Abstract
Point of care ultrasonography and the related focused assessment with sonography for trauma protocol, if performed by experienced physicians, is a highly sensitive examination, and specific for the detection of free fluids. Different systems and methods have been proposed for training, including simulation as one of the most efficient. This paper presents an ultrasound training system, specifically designed to be used during bedside high fidelity simulation scenarios, that could facilitate the learning process. The development of the proposed system exploited novel rapid prototyping electronic boards as a means to obtain good performances with a low cost. Moreover, the design of the data structure permits the construction of a library that caters for individual needs, with the possibility of adding emergency scenarios, collecting pictures or videos, as well as 3-D volumes. The device has been compared with currently commercial ultrasound simulators and its innovative aspects have been highlighted. Finally, it has been tested during a training session in order to evaluate features, such as realism and user-friendliness.
Keywords: Biomedical image processing, medical simulation, point of care ultrasonography, sensor systems and applications, training, ultrasound
The authors developed a versatile ultrasound simulator that could improve the effectiveness of ultrasound education and the quality of high-fidelity simulation sessions. The simulator exploits low-cost rapid prototyping boards: a microcontroller, an inertial sensor and a RFID reader. The simulator includes novel features regarding the visualization of 3D ultrasound volumes, two separated GUIs for instructor and trainees and a user extensible database of clinical cases.
I. Introduction
Ultrasound examination is rapidly increasing its usage in acute care specialties because of the evolution of Point-of-Care Ultrasonography (PoCUS) [1]: a novel patient’s bedside approach for diagnostic purposes. In emergency medicine, where the needs of rapid assessments are strongly prominent, the ultrasound-assisted examination is the new trend. In this mainframe, several standardized protocol for ultrasound-guided procedures have been proposed, such as the Abdominal and Cardiac Evaluation with Sonography in Shock (ACES) [2] or the Focus Assessment by Sonography in Trauma (FAST). They consist of a series of ultrasound scans focused on the proper windows in order to detect the presence of free fluid on critical traumatized patient.
The aim of FAST examination is to identify hemoperitoneum, hemothorax, or cardiac tamponade [3]. Hence training physicians to perform FAST examination is of great interest, allowing them to accomplish the skills necessary to acquire the adequate window as well as the ability to identify the presence of free fluids [4]. In sonography, image acquisition is complex and operator dependent: the quality of a scan may reflect the degree of training and there is a significant learning curve [5], [6]. Good transducer placement and orientation plus familiarity with US anatomy are required. It has previously been demonstrated that simulation may provide an efficient way of training [7]. Trainees using a US simulator have the opportunity to determine whether to use bedside ultrasound (indications), how to hold and place the probe properly (image generation) and, finally, how to assess scans (image interpretation) within the context of a high fidelity simulation scenario [8], [24]. Such training may involve great expense and should be based on the creation of image database to cover different clinical conditions. Unlike a few years ago, there are now many ultrasound simulators, with different technologies to calculate the orientation and position of the probe and different techniques for generating images. Most of these simulators are essentially designed as stand-alone skill trainers that help beginners to acquire the capability to correctly perform a particular ultrasound technique, e.g. transthoracic or transesophageal echocardiography (TTE, TEE), but they are not compatible with a complete simulation session. Hence, the aim of this work is to propose a versatile ultrasound simulator which could be used both as skill-trainer, for TTE and abdominal examinations, and as an extra tool of high fidelity emergency scenarios.
II. Methods and Procedures
High-fidelity, low-cost, portability, user-friendliness and a large and various case database are the requirements for a complete and efficient simulation system. Unfortunately, several of these features contradict each other, in particular high-fidelity often means an expensive equipment which includes the sensors, the controller boards and the visualization systems. The hardware, as well as the software and the tracking algorithm, here proposed is an upgrade of the prototype described in [9] with an improved care about the trade-off between cost and quality.
A. Hardware
The probe represents the main component of the simulator. It can be used jointly by any holding manikin, or even a human model. It consists of a printed shell of plastic material, containing the electronic boards. The shape of the probe should be as much as possible similar to a real ultrasound transducer, however its dimensions are physically limited by the size of the internal components, so that a meaningful selection criterion considered in the choice of the boards and the sensors has been their dimensions, as described in the following. Because of the symmetry of an ultrasound transducer, the probe is easily made up of two equal parts, built by a 3D printer.
Regarding the internal electronic components, they have to perform the acquisition, the elaboration and the transmission of the data concerning the information about the probe pose, understood as the combination of its position and orientation relative to the manikin. The adopted solution exploits low-cost Radio Frequency Identification (RFID) sensors and Inertial Measurement Units (IMU): such technologies, in the last decade, has undergone a noteworthy diffusion in the context of various medical applications [22], [23]. The position of the probe is tracked using a RFID reader that acquires the code of a set of RFID markers located under the manikin skin, in the points of interest chosen by the user (e.g. those assigned by the FAST protocol). It is worth noting that markers can be placed in any desired anatomic area, so that the simulation scenario is not limited to the sole FAST examination (that typically involves ten landmarks). Therefore, also the number, as well as the position, of the RFID markers can be chosen by the user. The adopted sensor is the InnovationⓇID-12: a programmable low-cost RFID reader, measuring only  mm. Markers are standard 12 byte code, 20 mm diameter. Using these components, the information about the position of the probe on a specific marker can be acquired in a sphere of about 30 mm diameter, fixed in the marker center. Indeed, when the marker is in the field of the reader it exchanges an identification code with the reader itself. The code identifies uniquely the anatomical landmark selected. The distance between two RFID markers should be at least equal to the RFID read range, in order to avoid the acquisition of a wrong code. This limitation does not affect the proper functioning of the system. Indeed, the anatomical areas considered in FAST protocol are typically placed at a distance of at least 5 cm.
mm. Markers are standard 12 byte code, 20 mm diameter. Using these components, the information about the position of the probe on a specific marker can be acquired in a sphere of about 30 mm diameter, fixed in the marker center. Indeed, when the marker is in the field of the reader it exchanges an identification code with the reader itself. The code identifies uniquely the anatomical landmark selected. The distance between two RFID markers should be at least equal to the RFID read range, in order to avoid the acquisition of a wrong code. This limitation does not affect the proper functioning of the system. Indeed, the anatomical areas considered in FAST protocol are typically placed at a distance of at least 5 cm.
