Abstract
In a patient-centered care era, rehabilitation can benefit from researcher-clinician collaboration to effectively and efficiently produce the interdisciplinary science that is needed to improve patient centered outcomes. The authors propose use of the Forging Alliances in Interdisciplinary Rehabilitation Research (FAIRR) logic model to provide guidance to rehabilitation scientists and clinicians who are committed to growing their involvement in interdisciplinary rehabilitation research. We describe the importance and key characteristics of the FAIRR model for conducting interdisciplinary rehabilitation research.
Keywords: interdisciplinary, rehabilitation, interdisciplinary research, researcher-clinician collaboration
INTRODUCTION
Rehabilitation relies on strong, productive interdisciplinary teams of scientists and clinicians from rehabilitation professions1. This reliance stems from the assumption that no single discipline can adequately solve major problems in rehabilitation2, whether they be related to understanding the functional consequences of an individual’s physical status (e.g., obesity, chronic conditions)3,4, improving health outcomes and access to care (e.g., disparities in birth outcomes and contributing maternal risk factors)5,6, or assessing for patient-reported outcomes of functioning (e.g., participation in activities)7,8. Rather, scientists and clinicians both have important, distinct roles to play in making scientific discoveries that can advance evidence for rehabilitation professions to improve patient centered outcomes9. However, rehabilitation research initiatives that leverage the expertise of clinicians and rehabilitation scientists are lacking2,10.
To date, efforts to increase the research capacity of interdisciplinary rehabilitation scientists have included: 1) international meetings and summits2; 2) the creation of organizations (e.g., Disability and Rehabilitation Research Coalition) and training mechanisms (e.g., K12 and T32 training grants, Training in Grantsmanship for Rehabilitation Research (TIGRR)); and 3) papers emphasizing a call to action for advancing rehabilitation research10-14. Similarly, primary and allied health professions have made a commitment to interdisciplinary practice. The Institute of Medicine recommended working in interdisciplinary teams (IDT) as one of five core competencies for all health care professionals15. Colleges and universities are also prioritizing opportunities for collaborative learning and scholarship in their curricula16,17. Clinical expertise and discipline specific skill training naturally lead to professional boundaries and controversies for enacting evidence-based practice in rehabilitation18. Therefore, training for effective partnerships within interdisciplinary clinical teams is now considered a core component of emerging educational frameworks for 21st century health care professionals19,20. Guidelines for successful interdisciplinary clinical partnerships among health care professionals focus on clear communication and common terminology, respect for and understanding of individual roles and expertise, identification of mutual goals, conflict resolution and assessment of group dynamics, accurate and timely dissemination of information among team members, and processes for coordinated and integrated care21. A wealth of literature has highlighted how communication styles influence collaborative partnerships22,23. However, a paucity of information exists on the importance of selecting potential research collaborators, what is communicated in an authentic interdisciplinary research partnership, and how information might be disseminated among partnering researchers and clinicians.
Efforts have been made to train rehabilitation clinicians and scientists to each individually contribute to interdisciplinary teams. Yet, few mechanisms guide clinicians and scientists as they actually engage in interdisciplinary work, or cross trained research clinicians who simultaneously assume both roles throughout scientific study. Despite this gap, there are multiple factors contributing to ripe conditions for advancing interdisciplinary rehabilitation research. Funding agencies and academic institutions are rewarding authentic scientist-clinician interdisciplinary scholarship17,24,25.
Professional organizations and institutions are developing tangible mechanisms to help advance their contributions to interdisciplinary rehabilitation research. For example, the American Occupational Therapy Association (AOTA), the American Occupational Therapy Foundation (AOTF) (the professional organization representing the interests and concerns of occupational therapy practitioners, and the scientific organization supporting occupational therapy research, respectively), and the Foundation for Physical Therapy (the scientific organization supporting physical therapy research) have made efforts to increase interdisciplinary research capacity26. When unified by a common question, scientists and clinicians from multiple disciplines have increased capacity to answer that question, and advance rehabilitation research23.
Challenges, however, do exist that make the task of developing interdisciplinary research collaborations with scientist and clinician engagement easier said than done. The task is particularly challenging in two situations: 1) when scientists and clinicians are establishing research careers, and 2) when scientists or clinicians are establishing a new collaboration to broaden their research portfolio. There is critical need for guidelines to help rehabilitation scientists, clinicians, and cross trained research clinicians in systematically building productive interdisciplinary research collaborations.
