Abstract
Background
This paper presents a case study of an automated clinical laboratory in a large urban academic teaching hospital in the North of Italy, the Spedali Civili in Brescia, where four laboratories were merged in a unique laboratory through the introduction of laboratory automation.
Materials and Methods
The analysis compares the preautomation situation and the new setting from a cost perspective, by considering direct and indirect costs. It also presents an analysis of the turnaround time (TAT). The study considers equipment, staff and indirect costs.
Results
The introduction of automation led to a slight increase in equipment costs which is highly compensated by a remarkable decrease in staff costs. Consequently, total costs decreased by 12.55%. The analysis of the TAT shows an improvement of nonemergency exams while emergency exams are still validated within the maximum time imposed by the hospital.
Conclusions
The strategy adopted by the management, which was based on re-using the available equipment and staff when merging the pre-existing laboratories, has reached its goal: introducing automation while minimizing the costs.
Significance for public health.
Automation is an emerging trend in modern clinical laboratories with a positive impact on service level to patients and on staff safety as shown by different studies. In fact, it allows process standardization which, in turn, decreases the frequency of outliers and errors. In addition, it induces faster processing times, thus improving the service level. On the other side, automation decreases the staff exposition to accidents strongly improving staff safety. In this study, we analyse a further potential benefit of automation, that is economic convenience. We study the case of the automated laboratory of one of the biggest hospital in Italy and compare the cost related to the pre and post automation situation. Introducing automation lead to a cost decrease without affecting the service level to patients. This was a key goal of the hospital which, as public health entities in general, is constantly struggling with budget constraints.
Key words: laboratory automation, direct and indirect costs, cost analysis, staff, equipment
Introduction
Clinical laboratories have rapidly evolved since the 1990s, mainly driven by technological advances that focus on automation.1,2 The level of automation depends on the needs and resources of laboratories, and the reasons for introducing automation vary on the basis of the application. Nowadays there is a consensus in the bioanalytical industry that automation in bioanalytical laboratories improves sample throughput and data integrity, shortens method development time and sample data turnaround time (TAT).2,3 Furthermore, laboratory services are an essential component of quality health-care delivery and require adequate space and equipment so that the quality of work and the safety of staff, patients, customers and visitors is not compromised. Clinical laboratories are potentially dangerous places because of biological hazards. Persons facing risk include laboratory staff, customers and visitors entering the laboratory environment. Introducing automation leads to a reduction of manipulation of biological sample by the staff, in particular sample transport, subsampling, analytical operations and waste management. Furthermore the automatic storage space maintain the integrity of samples and is adequately secured against unauthorized access. In addition to reducing occupational hazards, automation reduces tedious labour, employee turnover, allows reallocation of staff for growth and expansion and, in general, improves productivity.2,4
Consensus about the introduction of automation derives mainly from the fact that most of the studies performed till now evaluate TAT or outliers and clearly demonstrate the high contribution of automation to the improvement of these indicators.5,6 The TAT is commonly used as an indicator of the laboratory performance in terms of service level provided to patients. The TAT expected for each test result is usually agreed upon with users of the service and the laboratory must adhere to the agreement or advise the user of any delay. In addition, reducing the TAT also helps in reducing the average length of stay of patients in the hospital and the related costs.
Even though the study of these indicators is crucial, only few works exist that describe the economic advantage or disadvantage of turning to an automated laboratory. In our opinion, this is a further important factor to consider,7-9 since the sustainability of healthcare systems is a controversial issue, worldwide, as the annual increase in healthcare costs is unsustainable and the debate on strategies for reducing costs involves also laboratories. Furthermore, the increasing economic pressure has influenced the organization of laboratory activities and workflows, through the consolidation, merge and downsizing of existing institutions. All studies on health economics stress the importance of identifying new evaluation criteria for the performance of health institutions taking into account economic sustainability.
The case study presented in this paper is an example of decision driven by an economic sustainability objective. In fact, the management of the hospital decided to create a unified automated laboratory by merging four previous laboratories and re-using staff and equipment. This in contrast to most of the laboratories mentioned in the literature which are ex novo-automated laboratories. This means that generally the staff move to a new automated laboratory leaving old locals, analysers and contracts to a brandnew one. This strategy, that proved to be useful to improve the above mentioned indicators, could have a huge impact in terms of investments and costs for buying new analysers, making new contracts, and leaving contracts that are not yet expired. All these cost components should be considered when evaluating the cost per test8,10 and, consequently, the economic performance of the laboratory.