The tracking of the probe orientation is a more challenging problem to overcome. Several algorithms for the estimation of the orientation of a rigid body in the Earth Reference System have been developed and applied in different engineering domains [10], [11], including aerospace and robotics. Commonly adopted solutions concern the data coming from the on-board IMU sensors (accelerometer, gyroscope, and magnetometer) properly fused and processed through a nonlinear complementary filter [12], [13]. The study of the orientation tracking algorithm in the context of the ultrasound simulator application is described in detail in [9].
In order to obtain the orientation of the probe relative to the manikin, another IMU, with the same sensor equipment, but connected to the manikin itself, has to be exploited. The difference between the orientations relative to the Earth reference system of the two inertial platform is the desired information.
The InvenSenseⓇMPU9250 is a low-cost, small size IMU, containing the accelerometer, the magnetometer and the gyroscope within a sole microchip: it represents a suitable solution for the requirements of the simulator. Furthermore, this device features a Digital Motion Processor (DMP) capable of processing the orientation tracking algorithm. In more details, technical specifications for the inertial sensors are reported in Table 1.
TABLE 1. Sensor Specifications.
| Sensor | Sensitivity | Full Scale Range |
|---|---|---|
| Accelerometer | 2048 LSB/g | ±16 g |
| Gyroscope | 16.4 LSB/deg/s | ±2000 deg/s |
| Magnetometer | 1.6 LSB/ T T |
±4800 T T |
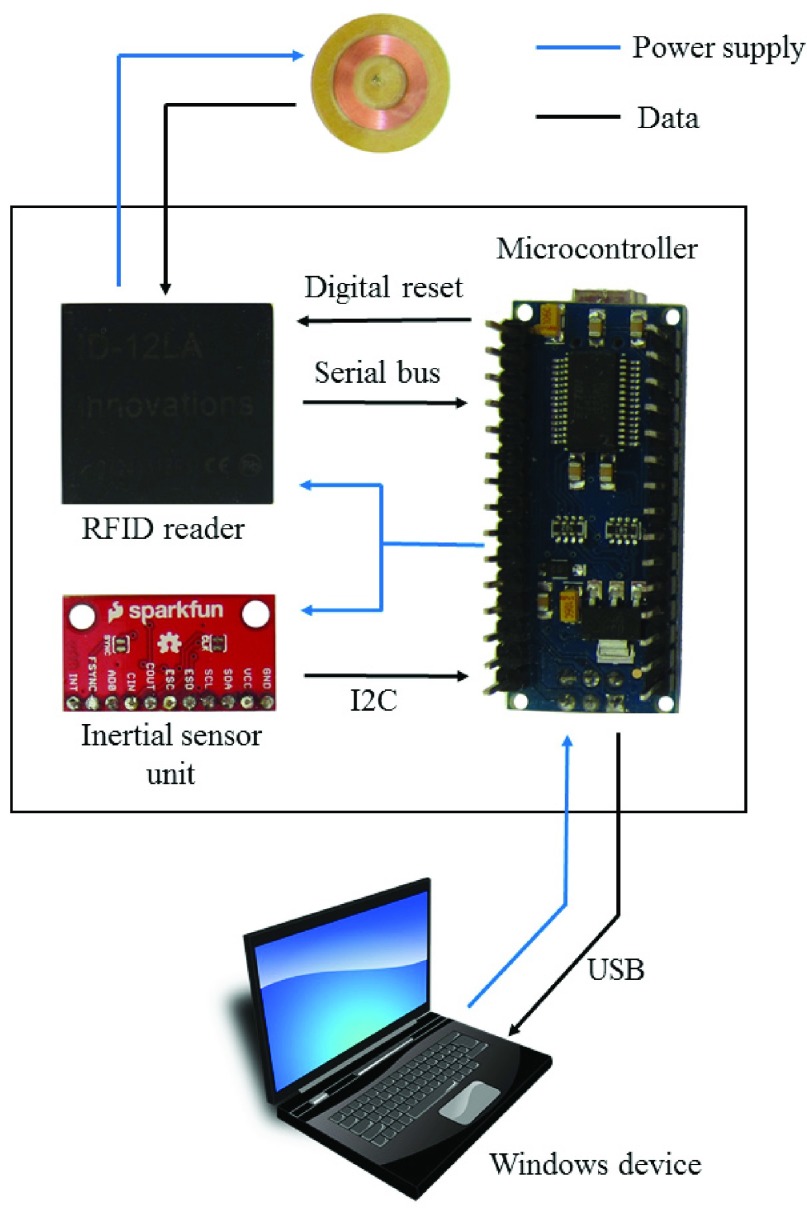
The data acquisition from the RFID reader and from the IMU is performed by the TeensyⓇ3.2: a  mm low-cost microcontroller based on a 32-bit ARM Cortex 72 MHz. This compact board is compatible with the widespread Arduino hardware and software environments [14]. Once the estimation of the probe pose has been performed, the microcontroller send the real-time information to the visualization system, as described in the following, through the serial bus. An overview of the exploited hardware components is reported in Figure 1 and Figure 2.
mm low-cost microcontroller based on a 32-bit ARM Cortex 72 MHz. This compact board is compatible with the widespread Arduino hardware and software environments [14]. Once the estimation of the probe pose has been performed, the microcontroller send the real-time information to the visualization system, as described in the following, through the serial bus. An overview of the exploited hardware components is reported in Figure 1 and Figure 2.
