Abstract
Objectives
Correctional employees exhibit elevated obesity rates. This study examines interrelations among health behaviors, health climate, BMI, and work schedule.
Methods
Using survey results from correctional supervisors (n=157), mediation and moderated-mediation analyses were performed to examine how health behaviors explain relationships between obesity, work health climate (WHC) and family health climate (FHC), and work schedule.
Results
Over 85% of the sample was overweight/obese (mean BMI=30.20). Higher WHC and FHC were associated with lower BMI, mediated by nutrition and physical activity. The interaction effect between health behavior and work schedule revealed a protective effect on BMI. Overtime shiftwork may share a relationship with BMI.
Conclusions
Findings may have implications for reexamining organizational policies on maximum weekly overtime in corrections. They provide direction for targeted obesity interventions that encourage a supportive FHC and promote healthy behaviors among supervisors working overtime.
Keywords: shiftwork, overtime, work health climate, family health climate, obesity, nutrition, physical activity, correctional supervisors
INTRODUCTION
Obesity rates in the United States continue to climb, with recent statistics indicating 34.9% of U.S. adults are obese.1 Healthcare costs, reductions in employee productivity, increased sick day use, workers’ compensation claims, and many other consequences of obesity continue to challenge employers.2,3 Despite awareness of the economic consequences of obesity, preventive health efforts remain fundamental and there is a growing need for innovative research to develop sustainable evidence-based interventions that improve employee health.4,5 Home and work environments are important contributors to health behavior, especially in workplaces that are authoritative, and employees have less control over their daily circumstances.
Correctional employees, the target population in the present study, are at risk for developing obesity and related comorbidities.6–8 Correctional institutions require 24-hour supervision and staffing. The nature of the work environment and interactions with an incarcerated population may not be conducive to psychological and physical health. Rotating shifts and working excessive overtime may lead to unhealthy eating choices and physical inactivity in employees maintaining sedentary work stations. Correctional employees typically hold sedentary positions, with the exception of short bursts of activity to respond to emergency codes.6 Furthermore, methods of coping with stress and mental health may influence lifestyle behaviors such as dietary habits.9 Additional barriers to optimal health include: inability to participate in organized sports or exercise programs due to inconsistent rotating work schedules, inability to leave the facility during shifts, inability to walk outside on breaks, and inability to use on-site fitness facilities during working hours due to concerns for injuries or delayed responses to emergency codes.6 Scheduling conflicts paired with environmental aspects of the workplace (e.g., a locked building, post rotations) limit opportunities for daily physical activity and promote sedentary behavior.6 Supervisors (the study population) may also be challenged by administrative responsibilities that increase sedentary work time. Consequently, correctional officers (COs) exhibit higher levels of overweight, obesity, hypertension, alcohol consumption, heart disease and diabetes compared to national averages.6
The average life expectancy of correctional employees is significantly lower than the general population,10,11 and the costs associated with chronic disease are skyrocketing. According to the CDC, preventable chronic health problems include: heart disease, stroke, cancer, type 2 diabetes, obesity, and arthritis.12 The incidence of these chronic conditions in relation to life expectancy in the correctional workforce is relatively unknown. Work schedules are recognized as a primary source of work-related stress for COs.13 Elevated rates of chronic disease among correctional employees6,8 may be linked to overtime and rotating shifts, which may exacerbate pre-existing health conditions during the work career, decrease life expectancy, and increase healthcare costs. Generalization of findings from research on similar occupations may be limited due to differences in job rotation, stress at work, mandatory versus elective overtime, and number of rest days between work periods which can confound interactions between overtime and health.
Addressing workplace and home environments as contributors to health behavior may be one approach to stimulate improvement or prevent worsening of lifestyle behaviors, particularly in an authoritative and understudied group, the correctional employee workforce. In this study, we hypothesize (Hypothesis 1) that work health climate (WHC) and family health climate (FHC) are essential aspects of their respective social environment, and that better perceived health climate is associated with healthier nutrition and physical activity behaviors, and thus, a lower measure of body mass index (BMI) (see Figure 1). In addition, we hypothesize (Hypothesis 2) that work schedule factors, such as shift and overtime will share relationships with health climate, health behaviors, and obesity (BMI) (see Figure 2). WHC and FHC are relatively new constructs that need further investigation. Following are definitions of WHC, FHC, and work schedule, as they pertain to the present study.
Figure 1. Mediation Model.
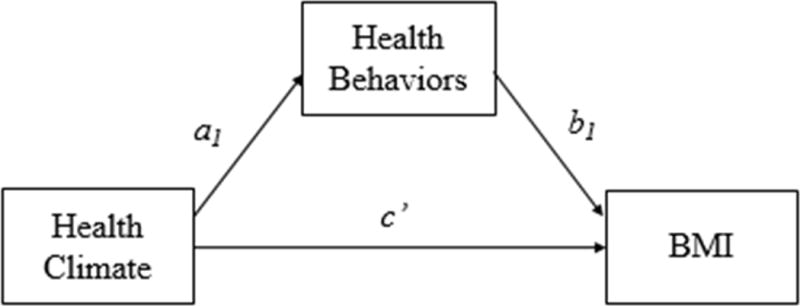
Relationship of health climate (WHC or FHC) and BMI as mediated by health behaviors (nutrition, physical activity).
Figure 2. Moderated Mediation Model.
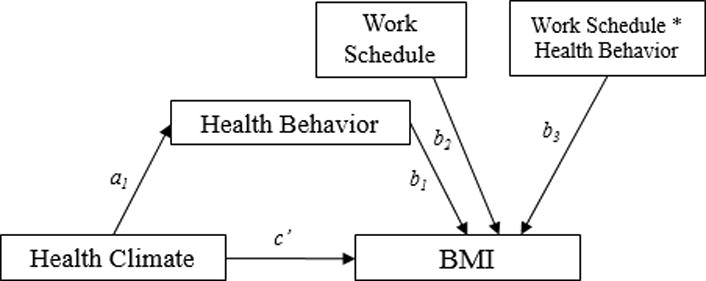
Relationship of health climate (WHC or FHC) and BMI as mediated by health behaviors (nutrition, physical activity) and moderated by work schedule (overtime hours, shift).
Work Health Climate
Using a social ecological approach to the workplace, researchers investigate and address how behavior is influenced at the individual, interpersonal, and organizational levels.14 Studies typically examine work health climate in two major ways: 1) the perceived environment, and whether it is supportive of health via policies, resources, or incentives, and 2) coworker social support for health. Higher levels of perceived coworker support and a supportive psychosocial work environment are associated with healthier behaviors.15–20 Organizational health climate, referred to in this study as “work health climate” (WHC), is a relatively new construct in the literature. Zweber et al. (2015) identify three levels in the workplace (i.e., workgroup, supervisor, organization) that play a role in developing a worksite culture supportive of health and well-being. Organizational-level aspects that contribute to a positive health climate include policies, resources, or opportunities to engage in healthy behaviors. These factors are important to direct intervention efforts at either individual or multiple levels that contribute to organizational health climate.21,22 For example, supervisors may play an important role in supporting health by increasing communication, helping workers manage stress, or encouraging participation in health promotion programs. Previous research reports positive associations between organizational or work health climate with health behaviors such as nutrition and physical activity.23,24
Family Health Climate
Family health climate (FHC) describes how routine everyday life tasks and experiences shape behavior and perceptions of health through interactions among family members.25 This construct, first defined by Niermann et al. (2014) encompasses daily health behaviors such as nutrition and physical activity that occur both in and outside the home environment. A positive perception of this climate indicates that these health behaviors are intrinsic in daily motivations and actions.25 Studies typically assessing FHC and health behaviors use inclusive psychosocial measures consistent with the concept, such as spouse or family social support for health behaviors, but not as an intuitive measure of health climate that captures relationships, attitudes, and behaviors in the home and family environment.26–29
Higher levels of social support and social health norms among family and social networks are associated with healthier behaviors.19,28–30 Furthermore, interventions may have a carryover effect on untreated members in the household.26,27 There may also be a combined benefit of a supportive social and physical environment, such as cues within the home, access to resources (i.e., healthy foods, exercise equipment), and support from family members.19,28,29
Work Schedule Factors
Certain features of work, such as long working hours and overtime are associated with poor health outcomes.31–33 However, some relationships between overtime and health behaviors remain unclear.34 According to Swensen et al. (2012), the negative health implications of these work schedule factors may impact cognitive, emotional, and physical function.35
Shift and long working hours may share a reciprocal relationship with health behaviors and outcomes, though findings are mixed. Gu et al. (2012) examined shiftwork, defined by the participants’ start time, with three classifications: day shift (start between 4–11AM), afternoon shift (start between 12–7PM), and midnight shift (start between 8PM–3AM). The authors reported an association between long working hours, waist circumference and BMI in males on midnight shift, controlling for potential covariates. This finding was non-significant for day and afternoon shifts. The authors attribute these findings to changes in lifestyle behaviors such as nocturnal eating, dysregulation in sleep patterns and stress.36 Health behaviors may play a partial role in health outcomes, and changes in physiological processes from increased overtime may cause strain and worsen health status.37 Nakamura et al. (1998) found weak associations between increased overtime, BMI and waist circumference when assessed longitudinally. Eating behaviors may play a role in moderating this relationship; however, more research is needed.38
There may be important effects dependent on age and length of time working night shift, as a dose-response relationship may influence chronic disease profile, including obesity. For example, working night shift short-term and in younger adults (< 25 years) may allow for resilience back to daily routines, and be less harmful to health.39 Research has been inconclusive when accounting for potential confounding variables such as body weight or activity level.32,40
Purpose
To our knowledge, no studies have collectively evaluated work health climate, family health climate, health behaviors and work schedule as predictors of obesity in a high-stress work environment. Although correctional supervisors may be exposed to shift work and excessive overtime, limited research examines the interacting relationship of health climate and health behaviors in this group. This group of middle managers may have the opportunity to change the health climate in the work environment, creating a ripple effect of perceived support for health, health norms, and health behavior change in the organization. WHC and FHC may be one approach to examine how psychosocial aspects of work and personal life are associated with health behaviors related to obesity.
