Abstract
Purpose
Low back pain (LBP) is the most disabling condition worldwide. Although LBP relates to different spinal pathologies, vertebral bone marrow lesions visualized as Modic changes on MRI have a high specificity for discogenic LBP. This review summarizes the pathobiology of Modic changes and suggests a disease model.
Methods
Non-systematic literature review.
Results
Chemical and mechanical stimulation of nociceptors adjacent to damaged endplates are likely a source of pain. Modic changes are adjacent to a degenerated intervertebral disc and have three generally interconvertible types suggesting that the different Modic change types represent different stages of the same pathological process, which is characterized by inflammation, high bone turnover, and fibrosis. A disease model is suggested where disc/ endplate damage and the persistence of an inflammatory stimulus (i.e., occult discitis or autoimmune response against disc material) create predisposing conditions. The risk to develop Modic changes likely depends on the inflammatory potential of the disc and the capacity of the bone marrow to respond to it. Bone marrow lesions in osteoarthritic knee joints share many characteristics with Modic changes adjacent to degenerated discs and suggest that damage-associated molecular patterns and marrow fat metabolism are important pathogenetic factors. There is no consensus on the ideal therapy. Non-surgical treatment approaches including intradiscal steroid injections, anti-TNF-α antibody, antibiotics, and bisphosphonates have some demonstrated efficacy in mostly non-replicated clinical studies in reducing Modic changes in the short term, but with unknown long-term benefits. New diagnostic tools and animal models are required to improve painful Modic change identification and classification, and to clarify the pathogenesis.
Conclusion
Modic changes are likely to be more than just a coincidental imaging finding in LBP patients and rather represent an underlying pathology that should be a target for therapy.
Keywords: Low back pain, Modic changes, Bone marrow lesion, Endplate damage, Pathobiology
Introduction
Low back pain (LBP) is the world’s most disabling condition with detrimental consequences due to increased use of health-care services and work disability [1]. Although LBP relates to different spinal pathologies, vertebral bone marrow lesions (BML) visualized as Modic changes (MC) on magnetic resonance imaging (MRI) have a high specificity for discogenic LBP [2]. Numerous clinical studies have investigated the prevalence, natural history, risk factors, and pain association of MC. However, comparably few studies have investigated the pathobiology of MC. Recent data indicate infectious and autoimmune etiologies, both of which presuppose structural damage of the disc. Additional insight comes from the study of BML in the femur/tibia of an osteoarthritic knee joint, which shares many characteristics with MC. This article reviews the current understanding of the pathobiology of MC and suggests a hypothetical disease mechanism. Uncovering this mechanism will be central for solidifying the role of MC in LBP.
Clinical presentation of Modic changes
BML are pathological changes of the BM composition. A subgroup of vertebral BML evident with MRI have been termed MC [3]. Modic changes are MRI signal intensity changes in the vertebral bone marrow (BM) that reflect lesions which are not related to marrow malignancy, pyogenesis, or seropositive rheumatic disorders [3, 4]. Three types of MC have been described based on their appearance in T1-weighted (T1w) and T2-weighted (T2w) images (Fig. 1). Modic changes type 1 (MC1) are hypointense on T1w and hyperintense on T2w. Modic changes type 2 (MC2) are hyperintense on T1w and hyper- or isointense on T2w. Modic changes type 3 (MC3) are hypointense on T1w and T2w [3]. However, the identification and classification can depend on the MRI field strength [105].
Fig. 1.
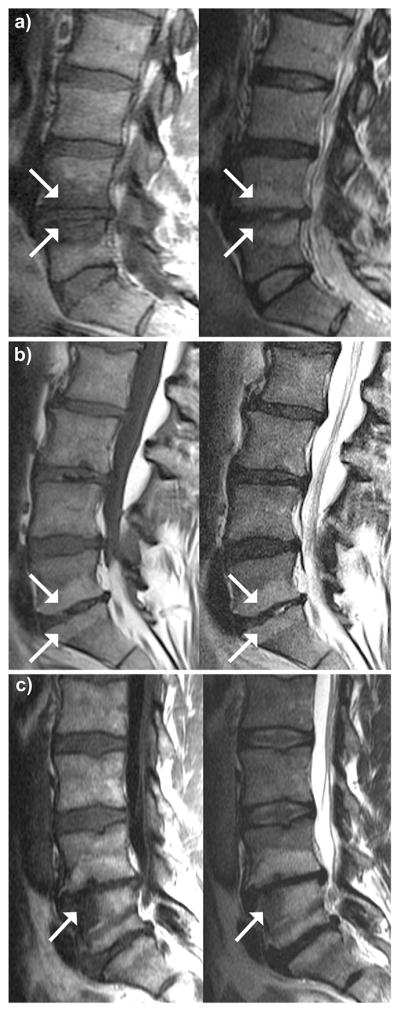
Mid-sagittal T1-weighted (left) and T2-weighted images (right) of lumbar spines showing the three types of Modic changes (arrows). a Modic change type 1 at inferior L4 and superior L5. b Modic change type 2 at inferior L5 and superior S1. c Mixed Modic change type 2/3 at superior-anterior L5 with arrowhead pointing at Modic change type 3. Modic changes type 2 are also present at inferior L4, inferior L5, and superior S1. Pure Modic changes type 3 are rare. No such MRI scans were available to us
Prevalence, natural history, and risk factors for MC have been extensively studied and are reviewed elsewhere [5–10]. Overall, MC prevalence is high in LBP patients (43 % median prevalence in a meta-study) compared to only 6 % median prevalence of the asymptomatic population [5]. Of the different MC types, MC1 has been more associated with LBP than the others [2, 11]. Modic changes are more prevalent and more severe at the lower lumbar levels (L4–S1) [3, 12], are more prevalent in the anterior third of the vertebra [13, 14], are generally symmetric cephalad and caudad to a particular disc [15], and are commonly associated with disc degeneration (DD) [16], DD severity [17], and disc herniations [18].