The analysis presented in this paper is aimed at showing the impact of the introduction of automation in the unified automated laboratory in Brescia, called Core-Lab from now on, both in terms of service level to patients (through the evaluation of TAT) and in terms of economic performance.
Design and Methods
The Spedali Civili in Brescia is one of the biggest hospital in Italy. It is a large urban academic teaching hospital, with 1650 beds, almost 70 thousands hospitalizations and more than 5 million ambulatory services in 2017. Staff is composed by more than 6 thousands units including managers, physicians, technicians, administrative and auxiliary staff. The Core-Lab acts as the main laboratory of the hospital, processing the majority of the exams requested by the hospital and by external ambulatories belonging to the same organization or by other organizations. It processes on average 3 thousands tubes per day. Thus, our analysis is representative of the impact of automation on big laboratories. The Core-Lab was introduced with the aim of joining four previously existing laboratories towards a more automated (and hopefully more efficient) system with particular attention to costs. The previous laboratories were located in different areas of the hospital with dedicated analysers and staff, processing different types of exams and with different opening times. When the management decided to introduce the unified laboratory, the strategy adopted was based on reusing, as much as possible, the equipment available and, consequently, the contracts with the corresponding companies providing the equipment and the materials. Moreover, a further goal was to offer a 24h service, with at least one technician and one physician always on duty. The study presented in this paper was conducted in 2016.
Analysers and staff
The Core-Lab was introduced in August 1st, 2015 and merged four previously existing laboratories performing the following activities: clinical chemistry, haematology, coagulation and immunometry. Before the introduction of the Core-Lab the different laboratories were open from 7 am to 4:50 pm (from Monday to Friday), and from 7 am to 1 pm on Saturday with dedicated technical staff and physicians. An exception was the emergency laboratory that was open 24h a day and was mainly handled by technical staff. During night and holidays one technician was on service and one physician on call. With the introduction of the Core-Lab, the staff previously engaged in the four laboratories, which was composed by 23 full time equivalent (FTE) physicians, 56.4 FTE technicians plus two coordinators, 10.3 FTE auxiliary personnel, converged in the unified laboratory.
The structure of the four pre-existing laboratories together with the corresponding equipment is shown in Figure 1. The red rectangles represent the four pre-existing laboratories while the blue ones form the unified automated laboratory. We also report the equipment of the pre-existing laboratories in the red rectangles.
Figure 1.
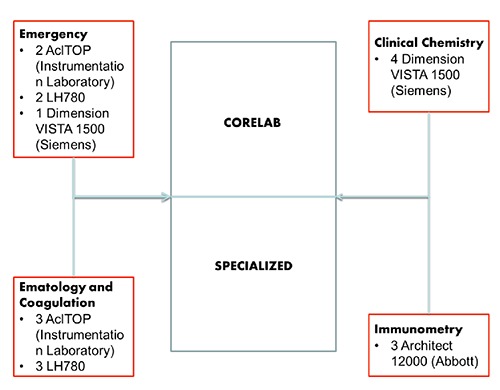
Pre- and post-automation structure of the laboratories.
The four laboratories were merged in a single laboratory composed of two areas: the Core-Lab, which corresponds to the analyser connected to the INPECO conveyor belt and on which we focus our analysis, and a specialized area with stand-alone equipment and dedicated technician staff. Auxiliary personnel and physician were involved in both areas of the laboratory.