The purpose of this study was to explore two health behaviors (i.e., nutrition, physical activity) as mediators of the relationships between work and family health climate and obesity, and to explore if work schedule factors moderate these relations. These findings will add to the literature by examining work schedule and health in an occupational group at increased risk of chronic disease.
MATERIALS AND METHODS
Design
This was a cross-sectional study using data collected from an online survey. This study utilized a Participatory Action Research (PAR) approach, as prior research supports conducting this design type in the correctional work setting.7,41 This PAR study was initiated by the correctional supervisors’ union who wished to partner with University researchers to: 1) assess the overall health of the State’s correctional supervisors, and 2) identify priority areas for health intervention within that workforce. Thus the purpose of this study extended beyond only conducting nutrition/physical activity research. To carry out the PAR project, we followed the standardized protocols of the Healthy Workplace Participatory Program (HWPP), developed by the Center for the Promotion of Health in the New England Workplace (CPH-NEW), a NIOSH Center of Excellence for Total Worker Health. Thus we used the HWPP All Employee Survey, developed by CPH-NEW researchers, which contains items from existing publicly accessible and validated instruments that were compiled into a condensed instrument. This was done by reducing measures to a minimum number of items that still retain good psychometric properties and are most strongly correlated with measures from a concurrently administered physical examination. Although the survey contains some single-item measures, research has shown that some single item measures are useful for capturing information about constructs that might otherwise go unmeasured, and that some single items of health are relatively strong predictors of health outcomes.42–44 We used the HWPP All Employee Survey as the core basis of the survey; it is a streamlined and standardized instrument that has been validated and widely used in workplace health studies conducted by CPH-NEW, and provides an overall assessment of a given worker population in terms of the perceived psychosocial and physical work environment, worker health status, and health behaviors. Due to the PAR method used in this study, correctional supervisors and university researchers all contributed equally to the survey design, adapting and adding measures from the All Employee Survey as necessary. Studies have demonstrated that employee-tailored survey questions are more relevant, acceptable, and feasible than conventional and generic survey measures.45 CPH-NEW instruments are publically available (at http://www.uml.edu/Research/centers/CPH-NEW/) for use in all sectors. Within CPH-NEW, they are being used in public safety community service work and healthcare.
Survey Development and Participants
Using the participatory process, supervisory staff collaborated with the research team to develop an acceptable and tailored survey for this project. To maximize statewide participation and increase response rate, an online survey platform was used. Participants were recruited via convenience sampling through internal advertising in the supervisors’ union bargaining unit (i.e., union leaders distributed survey invitations via email to their membership listserv). Inclusion criteria included: employment in a Connecticut Department of Correction (DOC) facility, union membership, and supervisory job category (lieutenant, captain, or counselor supervisor). A total of 157 correctional employees completed the survey.
Prior to participating in the survey, respondents were informed that there were no risks associated with participation, and that the potential benefits of participating included the development of future health and wellness initiatives for their work group. The survey consisted of 64 items and took approximately 20 minutes to complete. Participation was voluntary and anonymous. Items could be skipped if the participant felt uncomfortable answering any question. These methods were approved by the Institutional Review Board at the University of Connecticut and participants provided electronic consent prior to beginning the survey.
Measures
The following items were self-reported in the survey and explored in statistical analysis.
Demographic Variables
Age, sex, race, family income, educational status, marital status and job classification were self-reported on the survey.
Health Status
Body mass index (BMI) was used as an indicator of health status, and calculated using self-reported height (in inches) and weight (in pounds) with a conversion factor of 703, following the Centers for Disease Control and Prevention (CDC) equation.46
Health Climate
Work health climate (WHC) and family health climate (FHC) were assessed using a Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). Due to this study’s participatory action research method, correctional supervisors were involved in survey development to increase the acceptability and sensitivity of survey measures used.45 Thus the five-item measure used to assess WHC was a slightly adapted version of the scale created by Zweber et al. (2016) to evaluate workgroup, supervisor, and organization facets of organizational health climate.21 Items included: “In this facility, management considers employee safety to be important”, “In this facility, management considers employee health and well-being to be important”, “My coworkers would support my use of sick days for illness or mental health”, “My supervisor encourages healthy behaviors”, and “My organization provides me with opportunities to be healthy”.21 This construct was created using the sum score from survey items, and a higher score indicates better perceived work health climate. The total possible score for this item was 25.
FHC was assessed with four items to assess experiences pertaining to people with whom the participant shares a close relationship (i.e., family, friends). Items included: “We talk about improving health and preventing disease”, “Most people are very health conscious”, “People notice how well you take care of your health”, and “We encourage each other to make changes to improve our health.” This construct was created using the sum score from survey items; a higher score indicates better perceived family health climate. The total possible score for this item was 20. This item was created using a participatory design by the research team and supervisor union group, after reviewing the relatively few published measures of family health climate which were deemed inappropriate due to their numerous items and relevance only to specific types of health behaviors.47 The measure was intended to assess the social atmosphere among family members regarding health and to be brief enough so as not to pose an onerous burden on survey participants.
Health Behaviors
Nutrition and physical activity were each assessed with one item, by rating adherence to health behavior guidelines on a Likert scale from 1 (never) to 5 (always). Nutrition habits were assessed by asking the frequency of meeting expert recommended guidelines for fruit and vegetable consumption, as set by the U.S. Department of Agriculture and U.S. Department of Health and Human Services’ Dietary Guidelines for Americans, where a higher score indicates healthier eating habits.48 Physical activity habits were assessed by asking the frequency of meeting recommended guidelines for cardiovascular and resistance exercise, as set by the U.S. Department of Health and Human Services’ Physical Activity Guidelines for Americans, where a higher score indicates a higher likelihood of meeting national goals.49 Questions were selected in collaboration with the correctional supervisory group, and were not intended to comprise an extensive survey of diet and exercise behaviors given the prioritized interests of the supervisory council.
Work Schedule
Shift and overtime were self-reported. Participants were asked to report the primary shift to which they were assigned: first (7am–3pm), second (3pm–11pm), or third (11pm–7am). They were also asked the number of overtime hours they typically worked per week; response options included: none, 1–8 hours, 9–16 hours, 17–23 hours, 24 or more hours.
Statistical Analyses
Data was analyzed using IBM SPSS™ version 21 to recode variables and create new variables; SAS version 9.3 for descriptive statistics, frequency distributions, one-way ANOVAs, simple linear regression, and statistical test assumptions; and R version 3.2.2 for mediation and moderated-mediation analyses. The primary variables analyzed included demographic variables, BMI, and scores from the online workplace survey. Key variables were assessed for normality and the appropriate test assumptions prior to running statistical inference tests. Frequency analyses were run for categorical variables. Sum scores were created from health climate measures, which were treated as continuous variables, as this is considered a satisfactory statistical method.50,51 Simple linear regressions were run to analyze mediation assumptions by examining the a1, b1, and c’ paths (Figure 1). Residuals were analyzed due to violations of the normality assumption for health climate variables (WHC, FHC). To test for clustering among study participants within the different correctional facilities, an intraclass correlation (ICC) was tested by running an empty random effects model. The ICC was <0.10, indicating there was not enough dependence between facilities to suggest clustering, and thus a multilevel approach was not necessary. The cut-off for statistical significance was set at p < 0.05.