FIGURE 1.
The hardware components of the system, with the power supply and information flow charts. From up to down: the marker, the probe with its inner boards (the RFID reader, the IMU and the microcontroller), and the Windows device hosting the application.
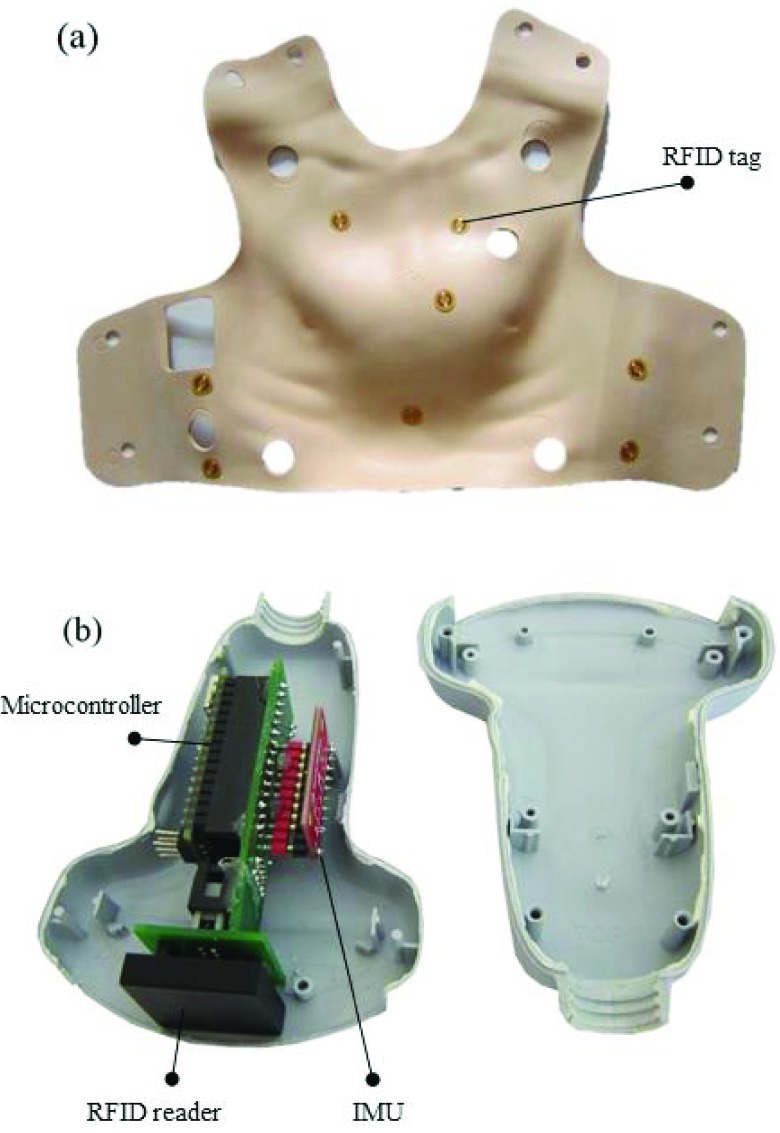
FIGURE 2.
The RFID markers placed under the manikin skin (a) and the assembled components into the simulator probe (b).
B. Experiments on DMP Accuracy
The accuracy of the relative orientation probe-manikin depends on the accuracy of the estimation provided by the DMPs integrated into the two IMU boards exploited to track the probe and the manikin. Therefore, the performance of DMP as inertial tracker has been studied by means of the following experiment.
A probe containing the microcontroller and the IMU has been fixed to the end-effector of a robot manipulator PUMA260 so that the IMU reference system is initially aligned to the robot reference system. It can be assumed that the forward robot kinematics provides the real-time reference value for the orientation of the end-effector and the IMU. Then, the robot end-effector has been forced to move from an initial orientation of  [0, 0, 0] deg, in terms of nautical angles roll, pitch, yaw, to an orientation of
[0, 0, 0] deg, in terms of nautical angles roll, pitch, yaw, to an orientation of  [45, 0, 0] deg and then come back to
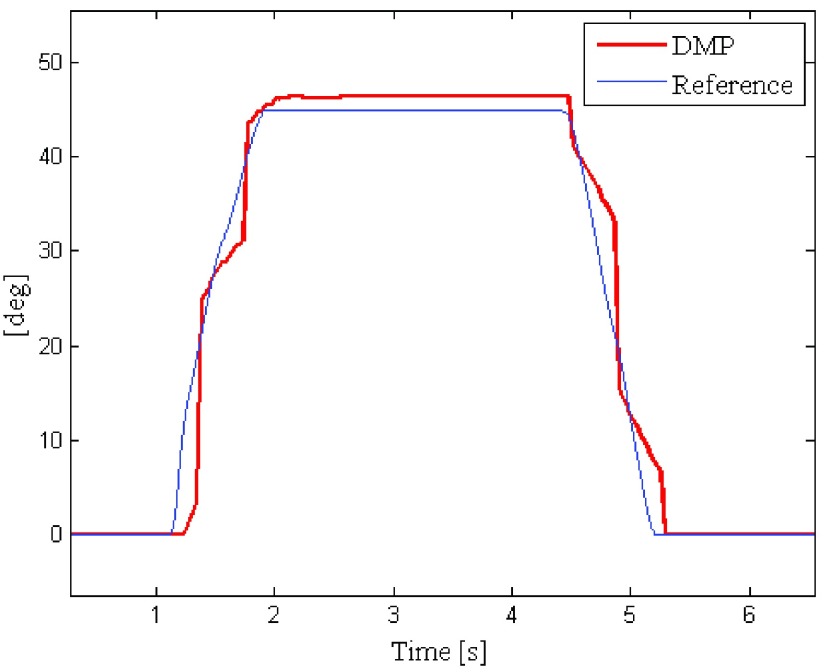
[45, 0, 0] deg and then come back to  . In the meanwhile, the orientation estimations of the DMP have been acquired. Figure 4 shows the comparison between the robot reference signal and the DMP estimation, considering the transient of the roll angle estimation. The signals have been synchronized.