Since the aim of the management was to move to automation by reusing, as much as possible, the analysers previously available in the pre-existing laboratories, most of them were reutilized and integrated in the Core-Lab. The resulting equipment of the Core-Lab is: one MUT HCTS2000 MK2 (Medical System) and one TECAN FE500 (Medical System) for preanalitical sorting. The preexisting four Dimension Vista 1500 (Siemens Health Care), three Acl TOP (Instrumental laboratories), three Architect (Abbott) were integrated with a Flex-Lab chain with an Input Output Module, Bulk Input Module, two centrifuges and one refrigerator to stock (Impeco) to constitute the Core-Lab and one work cell, made up by three DXH800 (Beckman Coulter) and a DXH800 stand-alone, for the specialized area. Since the Core-Lab uses the same analysers and materials used in the previous laboratories, there was no penalty for giving back the useless instruments in excess. At present, the type of exams proposed, the number of exams performed, the analysis methods, and number of tubes per patient are the same as in the pre-Core-Lab situation. Most of the exams that were previously performed on the four laboratories are now carried out in the Core-Lab. The exams that are not performed on the Core-Lab (because they are not performed on the analyzers that are part of the Core-lab) are processed on specific sectors of the unified laboratory with stand-alone instruments and dedicated staff that remained unvaried compared to the pre-Core-Lab situation and will not be considered in our analysis. The convergence on the Core-Lab raised the necessity of a redistribution of the staff to guarantee the presence of at least one physician and two technicians to cover the 24h service. Concerning the technical staff, of the 56.4 FTE previously employed in the four laboratories, 28.5 FTE were assigned to the activities that converged in the Core-Lab and will be considered in our analysis. The remaining ones are assigned to the specialized area. Concerning physicians, all off the 23 FTE are involved in the urgent care to guarantee the presence of at least one of them in the 24h. Thus, all the 23 FTE physicians are considered in our analysis, even if most of them are still responsible of analysis not included in the Core-Lab. Scheduled time for auxiliary staff has not changed.
Cost analysis
We consider the costs charged to the cost centre corresponding to the Core-Lab, both direct and indirect. As far as direct costs, we consider two terms: equipment and staff costs. The equipment costs are given by the monthly renting rates, while the staff costs are the monthly salary. The indirect costs are formed by two components. The first one, which is called indirect costs, is a fixed percentage of the sum of the equipment and staff costs and is equal to 4.6%. This term takes into account all minor costs related to the management of the laboratories. The second term, called general costs, is the 13.95% of the sum of direct and indirect costs as described above. This term amounts to the part of general managing and fixed cost of the hospital charged to the single centre of costs. Both percentages were provided from the hospital central administration, as well as equipment and staff costs.
Before presenting the results of our analysis, we would like to point out that we did not consider material costs in our analysis. In fact, the number of tubes and exams processed remained constant with respect to the pre-Core-Lab situation. This situation will change in the next future since when the unified laboratory will reach the long-term stable process routine. At present, it is still in a set-up phase where a number of issues are faced with a high frequency. These issues have an important impact on material costs. Thus, we leave the analysis of material cost for a future work.
Results
Analysers and staff
From the equipment point of view, given that the strategy adopted was based on reusing the already existing equipment and contracts, the status remained almost unchanged when moving to the Core-Lab. In particular, when considering the analysers only, the equipment cost of the pre-existing laboratories was slightly reduced, as shown in s 2 that highlights a decrease of monthly equipment costs related to coagulation (800€) and clinical chemistry (2750€). Costs related to immunometry remained stable while there was an increase in costs related to haematology (2050€). This last increase is due to the introduction of a specific total laboratory automation (TLA) dedicated to haematology. In order to better evaluate how the equipment cost is spread among the different areas involved in the Core-Lab, we determined the weight of the equipment cost with respect to the total for each area in the pre-Core-Lab and Core-Lab situation. We obtained that weight of haematology increased from 18% to 45%, clinical chemistry decreased from 62% to 41%, coagulation decreased from 12% to 5% and immunometry has a slight increase from 8% to 9%.
When considering the global equipment costs which involve, in addition to machinery costs, the cost related to the analyser that were connected to the conveyor belt and the cost of the preanalytic equipment, we obtain that the total cost of the pre-Core-Lab situation is €14950 while it increases to €20450 with the introduction of Core-Lab. This increase is due to the introduction of the conveyor belt and the corresponding management software in addition to the cost of the newly introduced preanalytic equipment.
When moving to the comparison in terms of staff involvement, we obtain the situation depicted in Table 1. From Table 1 we observe a reduction in total staff cost of €51,681.07, which corresponds to 14.64% of the staff cost of the pre-Core-Lab situation. We point out that the decrease in the staff composition (technicians and physicians) was achieved even if the same number of tubes and exams are processed with respect to the pre-Core-Lab situation. In addition, a 24h service is now guaranteed. Finally, even if most of the work done by this auxiliary staff have been substituted by preanalytical equipment, this area remained stable up to now and will be analysed in the future.
Table 1.