The mediation package in R software was used to evaluate different mediation and moderation modeling effects. Mediating and moderating variables were categorical (ordinal), and the independent and dependent variables were continuous. Mediation analyses use a series of multiple regression equations to help explain the mechanism of a particular outcome, in a sequential pattern.52 The mediation package is appropriate to test the hypotheses of this study because it allows for examination of mediation effects with a nonparametric approach using multiple types of variables (continuous, ordinal, etc.), and provides confidence intervals for interpretation of results.53
Mediation models were first tested independently prior to adding moderators to interpret the average causal mediation effects (ACME, indirect) and average direct effects (ADE). Exploratory analyses were performed to examine moderator effects on both the a1 and b1 paths. Proportion of the model mediated was examined for interpretation when there was absence of statistical significance to examine model effects. Standardized beta coefficients were utilized to assess the effect sizes for model paths,54 as regression coefficients are considered adequate measures of effect size indexes.55,56 For reference, r = 0.10 is considered a small effect, r = 0.25 is a medium effect, and r = 0.50 is a large effect size.57,58 Bootstrapping was used when running model syntax to estimate conditional indirect effects with a nonparametric approach. A generalized linear model function was used because the independent variable did not meet normality assumptions. Missing values were removed from analyses using a “drop observation” syntax. At most, only 1–2 participants were removed from statistical testing, leaving a minimum sample of n=155.
RESULTS
Descriptive Statistics
Survey respondents represented 20 facilities in Connecticut, with a response rate of 32%. Study respondents were primarily white (69.2%), male (78.2%), lieutenants (59.6%), and worked first shift (63.8%). In addition, respondents had some college education (38.8%) and most were married or living with their partner (73.0%). See Table I for additional demographic findings. Respondents had elevated rates of overweight (37.8%) and obesity (50.6%), defined as a body mass index ≥ 30. The mean [standard deviation (SD)] BMI was 30.0 (±4.6), which is classified as obese. On average, respondents were 42.3 (±6.1) years old. There was a significant difference in BMI by gender, and females (28.7±4.2) had a slightly lower mean BMI than males (30.7±4.3). BMI did not significantly differ by job classification, shift, or weekly reported overtime. Over half the sample (53%) reported working more than two overtime shifts per week. Refer to Buden et al. (2016) for additional descriptive statistical findings.59
Table I.
Demographic Results of Study Sample (n=157)
| % | |
|---|---|
| Gender | |
| Male | 78.2 % |
| Female | 21.8% |
| Race/Ethnicity | |
| White, European, or European American | 69.2% |
| Black, African American, or African | 16.0% |
| Hispanic, Latino or Hispanic American | 9.6% |
| Other | 3.2% |
| Asian, Asian American, or Pacific Islander | 1.3% |
| Middle Eastern, Arab, or Arab American | 0.6% |
| Education | |
| High school graduate or GED | 15.3% |
| Some college | 38.8% |
| College degree (2 or 4-year college) | 35.0% |
| Graduate degree | 10.8% |
| Marital Status | |
| Married or live with partner | 73.0% |
| Widowed | 1.9% |
| Divorced or separated | 16.0% |
| Single, never married | 8.9% |
| Family Income | |
| $50,000–74,999 | 1.3% |
| $75,000–99,999 | 24.5% |
| $100,000–124,999 | 29.7% |
| $125,000–149,999 | 15.5% |
| More than $150,000 | 29.0% |
| Job Classification | |
| Counselor Supervisor | 11.5% |
| Lieutenant | 59.6% |
| Captain | 28.8% |
| Shift | |
| First | 64% |
| Second | 21% |
| Third | 15% |
Demographic variables (age, gender, race/ethnicity, education status, marital status and family income) were not significantly associated with WHC or FHC. Family income as a predictor of FHC approached statistical significance (p=0.09). WHC score did not differ by shift (p=0.45), job tenure (p=0.82), job classification (p=0.12) or reported weekly overtime (p=0.28). There were statistically significant differences in WHC score by facility the participant worked in (p<0.001).
Simple Linear Regression
Corresponding to Figure 1, simple linear regressions were used to evaluate health climate (WHC, FHC) as predictors of health behaviors (nutrition, physical activity), a1 path; health behaviors (nutrition, physical activity) as predictors of BMI, b1 path, controlling for health climate measures; and health climate (WHC, FHC) as predictors of BMI, c’ path. These analyses were performed to test the assumptions for running a mediation model. First, examining the a1 path, WHC was a significant predictor of nutrition (β=0.04, p<0.05) but not physical activity (β=0.04, p=0.11) and FHC was a significant predictor of nutrition (β=0.09, p<0.01) and physical activity (β=0.13, p<0.01). Next, examining the b2 path, physical activity was a significant predictor of BMI when controlling for both WHC (β=−0.96, p<0.01) and FHC (β=−0.95, p<0.01). All relationships occurred as hypothesized; better perceived health climate was associated with healthier nutrition and physical activity, observed by the value of the parameter estimate (β). Last, examining the c’ path, perceived WHC score (β=−0.02, p=0.79) and FHC score (β=−0.13, p=0.35) did not significantly predict BMI in a linear fashion. Residuals for all models were normal, so a log transformation was not needed because it would not significantly influence the overall model.60 Lack of a significant regression between health climate measures and BMI does not justify a conclusion that complete mediation will not occur. Rather, statistical analysts suggest further analysis to evaluate other potential mediating effects.61
Mediation
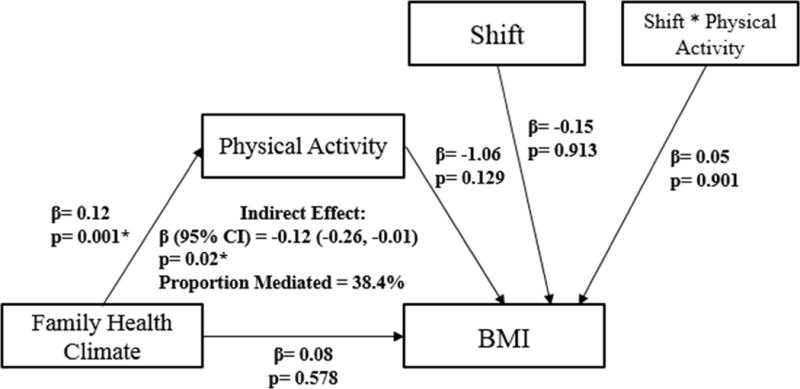
Mediation analyses were performed to test Hypothesis 1 and examine the effects of health climate (WHC, FHC) on obesity mediated by health behaviors, controlling for age and gender. FHC was associated with obesity mediated by physical activity, with a significant indirect effect (p<0.05) and 47.3% of the model mediated. However, the total effect was not significant (p=0.40), indicating that there was not complete mediation in this model. There was no significant indirect or total effect for the relationship between FHC on BMI mediated by nutrition. The indirect effects for WHC on BMI mediated by health behaviors (nutrition, physical activity) were not statistically significant (p=0.16 and p=0.12, respectively). However, nutrition mediated 18.1% of the model, and physical activity mediated 28.1%. No models revealed complete mediation, demonstrated by an absence of a significant total effect (not shown). Figure 3 provides visual depictions of these findings. In summary, all four models tested displayed results consistent with Hypothesis 1 in that better perceived health climate (WHC, FHC) was associated with healthier behaviors (nutrition, physical activity), and decreased BMI, as interpreted from the point estimates for the a and b paths of each model, refer to Figure 1. However, there was an absence of complete mediation in the four models.
Figure 3. Mediation models.
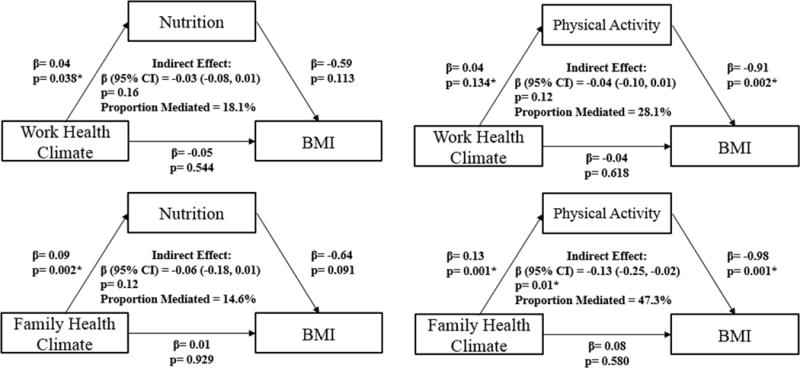
for relationship of health climate (WHC, FHC) and BMI as mediated by health behaviors (nutrition, physical activity).