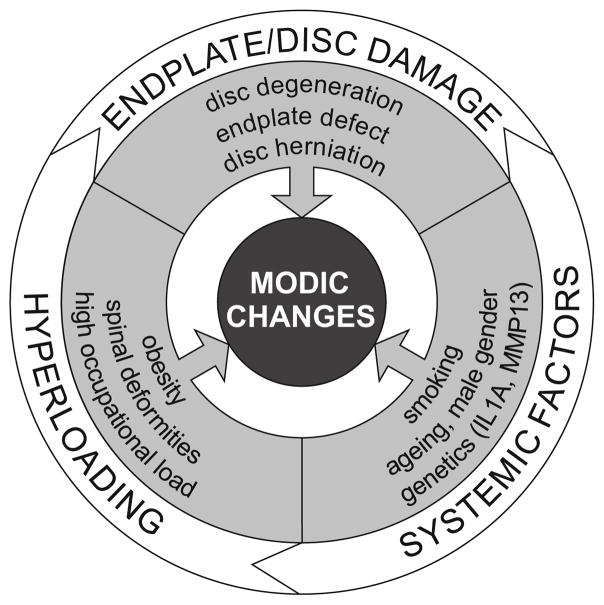
Elucidation of MC etiology is hindered by the dynamic clinical presentation and multifactorial pathophysiology. MC1 and MC2 are interconvertible over time and can eventually convert to MC3 [9, 10, 17]. About 20 % of the lesions are mixed-type MC1/2 or MC2/3 [9, 36]. Risk factors for MC can be classified into disc/endplate damage (DD, disc herniation, endplate defects), systemic factors (smoking, ageing, male gender, genetics), and hyperloading (obesity, spinal deformities, high occupational load) [7, 14–24] (Fig. 2). The unidentified and multifactorial nature of MC is especially true for MC1; conversely, MC2 mainly associates with hyperloading and systemic factors [7, 20, 22, 25].
Fig. 2.
Risk factors for Modic changes. Systemic factors may also affect hyperloading and disc/endplate damage pathologies. Hyper-loading may also affect disc/endplate damage
Growing evidences suggest that LBP patients with MC have a clinically different presentation than LBP patients without MC [16]: LBP patients with MC report a greater frequency and duration of LBP episodes and seek care more often [5]. This suggests different pain generators and potentially different responses to treatments [26–28]. For example, recent studies show that the presence of MC1 with chronic LBP is associated with a poor outcome to conservative treatment [6, 29]. MC1 patients also had worse outcomes after discectomy [30], which underscores the role of the vertebra as a possible pain generator. While the reason for vertebrogenic pain in MC is unknown [5], increased numbers of PGP-9.5 nerve fibers and TNF-α positive cells in MC1 and MC2 endplates may be important [31, 32] MC symptoms may also relate to psychosocial and genetic factors [33]. However, due to the absence of a treatment consensus for LBP patients with MC, insufficient clinical evidence currently exists supporting the effect of MC on the clinical outcome in patients with discogenic LBP [6].
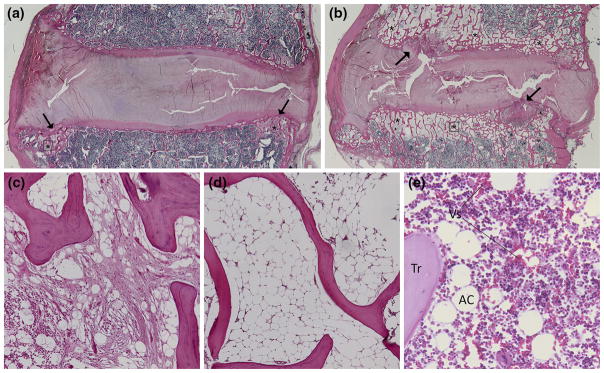
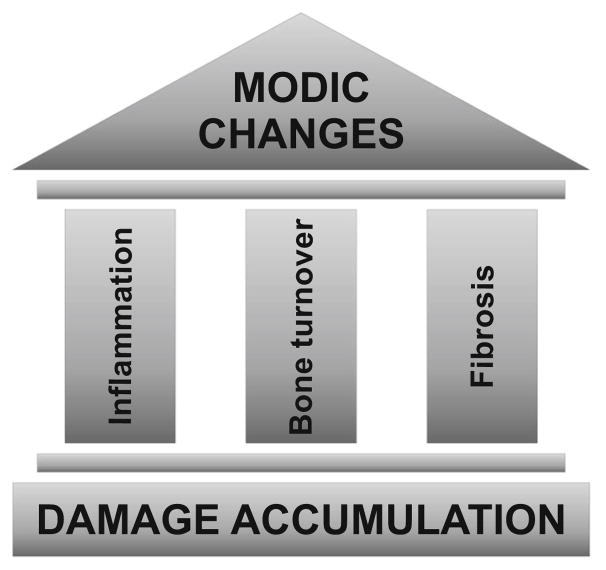
Despite an abundance of imaging data from MC studies, few reports detail the histology and pathoanatomy of MC. Fibrosis, inflammation, and high bone turnover were described in three MC1 and MC2 specimens [3]. In MC1, fibrous tissue replaces normal BM between thickened trabeculae, endplates appear disrupted, and bone–disc junction is filled with vascularized granulation tissue, a sign of inflammation. In MC2, fatty marrow replaces the normal BM. Similar to MC1, in MC2 the endplate is disrupted with the presence of fibrovascular granulation tissue at the disc/ endplate junction. This is in agreement with our recent findings in cadaveric tissue with MC (Fig. 3). The importance of endplate damage in the etiology of MC is underscored by studies of surgical waste tissue from MC1 and MC2 patients that show cartilaginous endplate fragments with extruded disc material [34]. Dynamic interdependencies between bone and marrow compartments in MC are demonstrated by histomorphometric analysis of biopsies that reveal a high bone turnover in MC1, reduced bone formation in MC2, and a stable sclerotic state in MC3 [35]. Sclerosis was also reported in mixed-type MC1/2 and MC2/3 [36]. In summary, the few histological studies show inflammation, high bone turnover, and fibrosis in MC (Fig. 4).