Comparison of staff costs.
| Pre-core-lab | Core-lab | |||
|---|---|---|---|---|
| Units | Monthly cost, € | Units | Monthly cost, € | |
| Technicians | 28.5 | 100,495.07 | 22.83 | 80,501.84 |
| Physicians | 23 | 215,906.37 | 20 | 187,744.67 |
| Auxiliary staff | 10.3 | 29,445.13 | 10.3 | 29,445.13 |
| Technician coordinators | 2 | 7052.29 | 1 | 3526.14 |
| Total | 63.8 | 352,898.86 | 54.13 | 301,217.78 |
Total cost
Moving to the comparison of the total costs, including equipment costs, staff costs and indirect costs, we obtain what is shown in Table 2.
Table 2.
Comparison of total costs.
| Pre-core-lab | Core-lab | |
|---|---|---|
| Direct costs, € | ||
| Equipment | 14,950.00 | 20,450.00 |
| Staff | 352,898.86 | 301,217.78 |
| Total | 367,848.86 | 321,667.78 |
| Indirect costs (4.61% of direct costs), € | 16,954.05 | 14,825.82 |
| General costs (13.95% of direct +indirect costs), € | 53,680.01 | 46,940.82 |
| Total, € | 438,482.91 | 383,434.18 |
Total costs decreased by €55,048.73 which corresponds to 12.55% of the total cost of the pre-Core-Lab situation.
Performance
We now report the analysis of the TAT for emergency, urgent and routine exams. The TAT is the time elapsed from the check in of the tube in the laboratory to the time of delivery of the laboratory clinical report. The hospital has established maximum validation times (measured by TAT): 1 hour for emergency exams, 2 hours for urgent and 1 day for routine. To have the most complete and realistic picture of the Core-Lab performance we report the average TAT for three classes of exams that require different methodology. In particular we analyse sodium, which is one of the most requested exams, performed with direct potentiometry on Dimension vista 1500. We performed the same analysis for potassium but we do not report the results as they are identical. In addition, we report emergency TAT for Troponin I (immune assay) which is often requested in emergency exams, and finally we evaluate colorimetric method by analysing urgent and routine TAT for glucose confirming that they were all on time. The results are shown in Figure 3 which shows, on the vertical axis, the average value of TAT for the month reported on the horizontal axis while the vertical axis reports time in minutes. We report data for the pre-automation period (July 2014 – June 2015) and the first year of Core-lab (July 2015 – June 2016). The figure show that the behaviour of TAT is very similar when comparing sodium with tro-ponin I for emergency exams or sodium with glucose for urgent and routine exams. In particular, there was a slight increase in emergency TAT, which however is still below 1 hour and has improved in the last period. For urgent and routine exams TAT improved quite remarkably. We note that the up-down behaviour of the routine graph is due to outliers whose analysis was not a goal of our study.
Figure 3.
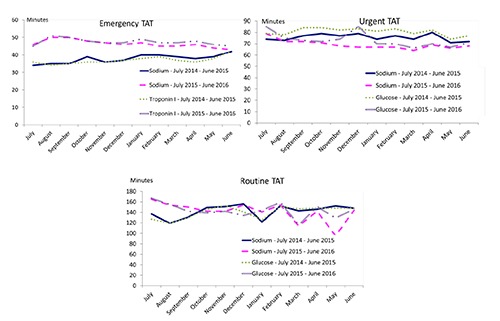
Analysis of turnaround time.
In addition to the previous analysis, we compared the Core-Lab situation with the pre-Core-Lab situation and also, using the eValuate software provided by Gene.sys (www.gene-sys.it),10 with the situation of a set of Italian laboratories by analysing, as shown in Figure 4, the differences in terms of FTE per number of tests. The horizontal axis in the figure reports the number of tests processed per year, while the vertical axis reports the FTE. The figure shows that the same number of tests is now provided with a smaller amount of FTE. Moreover, the Core-Lab can be classified as a big laboratory, as most of the other laboratories in the figure perform a much smaller number of tests.
Figure 4.
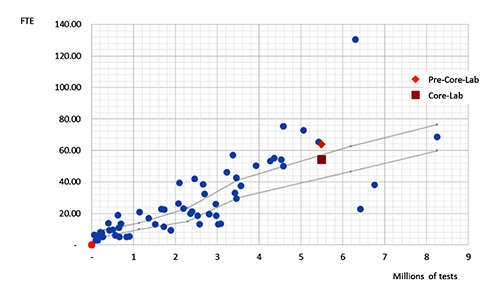
Comparison with other Italian laboratories in terms of full time equivalent per volume.