The purpose of this paper is two-fold: 1) to examine benefits and challenges of building productive interdisciplinary teams that include rehabilitation clinicians and scientists working together, and 2) to introduce a logic model that can be systematically used as a roadmap to forge alliances in interdisciplinary rehabilitation research (FAIRR) that is inclusive of authentic scientist-clinician partnerships for improved scientific outcomes. Previous literature on the topic of interdisciplinary research has focused on a call to action2,20, the use of an interdisciplinary approach to education27 or an implementation of interdisciplinary collaborations as it applies to practice28. This paper is unique in introducing a new model that can be used by clinicians and researchers from multiple disciplines who are prepared to engage in interdisciplinary rehabilitation research.
CLARIFYING TERMS IN INTERDISCIPLINARY REHABILITATION RESEARCH
While rehabilitation scientists have a strong interdisciplinary tradition, a challenge has been the use of terms that appear to be synonymous with interdisciplinary work (e.g., multidisciplinary). Therefore, it is imperative to define the meaning of interdisciplinary and multidisciplinary research and identify our interpretation of the differences between them. Interdisciplinary research refers to multiple clinicians (e.g., OT, PT, MD, MSW, RN) and scientists (e.g., PhD, ScD) or clinician scientists (e.g., OT, ScD) from two or more disciplines who collaborate together guided by shared language and multiple practice frameworks or intersecting theoretical models, to develop and implement a shared research agenda. Throughout the research process, relevant terminology, conceptual designs, and methodological approaches to data collection and analysis from participating disciplines are valued, shared, and integrated, and research findings are disseminated using common language in joint publications.
In contrast, multidisciplinary research typically involves several clinicians and researchers from various disciplines working together with one discipline, often with most expertise in the health condition under study or area of inquiry, assuming a dominant role and setting the research agenda. Hence, clinicians and scientists offer their individual expertise but remain within their professional boundaries by contributing distinct components to the project, and team members disseminate findings in discipline specific or condition specific journals. Therefore, research objectives are related but not unified, and terminology is not shared among all members of the research team18,29.
Some teams may begin and remain interdisciplinary or multidisciplinary. However, teams may use more than one of these approaches at one point in time or shift from one approach to another in pursuit of a line of research. For example, an interdisciplinary team of researchers may conduct a project with a multidisciplinary component to focus on one area of expertise. In contrast, a team may initially be assembled to conduct a multidisciplinary research project, and then discover that the results of the initial project feed into the design of an interdisciplinary project with jointly developed aims and methods.
FAIRR LOGIC MODEL FOR INTERDISCIPLINARY REHABILITATION RESEARCH
Scientists who are establishing or expanding their research portfolio may find it challenging to create an interdisciplinary rehabilitation research team. One aspect of the challenge is that learning how to reach out to non-university-based partners (e.g., community organizations) is not always a formal part of scientific training20. In turn, non-university-based organizations may be more accustomed to seeking partnerships with similar organizations rather than with university-based groups20.
We suggest the use of a logic model that we (the authors) have constructed and used to build and sustain an interdisciplinary research career trajectory that supports scientist-clinician partnerships. Our logic model, Forging Alliances in Interdisciplinary Rehabilitation Research (FAIRR) (Figure 1A-E) has the following goals: 1) to provide investigators a framework to systematically build interdisciplinary research teams that engage both scientists and clinicians, 2) to create an awareness of the benefits and obstacles faced when harnessing expertise to build an interdisciplinary research team, and 3) to formalize less transparent aspects of constructing an interdisciplinary research career that are as critical as conducting sound research.
Figure 1.
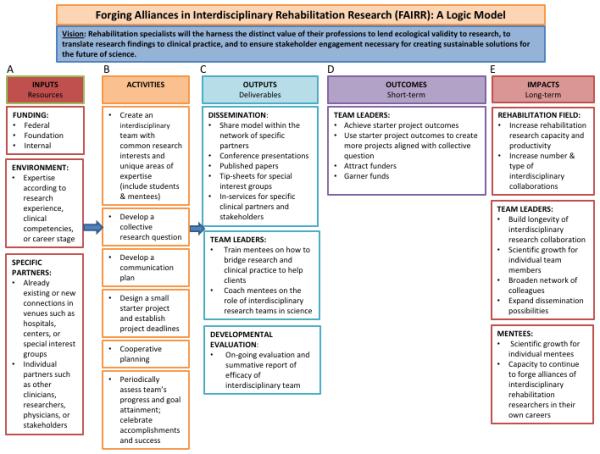
Forging Alliances in Interdisciplinary Rehabilitation Research (FAIRR) logic model. This figure delineates components of the FAIRR model, which include inputs (A), activities (B), outputs (C), outcomes (D), and impacts (E).
