DYNAMISM
Medicine is a dynamic discipline, which has evolved to keep pace with changing requirements. These changes are fostered by modifications in our external environment, both physical and social, which in turn lead to drifts and shifts in the morbidity profile of humankind. Evolution of medical challenges is met by advances in science, which help us understand the etiology, pathogenesis, clinical features, and natural history of illness. This understanding stimulates research which creates newer methods of diagnosis and treatment, this helps limit a particular target disease.
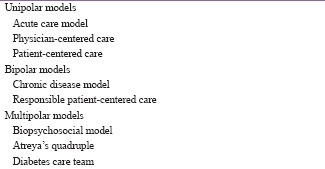
In parallel with these scientific growths, an equally remarkable development has taken place in the art of medicine [Box 1]. This development is new in semantics, yet ancient in origin; seemingly complex, yet intrinsically simple in its structure. It is considered difficult to teach, yet easy to share; tough to master, yet relaxing if internalized. We focus in this editorial on the relationship in the context of chronic disease management, specifically diabetes.
Box 1.
Evolution of diabetes care models
PHYSICIAN UNIPOLARITY
The traditional model of medical care is a physician centered one. Suited (perhaps) for the management of acute illness, it assumes a one-sided or unidirectional transfer of information and advice, from physician to patient. The patient is taken to be a passive participant in the process of health care.[1] Patient-centered care, too, can be criticized for being a unipolar construct as it focuses only on the needs, wishes, and attitudes of the patient.[2]
PATIENT PHYSICIAN DYAD
Changes in medical morbidity and emancipation of society gradually led to the creation of the chronic disease care model.[1] This model takes the patient and physician to be equally important partners on the road to health. It encourages a bidirectional sharing of ideas and thoughts, thus fostering information equipoise[3] and shared decision-making.[4] This facilitates concordance with each other's aim and achievement of mutually decided therapeutic targets. The framework of “diabetes therapy by the ear” has also evolved from a unidirectional to a bidirectional concept.[5] Similarly, unipolar patient-centered care has been replaced by a mutually respectful responsible patient-centered care paradigm,[6] which highlights the responsibility of the physician to ensure good health for the patient.
The human being is much more than a collection of various organ systems. Every individual has a unique personality and “psycho type,” which modulates his attitudes, wishes, and needs. This informs his or her healthcare-related behavior. No health-care intervention will be successful if these aspects are not taken into consideration. Thus, the psychological aspects of health and disease gained prominence in the chronic care model.
BIO PSYCHOSOCIAL TRIPTYCH
However, it is understood that the patient–physician dyad does not exist in isolation. The patient and physician as well as the health-care system, are a part of, and are influenced by society. This realization generated the biopsychosocial model,[7] which highlights not only the biomedical and psychological but also the social aspects of health. The biopsychosocial model is a supposedly “modern” concept, which has helped analyze and improve chronic disease.
ATREYA'S QUADRUPLE
The quadruple of Atreya,[8] postulated by the pioneer Ayurvedic Guru, predates these models by thousands of years. Atreya listed four determinants, which contribute equally to desired therapeutic outcomes. The success of clinical intervention is dependent on four variables: The patient, the physician, the drug, and the attendant. This quadruple is further qualified by four quadruplets, which list four desired qualities that each of these players must possess.
The Atreyan rubric is commendable for its farsightedness. By including both patient and physician as equal partners, it subsumes the chronic disease model of health care. Atreya lists “attendants,” which may be taken today to mean family members, nursing staff, paramedical workers, or the health-care system. Thus, it covers the concept of teamwork and suggests the importance of therapeutic patient education and peer support in diabetology. By involving nonphysician and nonpatient players, it also addresses the “social” component of the biopsychosocial triptych.
THE 3 × 3P RUBRIC
Modern society is much more complex than that which existed in Atreya's times. Various stakeholders, such as governments, nongovernmental organizations, pharmaceutical companies, and health insurance companies, play a role in determining diabetes care policies, priorities, practices, and procedures.
We propose a nine point framework, structured as a 3 × 3 table [Table 1], to include all these players. The nonagonal rubric lists patient, physician, partner (=family), paramedical staff, pharmaceutical (=drug), public (=society), policymaker (=government), payer (=insurance), and process (health-care system). While Atreya uses a quadruple to describe the factors which define health outcomes, the 3 × 3 model enumerates nine such factors, categorizing them into three clades. These include the person with diabetes, who is at the center of the model, her partner (family) and the public (society). This people-centric clade is supported by the physician, paramedical diabetes care professionals, and the health-care system (which we term “process” for alliterative purposes). These constituents of the “professional” clade are regulated by a third clade which includes the policymaker (government), payer (=insurance), and pharmaceutical sector (=drugs), termed the “parallel players.”
Table 1.