Conclusions
This paper presents a cost analysis related to the introduction of an automated laboratory in one of the biggest hospital in Italy. Our analysis shows that the introduction of the laboratory automation, which permitted to merge four pre-existing laboratories, lead to important cost savings mainly in terms of staff costs, without affecting the TAT, and thus the service level to patients, even considering the short operative period which included all setup issues. This allows to state that the management strategy, with the goal of introducing automation while minimizing the corresponding costs, has been successfully achieved.
Since the strategy adopted was based on reusing most of the already existing equipment and contracts, integrating with few analysers and the pre analytical machines, the status remained almost unchanged when moving to the Core-Lab. In particular, when considering only the analysers, the equipment cost of the pre-existing laboratories was slightly reduced. The reduction of costs is due to the reduction in the number of analysers used, thanks to the fact that most of the analysis performed in the different laboratories were converged in a unified laboratory. In addition, thanks again to the convergence, there was no need for all the backup analysers that were used in the previous laboratories. This happened in particular for coagulation and clinical chemistry. The only costs that increased are those related to haematology due to the introduction of a specific new total laboratory automation (TLA). When considering the global equipment costs which involve also the conveyor belt and the preanalitical equipment that was not present in the pre-Core-Lab, and therefore was acquired ex novo, costs increase.
Regarding staff, we observed a reduction of almost 15% in total staff cost. We would like to recall that the Core-Lab offers a 24h service and the reduction in total staff cost was achieved even though there was the need for medical staff to be present 24h a day and validate all exams, while this was not the case before when only one technician was present 24h. Furthermore, thanks to the consolidation, there was no need to recruit new medical staff in order to replace the 3 FTE who left (for layoffs and retirements). For the technical staff, a decrease in the number of technicians, from 28.5 FTE to 22.8 FTE, was achieved to perform the same number of tests. This happened thanks to consolidation of activities. At present, it is required that at least two technicians are always on duty: one is in the group of technicians that were previously engaged in the emergency laboratory and thus has more experience when dealing with all kind of exams and emergency treatment. The second may be one that was previously engaged on a routine laboratory, and thus with less experience. This strategy will be revised in the future when a sufficient experience will be acquired by all technicians and, as a consequence, only one technician will be on duty during the night. This will further reduce the staff cost. The only area that remained stable is the area of auxiliary staff, even if we believe that most of the work done by this staff have been substituted by preanalytical equipment. Once operative work flow becomes stable and all set-up problems are solved, there will likely be an important reduction in auxiliary staff too.
One important aspect to be highlighted is that, differently from most of the other works described in the literature where staff moves to a new automated system leaving old analysers in the old spaces, instrument were moved to the new space in few days and there was no interruption of service during relocation of the reuti-lized analysers. This happened thanks to the efficient schedule of the reallocation of analysers and staff. Furthermore, staff was trained in advance to help the transition. This is an important aspect especially when dealing with emergency exams whose delay could seriously affect patients safety and, as a consequence, have legal consequences. Clearly, as emerged from the TAT analysis, the months just after the reallocation of the laboratories suffered anyway a bit as a consequence of transition. However, the TAT always satisfied the constrains established by the hospital.
As expected there has been a decrease in staff cost and an increase in equipment cost since automation leads to an investment in new equipment (even if marginal like in the case of Spedali Civili) which, in turn, allows to reduce the staff involved in the operational management of the laboratory.
As shown by the analysis of the TAT, the service level to patients did not deteriorate despite the cost decrease, as the TAT of the analysis we measured was in time with what agreed in the pre-Core-Lab situation. This is an important aspect, as a fast response is a key factor for an early diagnosis and a proper disease treatment and, also, the respect of TAT avoid risk of extra hospital operating costs related to a postponed diagnosis. By comparing the FTE per number of tests of the pre and post automation situation, we note an improvement, i.e., a decrease of FTE per test. This is probably the consequence of the consolidation of activities in a single laboratory. Moreover, the Core-Lab compares favourably with other big Italian laboratories as it requires on average a lower number of FTE per tests processed.