In this next section, we introduce components of the FAIRR model and illustrate how these components have been operationalized in the context of three interdisciplinary research projects. These interdisciplinary research collaborations range in scope from improving early intervention (EI) outcomes research using new patient-reported outcome (PRO) measures (Figure 2), to web-based technology interventions for minimizing preconception health risks among African American women (Figure 3), to engaging health economics and informatics expertise to advance big data research for EI program improvement (Appendix).
Figure 2.
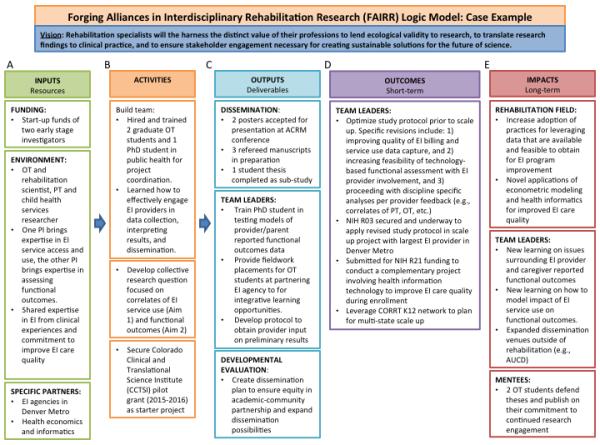
Case Example 1 of the Forging Alliance in Interdisciplinary Rehabilitation Research (FAIRR) logic model. This figure illustrates the components of the FAIRR model when applied to an interdisciplinary research collaboration to advance early intervention outcomes research using patient-reported outcome (PRO) measures. ACRM = American Congress of Rehabilitation Medicine; AUCD = Association of University Centers on Disabilities; CORRT = Comprehensive Opportunities in Rehabilitation Research Training; EI = Early Intervention; PT = Physical Therapy; OT = Occupational Therapy
Figure 3.
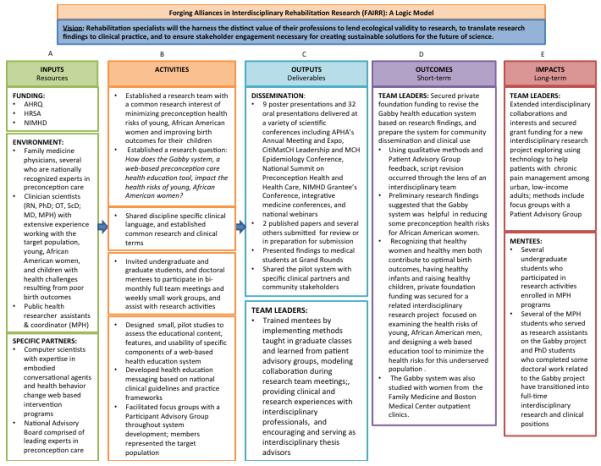
Case Example 2 of the Forging Alliance in Interdisciplinary Rehabilitation Research (FAIRR) logic model. This figure illustrates the components of the FAIRR model when applied to an interdisciplinary research collaboration focused on preconception care among African American women. AHRQ = Agency for Healthcare Research and Quality; HRSA = Health Resources and Services Administration; NIMHD = National Institute on Minority Health and Health Disparities; RN = Registered nurse; PhD = Doctor of Philosophy; OT = Occupational Therapy or Occupational Therapist; ScD = Doctorate of Science; MD = Medical Doctor; MPH = Master’s of Public Health; MCH = Maternal and Child Health; APHA = American Public Health Association; NIMHD = National Institute on Minority Health and Health Disparities
FAIRR INPUTS AND CONSIDERATIONS PRIOR TO GETTING STARTED
The first part of the FAIRR logic model includes inputs (Figure 1A). Inputs are resources that are needed before formalizing the interdisciplinary team and engaging in research activities (Figure 1B). Common examples include funding, the research environment, and specific research partners from two or more disciplines. It is important to identify, assess, and secure selected inputs before expecting productivity from the interdisciplinary team.