Moderated-Mediation
To test Hypothesis 2, we proceeded with moderated-mediation modeling to determine the role of another predictor variable. Moderated-mediation models allow us to determine the strength of the indirect effect on different levels of the moderating variables, overtime and shift. Using guidance from Preacher, Rucker, and Hayes (2007),62 a model was created in which the moderator exhibits its’ effects on the b1 path, as this lead to the most significant effects for interpretation of the data. Examination of the b1 path allows for interpretation of changes in BMI when health behaviors interact with the associated work schedule factor. Regression coefficients (β) and p values were analyzed for the moderating paths to interpret effects on the dependent outcome variable (BMI). Exploratory analyses were performed with several different approaches to determine the conditional indirect effect, i.e., the mediation effect occurring at different levels of the categorical overtime and shift variables, controlling for age and gender.
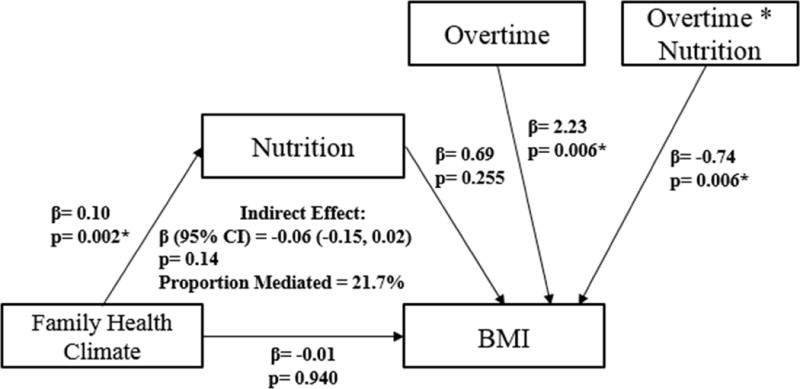
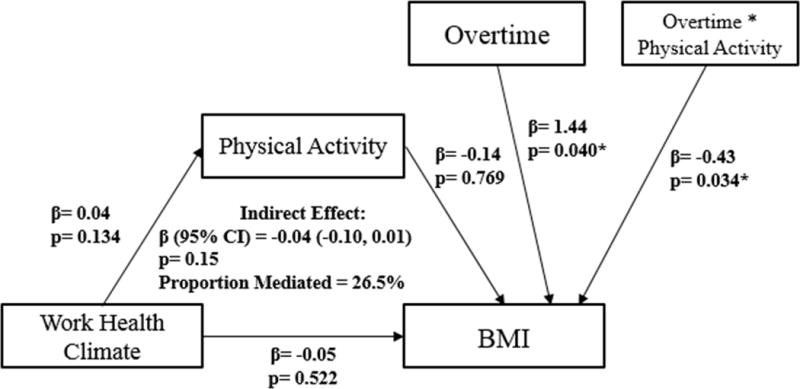
Overtime
There was a conditional indirect effect for all four models tested, suggesting inconsistent mediation. This means the indirect effect is conditional depending on the level of the moderating variable, overtime hours. Demonstrated in Figures 4–7 and examining the b2 path (overtime → BMI), overtime acted as a significant moderator for WHC mediated by nutrition (β=2.21, p<0.01) and physical activity (β=1.44, p<0.05); and for FHC mediated by nutrition (β=2.23, p<0.01) and physical activity (β=1.40, p<0.05). The interaction effect for the moderator overtime with the mediating health behavior variable revealed a negative estimate, indicating that the interaction was associated with decreased BMI. When evaluating the models as a whole, FHC on BMI mediated by physical activity had a significant indirect effect (p<0.05). The indirect and total effects of all other models did not reach statistical significance, which is attributed to inconsistent mediation discussed below.
Figure 4. Moderated-mediation.
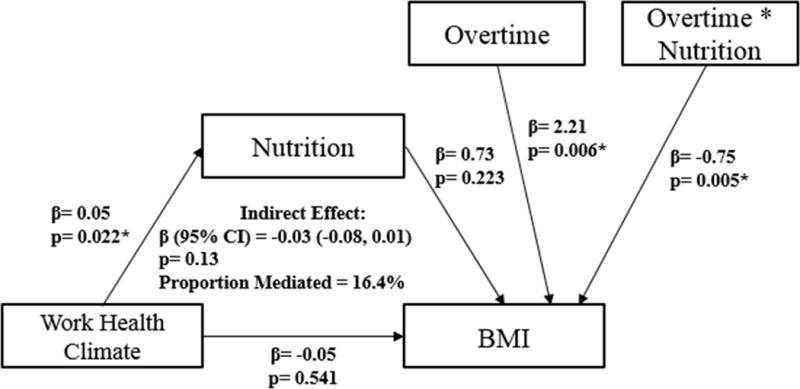
Relationship of work health climate (WHC) and BMI as mediated by nutrition and moderated by overtime hours.
Figure 7. Moderated-mediation.
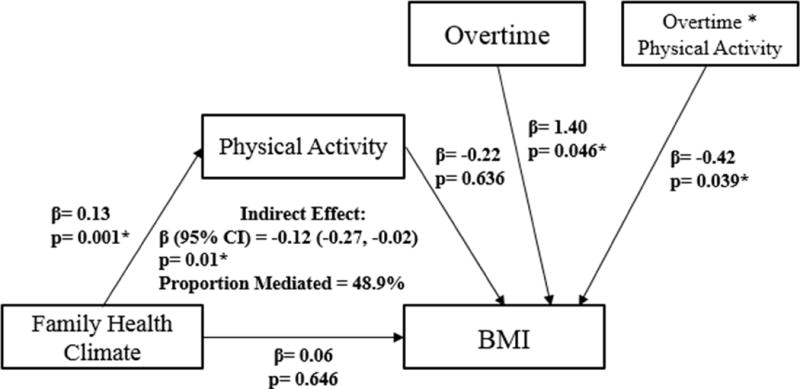
Relationship of family health climate (FHC) and BMI as mediated by physical activity and moderated by overtime hours.
Comparison of the models mediated at different levels of overtime provides insight as to when the relationships become significant and reveal inconsistent mediation. Overtime became a significant moderator when working more than one additional shift per week (for 9–16 hours, 17–23 hours, 24 or more hours) for work and family health climate mediated by nutrition (indirect effect for 9–16 hours: β=−0.04, p<0.05 and β=−0.08, p<0.05, respectively) and family health climate mediated by physical activity (β=−0.14, p<0.001), demonstrated in Tables II–III. The proportion of the model mediated increased with overtime frequency.
Table II.
Moderated-mediation effect for work health climate on BMI moderated by different levels of overtime
| Overtime Hours | Direct Effect Path c’ (β) |
Indirect Effect Bootstrapped Path a*b (β) |
Total Effect Path c (β) |
Proportion Mediated (%) | Bootstrapped 95% CI for Indirect Effect |
|---|---|---|---|---|---|
| Work health climate mediated by nutrition | |||||
| 0 | −0.05 | 0.03 | −0.02 | −5.48 | −0.02, 0.10 |
| 1–8 | −0.05 | −0.00 | −0.05 | 0.25 | −0.05, 0.04 |
| 9–16 | −0.05 | −0.04* | −0.09 | 25.70 | −0.09, −0.00* |
| 17–23 | −0.06 | −0.07* | −0.13 | 46.30 | −0.16, −0.01* |
| 24+ | −0.05 | −0.11** | −0.16 | 59.80 | −0.24, −0.02* |
| Work health climate mediated by physical activity | |||||
| 0 | −0.05 | −0.01 | −0.06 | 3.18 | −0.05, 0.04 |
| 1–8 | −0.05 | −0.02 | −0.08 | 16.50 | −0.07, 0.01 |
| 9–16 | −0.06 | −0.04 | −0.10 | 30.90 | −0.10, 0.01 |
| 17–23 | −0.06 | −0.06 | −0.11 | 39.60 | −0.14, 0.02 |
| 24+ | −0.05 | −0.07 | −0.13 | 47.10 | −0.19, 0.02 |
p < 0.05.
p < 0.01.
Table III.