Finally, we would like to emphasize what stated previously, i.e., the strategy that the management of the hospital adopted when deciding to introduce the automation. Automated laboratories has been introduced in many other hospitals before, as witnessed by the large number of papers devoted to their analysis5,7,11 and by the experience of hospitals located also in the county of Brescia. However, in most cases the aim was to focus on the performance of new automated laboratory, either in terms of reduction of TAT or prevention of outliers.6,12 In the case of the Core-Lab of Brescia, the focus was on the minimization of costs. Our analysis showed that this goal has been achieved. Further improvements may be implemented in a longer term, especially related to reduction in auxiliary and technical staff. Moreover, a more efficient scheduling of the activities on the conveyor belt could further improve the performance of the laboratory, both in terms of costs and TAT. Anyway, to the best of our knowledge, our experience is the first one where the focus has been on cost effectiveness. As suggested by Maynard,13 given the universal scarcity of resources, economic recession and austerity, the absence of a marriage of strategies between public health and economic needs makes prioritisation of competing investments impossible. We believe that our analysis goes in the direction of achieving this marriage.
Figure 2.
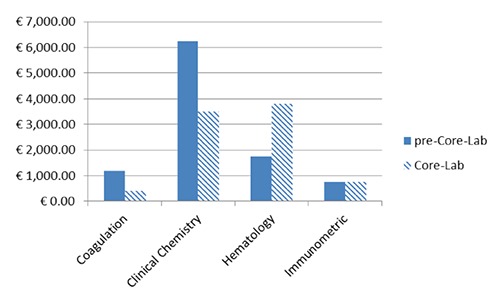
Comparison of equipment cost: absolute values.
References
- 1.Zaninotto M, Plebani M. The Hospital Central Laboratory: automation, integration and clinical usefulness. Clin Chem Lab Med 2010;48:911-7. [DOI] [PubMed] [Google Scholar]
- 2.Hawker CD. Laboratory automation: total and subtotal. Clin Lab Med 2007;27:749-70. [DOI] [PubMed] [Google Scholar]
- 3.Peck-Palmer OM. Total lab automation takes teamwork. MLO Med Lab Obs 2009:30-5. [PubMed] [Google Scholar]
- 4.Plebani M. Laboratory diagnostics in the third millennium: where, how and why. Clin Chem Lab Med 2010;48:901-2. [DOI] [PubMed] [Google Scholar]
- 5.Ialongo C, Porzio O, Giambini I, Bernardini S. Total automation for the core laboratory: improving the turnaround time helps to reduce the volume of ordered STAT tests. J Lab Autom 2016;21:451-8. [DOI] [PubMed] [Google Scholar]
- 6.Li M. Automation in the bioanalytical laboratory: what is the future? Bioanalysis 2013;5:2859-61. [DOI] [PubMed] [Google Scholar]
- 7.Angeletti S, De Cesaris M, Hart JG, et al. Laboratory automation and intra-laboratory turnaround time: experience at the University Hospital Campus Bio-Medico of Rome. J Lab Autom 2015;20:652-8. [DOI] [PubMed] [Google Scholar]
- 8.Lippi G, Mattiuzzi C. Testing volume is not synonymous of cost, value and efficacy in laboratory diagnostics. Clin Chem Lab Med 2013;51:243-5. [DOI] [PubMed] [Google Scholar]
- 9.Barletta G, Zaninotto M, Faggian D, Plebani M. Shop for quality or quantity? Volumes and costs in clinical laboratories. Clin Chem Lab Med 2013;51:295-301. [DOI] [PubMed] [Google Scholar]
- 10.Barletta G, Nese S, Becciolini S, Plebani M. Healthcare is a giant with feet of clay. Diagnosis. [In Press] [DOI] [PubMed] [Google Scholar]
- 11.Allinson JL, Blick KE, Cohen L, et al. Ask the experts: automation: part I. Bioanalysis 2013;5:1953-62. [DOI] [PubMed] [Google Scholar]
- 12.Yuan L, Ji QC. Automation in new frontiers of bioanalysis: a key for quality and efficiency. Bioanalysis 2012;4:2759-62. [DOI] [PubMed] [Google Scholar]
- 13.Maynard A. Public health and economics: a marriage of necessity. J Public Health Res 2012;1:11-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