When exploring potential partners as potential inputs researchers and clinicians should not only consider their own contributions, but what other potential collaborators can offer to an integrated research team. Researchers and clinicians should also appraise their own internal biases, goals, commitment to scientific inquiry, and prior experience working on a team. They should be prepared to explore these topics with potential partners and negotiate institutional support for the proposed collaboration. Identifying, acknowledging, trusting, and listening to potential team members’ unique expertise is critical to establishing mutual respect among new team members1. In addition, initially highlighting the distinct competencies of each team member allows for pairing areas of weakness for some investigators with strengths from others28. For example, one potential collaborator may be skilled in grantsmanship while another may be an astute experimentalist, or potential collaborators may have expertise in different research methodologies.
Along with appraising collaborator contributions, team members can assess external expertise needed to enhance their research. Expert senior scholars or clinicians can provide ad hoc advice to the team. The team can determine when and how this advice is provided, whether informally (e.g., ad hoc discussions with senior researchers or clinicians) or formally (e.g., an advisory board of researchers and clinicians constructed like those built into grant proposals to the National Science Foundation or National Institutes of Health K12 grant mechanisms).
As conducting interdisciplinary rehabilitation research requires a high level of sustained commitment and a collaborative character, it is important to choose partners carefully. In choosing collaborators, balancing compatibility of character (e.g., common goal and commitment) and communication style can be as important as choosing individuals based on their areas of expertise. There are different perspectives and pedagogy between disciplines towards professional collaboration, and these learned norms may impact professional socialization and value of interdisciplinary research. Therefore, regardless of professional affiliation, it may best to search for collaborators who display three characteristics: flexibility of thought, open mindedness, and critical thinking28. Interdisciplinary team members must possess these characteristics to challenge the limits of their own professional norms, explore and envision alternate explanations, and value the knowledge learned across professional boundaries30.
Former graduate school classmates or post-doctoral fellows may be good collaborators because of shared interests and a history of character compatibility, work ethic, and communication style. Cross trained clinician scientists may also be good partners. If considering adding unfamiliar researchers to the interdisciplinary team, it is helpful to seek the input of others or to interact casually with researchers prior to inviting them to collaborate. For example, colleagues may have insight as to the researcher’s projects or whether the researcher is known for being a difficult collaborator. Initiating an informal meeting with potential clinical collaborators also allows an opportunity to explore common research interests and get a sense for work ethic, character, and communication style fit. Researchers creating teams must also consider how all collaborators will work with one another. Although one collaborator may work well with the researcher that initiated the team, that same collaborator may not work well with others in the group.
FAIRR ACTIVITIES
A second component of the FAIRR logic model involves activities (Figure 1B). Activities are practical steps that can be taken to achieve outputs, outcomes, and impacts. In the context of a productive interdisciplinary collaboration, we intend for FAIRR to minimize challenges inherent in building interdisciplinary teams by outlining specific activities that improve long-term research productivity. For example, team members may have different communication and work styles, however, achieving shared expectations around what is communicated and how information is shared throughout the research process is important. Therefore, an facilitating effective communication plan may first involve asking about team members’ preferred form of communication; some members may prefer to communicate via email and others may require frequent face-to-face communication. It is also helpful if researchers are direct about how they best work. For example, some researchers may thrive if mini-deadlines and frequent meetings are created rather than a longer deadline and a more inclusive meeting agenda scheduled months away.
An overarching research question built on shared research interests is the foundation of the interdisciplinary team. However, beginning with a mammoth project such as redefining a theory may be too large of a task to accomplish at the start of a new collaboration. Chiseling away at a big question with pilot research projects, small grant proposals, or systematic reviews, allows the team to collaborate while settling into their respective roles and learning how to best work together. Starting small may also include beginning with a small team (e.g., one or two other researchers) rather than starting with a large team. However, the size of the group will ultimately depend upon the research agenda and scope of work.