Fig. 3.
Mid-sagittal histological sections of spinal segments with bone marrow lesions characterized as Modic changes on MRI. Sections are stained with hematoxylin and eosin. Original magnifi-cations are ×0.5 (a, b), and ×10 (c–e). c and d are magnifications from the areas indicated on a and b, respectively. a, c Modic change type 1 characterized by fibrovascular tissue (asterisks) and trabecular thickening. The changes parallel endplate irregularities (arrow). b, d Modic change type 2. Fatty marrow replacement (asterisks) occurs along the entire endplates cephalad and caudad to the disc. Fibrotic tissue can be found at locations of endplate damage (arrows). e Healthy vertebral bone marrow with (Tr) trabecular bone, (AC) adipocytes, and (VS) vascular sinus
Fig. 4.
The three pathobiological pillars of Modic changes
Etiopathogenesis of Modic changes
Despite the clinical evidence that MC are painful, the etiology and pathobiology of MC are unknown. Although MC strongly associate with DD, it remains unclear why some patients with DD develop MC and others do not. It is likely that the propensity to develop MC relates to the composition and function of the BM and its communication with the disc through the endplates. The fact that all MC are interconvertible and that mixed-type MC1/2 and MC2/3 exist suggests that different MC types represent different stages of the same pathological process [2]. However, one pathogenesis does not inevitably exclude multiple etiological factors. Different conditions may predispose to new MC1 or MC2 or to convert existing MC to another type. These conditions are discussed below.
Etiological factors
In contrast to age-related “red” to “yellow” marrow conversion, which starts in the diaphyseal region and extends toward proximal and distal metaphysis [37], MC typically starts adjacent to a degenerated discs at the endplates [3, 4, 16, 19]. The bigger the MC, the more likely is the disc degenerated [17]. These observations provide compelling evidence of a connection between DD and MC and suggest that MC is unrelated to age-related marrow conversion. Despite the high specificity of MC for DD, the low sensitivity indicates that DD alone is not sufficient to trigger MC in most cases [16].
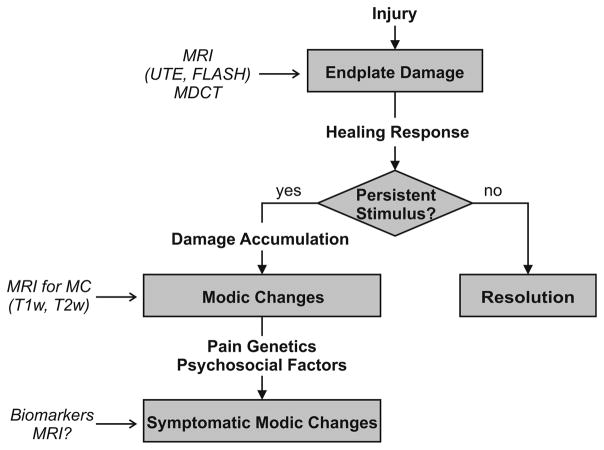
The presence of endplate defects may explain the difference between specificity and sensitivity. Endplate defects co-locate with MC and are predictive for future MC [3, 38]. Yet, because endplate damage promotes DD [38–41], evidences linking endplate damage to MC independently of DD are unavailable. Similar to endplate damage, disc herniation predisposes to DD and MC [18, 19]. Given the specificity of MC for disc damages (endplate damage and disc herniation), disc damage should be considered as a predisposing factor to MC rather than an incidental finding (Fig. 5).
Fig. 5.