. In the meanwhile, the orientation estimations of the DMP have been acquired. Figure 4 shows the comparison between the robot reference signal and the DMP estimation, considering the transient of the roll angle estimation. The signals have been synchronized.
FIGURE 4.
The DMP estimations during the transient of the roll angle, compared to the robot reference signal.
The percent root mean square error (RMSE%) and the variance of the error between the DMP estimations and the reference robot signal have been computed as performance indices considering the steady condition after the first robot movement. Results are reported in Table 2. The obtained values demonstrates that the DMP performances satisfy the requirement of the application. Indeed, it has been observed that even expert users cannot detect errors in image visualization for values of RMSE% < 5%.
TABLE 2. Performance Indices of DMP Estimations.
| Index | Value |
|---|---|
| RMSE | 1.2 deg |
| RMSE% | 2.8 % |
| variance | 0.01 deg2 |
C. The Visualization System
The visualization system has been developed as a versatile tool, as it allows users to interact with static images, videos or 3D interpolated volumes, coming either from real ultrasound scans or from computer graphic virtualization, depending on the availability of the database.
The displaying of a static image or a video does not require any particular elaboration. However, the software permits to insert different videos or images within a single view: the selection of the proper dataset depends on the current probe orientation. As a result, the user can visualize, for example, a video for the sagittal plane and another one for the longitudinal plane, concerning the same anatomical landmark.
3D volumes are processed by the visualization system using two interpolative steps. Firstly, the volume is created by fetching from the database the related set of 2D slices, all of them having the same cutting plane. Afterwards, the resulting volume is real-time sliced, along the plane properly tilted on the basis of the information about the probe orientation, so that the current image can be displayed. The choice of generating volumes from slices instead of managing 3D models directly, is due to the user difficulties to obtain that kind of dataset.
Furthermore, in order to overcome this problem, a novel feature has been implemented on the simulator: the so-called pseudo-volume. It is created by acquiring a real video of a pathological case: the operator has to locate the ultrasound transducer on the desired anatomical landmark and rotate it along its axis of approximately 360 deg. Once the video has been acquired and inserted into the simulator database, the visualization system can select the proper frame run-time, basing on the probe orientation. The main advantages of pseudo-volumes are the easiness and the quickness of acquisition. Indeed, medical operators can get the basic video during their normal activity, without any risk for patient health. Pseudo-volumes offer a very realistic simulation when the probe is rotated along its axis, but this degree of freedom is the only one that can be processed by the visualization system. When the probe is tilted along the other axes, the orientation changing effects are not simulated correctly.
Further development are required to include four-dimensional dataset, as volumes or pseudo-volumes does not fit for dynamic dataset visualization, in which the time is a prominent component (e.g. cardiac ultrasound).
The graphic tool exploited by the simulator is the Visualization Toolkit (VTK): an open source set of graphic libraries commonly used for scientific data processing [25]. It provides powerful and optimized functions to manage huge dataset and to render appropriate views on the screen.
D. Instructor and Student Side Software Interfaces
According to the increasing demand of standardized proficiency assessment procedures [15], the software provides a typical instructor-student behavior allowing a possible usage as a skill-trainer device [16]. Furthermore, the proposed simulator features two separate Graphical User Interfaces (GUIs) that make the device compatible with a complete high-fidelity simulation session [24].
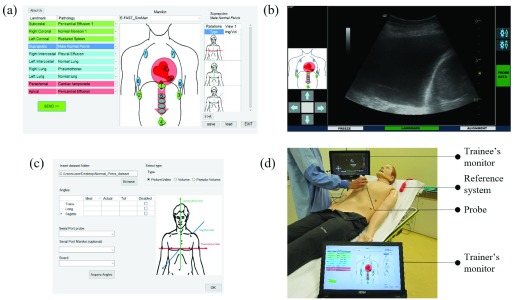
Two different applications have been developed in Microsoft .NETⓇframework so that they can run on any Microsoft Windows device. One application is executed on the instructor device, and allows the trainer to select the desired scenario from the case database. The screen is divided into three sections: the central one shows a picture of the selected manikin with its numbered landmarks. A table itemizing the landmarks and the associated pathology is located on the left, whereas the table on the right summarizes the information about the available dataset for a selected couple landmark-pathology. Once the instructor has choose the desired scenario, it can be transmitted to the student application through a network socket. Figure 3 (a) shows the instructor’s GUI.
FIGURE 3.
The trainer’s GUI (a), the trainee’s GUI with the visualization of an interpolated image (b), the user-extensible database editor (c) and the system set-up (d) which includes the instructor’s and the trainee’s devices, the probe and the manikin reference system.
The student application hosts the database and the visualization system, as its main purpose is the simulation of the ultrasound monitor. It is connected to the probe microcontroller via serial bus and it receives the current information about the probe pose, so that the visualization system can generate the proper view. The trainee can interact with the system freezing the current viewand performing some measurements as in a real ultrasound monitor.
The application has a multithread architecture, as multiple operations have to be perform at the same time. The core threads take care of the communication with the instructor application, as well as the transmission of the current dataset to the visualization thread, once the on-line acquisition of the probe orientation has been performed. On the other hand, the visualization thread implements the VTK pipeline and provides the rendered viewto the monitor. Figure 3 (b) depicts the trainee’s GUI, while Figure 3 (d) shows the overall system set-up.