Once a small project is selected, short and long term deadlines are created, interdisciplinary teams collectively plan how to achieve common goals, and identify the team members and leaders involved. Cooperative planning is vital to the integrity and productivity of interdisciplinary teams. For instance, a principal investigator may be eager to achieve a goal set by the team and make decisions without the team’s consent. When faced with participant enrollment challenges, the research coordinator and senior research associate may collaboratively revise recruitment strategies. When a submitted manuscript is rejected, the lead author may decide to resubmit the manuscript to another journal without consulting with co-authoring team members. Besides ensuring voice and respect among all team members, cooperative planning often facilitates professional growth by revealing new avenues not familiar to individual team members (e.g., adding recruitment sites unknown to some team members or submitting to a new journal not previously considered). Cooperative planning creates clear expectations and roles for decision-making providing the necessary framework for team members to meet deadlines and work towards common goals. When it is clear who is responsible for various decisions throughout the research process, it is easier to voice disagreements with the shared research agenda and methodological decisions. This can help avoid misunderstandings about research activities and quell conflicts between team members leading to a more sustainable, productive, long-term partnership.
Acknowledging that interdisciplinary collaboration involves work is key. Along the way, team members should periodically assess the team’s progress, recognize when project goals are attained, and celebrate research accomplishments to help maintain commitment to the research team. Assessing program involves periodically reviewing whether the research activities align with the original goals, and whether the team members still share the same goals. This process would be facilitated by the principal investigator, designated project leader, or via informal or formal advice from senior participating researchers or clinicians. Team members committed to continuing the interdisciplinary team should ensure that the researchers involved wish to maintain a unified research agenda. Members may consider revising the goals, forming multidisciplinary collaborations, or working with new researchers. At times, it may be appropriate to disband the team following completion of the small, starter project, which should be prioritized over lack of productivity due to decreased interest among the members.
FAIRR OUTPUTS: EXPECTED DELIVERABLES
A third component of our FAIRR logic model includes outputs: deliverables that team members can expect based on their inputs and activities (Figure 1C). Interdisciplinary research teams consist of scientists, clinicians, and clinician scientists from multiple disciplines working toward a unified goal. However, they may be faced with dissemination venues that are not interdisciplinary. Therefore, team members should determine up front whether they will target journals or conferences reflecting their individual disciplines, interdisciplinary journals, or a combination. Submitting to journals within team members’ disciplines requires balancing lead authorship and responsibilities among team members. An occupational therapy team member may serve as lead author on a manuscript for the American Journal of Occupational Therapy, whereas a physical therapy team member may be lead author on a paper for the Physical Therapy Journal. If there are two research labs contributing, then collaborators might take turns with lead authorship roles. Targeting interdisciplinary journals means devising a common language among team members.
Where and when to publish is often dictated by team members’ attempts to balance multiple agendas (e.g., institutional expectations and cultures). For instance, early stage investigators may chose discipline-specific journals for fear of losing discipline specific language or not being credited with scientific impact for promotion purposes. This is a completely valid approach. However, publishing in an interdisciplinary journal can be an exciting opportunity for the team to share their collective visions with their colleagues. In addition, opportunities to disseminate one’s research via interdisciplinary venues can help early stage investigators validate their scientific impact in a major area.
FAIRR: OUTCOMES
A fourth aspect of the FAIRR logic model includes outcomes (Figure 1D). To ensure the longevity and sustainability of the interdisciplinary research team, it is necessary for the team to achieve a positive working environment and scientific goals associated with the initial project. The main results of the project can be used as preliminary data for grant proposals. The team’s scientific success on a starter project can also be documented in grant proposals to convince a funding agency that this team has the infrastructure needed to ensure rigor and efficiency. In both ways, the shared success of a starter project can lead to deliverables that attract potential funders and lead to the team’s ability to garner larger research awards.
FAIRR: IMPACTS
The final part of the FAIRR model includes impacts (Figure 1E). The FAIRR model may help clinicians and researchers create collaborations that influence the rehabilitation field, build long-lasting partnerships that enhance rehabilitation research, and create a climate for mentees to become successful researchers. Despite a difficult funding climate, pooling resources by creating interdisciplinary teams can be advantageous. Decreasing funding rates make sustaining large, individual research programs less feasible. For example, in 2005 at the National Institutes of Health (NIH), 27.6% of grant applicants received funding, but funding rates dropped to 17.5% of funded applications in 2013. However, the likelihood of obtaining funding may increase with a group of researchers interested in tackling larger questions and increased venues for grant submissions reflecting each discipline. Along with expanding funding venues, organizations are creating opportunities for interdisciplinary grant proposals (e.g., the NIH Building Interdisciplinary Research Team Revision Awards). Interdisciplinary funding opportunities are not limited to federal grant agencies. Foundations (e.g., the American Occupational Therapy Foundation) and internal grant mechanisms (e.g., the Boston University Coulter Translational Partnership) offer chances for interdisciplinary teams to apply for funding. Federal, foundation, and internal grant mechanisms are available and target specific career stages such as K-awards, which further expands funding opportunities. From a rehabilitation science perspective, a competitive proposal requires building interdisciplinary teams with contributing clinicians translating research findings into evidence-based practice. Internal funding mechanisms can be used to pay for clinicians’ time as part of their workload or to fund students. Federal and foundation funds can also be used to pay clinicians as consultants or co-investigators or to fund student mentees who or post-doctoral fellows.