Moderated-mediation effect for family health climate on BMI moderated by different levels of overtime
| Overtime Hours | Direct Effect Path c’ (β) |
Indirect Effect Bootstrapped Path a*b (β) |
Total Effect Path c (β) |
Proportion Mediated (%) | Bootstrapped 95% CI for Indirect Effect |
|---|---|---|---|---|---|
| Family health climate mediated by nutrition | |||||
| 0 | −0.01 | 0.07 | 0.05 | 23.80 | −0.04, 0.21 |
| 1–8 | −0.01 | −0.01 | −0.01 | 2.43 | −0.10, 0.09 |
| 9–16 | −0.01 | −0.08* | −0.08 | 39.20 | −0.17, −0.01* |
| 17–23 | −0.01 | −0.15** | −0.16 | 70.40 | −0.29, −0.04** |
| 24+ | −0.01 | −0.22** | −0.23 | 89.00 | −0.43, −0.06** |
| Family health climate mediated by physical activity | |||||
| 0 | −0.07 | −0.03 | 0.04 | 2.42 | −0.18, 0.09 |
| 1–8 | 0.07 | −0.08 | −0.02 | 8.75 | −0.20, 0.00 |
| 9–16 | 0.07 | −0.14** | −0.07 | 72.20 | −0.26, −0.04** |
| 17–23 | 0.06 | −0.20** | −0.14 | 99.90 | −0.37, −0.07** |
| 24+ | 0.07 | −0.25** | −0.19 | 110.99 | −0.48, −0.08** |
p < 0.05.
p < 0.01.
Inspection of the indirect effects at different levels of overtime reveal a non-significant moderated-mediation when individuals work no overtime. As mentioned above, the protective effect of health behaviors was due to inconsistent mediation in the model. This finding is confirmed by a negative proportion mediated for WHC mediated by nutrition when the moderator, overtime, was set at 0 hours/week. Similarly, this is confirmed by a proportion mediated greater than 100% when FHC is mediated by physical activity. Mediation is still occurring, but due to the unique nature of the variables, the direct and indirect effects cancel each other out, resulting in a small total effect, which was not statistically significant. Displayed in Figures 4–7 this relationship is occurring because of the suppressor effect from the mediating variables, nutrition and physical activity, and can be confirmed by evaluating the signs of ab and c’.61,63
Shift
Similar to the overtime models, there was inconsistent mediation in the models for health climate (WHC, FHC) on BMI mediated by health behaviors (nutrition, physical activity), and moderated by shift. Examination of the b2 paths (shift → BMI) in Figures 8–9 revealed positive parameter estimates, though nonsignificant. The opposite was true when FHC was the independent variable, and the b2 paths (shift → BMI) had negative parameter estimates, though nonsignificant (refer to Figures 10–11). The interaction effect in all models between shift and health behaviors (nutrition, physical activity) was also nonsignificant. Working first (β=−0.12, p<0.05) or second shift (β=−0.11, p<0.05) were significant moderators for the indirect model effect of FHC on BMI mediated by physical activity. First and second shifts mediated 44.5% and 46.1% of the models, respectively. The overall model had a significant indirect effect, but nonsignificant total effect, revealing inconsistent mediation (β=−0.12, p<0.05). The overall model approached significance for WHC on BMI mediated by physical activity (β=−0.04, p=0.09). Working first (β=−0.04, p=0.07) or second shift (β=−0.04, p=0.08) approached significance for the indirect model effect of WHC on BMI mediated by physical activity. The proportion of the model mediated was highest for third shift for WHC on BMI mediated by nutrition (40.5%) and FHC on BMI mediated by nutrition (50.4%), see Tables IV–V.
Figure 8. Moderated-mediation.
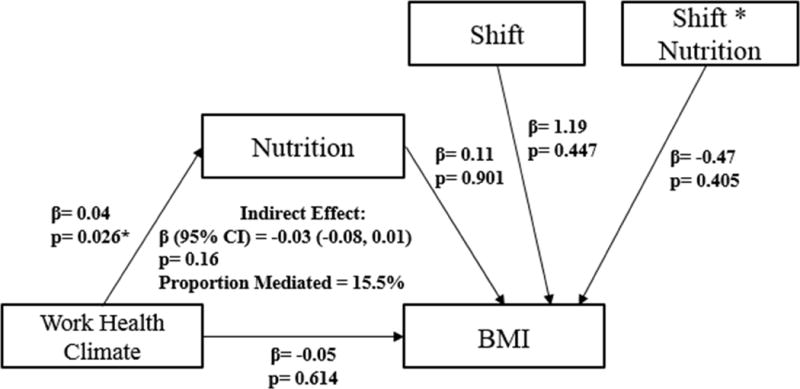
Relationship of work health climate (WHC) and BMI as mediated by nutrition and moderated by shift (first, second, third).
Figure 9. Moderated-mediation.
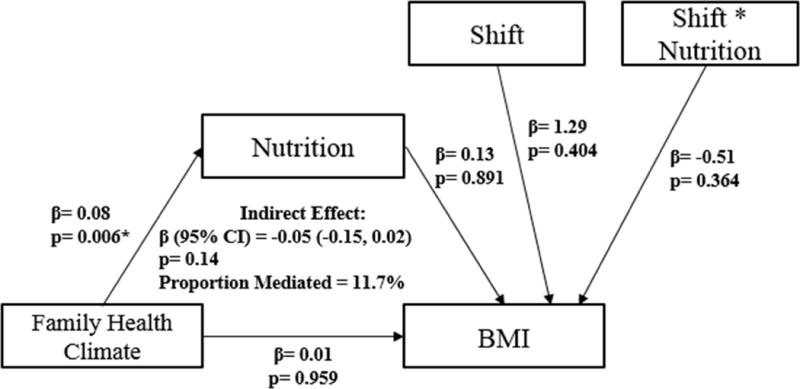
Relationship of family health climate (FHC) and BMI as mediated by nutrition and moderated by shift (first, second, third).
Figure 10. Moderated-mediation.
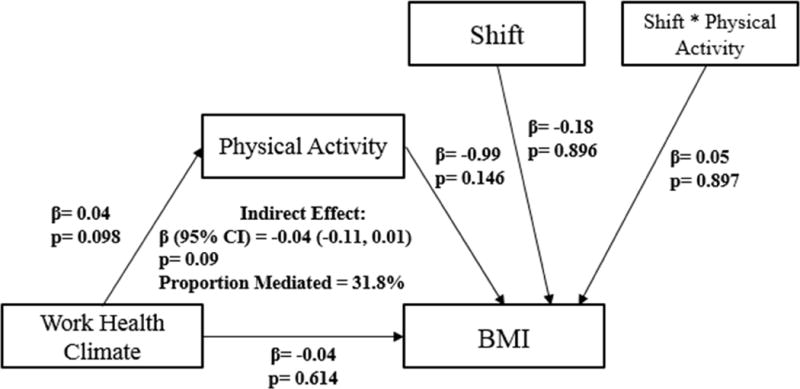
Relationship of work health climate (WHC) and BMI as mediated by physical activity and moderated by shift (first, second, third).
Figure 11. Moderated-mediation.
Relationship of family health climate (FHC) and BMI as mediated by physical activity and moderated by shift (first, second, third).
Table IV.
Moderated-mediation effect for work health climate on BMI moderated by different shifts
| Shift | Direct Effect Path c’ (β) |
Indirect Effect Bootstrapped Path a*b (β) |
Total Effect Path c (β) |
Proportion Mediated (%) | Bootstrapped 95% CI for Indirect Effect |
|---|---|---|---|---|---|
| Work health climate mediated by nutrition | |||||
| 1st | −0.05 | −0.02 | −0.07 | 11.53 | −0.07, 0.03 |
| 2nd | −0.04 | −0.04 | −0.08 | 27.29 | −0.10, 0.01 |
| 3rd | −0.05 | −0.06 | −0.11 | 40.52 | −0.18, 0.02 |
| Work health climate mediated by physical activity | |||||
| 1st | −0.04 | −0.04 | −0.08 | 33.44 | −0.11, 0.00 |
| 2nd | −0.05 | −0.04 | −0.09 | 28.85 | −0.11, 0.00 |
| 3rd | −0.05 | −0.04 | −0.08 | 23.96 | −0.13, 0.02 |
p < 0.05.
p < 0.01.
Table V.
Moderated-mediation effect for family health climate on BMI moderated by different shifts
| Shift | Direct Effect Path c’ (β) |
Indirect Effect Bootstrapped Path a*b (β) |
Total Effect Path c (β) |
Proportion Mediated (%) | Bootstrapped 95% CI for Indirect Effect |
|---|---|---|---|---|---|
| Family health climate mediated by nutrition | |||||
| 1st | 0.01 | −0.03 | −0.02 | 5.20 | −0.12, 0.06 |
| 2nd | 0.01 | −0.08 | −0.07 | 32.91 | −0.18, 0.01 |
| 3rd | 0.00 | −0.12 | −0.11 | 50.41 | −0.32, 0.03 |
| Family health climate mediated by physical activity | |||||
| 1st | 0.08 | −0.12** | −0.04 | 44.53 | −0.26, −0.03* |
| 2nd | 0.08 | −0.11** | −0.03 | 46.10 | −0.23, −0.02* |
| 3rd | 0.09 | −0.11 | −0.02 | 38.56 | −0.30, 0.05 |
p < 0.05.
p < 0.01.