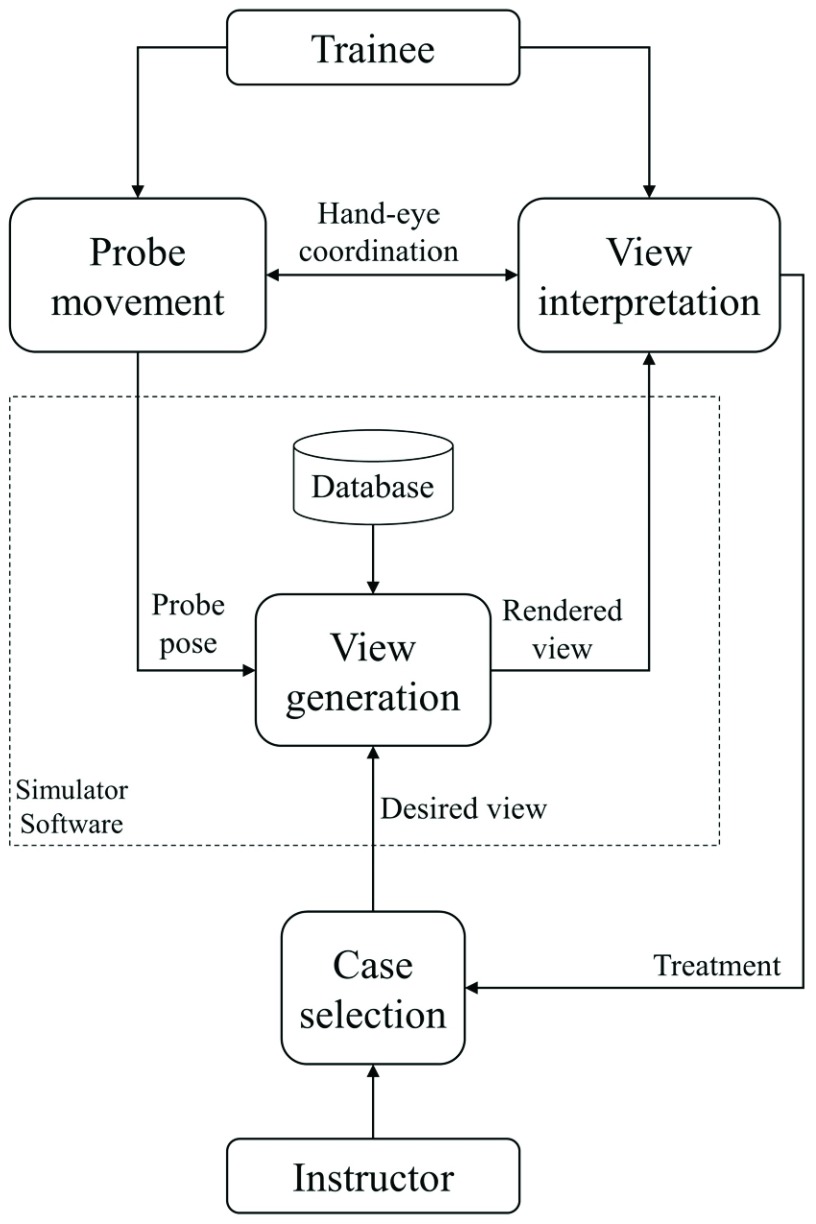
E. Performing the Simulation
As mentioned above, the choice of developing two separated GUIs allows an effective usage of the system in high-fidelity simulation scenarios. Indeed, a typical emergency scenario is represented by means of two separated environments: the director room, where the instructor handles the manikin parameters and the simulation room, where the trainee examines the manikin representing the patient. It is often required that the trainee have no contact with the trainer during the session, but the instructor can observe the scene and modify the manikin parameters, on the basis of the trainee’s actions. Therefore, the proposed simulator can be applied to that kind of scenarios as follows:
-
1)
The instructor selects the desired case, which is loaded by the visualization system from the database, so that the desired view can be generated on the trainee’s monitor, on the basis of the probe pose information;
-
2)
The trainee uses the simulator probe to perform the ultrasound examination on the manikin. It mainly regards the hand-eye coordination in the simultaneous actions of moving the probe and interpreting the visualized view.
-
3)
The trainee performs a treatment on the patient, based on the diagnosis;
-
4)
The instructor selects a different case in response to the treatment, so that the trainee can analyze the real-time effect of its actions.
Figure 5 shows the flowchart of typical high-fidelity simulation session.
FIGURE 5.
The flowchart of a simulation session, where the instructor changes the simulation parameter in real-time, on the basis of the trainee’s actions.
F. The User-Extensible Database
The simulator implements a user-friendly editor, whereby the operator can manage the database by adding, removing or modifying cases. Therefore, the user is stimulate in acquiring images, videos, volume slices, and pseudo-volumes from real examinations, in order to customize the database according to its own needs. The collected material can be easily shared among users. The operator who performs the acquisition of a data set from the patient has to provide a sufficiently accurate description of probe position and orientation during the acquisition. A video can be acquired when the probe is motionless and directly inserted into the database, while a volume can be elaborated from the frame sequence of a video acquired by means of a probe translation (of about 2 cm). Similarly, a pseudo-volume is generated on the basis of the frame sequence of a video in which the probe rotates around its axis. Figure 3 (c) shows the editor of the user-extensible database.
III. Comparison of Ultrasound Simulators
An overview on similar computer-based ultrasound simulators can be found in [17], where the authors describe the main features of their design. In this work, an updated comparison is shown, but the focus is placed on the characteristics of each device from the user point of view. The simulators included into the comparison are: SonoSimⓇ, CAE VimedixⓇ, SchallwareⓇ [18], HearthWorksⓇ [19], SimuLab SonoManⓇ, as well as the proposed simulator.
The ultrasound visualization system is the first key-point considered: CAEVimedix and HeartWorks exploit generative model-based views, coming from the elaboration of a virtual model of the patient. The realism depends largely on the fidelity of the model and the building of the model itself is a time consuming procedure, which restrains the diffusion of multiple cases. Schallware, SonoSim and the proposed simulator use interpolative methods to process real datasets characterized by more than two dimensions. However, it is worth observing that the proposed simulator can visualize also generative model-based views, pre-elaborated in form of image sequences. This feature allows the usage of the simulator for basic skill training, while in a simulation session users tend to prefer interpolated real views, because of their higher realism. In this context, another peculiarity of the proposed system is the opportunity to visualize static images, videos, volumes, or pseudo-volumes, depending on the available data sets.