CASE APPLICATIONS OF THE FAIRR MODEL
The FAIRR model may be applicable to a broad range of rehabilitation research initiatives. For example, Figure 2 depicts a new research collaboration, whereby an occupational therapist and rehabilitation scientist with expertise in outcomes measurement pairs up with a physical therapist and child health services researcher with expertise in large data research. They have distinct areas of expertise but share clinical interests in early intervention (EI) program improvement based on their prior experiences providing EI services. Hence, they embarked on a collaboration to advance PRO uptake for improved EI outcomes research. To do this, they obtained a pilot grant to test the feasibility of linking electronic administrative and functional outcomes data to examine correlates of EI service use and outcomes. By starting small, they invested in building an equitable academic-community partnership to optimize their study protocol. They learned how to work effectively with EI staff to convert administrative data from paper to electronic form and enroll families in technology-based functional outcomes data collection during service visits. Graduate students completed their research and clinical training with the partnering EI agency, resulting in sub-study opportunities to enhance project deliverables. They co-developed a dissemination plan document to plan their dissemination efforts with EI provider and student involvement. These initial successes contributed to their decision to continue collaboration with an NIH R03 scale-up study that is now underway. In a complementary line of inquiry, one of the collaborators is leading efforts to further build this research team to improve methods for conducting large data research specific to early intervention (see Appendix).
As another example, Figure 3 depicts an interdisciplinary research collaboration between an occupational therapist with expertise in qualitative methods, health behavior change and health management routines among African American families, and a family medicine physician with expertise in quantitative methodology, and health behavior change among women and individuals with chronic illness. They collaboratively developed components of a web-based intervention designed to assess preconception health risks among African American women and offer culturally tailored interventions to minimize them. Both collaborators identify as research clinicians and share a common interest in minimizing factors that contribute to health risks in young, African American women. The collaborators identified several components of the larger web-based system to collaboratively develop, including scripts for the physical activity module as well as nutrition and stress reduction. They were able to share and integrate each profession’s theoretical models around health behavior change and frameworks for patient-centered care into scripts that motivated users to adopt physical activity routines. The scripts not only made recommendations based on national clinical guidelines which physicians often reference29, but considered the environmental factors, personal preferences, and performance skills that occupational science suggest impact decisions around engagement in activities including physical activity30. This initial collaboration led to continued collaboration on other aspects of the web-based system, multiple oral and poster presentations at various professional and scientific conferences, and two published manuscripts. These initial successes led to the decision to continue the collaboration on a new line of inquiry examining similar technology based interventions with other patient populations such as patients with chronic pain.
LIMITATIONS
We acknowledge several limitations of the FAIRR model. First, the current academic system often reinforces disseminating research in one’s discipline to establish professional jurisdiction. Such an emphasis can be especially strong during the early stages of an academic career.
Second, researchers should be aware of the challenges involved with creating interdisciplinary research teams. Being a part of an interdisciplinary team may lead to reduced or redefined professional autonomy. Members of an interdisciplinary team may not immediately benefit from the collaboration. New projects, which reflect unchartered territory, may require logistics such as coordinating shared resources to collect data, maintaining a central repository for data, and more meetings. To mitigate reduced autonomy and the time that it takes to reap the benefits of the collaboration, investigators’ research portfolios can include a combination of projects: some which are interdisciplinary and others that are multidisciplinary.
Last, one challenge with creating sustainable, productive interdisciplinary teams is the lack of consensus in the literature about the meaning of the term interdisciplinary. We stated our definition of the term interdisciplinary and used that term to guide model creation. However, we recognize that the term multidisciplinary is sometimes used interchangeably. Therefore, prior to implementing the model, it may be important for teams to consider whether they have consensus on the definition of interdisciplinary which was formative in creating the FAIRR model.