In summary, with the exception of some findings where shift was the moderator, an increased frequency of overtime hours was significantly associated with higher BMI. The interaction effect between overtime and health behavior (nutrition, physical activity) was “protective”, and associated with lower BMI. There was a significant conditional indirect effect in the relationships between health climate (WHC, FHC), BMI, and health behaviors when moderated by one or more additional overtime shift per week; however, there was no conditional indirect effect for WHC on BMI mediated by physical activity when moderated by overtime. Our findings also revealed a significant indirect model effect for FHC on BMI mediated by physical activity when moderated by first and second shifts; this approached significance for WHC. There were no other significant conditional indirect effects when shift was the moderator. The interaction effect between shift and health behavior did not consistently align with the hypothesis of this study in that some shifts may be associated with higher or lower BMI. There was an absence of complete mediation in all moderated-mediation models, which may be attributed to inconsistent mediation. However, the results of the conditional indirect effects are telling and these results are partially consistent with Hypothesis 2.
DISCUSSION
Respondents were mostly middle-aged correctional supervisors, primarily working first shift and working frequent overtime. Our goal in this study was to examine whether these schedule-based job characteristics have a damaging effect on the health status of correctional supervisors and how this situation might be addressed to improve their health through the development and implementation of targeted interventions. For example, providing opportunities to improve nutrition and physical activity of shiftwork employees or interrupting maximum weekly overtime hours may provide direction for organizational change. In addition, intervening at the family level may produce sustainable health behavior change.
Demographic and work schedule factors (shift, overtime) were not associated with WHC or FHC. Controlling for age and gender, higher WHC and FHC scores tended to be associated with lower BMI mediated by nutrition and physical activity. Only one of four mediation models tested revealed a statistically significant indirect effect. No models had significant total effects. Lack of significance may be related to sample size and/or provides rationale for adding more variables to the models for further exploration. The model evaluating the association of FHC and BMI as mediated by physical activity had a significant indirect effect suggesting that the relationship between health climate in the home domain and BMI may be largely influenced by physical activity level. This finding, supported by previous studies suggesting that family social support is associated with physical activity,64–66 is informative for the development of targeted interventions. These associations may imply that lifestyle behaviors are related to access, availability, and social support for healthy eating and physical activity.
Work schedule (shift, overtime) may share a relationship with health behaviors37,67 and health outcomes.37,40,68,69 In this study we explored the role of overtime and shift work by examining their interrelationship with health climate, health behaviors and BMI. Moderated-mediation models tested in this study revealed a significant moderating effect on the b path, indicating that the mediation effect is dependent on different levels of the moderating variable, overtime. This is consistent with previous research suggesting the effects of overtime work on health may be dose dependent, and are best examined longitudinally.37 There was inconsistent mediation in the models, in that models became significant when participants worked two or more overtime shifts per week. This finding indicates that at a minimum of two overtime shifts a week, the role of overtime plays an interacting role with health climate, health behaviors, and BMI. Working more than two additional shifts per week may begin to have a negative effect on BMI. It may be at this juncture that practicing healthy behaviors becomes especially important in protecting against weight gain, and is a promising point of intervention. Further, barriers to engaging in healthy behaviors due to increased time spent at work must be a consideration of targeted interventions.
The difference in the indirect effect for overtime levels was statistically significant for WHC and FHC on BMI mediated by nutrition and for FHC on BMI mediated by physical activity. The interaction between overtime and health behavior (nutrition, physical activity) revealed a negative parameter estimate, suggesting that despite working more hours, health behaviors may suppress, or protect against higher levels of BMI. This is consistent with prior mixed findings between overtime and obesity explained by health behaviors.34 Some studies report weak and inconsistent associations between overtime, health behaviors and obesity and suggest that health behaviors are unchanged with long working hours.34,70 However, working a certain number of hours in the work week71 or overtime over a long period of time with minimal recovery may impact health behaviors and obesity.37,38 This may explain why overtime in this study started to impact BMI as overtime frequency increased. Individuals working the most frequent overtime may benefit from practicing healthy behaviors to protect against aging and overtime work.
The moderating effect found with overtime was not significant when shift was the moderator, conflicting with previous findings linking shiftwork to increased obesity.31,39 Lack of significant results for shiftwork may be attributed to the small sample size or large proportion of survey respondents working first shift (64%), in which we were unable to recognize significant effects. First and second shift had a significant indirect effect on BMI in the model examining FHC mediated by physical activity. Individuals working first or second shift may have better family support for health behaviors and less time-based barriers to being physically active, thus resulting in lower BMI. This is consistent with prior research linking family social support with increased physical activity19,29,72 and lower BMI among day shift workers compared to rotating and night shifts.68,73–75 Working first or second shift may have positive associations with health climate, physical activity and BMI compared to third shift. Despite finding some significant relationships when shiftwork and overtime were added to the models, the distribution of overtime throughout the work week is unknown. The importance of recovery may be vital when exposed to extended work hours.76
Future research should explore whether overtime is done over a 7-day period, or condensed into a 5-day week with little time to rejuvenate between shifts. Other factors, such as what shift overtime is performed and whether it is mandatory or voluntary in nature, may influence emotional feelings associated with the workplace and interfere with opportunities to practice healthy behaviors. Health climate may vary within different work environments and assessing it may help researchers identify at-risk populations that perceive their physical and social environment as unsupportive of their health.23 In addition, these findings may strengthen the validity of the WHC and FHC measures, for application in other high-stress occupations.
In conclusion, correctional institutions are high-demand, low-control workplaces with unstructured overtime and unpredictable shifts. There is a high prevalence and incidence of chronic disease in correctional employees, including overweight and obesity.6,8,9 A more supportive perceived work and family health climate may share a relationship with health behaviors, and thus, obesity. Shiftwork and excess overtime may interact favorably or negatively with these health variables, and thus are an important consideration in occupations that require 24-hour staffing. Understanding the interrelations between work environment, family environment, and individual behavior are important for developing tailored, workplace-specific and cost-effective interventions. The findings of this study will be instrumental in developing tailored health interventions for supervisors at the Connecticut DOC, using a participatory design. This study also lays the groundwork for future research in high-stress occupations using relatively new health climate constructs. Interventions targeting worksite and family psychosocial environments may be the most effective in changing behaviors.
Limitations
Despite the promising findings from this study, there are several limitations worth discussing. The results presented throughout this study are preliminary findings acknowledging an understudied occupational group. The statistical results and interpretation of statistical modeling methodology may be limited in nature by the cross-sectional study design. In addition, this study was reliant on self-reported data and measurement tools that have not been validated to assess health behaviors or family health climate. However, use of a participatory design for survey development may have improved the validity and reliability of these findings to capture relationships within these networks. Lastly, this study may have limited generalizability to other middle-management groups, due to the high-demand and low-job control nature of corrections. Study findings may not offer generalizability to line-level correctional employees due to differences in other confounding variables, such as income, educational attainment, and job responsibilities. However, limited research to date has investigated correctional supervisor staff. These employees are well-respected in the chain of command, and may have an influential role on workplace health climate.
IMPLICATIONS OF FINDINGS
Our results indicate that family support for physical activity may be especially important to maintain a healthy BMI, and working two or more overtime shifts per week may negatively impact health climate, health behaviors, and BMI. Future research may test these models and relationships on a larger sample size, with more advanced study designs and in a longitudinal manner. The intent of this study was not to make comparisons among COs versus supervisors, though this may be an interesting direction for future research. Practicing healthy nutrition and physical activity behaviors despite increased overtime shifts may have a protective effect on BMI. This may provide direction for interventions that aim to reduce the health consequences of overtime in occupational groups where modifying the root cause, such as mandated overtime, may not be feasible. Providing resources supportive of health in the workplace may positively contribute to health outcomes when individuals have extended work shifts. Development of innovative policies in corrections for either maximum overtime hours or allowance of split-shifts may promote employee health and well-being. Interventions that address health climate, health behaviors, and work schedule are needed to expand upon these findings for application to health promotion approaches that are more effective, acceptable, and feasible.
Figure 5. Moderated-mediation.
Relationship of family health climate (FHC) and BMI as mediated by nutrition and moderated by overtime hours.
Figure 6. Moderated-mediation.
Relationship of work health climate (WHC) and BMI as mediated by physical activity and moderated by overtime hours.
Acknowledgments
This work was supported by the Center for the Promotion of Health in the New-England Workplace (CPH-NEW).