Hypothetical model for the pathogenesis of Modic changes. An endplate damage is a predisposing condition for Modic changes. Endplate damage can be diagnosed with UTE and FLASH MRI sequences as well as with multidetector computed tomography (MDCT). Endplate damage triggers a healing response. The Modic etiology requires a persistent stimulus, which impedes resolution of the damage. The concomitant existence of a healing response and a persistent stimulus leads to accumulation of damage and to a ‘frustrated healing response’ characterized by chronic inflammation, high bone turnover, and fibrosis, the three pathobiological pillars of Modic changes, which can be visualized with T1-and T2-weighted MRI sequences. The severity and persistency of the stimulus as well as individual factors (pain genetics, psychosocial factors) may decide if the Modic changes become painful. Novel diagnostic tools (biomarkers, MRI) are required to distinguish painful from non-painful Modic changes
Endplate damage causes a cascade of degenerative changes in both the vertebra and the disc. Endplate damage increases intraosseous pressure [42] and causes stress concentrations within the disc, both of which could deteriorate cell metabolism and promote degenerative changes [39, 43–45]. Endplate damage also affects metabolite transport between the BM and the disc [46, 47]. Endplate damage as a result of acute or chronic overloading leads to a hydraulic disc/vertebra coupling, increased convective flow [46–48], and efflux of inflammatory mediators and extracellular matrix (ECM) catabolites from the disc into the BM. For example, acute vertebral burst fracture and focal endplate collapse can cause MC1-like BML in the adjacent BM [49, 50]. Yet, most BML related to acute endplate injury stabilize over time, and the pain is short lived [50]. Hence, in traumatic cases it appears that the BML stimulus can resolve. However, when endplate damage is more severe, LBP is more likely to be chronic [51], indicating a persistent stimulus and a prolonged inflammatory process [41, 51]. This is consistent with the general healing paradigm, where a failure to remove the inflammatory stimulus causes a chronic inflammation with fibrosis and granulation tissue. Coexistence of persistent inflammatory stimuli with ineffective healing leads to damage accumulation and a “frustrated healing response” characterized by chronic inflammation, fibrosis, and high bone turnover (Fig. 4). Two etiologies are suggested for MC1, which explain the nature of the persistent stimuli: (1) occult discitis; and (2) autoimmune reaction of BM to disc cells/ECM [52, 53]. Both etiologies presuppose structural disc damage, either herniation or endplate damage.
Biologic plausibility for an infectious etiology stems from the disc’s anaerobic environment, the high potential for disc tissue damage, and the low capacity for repair. Peripheral disc damage could allow access by low virulent skin microorganisms such as anaerobic Propionibacterium acnes (P. acnes) [54]. These bacteria can invade the circulatory system due to innocuous events such as tooth brushing [55]. Immune surveillance and the aerobic environment in the blood and BM hinder a systemic infection and diagnosis [56]. However, the absence of immune surveillance and low oxygen tension in the disc provides an ideal environment for bacterial growth. The slowly developing occult discitis gives rise to increasing amount of bacterial metabolites (propionic acid, lipase) and cytokines as a response of disc cells to the infection [54]. Disc cells secrete IL-6, IL-8, and PGE-2 after stimulation by bacterial endotoxins [57]. The persistent efflux of cytokines and bacterial metabolites from the disc could cause inflammation of the adjacent BM [56]. Elevated high-sensitivity C-reactive protein serum values in MC1 patients corroborate the presence of inflammation [58]. Furthermore, patients with infected herniated discs developed significantly more MC1 at the herniation level than non-infected herniations (80 vs. 44 %) [59]. However, a best-evidence synthesis from 11 studies investigating the relationship between bacteria and LBP or MC concluded that only moderate evidence exists to support a relationship between the presence of bacteria and both LBP with disc herniation and Modic Type 1 change with disc herniation [101].
The etiology of MC may also include autoimmunity. After embryologic formation of the disc, the nucleus pulposus (NP) no longer makes any contact with the systemic circulation, and consequently it is sequestered from leukocytes. NP cells maintain the immune privilege by expressing Fas ligand, which induces apoptosis in infiltrating lymphocytes [60]. Endplate damage co-locates NP with BM leukocytes. Increased levels of Fas receptor have been found in MC endplates, indicating an adaptive response to higher levels of Fas ligand, possibly from co-located NP [61]. Peripheral disc damage can expose the NP to the immune system, where it is recognized as “foreign” and triggers an autoimmune response [62–65]. Indeed, autografting the NP into immune-active tissue in animal models causes an abundant expression of cytokines [62, 64] and infiltration of macrophages, activated B- and T-cells [62, 66]. This is in agreement with findings in herniated and degenerated discs [63, 67]. In addition, NP cells elicit a primary immune response in macrophages and natural killer cells [68, 69]. Disc ECM is also linked to immunity, as disc proteoglycans can enhance lymphocyte transformation in vitro [65] and mice immunized with cartilage proteoglycans show strong mononuclear cell infiltration into the disc and almost completely resorbed discs [70]. It is not surprising therefore that this form of autoimmunity is presumed to prolong clinical symptoms in LBP patients [65].
Pathobiological factors
Disc/endplate damage, occult discitis, and autoimmunity are plausible explanations for MC etiology, but they do not account for why some patients with disc/endplate damage develop MC while some do not. This discrepancy may ultimately relate to the inflammatory potential of the disc and the capacity of the BM to respond to the inflammatory stimulus.