CONCLUSION
In summary, clinicians and scientists can use the FAIRR model to guide their efforts in building a strong and productive interdisciplinary rehabilitation research team. Use of the FAIRR model can help clinicians and scientists highlight the contributions and expertise of their individual disciplines. Implementation of the model can also advance rehabilitation research at a time that is ripe with opportunities for collaborative work.
Supplementary Material
Figure 4 (Supplementary Digital Content). Application of the Forging Alliances in Interdisciplinary Rehabilitation Research (FAIRR) logic model with a pediatric population. This figure delineates components of the FAIRR model applied to an interdisciplinary research project focusing on a pediatric population. HSR = health services research; HRSA = Health and Research Services Administration; CORRT = Comprehensive Opportunities in Rehabilitation Research Training; EI = Early Intervention; PT = Physical Therapy; OT = Occupational Therapy
Acknowledgments
Funding: This work was supported in part by NIH grants K12HD055931 (S.V. Gill M.A. Khetani, and B. M. McManus) and 1R01MD006213-0181 (P. Gardiner and L.Yinusa-Nyahkoon), and W.F. Kellogg Foundation (P3024018) (P. Gardiner and L. Yinusa-Nyahkoon).
Footnotes
Conflicts of interest: The authors declare no conflicts of interest.
References
- 1.Rondinelli RD. Collaboration as an adaptive strategy for the association of academic physiatrists. American journal of physical medicine & rehabilitation / Association of Academic Physiatrists. 2005;84(10):727–732. doi: 10.1097/01.phm.0000179441.70748.a8. [DOI] [PubMed] [Google Scholar]
- 2.Frontera WR, Fuhrer MJ, Jette AM, et al. Rehabilitation medicine summit: building research capacity. Executive summary. Archives of physical medicine and rehabilitation. 2006;87(1):148–152. doi: 10.1016/j.apmr.2005.10.021. [DOI] [PubMed] [Google Scholar]
- 3.Hung YC, Gill SV, Meredith GS. Influence of dual task constraints on whole body organization during walking in overweight and obese children. American Journal of Physical Medicine and Rehabilitation. 2013;92:461–467. doi: 10.1097/PHM.0b013e31828cd59d. [DOI] [PubMed] [Google Scholar]
- 4.Gill SV, Hung YC. Influence of weight classification on children stepping over obstacles. American Journal of Physical Medicine and Rehabilitation. 2012;91:625–630. doi: 10.1097/PHM.0b013e31824fa81e. [DOI] [PubMed] [Google Scholar]
- 5.Gardiner P, Hempstead MB, Ring L, et al. Reaching women through health information technology: the Gabby preconception care system. American journal of health promotion : AJHP. 2013;27(3 Suppl):eS11–20. doi: 10.4278/ajhp.1200113-QUAN-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jack B, Bickmore T, Hempstead M, et al. Reducing Preconception Risks Among African American Women with Conversational Agent Technology. J Am Board Fam Med. 2015;28(4):441–451. doi: 10.3122/jabfm.2015.04.140327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khetani MA, Graham JE, Davies PL, Law MC, Simeonsson RJ. Psychometric properties of the Young Children's Participation and Environment Measure. Archives of physical medicine and rehabilitation. 2015;96(2):307–316. doi: 10.1016/j.apmr.2014.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khetani MA. Validation of environmental context in the Young Children's Participation and Environment Measure. Archives of physical medicine and rehabilitation. 2015;96:317–322. doi: 10.1016/j.apmr.2014.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khetani MA, Kasiraj JM. Strengthening the Researcher-Practitioner Relationship to Support Best Practice in the Infant-Family Field. Zero to Three. 2009;29:8–12. [Google Scholar]
- 10.Jette AM. Without scientific integrity, there can be no evidence base. Physical therapy. 2005;85(11):1122–1123. [PubMed] [Google Scholar]
- 11.Stucki G, Celio M. Developing human functioning and rehabilitation research. Part II: Interdisciplinary university centers and national and regional collaboration networks. Journal of rehabilitation medicine. 2007;39(4):334–342. doi: 10.2340/16501977-0038. [DOI] [PubMed] [Google Scholar]