The second feature analyzed is the probe tracking system. Almost every simulator implements the pose tracking, including position and orientation of the probe, but this result is achieved exploiting different methods. The trade-off is between costs and tracking accuracy: Schallware, CAE Vimedix, and HeartWorks simulators use an expensive electromagnetic system to record the probe pose relative to the manikin. A device rigidly connected to the manikin generates an electromagnetic field. Then, the probe perturbs the field as a function of its position and orientation, so that the probe pose relative to the manikin can be calculated in every point inside the field. The effect of electromagnetic disturbances could be a drawback.
The SonoSim and the proposed simulators have a cheaper RFID - IMU system that provides a discretized solution for the position as well as a less accurate estimation of the orientation, though achieving satisfactory performances. The Simulab SonoMan can track only the probe position.
Some simulators (i.e. the SonoSim and the Simulab Sonoman) do not include a reference system for the manikin, which is instead exploited by the proposed system, CAE Vimedix, Schallware and HeatWorks, to allow the real-time tracking of the relative orientation probe-manikin. Simulators without that feature require the execution of an alignment procedure every time the manikin is accidentally moved.
A further index of comparison is the ultrasound techniques which can be performed. As mentioned above, the proposed device can simulate TTE and abdominal examinations. The same applications are related to Schallware, SonoSim and Simulab, while Heartworks and CAE Vimedix are designed for TTE and TEE.
Finally, two noteworthy features that characterize the proposed simulator with respect to the others are highlighted. Firstly, the two separated GUIs make the system compatible with a high-fidelity simulation session. Secondly, the extensible database offer the user the opportunity to freely manage the database, while most of commercial devices provide a limited number of case modules, not completely free available.
Table 3 shows the comparison among the considered simulators. The last column reports an approximate cost analysis, which considers only the device cost, and not the additional modules. For the proposed simulator the commercial cost is not yet specified, but since the overall hardware cost is about 300 $, it can be expected that a commercial version would cost ten times less than the cheapest mentioned alternative.
TABLE 3. The Comparison Among the Computer-Based Ultrasound Simulators.
| SIMULATOR | Visualization datasets | Tracking System | Reference System | Instructor/Student Interface/s | Database | Medical Application | Cost ($) |
|---|---|---|---|---|---|---|---|
| Proposed Simulator | 2D images or video, 3D interpolative volumes or pseudo-volumes | Position: RFID Orientation: IMU | Yes | Two separated | User extensible | TTE, abdominal | – |
| CAE Vimedix | 4D model-based volumes | Position + Orientation: Magnetic system | Yes | Single | Limited number of modules | TTE, TEE | ~60000 |
| Schallware | 3D and 4D interpolative volumes | Position + Orientation: Magnetic system | Yes | Single | Limited number of modules | TTE, abdominal | ~28000 |
| HeartWorks | 4D model-based volumes | Position + Orientation: Magnetic system | Yes | Single | Limited number of modules | TTE, TEE | ~75000 |
| SonoSim | 3D interpolative volumes | Position: RFID Orientation: IMU | No | Single | Limited number of modules | TTE, abdominal | ~20000 |
| Simulab SonoMan | 2D videos | Position | No | Single | Limited number of modules | TTE, abdominal | ~7000 |
IV. Results
The simulator has been tested and evaluated during a training session in the context of the  national Workshop
national Workshop
on Trauma: Update and Organization, held in Bologna (Italy) in February 2015. A group of physicians from the Maggiore Hospital of Bologna, with a prominent ultrasound experience, held a course on the usage of the ultrasound examination in trauma, particularly focused on the FAST protocol. The participants were 15 anesthesiologist, coming from different national hospitals, with a very low ultrasound experience. During the morning, they were given a theoretical lesson on FAST background and methods, whereas in the afternoon, they were subdivided into three workstations, each of them consisting of a simulator and a tutor, who selected the desired case and assists the residents training. Every data set was previously acquired by the tutor itself, in the form of real ultrasound scans (images, videos, and 3D pseudo-volumes).
The manikins used jointly by the simulator were the SimManⓇLaerdal, a well tested [20] high-fidelity patient simulator.
The trainees had to apply the FAST protocol by positioning and orientating the probe correctly, and they had the proper monitor response.
At the end of the training session, the participants were asked to evaluate the simulator. The proposed 5-point Likert-scale questionnaire about the impression and usefulness of the simulator follows the guidelines described in [21] but adapted for the ultrasound simulation. The questionnaire is reported in the following, and Table 4 shows the results.
TABLE 4. Questionnaire Results.
| Strongly Agree | Agree | Undecided | Disagree | Strongly Disagree | |
|---|---|---|---|---|---|
| Simulator Design | |||||
| 1 | 40% | 46.7% | 6.7% | 6.7% | 0% |
| 2 | 46.7% | 26.7% | 13.3% | 13.3% | 0% |
| 3 | 40% | 33.3% | 6.7% | 20% | 0% |
| Simulator Usefulness | |||||
| 4 | 40% | 33.3% | 0% | 20% | 6.7% |
| 5 | 46.7% | 40% | 6.7% | 6.7% | 0% |
| 6 | 40% | 53.3% | 0% | 6.7% | 0% |
| 7 | 40% | 33.3% | 20% | 6.7% | 0% |
| 8 | 40% | 40% | 13.3% | 0% | 6.7% |
Questionnaire:
-
1)
What is your opinion about the appearance of the simulator?
-
2)
What is your opinion about the realism of the simulator?
-
3)
What is your opinion about the user-friendliness of the simulator?