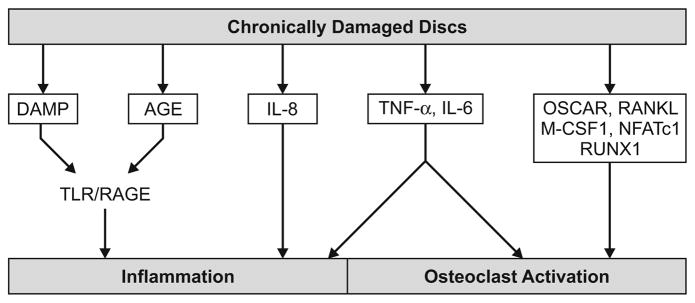
Discs adjacent to MC produce higher amounts of cytokines (IL-6, IL-8, TNF-α) and osteoclastic factors (RANKL, M-CSF, NFATc1, RUNX1, OSCAR) than discs of the same degeneration degree without adjacent MC (Fig. 6) [71, 72]. These cytokines interfere with the cellular composition of the adjacent BM (Fig. 7) and alter trabecular bone mass. For example, MC biopsies reveal high bone turnover in MC1, possibly due to an inflammatory process and reduced bone formation in MC2 [35]. On the other hand, trabecular thickening in histological sections of MC1 [3] (Fig. 3) and sclerosis in MC3 and mixed-type MC1/2 and MC2/3 were reported [3, 36]. Therefore, bone formation/resorption is a transient or individual phenomenon depending on the osteocyte/osteoclast ratio.
Fig. 6.
Factors released by a chronically damaged disc can cause inflammation and osteoclast activation in the adjacent bone marrow. Endplate damage leads to a hydraulic disc/vertebra coupling and increased efflux of these factors into the adjacent bone marrow where they can cause Modic changes
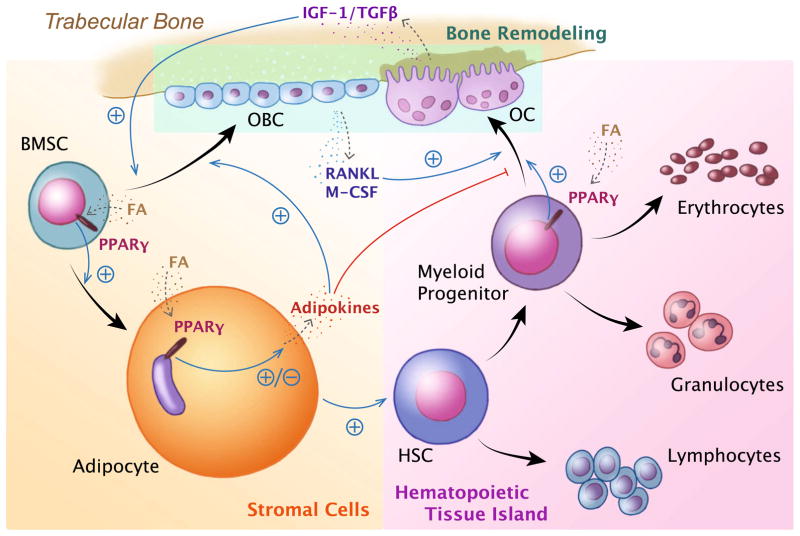
Fig. 7.
Interdependency of stromal and hematopoietic bone marrow cell differentiation and their effects on bone remodeling. Bone marrow-derived mesenchymal stem cells (BMSC) differentiate mainly into adipocytes or osteoblast cells (OBC) in a reciprocal manner. Hematopoietic stem cells (HSC) differentiate into osteoclasts (OC) besides other blood cells. Osteoblasts and osteoclasts deposit and erode the bone matrix, respectively. Fatty acids (FA) bind to PPARγ. PPARγ regulates the lineage commitment of both BMSC toward adipocytes and away from osteoblasts, and of myeloid progenitors toward OC. In adipocytes, PPARγ stimulation regulates adipokine secretion. Adipokines positively regulate osteoblastogenesis and negatively regulate osteoclastogenesis. Osteoclastogenesis is positively regulated by M-CSF and RANKL, which can be secreted by OBCs. OC secrete IGF-1 and TGFβ, which drive OBC differentiation
Toll-like receptor (TLR) stimulation of disc and marrow cells likely plays an important role in MC. Degenerated discs express more TLR1/2/4/6 than non-degenerated discs, possibly due to higher TNF-α/IL-1β levels [73, 74], and TNF-α/IL-1β enhances TLR2-mediated IL-6 and IL-8 secretion by disc cells, the same cytokines that are increased in discs adjacent to MC. TLR activation enhances transcription of NF-κB-responsive genes, a central signaling pathway in DD and OA [75]. TLR signaling is also linked to T cell activation and autoimmunity [76]. TLR are receptors for bacterial cell wall proteins and damage-associated molecular pattern (DAMPs). DAMPs are a heterogeneous group of molecules and are considered as “danger molecules”, because they are released from necrotic cells or generated after mechanical or enzymatic tissue damage (Fig. 6). ECM fragments (fibronectin, short hyaluronic acid fragments) are DAMPs that play a crucial role in OA [75].
The response of the BM to cytokines and DAMPs leaking from the disc through endplate defects into the BM depends on the composition of the BM itself. It is known that vertebral marrow adipose tissue (MAT) content is higher in males, at lower lumbar levels, and in older individuals [77]. These same three factors associate with the prevalence of MC [14]. MAT has high amounts of saturated fatty acids, minimally modified and oxidized low-density lipoproteins, which activate TLR2/4 [75, 77]. Therefore, ECM fragments draining from a degenerated disc into a fatty BM increase the total concentration of TLR ligands and NF-κB-controlled cytokines. This process may be triggered off MC in patients treated with chemonucleolysis, a non-surgical technique for treating a bulging disc by injecting an enzyme to digest the disc ECM. The enzymatic process leads inevitably to the generation of abundant ECM catabolites and DAMPs, which may be the cause for the development of MC in these patients. Chronic stimulation of TLRs was demonstrated to cause neo-adipogenesis [78] and induce adipocyte hypertrophy [79], thereby facilitating fatty marrow conversion as in MC2.
