 10.1016/j.ajog.2006.01.076. [DOI] [PubMed] [Google Scholar]
- 4.Fernando RJ, Thakar R, Sultan AH, Shah SM, Jones PW. Effect of vaginal pessaries on symptoms associated with pelvic organ prolapse. Obstet and Gynecol. 2006;108:93–9. doi: 10.1097/01.AOG.0000222903.38684.cc. [DOI] [PubMed] [Google Scholar]
- 5.Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7) Am J Obstet Gynecol. 2005;193:103–13. doi: 10.1016/j.ajog.2004.12.025. [DOI] [PubMed] [Google Scholar]
- 6.Bump RC, Mattiasson A, Bo K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175:10–7. doi: 10.1016/s0002-9378(96)70243-0. [DOI] [PubMed] [Google Scholar]
- 7.Vickers AJ, Altman DG. Analysing controlled trials with baseline and follow up measurements. BMJ. 2001;323:1123–4. doi: 10.1136/bmj.323.7321.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Uebersax JS, Wyman JF, Shumaker SA, et al. Short forms to assess life quality and symptom distress for urinary incontinence in women: the Incontinence Impact Questionnaire and the Urogenital Distress Inventory. Neurourol Urodyn. 1995;14:131–9. doi: 10.1002/nau.1930140206. [DOI] [PubMed] [Google Scholar]
- 9.Brincat C, Kenton K, FitzGerald MP, Brubaker L. Sexual activity predicts continued pessary use. Am J Obstet Gynecol. 2004;191:198–200. doi: 10.1016/j.ajog.2004.03.083. [DOI] [PubMed] [Google Scholar]
- 10.Clemons JL, Aguilar VC, Tillinghast TA, Jackson ND, Myers DL. Patient satisfaction and changes in prolapse and urinary symptoms in women who were fitted successfully with a pessary for pelvic organ prolapse. Am J Obstet Gynecol. 2004;190:1025–9. doi: 10.1016/j.ajog.2003.10.711. [DOI] [PubMed] [Google Scholar]
- 11.Donnelly MJ, Powell-Morgan S, Olsen AL, Nygaard IE. Vaginal pessaries for the management of stress and mixed urinary incontinence. Int Urogynecol J. 2004;15:302–7. doi: 10.1007/s00192-004-1163-7. [DOI] [PubMed] [Google Scholar]