-
4)
What is your opinion about the simulator’s usefulness in improving hand-eye coordination?
-
5)
The simulator can become a useful instrument to train novice physicians in ultrasound techniques.
-
6)
The simulator is a useful instrument to teach basic ultrasound procedures.
-
7)
The simulator can become a useful instrument to measure ultrasound procedure performance.
-
8)
The simulator was a useful instrument to improve ultrasound skills.
The first three questions concern the participants’ impression about the appearance, the fidelity, and the user-friendliness of the simulator: most responses (more than 70%) are good/excellent (4/5 Likert-scale points), whereas less than the 20% of the participants gave a medium-bad score (2 points). This result validates the simulator as a user-friendly device and motivate further improvements, particularly in the visualization of dynamic 4D datasets, in which the time is a prominent dimension. Volumes or pseudo-volumes are not a suitable solution to represent them, as their acquisition procedure entails the loss of time evolution.
The other questions are about the usefulness of the simulator. Also the results in this section are quite positive: indeed, about the 80% of the participants states that the simulator is a useful instrument in medical education (teaching as well as learning) and training. Moreover, it could be exploited as an indicator of ultrasound procedure performances.
Further studies are needed to verify whether the system has positive long-term learning effect.
V. Conclusion
The authors developed a versatile ultrasound simulator, in order to improve the effectiveness of ultrasound education and the quality of high-fidelity simulation scenarios.
Despite its low cost, the proposed system collects the main advantages of the currently commercially available devices and implements some novel feature concerning the probe tracking, the visualization of ultrasound 3D volumes, and the user extensible case database.
The simulator has been tested during a training session, in which several expert physicians helped a group of novice physicians to perform the simulation of the Point of Care Ultrasonography. The participants’ feedback has been reported in a questionnaire about their first impressions on the design and the usage of the simulator. As a result, most of the participants assert that the proposed simulator is a useful tool to improve ultrasound skills.
Potential issues that could be faced during the commercialization involve the creation of a large and complete database to attach to the simulator. Indeed, certain pathologies are difficult to find because of their rarity and other pathologies can be difficult to acquire because of the urgent treatment required by the patient. Nevertheless, users are always able to customize the system with their own database of images, acquired during clinical practices. Moreover, the feedback of users belonging to different medical disciplines can be useful to properly extend the usage of the simulator in such disciplines.
Further developments could concern the visualization of time-varying ultrasound volumes and the inclusion of a transesophageal echocardiographic simulation system. In addition, the compression ultrasonography, a technique used to diagnose deep vein thrombosis, can be implemented by integrating an additional force sensor.
Biographies

Saverio Farsoni received the M.Sc. degree in informatics and automation engineering and the Ph.D. degree in science of engineering from the University of Ferrara, in 2012 and 2016, respectively. Since 2012, he has been focused on ultrasound simulation. He has published about 10 refereed journal and conference papers. His research activities include robotics, control systems, fault diagnosis, fault tolerant control, and system identification.

Luca Astolfi received the master’s degree in electronic engineering from the University of Bologna, in 2002. He is currently a Researcher with the University of Ferrara. His research centers around high fidelity medical simulation.

Marcello Bonfè received the M.Sc. degree in electronic engineering in 1998, and the Ph.D. degree in information engineering in 2003. He is an Assistant Professor of Automatic Control with the University of Ferrara, Italy. He has published over 70 refereed journal and conference papers. His main research interests include the formal verification of discrete event systems, modelling and control of mechatronic systems, fault detection and fault tolerant control, and robotics and motion planning.

Savino Spadaro is currently a Researcher of Anesthesia and Intensive Care with the University of Ferrara, Italy. He has been involved in several research project in Critical Care Research since 2013. He is one of the certified Instructor of Simulation with the Center of Ferrara. His current focus is on mechanical ventilation and ultrasound simulation, with a research interest in the respiratory medicine and medical education in Italy.

Carlo Alberto Volta is the Director of the Section of Anesthesia and Intensive Care with S. Anna University Hospital, University of Ferrara, Italy, and the Director of the School of Specialization in Anaesthesia and Intensive Care with the University of Ferrara, where he is a Teacher of Anaesthesia and Intensive Care Medicine. He was a Research Fellow with the Meakins-Christie Laboratories, McGill University, Montreal, Canada, from 1993–1995. His research activities include respiratory physiology and pathophysiology, mechanical ventilation, respiratory muscle fatigue, COPD, weaning from mechanical ventilation, fluids therapy, and simulation in healthcare. He is a Senior Editor of the Journal of Inflammation and a Reviewer of the European Respiratory Journal, Intensive Care Medicine, Thorax, Anesthesia Analgesia, Respiration, Acta Anaesthesiologica Scandinavica, Minerva Anestesiologica, Molecular Biology Reports, the Journal of Inflammation, Emergency Medicine International, Multidisciplinary Respiratory Medicine, the Journal of Clinical Monitoring and Computing, and PLOS ONE.
He is fellow of the European Respiratory Society, the European Society of Intensive Care Medicine, and the Italian Society of Anaesthesia, Analgesia, and Intensive Care.
Funding Statement
This work was supported by the Arcispedale Sant’Anna of Cona, Ferrara, Italy.