The interrelationship between fat metabolism and marrow composition and its relationship to MC is unknown, but some insights may be gained from the studies of BML in osteoarthritis (OA). Modic changes adjacent to a degenerated disc share many characteristics with BML in the femur/tibia of an osteoarthritic knee joint (Table 1). High serum lipids, obesity, age, and male gender increase the risk of developing BML in the knee [80]. OA patients also show an increased prevalence for DD [81], pointing to shared pathological variables at a systemic level. Therefore, knowledge from OA/BML research at peripheral skeletal sites may also help clarify the etiopathogenesis of MC.
Table 1.
| Characteristic | Similarity |
|---|---|
| MRI modalities | MC1 and OA-BML are identified as T1w↓, T2w↑ |
| Prevalence | Prevalence is higher in clinical (OA-BML and MC: 6 and 14 %) than non-clinical (OA-BML and MC: >50 and 43 %) population |
| Pain | MC and OA-BML are mostly painful in conjunction with joint degeneration, but the reason for pain is unknown. |
| Joint degradation | Lesion is dynamic and associates with the progression of joint degeneration |
| Risk factors | Shared risk factors for MC and OA-BML are age, male, obesity, and joint misalignment. These are also risk factors for disc degeneration and knee cartilage degeneration |
| Suggested etiologies | Overload, damage of joint cartilage, and inflammation |
| Natural history | Dynamic, conversion/resolution generally within 1–3 years in < 37 % (MC) and <66 % (OA-BML) |
‘Joint’ refers to disc and knee, ‘joint degeneration’ to DD and OA
MRI magnetic resonance imaging, MC modic changes, BML bone marrow lesion, OA osteoarthritis, T1w T1-weighted images
The adverse biological effects of fat on OA and DD are manifold. Long chain fatty acids increase MAT by binding to PPARγ [82] (Fig. 7), which in turn reduces bone density and increases fracture risk [83]. Higher serum lipid concentration also enhances lipid peroxidation, a process resulting in increased advanced-glycation end products (AGE) [84]. AGEs are formed through non-enzymatic reactions between glucose and proteins. AGEs cross-link ECM molecules and decrease the hydrophilic charge of proteoglycans [85], changes that directly and indirectly increase tissue stiffness. Besides the physical consequences of AGE accumulation, there are biological consequences as well. AGEs and one of their receptors (RAGE) elevate the level of reactive oxygen species, induce inflammatory changes that promote ECM catabolism, and also promote DD in diabetes mellitus [86, 87]. In OA, the adverse effects of AGE are amplified by the overexpression of RAGE [88]. RAGE cross talks with TLR [89], which is important since RAGE is also a receptor for DAMPs [73, 89].
In addition to the osteoclastic factors released by discs adjacent to MC, high MAT further stimulates osteoclastogenesis by the activation of PPARγ with fatty acids [90]. The adipogenic and anti-hematopoietic effect of PPARγ also leads to the depletion of BM cellularity [82, 91]. However, since adipocytes maintain the most primitive hematopoietic stem cell, recovery of a normal BM cellularity is possible [17, 91]. Indeed, resolution of MC2 occurs [17]. However, if in addition to the hematopoietic depletion also the adipocytic compartment is ablated and irreversible osteogenesis occurs [91], a situation resembling MC3 [17].
Hyperloading-related risk factors indicate that mechanical aspects also intervene with MC pathobiology (Fig. 2). The interrelationship of mechanical and biological factors is implicated by Wolff’s law, which posits that loading alters bone metabolism [92]. The intricate co-regulation of osteogenesis, adipogenesis, and hematopoiesis [82, 93] further suggests that chronic hyperloading also affects adipogenesis and hematopoiesis. Therefore, obesity may be a risk factor not only because of increased spinal forces, but also because of its influence on osteogenesis, adipogenesis, and hematopoiesis. For example, greater abdominal fat correlates with higher MAT [77], which associates with bone weakness (fragility fracture, Schmorl’s nodes, wedging) [83, 94] possibly due to lower trabecular bone mineral density [77].
Taken together, evidence suggests that structural damage triggers a pro-inflammatory reaction in the disc, which in turn could allow microbial infiltration and/or autoimmune reactions that intensify and prolong nociceptor stimulation by chemical or mechanical stimuli. The increased inflammatory potential of the disc activates pro-inflammatory signaling cascades in the BM and favors adipogenesis and osteoclast activation. The propensity to develop MC1 or MC2 may depend on the intensity and persistency of the inflammatory stimuli as well as on the composition and metabolic state of the BM.
Experimental models
The gaps in knowledge about MC pathophysiology, such as the molecular and cellular changes in MC and their relation to disc health and metabolism, combined with the practical and ethical limitations of clinical studies, motivate the development of experimental models. Only few animal models succeeded in generating marrow changes, always in conjunction with inducing DD in the adjacent disc [99–101]. Chronic axial compression of mouse tail segments induced DD and BML consistent with increased marrow vascularity and cellularity [99]. Enzymatic and surgical disc decompression caused trabecular microfracture and subsequent healing with endochondral ossification and mesenchymal replacement of BM [101]. Triple stab injury of rat tail discs induced trabecular thickening and fibrovascular replacement of the adjacent BM [100]. All three studies indicate that disc injury may play an important role in promoting MC. However, disc injury inevitably alters load distribution of the vertebrae and increases cytokine expression. Clarifying the relative importance of these factors in MC etiology will represent an important step toward developing effective therapeutic interventions.