- 12.Grabois M. Through the looking glass: a personal view of the field of rehabilitation medicine. The 56th John Stanley Coulter Memorial Lecture. Archives of physical medicine and rehabilitation. 2007;88(4):408–412. doi: 10.1016/j.apmr.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 13.Ottenbacher KJ, Jette AM, Fuhrer MJ, Granger CV. Looking back and thinking forward: 20 years of disability and rehabilitation research. Archives of physical medicine and rehabilitation. 2012;93(8):1392–1394. doi: 10.1016/j.apmr.2012.02.028. [DOI] [PubMed] [Google Scholar]
- 14.Seelman KD. Science and technology policy: is disability a missing factor? Assist Technol. 2000;12(2):144–153. doi: 10.1080/10400435.2000.10132020. [DOI] [PubMed] [Google Scholar]
- 15.Peterson C. Health professions education: a bridge to quality. Tar Heel Nurse. 2003;65(4):12. [PubMed] [Google Scholar]
- 16.Pechak C, Gonzalez E, Summers C, Capshaw S. Interprofessional education: a pilot study of rehabilitation sciences students participating in interdisciplinary international service-learning. J Allied Health. 2013;42(3):e61–66. [PubMed] [Google Scholar]
- 17.University TJ. 2015 http://www.jefferson.edu/university/interprofessional_education/
- 18.Dijkers MP, Murphy SL, Krellman J. Evidence-based practice for rehabilitation professionals: concepts and controversies. Archives of physical medicine and rehabilitation. 2012;93(8 Suppl):S164–176. doi: 10.1016/j.apmr.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 19.Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376(9756):1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 20.Gill SV, Vessali M, Pratt JA, et al. The importance of interdisciplinary research training and community dissemination. Clinical and Translational Science. 2015;8:611–614. doi: 10.1111/cts.12330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.White MJ, Gutierrez A, McLaughlin C, et al. A pilot for understanding interdisciplinary teams in rehabilitation practice. Rehabil Nurs. 2013;38(3):142–152. doi: 10.1002/rnj.75. [DOI] [PubMed] [Google Scholar]
- 22.Leonard M, Graham S, Bonacum D. The human factor: the critical importance of effective teamwork and communication in providing safe care. Qual Saf Health Care. 2004;(13 Suppl 1):i85–90. doi: 10.1136/qshc.2004.010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gill SV, Khetani MA, Tickle-Degnen L, Yinusa-Nyahkoon L. Benefits and realities of engaging in interdisciplinary research relevant to pediatric occupational therapy practice. American Occupational Therapy Association; Nashville, TN: Apr, 2015. [Google Scholar]
- 24.NAS. NAE. IOM Facilitating interdisciplinary research. 2014 http://www.nap.edu/openbook.php?record_id=11153&page=16.
- 25.Bennett ML, Gadlin H, Levine-Finley S. Team science: A field guide. 2010 http://www.teamscience.nih.gov/
- 26.Rosenfeld JE, Garden FH. Interdepartmental education and collaboration in the academic setting. A commentary. American journal of physical medicine & rehabilitation / Association of Academic Physiatrists. 1994;73(3):217–218. doi: 10.1097/00002060-199406000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Aboelela SW, Larson E, Bakken S, et al. Defining interdisciplinary research: conclusions from a critical review of the literature. Health Serv Res. 2007;42(1 Pt 1):329–346. doi: 10.1111/j.1475-6773.2006.00621.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McCallin AM. Interdisciplinary researching: exploring the opportunities and risks of working together. Nurs Health Sci. 2006;8(2):88–94. doi: 10.1111/j.1442-2018.2006.00257.x. [DOI] [PubMed] [Google Scholar]
- 29.CDC How much physical activity do adults need? 2015 https://www.google.com/-q=cdc+physical+activity+guidelines+for+adults.
- 30.AOTA Occupational therapy practice framework: Domain and process. American Journal of Occupational Therapy. 2014;68:S1–S48. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure 4 (Supplementary Digital Content). Application of the Forging Alliances in Interdisciplinary Rehabilitation Research (FAIRR) logic model with a pediatric population. This figure delineates components of the FAIRR model applied to an interdisciplinary research project focusing on a pediatric population. HSR = health services research; HRSA = Health and Research Services Administration; CORRT = Comprehensive Opportunities in Rehabilitation Research Training; EI = Early Intervention; PT = Physical Therapy; OT = Occupational Therapy