The authors would like to acknowledge the Correctional Supervisors Council for their initiation and support of the project, as well as their ongoing participation on the intervention Design Team. The authors would also like to acknowledge the Connecticut Department of Correction whose leaders support this project and whose supervisors participated in the study.
Funding: all sources of funding including disclosure of funding received for this work from any of the following organizations: National Institutes of Health (NIH); Wellcome Trust; Howard Hughes Medical Institute (HHMI); and other(s)
Grant sponsor: This publication was supported by The National Institute for Occupational Safety and Health (NIOSH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH. Grant Number: R01OH008929.
Footnotes
Institution at which the work was performed: University of Connecticut
All conflicts of interest (COI)
None declared.
References
- 1.Ogden C, Carroll M, Kit B, Flegal K. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Borak J. Obesity and the workplace. Occup Med (Lond) 2011;61(4):220–222. doi: 10.1093/occmed/kqr030. [DOI] [PubMed] [Google Scholar]
- 3.Finkelstein E, Ruhm C, Kosa K. Economic causes and consequences of obesity. Annu Rev Public Health. 2005;26:239–257. doi: 10.1146/annurev.publhealth.26.021304.144628. [DOI] [PubMed] [Google Scholar]
- 4.Anderson L, Quinn T, Glanz K, et al. The effectiveness of worksite nutrition and physical activity interventions for controlling employee overweight and obesity: A systematic review. Am J Prev Med. 2009;37(4):340–357. doi: 10.1016/j.amepre.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 5.Pelletier K. A review and analysis of the clinical and cost-effectiveness studies of comprehensive health promotion and disease management programs at the worksite: Update VIII 2008 to 2010. J Occup Environ Med. 2011;53(11):1310–1331. doi: 10.1097/JOM.0b013e3182337748. [DOI] [PubMed] [Google Scholar]
- 6.Morse T, Dussetschleger J, Warren N, Cherniack M. Talking about health: Correction employees’ assessments of obstacles to healthy living. J Occup Environ Med. 2011;53(9):1037–1045. doi: 10.1097/JOM.0b013e3182260e2c. [DOI] [PubMed] [Google Scholar]
- 7.Dugan A, Farr D, Namazi S, et al. Process evaluation of two participatory approaches: Implementing total worker health interventions in a correctional workforce. Am J Ind Med. 2016;59(10):897–918. doi: 10.1002/ajim.22593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brower J, OJP Diagnostic Center Correctional officer wellness and safety literature review. Correctional Officer Health and Safety Literature Review. 2013 [Google Scholar]
- 9.Faghri P, Mignano C, Cherniack M, Huedo-Medina T. Psychological health and overweight and obesity among high stressed work environments. 2015;1(1) doi: 10.16966/2380-5528.101. http://dx.doi.org/10.16966/ooa.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheek F. Stress management for correctional officers and their families. 1984 [Google Scholar]
- 11.Parker J. Florida mortality study: Florida law enforcement and corrections officers compared to Florida general population. 2011 [Google Scholar]
- 12.National Center for Chronic Disease Prevention and Health Promotion. Chronic disease overview. Chronic Disease Prevention and Health Promotion Web site. https://www.cdc.gov/chronicdisease/overview/ Updated 2016. Accessed March, 2017.
- 13.Triplett R, Mullings J, Scarborough K. Work- related stress and coping among correctional officers: Implications from organizational literature. Journal of Criminal Justice. 1996;24(4):291–308. [Google Scholar]
- 14.McLeroy K, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 15.Apostolopoulos Y, Shattell M, Sonmez S, Strack R, Haldeman L, Jones V. Active living in the trucking sector: Environmental barriers and health promotion strategies. J Phys Act Health. 2012;9(2):259–269. doi: 10.1123/jpah.9.2.259. [DOI] [PubMed] [Google Scholar]
- 16.Bopp M, Child S, Campbell M. Factors associated with active commuting to work among women. Women Health. 2014;54(3):212–231. doi: 10.1080/03630242.2014.883663. [DOI] [PubMed] [Google Scholar]
- 17.Lucove J, Huston S, Evenson K. Workers’ perceptions about worksite policies and environments and their association with leisure-time physical activity. Am J Health Promot. 2007;21(3):196–200. doi: 10.4278/0890-1171-21.3.196. [DOI] [PubMed] [Google Scholar]
- 18.Umstattd M, Baller S, Blunt G, Darst M. Correlates of perceived worksite environmental support for physical activity. J Phys Act Health. 2011;8(Suppl 2):S222–7. [PubMed] [Google Scholar]
- 19.Kegler M, Swan D, Alcantara I, Wrensford L, Glanz K. Environmental influences on physical activity in rural adults: The relative contributions of home, church and work settings. J Phys Act Health. 2012;9(7):996–1003. doi: 10.1123/jpah.9.7.996. [DOI] [PubMed] [Google Scholar]
- 20.Lemon S, Zapka J, Li W, Estabrook B, Magner R, Rosal M. Perceptions of worksite support and employee obesity, activity and diet. Am J Health Behav. 2009;33(3):299–308. doi: 10.5993/ajhb.33.3.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zweber Z, Henning R, Magley V. A practical scale for multi-faceted organizational health climate assessment. J Occup Health Psychol. 2016 doi: 10.1037/a0039895. [DOI] [PubMed] [Google Scholar]
- 22.Zweber Z, Henning R, Magley V, Faghri P. Considering the differential impact of three facets of organizational health climate on employees’ well-being. ScientificWorldJournal. 2015;2015:407232. doi: 10.1155/2015/407232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ribisl K, Reischl T. Measuring the climate for health at organizations. development of the worksite health climate scales. J Occup Med. 1993;35(8):812–824. doi: 10.1097/00043764-199308000-00019. [DOI] [PubMed] [Google Scholar]
- 24.Hoert J. Employee work and health behaviors: The role of leadership support for health promotion and organizational health climate. [PhD] University of Louisville; 2014. [Google Scholar]
- 25.Niermann C, Krapf F, Renner B, Reiner M, Woll A. Family health climate scale (FHC-scale): Development and validation. The International Journal of Behavioral Nutrition and Physical Activity. 2014;11:30–30. doi: 10.1186/1479-5868-11-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gorin A, Raynor H, Fava J, et al. Randomized controlled trial of a comprehensive home environment-focused weight-loss program for adults. Health Psychol. 2013;32(2):128–137. doi: 10.1037/a0026959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gorin A, Wing R, Fava J, et al. Weight loss treatment influences untreated spouses and the home environment: Evidence of a ripple effect. Int J Obes (Lond) 2008;32(11):1678–1684. doi: 10.1038/ijo.2008.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kegler M, Alcantara I, Veluswamy J, Haardorfer R, Hotz J, Glanz K. Results from an intervention to improve rural home food and physical activity environments. Prog Community Health Partnersh. 2012;6(3):265–277. doi: 10.1353/cpr.2012.0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kegler M, Swan D, Alcantara I, Feldman L, Glanz K. The influence of rural home and neighborhood environments on healthy eating, physical activity, and weight. Prev Sci. 2014;15(1):1–11. doi: 10.1007/s11121-012-0349-3. [DOI] [PubMed] [Google Scholar]
- 30.Sorensen G, Stoddard A, Dubowitz T, et al. The influence of social context on changes in fruit and vegetable consumption: Results of the healthy directions studies. Am J Public Health. 2007;97(7):1216–1227. doi: 10.2105/AJPH.2006.088120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amani R, Gill T. Shiftworking, nutrition and obesity: Implications for workforce health- a systematic review. Asia Pac J Clin Nutr. 2013;22(4):505–515. doi: 10.6133/apjcn.2013.22.4.11. [DOI] [PubMed] [Google Scholar]
- 32.Wang X, Armstrong M, Cairns B, Key T, Travis R. Shift work and chronic disease: The epidemiological evidence. Occup Med (Lond) 2011;61(2):78–89. doi: 10.1093/occmed/kqr001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bannai A, Tamakoshi A. The association between long working hours and health: A systematic review of epidemiological evidence. Scand J Work Environ Health. 2014;40(1):5–18. doi: 10.5271/sjweh.3388. [DOI] [PubMed] [Google Scholar]
- 34.Caruso C, Hitchcock E, Dick R, Russo R, Schmit J. Overtime and extended work shifts: Recent findings on illnesses, injuries, and health behaviors. U S Department of Health and Human Services: National Institute for Occupational Safety and Health (NIOSH) 2004 [Google Scholar]
- 35.Swenson D, Waseleski D, Hartl R. Shift work and correctional officers: Effects and strategies for adjustment. 2008:14. [Google Scholar]
- 36.Gu J, Charles L, Burchfiel C, et al. Long work hours and adiposity among police officers in a US northeast city. J Occup Environ Med. 2012;54(11):1374–1381. doi: 10.1097/JOM.0b013e31825f2bea. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Taris T, Ybema J, Beckers D, Verheijden M, Geurts S, Kompier M. Investigating the associations among overtime work, health behaviors, and health: A longitudinal study among full-time employees. Int J Behav Med. 2011;18(4):352–360. doi: 10.1007/s12529-010-9103-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nakamura K, Shimai S, Kikuchi S, et al. Increases in body mass index and waist circumference as outcomes of working overtime. Occup Med (Lond) 1998;48(3):169–173. doi: 10.1093/occmed/48.3.169. [DOI] [PubMed] [Google Scholar]
- 39.Ramin C, Devore E, Wang W, Pierre-Paul J, Wegrzyn L, Schernhammer E. Night shift work at specific age ranges and chronic disease risk factors. Occup Environ Med. 2015;72(2):100–107. doi: 10.1136/oemed-2014-102292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.van Drongelen A, Boot C, Merkus S, Smid T, van der Beek A. The effects of shift work on body weight change - a systematic review of longitudinal studies. Scand J Work Environ Health. 2011;37(4):263–275. doi: 10.5271/sjweh.3143. [DOI] [PubMed] [Google Scholar]
- 41.Reeves D, Walsh B, Tuller M, Magley V. The positive effects of participative decision making for midlevel correctional management. Crim Justice Behav. 2012;39(10):1361–1372. [Google Scholar]
- 42.Bird C, Fremont A. Gender, time use, and health. J Health Soc Behav. 1991;32(2):114–129. [PubMed] [Google Scholar]
- 43.Fisher G, Matthews R, Gibbons A. Developing and investigating the use of single-item measures in organizational research. J Occup Health Psychol. 2016;21(1):3–23. doi: 10.1037/a0039139. [DOI] [PubMed] [Google Scholar]
- 44.Verbrugge L. The twain meet: Empirical explanations of sex differences in health and mortality. J Health Soc Behav. 1989;30(3):282–304. [PubMed] [Google Scholar]
- 45.Nielsen K, Abildgaard J, Daniels K. Putting context into organizational intervention design: Using tailored questionnaires to measure initiatives for worker well-being. Human Relations. 2014;67(12):1537–1560. [Google Scholar]
- 46.Division of Nutrition, Physical Activity and Obesity, National Center for Chronic Disease Prevention and Health Promotion. Healthy weight. Centers for Disease Control and Prevention (CDC) Web site. http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html#Interpreted Updated 20152016.