Conclusion and future direction
Current knowledge about MC is derived almost exclusively from cross-sectional or longitudinal clinical studies. Data indicate infectious and autoimmune etiologies, both of which presuppose structural damage of the disc/endplate anatomy. These different etiologies may also work in conjunction and eventually proceed along common pathological pathways. Further, different types of MC may represent different stages of the same pathological process. The pathway is not necessarily a sequential progression through the different types of MC, but conversion from MC1 or MC2 to any other MC is possible. Ultimately, the propensity to develop MC seems to depend on three factors: structural disruption of the disc/endplate, inflammatory potential of the disc, and the capacity of the BM to respond to higher inflammatory stimuli. In vitro and animal experiments are required addressing the role of these factors in the pathogenesis of MC. Furthermore, basic research will have to increase the body of evidence for the autoimmune and the infectious etiology.
The treatment of MC is limited by several factors. First, MC are often under-appreciated as a source of pain. Second, it is unknown why MC hurt. Third, no treatment consensus is established because, fourth, the etiology and the underlying pathogenesis is unknown. Clinical trials for novel non-surgical treatments of MC focused on suppressing inflammation/infection with anti-TNF-α antibody, antibiotics, or intradiscal steroid injections [27, 28, 95, 96]. Attempts have also been made to attenuate bone resorption and osteoclast recruitment with bisphosphonates [97], because it is known that OA patients taking the bisphosphonate alendronate have less frequent BML [98]. While these studies showed some beneficial effects at the 1-year follow-up, larger studies with long-term follow-up are needed.
Diagnostic tools are needed to define MC phenotypes and their variants and identify painful MC. Traditional T1w and T2w MRI may not be sensitive enough to pick up early signs of MC or the clinically most relevant phenotypes. In this regard, imaging of endplate degeneration [102] may become an essential decision-making tool in LBP patients. Furthermore, diagnostic strategies based on serum/urine biomarkers or BM biopsies may help distinguish infectious from autoimmune etiologies. Biomarkers and new imaging sequences may also be employed to distinguish symptomatic from non-symptomatic MC (Fig. 5). Finally, animal models that recapitulate the key features of MC are needed to test therapy mechanisms and screen for new treatments. Summarizing, we recommend testing the following hypotheses to develop an effective treatment for MC.
The formation of Modic changes requires at least a disc/endplate damage plus a persistent stimulus.
Disc/endplate damage causes detrimental biological and biomechanical changes in the disc and the bone marrow.
Occult discitis and innate-type immune response to disc material are persistent stimuli.
The composition of the bone marrow affects the severity of the response to the persistent stimulus and ultimately decides on the formation of MC.
Treatments that do not target the etiological factors (endplate damage, persistent stimulus, bone marrow composition) are not effective in the long term.
Modic changes and bone marrow lesions in osteoarthritic joints share similar basic pathogenetic mechanisms.
Ultimately, MC are likely more than just a coincidental imaging finding in LBP patients, but rather represent an underlying pathology that should be a target for therapy.
Acknowledgments
We acknowledge our funding sources: Swiss National Science Foundation Grant PBEZP3_145961 and National Institutes of Health Grant AR063705. We also acknowledge Jaakko Niinimäki for providing MRI scans of MC.
Footnotes
Compliance with ethical standards
Conflict of interest None of the authors has any potential conflict of interest
References
- 1.Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2163–2196. doi: 10.1016/S0140-6736(12)61729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson KJ, Dagher AP, Eckel TS, et al. Modic changes on MR images as studied with provocative diskography: clinical relevance–a retrospective study of 2457 disks. Radiology. 2009;250:849–855. doi: 10.1148/radiol.2503080474. [DOI] [PubMed] [Google Scholar]
- 3.Modic MT, Steinberg PM, Ross JS, et al. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166:193–199. doi: 10.1148/radiology.166.1.3336678. [DOI] [PubMed] [Google Scholar]
- 4.De Roos A, Kressel H, Spritzer C, Dalinka M. MR imaging of marrow changes adjacent to end plates in degenerative lumbar disk disease. AJR Am J Roentgenol. 1987;149:531–534. doi: 10.2214/ajr.149.3.531. [DOI] [PubMed] [Google Scholar]