References
- [1].Vignon P., “PRO: Physician-performed ultrasound: The time has come for routine use in acute care medicine,” Anesthesia Analgesia, vol. 115, no. 5, pp. 999–1003, Nov. 2012. [DOI] [PubMed] [Google Scholar]
- [2].Atkinson P. R., et al. , “Abdominal and cardiac evaluation with sonography in shock (ACES): An approach by emergency physicians for the use of ultrasound in patients with undifferentiated hypotension,” Emerg. Med., vol. 26, no. 2, pp. 87–91, 2009. [DOI] [PubMed] [Google Scholar]
- [3].Gillman L. M., Ball C. G., Panebianco N., Al-Kadi A., and Kirkpatrick A. W., “Clinician performed resuscitative ultrasonography for the initial evaluation and resuscitation of trauma,” Scandinavian J. Trauma, Resuscitation Emergency Med., vol. 17, no. 1, p. 34, 2009, doi: 10.1186/1757-7241-17-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Royse C. F., Canty D. J., Faris J., Haji D. L., Veltman M., and Royse A., “Core review: Physician-performed ultrasound: The time has come for routine use in acute care medicine,” Anesthesia Analgesia, vol. 115, no. 5, pp. 1007–1028, 2012. [DOI] [PubMed] [Google Scholar]
- [5].Freeman P., “The role of ultrasound in the assessment of the trauma patient,” Austral. J. Rural Health, vol. 7, no. 2, pp. 85–89, May 1999. [DOI] [PubMed] [Google Scholar]
- [6].Oxorn D. and Pearlman A., “CON: Physician-performed ultrasound: The time has come for routine use in acute care medicine,” Anesthesia Analgesia, vol. 115, no. 5, pp. 1004–1006, 2012. [DOI] [PubMed] [Google Scholar]
- [7].Parks A. R., Atkinson P., Verheul G., and LeBlanc-Duchin D., “Can medical learners achieve point-of-care ultrasound competency using a high-fidelity ultrasound simulator?: A pilot study,” Critical Ultrasound J., vol. 19, no. 1, pp. 5–9, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Maran N. J. and Glavin R. J., “Low- to high-fidelity simulation—A continuum of medical education?” Med. Educ., vol. 37, no. s1, pp. 22–28, Nov. 2003. [DOI] [PubMed] [Google Scholar]
- [9].Farsoni S., Astolfi L., Bonfè M., and Spadaro S., “Design of an ultrasound simulator with probe pose tracking and medical dataset processing and visualization,” IFAC-PapersOnLine, vol. 48, no. 20, pp. 377–382, 2015. [Google Scholar]
- [10].Madgwick S. O. H., Harrison A. J. L., and Vaidyanathan R., “Estimation of IMU and MARG orientation using a gradient descent algorithm,” in Proc. IEEE Int. Conf. Rehabil. Robot. (ICORR), Jun. 2011, pp. 1–7. [DOI] [PubMed] [Google Scholar]
- [11].Premerlani W. and Bizard P., “Direction cosine matrix IMU: Theory,” in Proc. DIY DRONE USA, 2009. [Google Scholar]
- [12].Mahony R., Hamel T., and Pflimlin J.-M., “Nonlinear complementary filters on the special orthogonal group,” IEEE Trans. Autom. Control, vol. 53, no. 5, pp. 1203–1218, Jun. 2008. [Google Scholar]
- [13].Hua W., et al. , “Polyphase FIR complementary filters for control systems,” in Proc. Spring Topical Meeting Control Precis. Syst., Cambridge, U.K., Apr. 2004, pp. 1–6. [Google Scholar]
- [14].D’Ausilio A., “Arduino: A low-cost multipurpose lab equipment,” Behavior Res. Methods, vol. 44, no. 2, pp. 305–313, 2012. [DOI] [PubMed] [Google Scholar]
- [15].Monsky W. L., et al. , “Using a sonographic simulator to assess residents before overnight call,” Amer. J. Roentgenol., vol. 178, no. 1, pp. 35–39, 2002. [DOI] [PubMed] [Google Scholar]
- [16].Mircea P.-A., Badea R., Fodor D., and Buzoianu A. D., “Using ultrasonography as a teaching support tool in undergraduate medical education-time to reach a decision,” Med. Ultrasonograph., vol. 14, no. 3, pp. 211–216, 2012. [PubMed] [Google Scholar]
- [17].Blum T., Rieger A., Navab N., Friess H., and Martignoni M., “A review of computer-based simulators for ultrasound training,” Simul. Healthcare, J. Soc. Simul. Healthcare, vol. 8, no. 2, pp. 98–108, 2013. [DOI] [PubMed] [Google Scholar]
- [18].Maul H., Scharf A., and Sohn C., “Was kann der sonotrainer-ultraschallsimulator?” Der Gynäkologe, vol. 39, no. 11, pp. 870–877, Nov. 2006. [Google Scholar]
- [19].Bose R., et al. , “Transesophageal echocardiography simulator: A new learning tool,” J. Cardiothoracic Vascular Anesthesia, vol. 23, no. 4, pp. 544–548, 2009. [DOI] [PubMed] [Google Scholar]
- [20].Swamy M., Sawdon M., Chaytor A., Cox D., Barbaro-Brown J., and McLachlan J., “A study to investigate the effectiveness of SimMan as an adjunct in teaching preclinical skills to medical students,” BMC Med. Edu., vol. 14, no. 1, p. 231, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Cha J., et al. , “The box simulator is useful for training novice endoscopists in basic endoscopic techniques,” Yonsei Med. J., vol. 53, no. 2, pp. 304–309, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Huang H., et al. , “RFID tag helix antenna sensors for wireless drug dosage monitoring,” IEEE J. Transl. Eng. Health Med., vol. 2, pp. 1–8, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Pande A., Zhu J., Das A. K., Zeng Y., Mohapatra P., and Han J. J., “Using smartphone sensors for improving energy expenditure estimation,” IEEE J. Transl. Eng. Health Med., vol. 3, pp. 1–12, 2015, doi: 10.1109/JTEHM.2015.2480082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Butcher C., et al. , “Emergencies and resuscitation in the catheter laboratory: High-fidelity simulation as a training tool to improve multidisciplinary team communication and confidence,” Circulation, vol. 130, no. 2, p. A263, 2014. [Google Scholar]
- [25].Schroeder W., Martin K., and Lorensen B., An Object-Oriented Approach To 3D Graphics, vol. 429 Englewood Cliffs, NJ, USA: Prentice-Hall, 1997. [Google Scholar]