- 47.Dugan A. Correctional supervisors’ council healthy workplace survey. 2014 [Google Scholar]
- 48.U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary guidelines for americans. 2010 http://www.cnpp.usda.gov/DGAs2010-PolicyDocument.htm Published December 2010. Accessed March 12, 2014.
- 49.U.S. Department of Health and Human Services. 2008 pysical activity guidelines for americans. 2010 [Google Scholar]
- 50.Carifio J, Perla R. Two common misunderstandings, misconceptions, persistent myths and urban legends about Likert scales and Likert response formats and their antidotes. Journal of Social Sciences. 2007;3(3):106–116. [Google Scholar]
- 51.Zumbo B, Zimmerman D. Is the selection of statistical methods governed by level of measurement? Canadian Psychology. 1993;34:390–400. [Google Scholar]
- 52.Gunzler D, Chen T, Wu P, Zhang H. Introduction to mediation analysis with structural equation modeling. Shanghai Arch Psychiatry. 2013;25(6):390–394. doi: 10.3969/j.issn.1002-0829.2013.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Imai K, Keele L, Tingley D, Yamamoto T. Advances in social science research using R. Springer; 2010. Causal mediation analysis using R; pp. 129–154. [Google Scholar]
- 54.Preacher K, Kelley K. Effect size measures for mediation models: Quantitative strategies for communicating indirect effects. Psychol Methods. 2011;16(2):93–115. doi: 10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- 55.Borenstein M, Hedges L, Higgins J, Rothstein H. Introduction to meta-analysis. Chichester: Wiley; 2009. [Google Scholar]
- 56.Becker B, Wu M. The synthesis of regression slopes in meta-analysis. 2007:414–429. [Google Scholar]
- 57.Cohen J. Statistical power analysis for the behavioral sciences. Routledge; 1988. [Google Scholar]
- 58.Cohen J. A power primer. Psychol Bull. 1992;112(1):155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 59.Buden J, Dugan A, Namazi S, Huedo-Medina T, Cherniack M, Faghri P. Work characteristics as predictors of correctional supervisors’ health outcomes. Journal of Occupational and Environmental Medicine. 2016;58(9):e325–e334. doi: 10.1097/JOM.0000000000000843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chen X, Ender P, Mitchell M, Wells C. Regression with SAS. 2003 [Google Scholar]
- 61.Kenny D. Inconsistent mediation. Mediation Web site. http://davidakenny.net/cm/mediate.htm Updated 2015. Accessed November, 2015.
- 62.Preacher K, Rucker D, Hayes A. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate behavioral research. 2007;42(1):185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- 63.Fritz M, Mackinnon D. Required sample size to detect the mediated effect. Psychol Sci. 2007;18(3):233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ickes M, Sharma M. A systematic review of physical activity interventions in hispanic adults. J Environ Public Health. 2012;2012:156435. doi: 10.1155/2012/156435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kelly S, Martin S, Kuhn I, Cowan A, Brayne C, Lafortune L. Barriers and facilitators to the uptake and maintenance of healthy behaviours by people at mid-life: A rapid systematic review. PLoS One. 2016;11(1):e0145074. doi: 10.1371/journal.pone.0145074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Seefeldt V, Malina R, Clark M. Factors affecting levels of physical activity in adults. Sports Med. 2002;32(3):143–168. doi: 10.2165/00007256-200232030-00001. [DOI] [PubMed] [Google Scholar]
- 67.Nabe-Nielsen K, Quist H, Garde A, Aust B. Shiftwork and changes in health behaviors. J Occup Environ Med. 2011;53(12):1413–1417. doi: 10.1097/JOM.0b013e31823401f0. [DOI] [PubMed] [Google Scholar]
- 68.Antunes L, Levandovski R, Dantas G, Caumo W, Hidalgo M. Obesity and shift work: Chronobiological aspects. Nutr Res Rev. 2010;23(1):155–168. doi: 10.1017/S0954422410000016. [DOI] [PubMed] [Google Scholar]
- 69.Atkinson G, Fullick S, Grindey C, Maclaren D. Exercise, energy balance and the shift worker. Sports Med. 2008;38(8):671–685. doi: 10.2165/00007256-200838080-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lallukka T, Lahelma E, Rahkonen O, et al. Associations of job strain and working overtime with adverse health behaviors and obesity: Evidence from the Whitehall II study, Helsinki health study, and the Japanese civil servants study. Soc Sci Med. 2008;66(8):1681–1698. doi: 10.1016/j.socscimed.2007.12.027. [DOI] [PubMed] [Google Scholar]
- 71.Sparks K, Cooper C, Fried Y, Shirom A. The effects of hours of work on health: A meta- analytic review. J Occup Organ Psychol. 1997;70:391–408. [Google Scholar]
- 72.da Silva I, Azevedo M, Goncalves H. Leisure-time physical activity and social support among Brazilian adults. J Phys Act Health. 2013;10(6):871–879. doi: 10.1123/jpah.10.6.871. [DOI] [PubMed] [Google Scholar]
- 73.Tada Y, Kawano Y, Maeda I, et al. Association of body mass index with lifestyle and rotating shift work in Japanese female nurses. Obesity (Silver Spring) 2014;22(12):2489–2493. doi: 10.1002/oby.20908. [DOI] [PubMed] [Google Scholar]
- 74.Almajwal A. Correlations of physical activity, body mass index, shift duty, and selected eating habits among nurses in Riyadh, Saudi Arabia. Ecol Food Nutr. 2015;54(4):397–417. doi: 10.1080/03670244.2015.1004400. [DOI] [PubMed] [Google Scholar]
- 75.Morikawa Y, Nakagawa H, Miura K, et al. Effect of shift work on body mass index and metabolic parameters. Scand J Work Environ Health. 2007;33(1):45–50. doi: 10.5271/sjweh.1063. [DOI] [PubMed] [Google Scholar]
- 76.Jansen N, Kant I, van Amelsvoort L, Nijhuis F, van den Brandt P. Need for recovery from work: Evaluating short-term effects of working hours, patterns and schedules. Ergonomics. 2003;46(7):664–680. doi: 10.1080/0014013031000085662. [DOI] [PubMed] [Google Scholar]