The 3×3 rubric: Active stakeholders in diabetes care
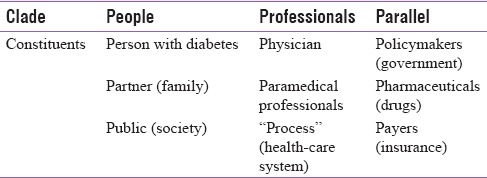
The 3 × 3P rubric provides an umbrella for all existing models and theories of chronic care, including diabetes care. The person with diabetes is listed in first place and shares her clade with her family and society. This underscores the importance of psychological and social factors in diabetes management and reinforces the relevance of the biopsychosocial model. It also reminds us that diabetes should be managed from a person-centered, family-oriented, and community-based viewpoint. The physician and other members of the diabetes care team are complemented by the “process” (or health-care system) in which they work. All three aspects of this clade work with each other to provide care to persons with diabetes. Achieving synergy and concordance between these players is the key to ensuring provision of optimal care.
Both patients and professionals, however, need assistance and support from external sources. These are listed in the third clade of the 3 × 3 rubric and include policymakers, drug manufactures, and payers. This clade provides a metonymic arch for the concepts of public-private partnership, health insurance for persons with diabetes, and social pharmacology. Proactive support from members of this “nonmedical” clade can help influence diabetes care in a positive way [Figure 1].
Figure 1.
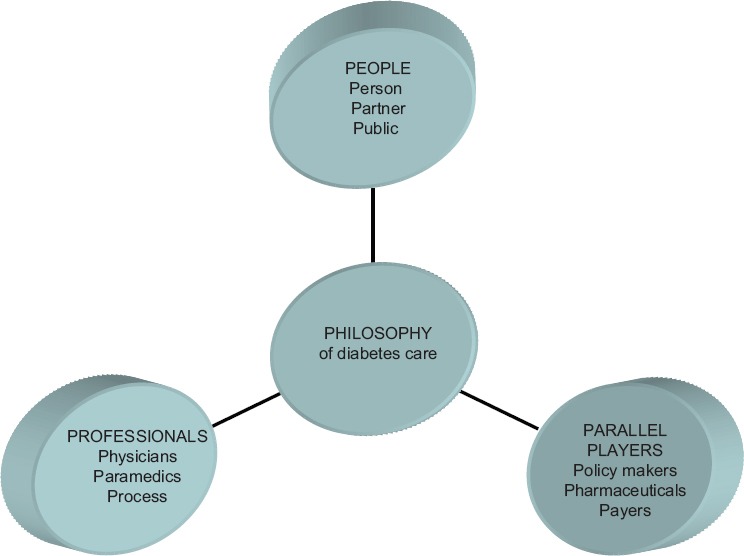
The 3 × 3P framework
SUMMARY
The philosophy of diabetes care has evolved over the last century. The future will witness developments in diabetology which cannot be foreseen. What can be predicted, however, with certainty, is that there is no single, and no simple, solution to the endemic. Multiple interventions, involving multiple stakeholders, will be required at multiple levels to address the situation. The 3 × 3P rubric provides a simple way of bringing all these together. The three clades, such as people, professionals, and parallel players, must work in concordance with each other, to reach a common goal: Health for all persons living with diabetes.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Runyan JW, Jr, Phillips WE, Herring O, Campbell L. A program for the care of patients with chronic diseases. JAMA. 1970;211:476–9. [PubMed] [Google Scholar]
- 2.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the Twenty-First Century. Washington: National Academy Press; 2001. [Google Scholar]
- 3.Kalra S, John M, Unnikrishnan AG. Glycemic equipoise. Indian J Endocrinol Metab. 2017;21:18–20. doi: 10.4103/2230-8210.194361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Charles C, Gafni A, Whelan T. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med. 1999;49:651–61. doi: 10.1016/s0277-9536(99)00145-8. [DOI] [PubMed] [Google Scholar]
- 5.Kalra S, Unnikrishnan AG, Baruah MP. Diabetes therapy by the ear. Indian J Endocrinol Metab. 2013;17(Suppl 3):S596–8. doi: 10.4103/2230-8210.123541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kalra S, Baruah MP, Unnikrishnan AG. Responsible patient centred care. Indian J Endocrinol Metab. 2017 doi: 10.4103/ijem.IJEM_543_16. In this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Engel GL. The clinical application of the biopsychosocial model. Am J Psychiatry. 1980;137:535–44. doi: 10.1176/ajp.137.5.535. [DOI] [PubMed] [Google Scholar]
- 8.Kalra S, Magon N, Malik S. Patient-centered care and therapeutic patient education: Vedic inspiration. J Midlife Health. 2012;3:59–60. doi: 10.4103/0976-7800.104451. [DOI] [PMC free article] [PubMed] [Google Scholar]