- 5.Jensen TS, Karppinen J, Sorensen JS, et al. Vertebral endplate signal changes (Modic change): a systematic literature review of prevalence and association with non-specific low back pain. Eur Spine J. 2008;17:1407–1422. doi: 10.1007/s00586-008-0770-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jensen RK, Leboeuf-Yde C. Is the presence of Modic changes associated with the outcomes of different treatments? A systematic critical review. BMC Musculoskelet Disord. 2011;12:183. doi: 10.1186/1471-2474-12-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Karppinen J, Solovieva S, Luoma K, et al. Modic changes and interleukin 1 gene locus polymorphisms in occupational cohort of middle-aged men. Eur Spine J. 2009;18:1963–1970. doi: 10.1007/s00586-009-1139-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rahme R, Moussa R. The modic vertebral endplate and marrow changes: pathologic significance and relation to low back pain and segmental instability of the lumbar spine. AJNR Am J Neuroradiol. 2008;29:838–842. doi: 10.3174/ajnr.A0925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Y, Videman T, Battié MC. Modic changes: prevalence, distribution patterns, and association with age in white men. Spine J. 2012;12:411–416. doi: 10.1016/j.spinee.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kääpä E, Luoma K, Pitkäniemi J, et al. Correlation of size and type of modic types 1 and 2 lesions with clinical symptoms: a descriptive study in a subgroup of patients with chronic low back pain on the basis of a university hospital patient sample. Spine (Phila Pa 1976) 2012;37:134–9. doi: 10.1097/BRS.0b013e3182188a90. [DOI] [PubMed] [Google Scholar]
- 11.Järvinen J, Karppinen J, Niinimäki J, et al. Association between changes in lumbar Modic changes and low back symptoms over a two-year period. BMC Musculoskelet Disord. 2015;16:98. doi: 10.1186/s12891-015-0540-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kuisma M, Karppinen J, Niinimäki J, et al. Modic changes in endplates of lumbar vertebral bodies: prevalence and association with low back and sciatic pain among middle-aged male workers. Spine (Phila Pa 1976) 2007;32:1116–1122. doi: 10.1097/01.brs.0000261561.12944.ff. [DOI] [PubMed] [Google Scholar]
- 13.Chung CB, Vande Berg BC, Tavernier T, et al. End plate marrow changes in the asymptomatic lumbosacral spine: frequency, distribution and correlation with age and degenerative changes. Skeletal Radiol. 2004;33:399–404. doi: 10.1007/s00256-004-0780-z. [DOI] [PubMed] [Google Scholar]
- 14.Karchevsky M, Schweitzer ME, Carrino JA, et al. Reactive endplate marrow changes: a systematic morphologic and epidemiologic evaluation. Skeletal Radiol. 2005;34:125–129. doi: 10.1007/s00256-004-0886-3. [DOI] [PubMed] [Google Scholar]
- 15.Kuisma M, Karppinen J, Niinimäki J, et al. A three-year follow-up of lumbar spine endplate (Modic) changes. Spine (Phila Pa 1976) 2006;31:1714–1718. doi: 10.1097/01.brs.0000224167.18483.14. [DOI] [PubMed] [Google Scholar]
- 16.Kjaer P, Korsholm L, Bendix T, et al. Modic changes and their associations with clinical findings. Eur Spine J. 2006;15:1312–1319. doi: 10.1007/s00586-006-0185-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jensen TS, Bendix T, Sorensen JS, et al. Characteristics and natural course of vertebral endplate signal (Modic) changes in the Danish general population. BMC Musculoskelet Disord. 2009;10:81. doi: 10.1186/1471-2474-10-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jensen TS, Kjaer P, Korsholm L, et al. Predictors of new vertebral endplate signal (Modic) changes in the general population. Eur Spine J. 2010;19:129–135. doi: 10.1007/s00586-009-1184-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Albert HB, Briggs AM, Kent P, et al. The prevalence of MRI-defined spinal pathoanatomies and their association with modic changes in individuals seeking care for low back pain. Eur Spine J. 2011;20:1355–1362. doi: 10.1007/s00586-011-1794-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arana E, Kovacs FM, Royuela A, et al. Modic changes and associated features in Southern European chronic low back pain patients. Spine J. 2011;11:402–411. doi: 10.1016/j.spinee.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 21.Määttä JH, Kraatari M, Wolber L, et al. Vertebral endplate change as a feature of intervertebral disc degeneration: a heritability study. Eur Spine J. 2014;23:1856–1862. doi: 10.1007/s00586-014-3333-8. [DOI] [PubMed] [Google Scholar]
- 22.Kuisma M, Karppinen J, Haapea M, et al. Are the determinants of vertebral endplate changes and severe disc degeneration in the lumbar spine the same? A magnetic resonance imaging study in middle-aged male workers. BMC Musculoskelet Disord. 2008;9:51. doi: 10.1186/1471-2474-9-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leboeuf-Yde C, Kjaer P, Bendix T, Manniche C. Self-reported hard physical work combined with heavy smoking or overweight may result in so-called Modic changes. BMC Musculoskelet Disord. 2008;9:5. doi: 10.1186/1471-2474-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Farshad-Amacker NA, Hughes AP, Aichmair A, et al. Determinants of evolution of endplate and disc degeneration in the lumbar spine: a multifactorial perspective. Eur Spine J. 2014;23:1863–1868. doi: 10.1007/s00586-014-3382-z. [DOI] [PubMed] [Google Scholar]
- 25.Wu H-L, Ding W-Y, Shen Y, et al. Prevalence of vertebral endplate modic changes in degenerative lumbar scoliosis and its associated factors analysis. Spine (Phila Pa 1976) 2012;37:1958–1964. doi: 10.1097/BRS.0b013e31825bfb85. [DOI] [PubMed] [Google Scholar]
- 26.Kleinstück F, Dvorak J, Mannion AF. Are “structural abnormalities” on magnetic resonance imaging a contraindication to the successful conservative treatment of chronic non-specific low back pain? Spine (Phila Pa 1976) 2006;31:2250–2257. doi: 10.1097/01.brs.0000232802.95773.89. [DOI] [PubMed] [Google Scholar]
- 27.Buttermann GR. The effect of spinal steroid injections for degenerative disc disease. Spine J. 2004;4:495–505. doi: 10.1016/j.spinee.2004.03.024. [DOI] [PubMed] [Google Scholar]
- 28.Fayad F, Lefevre-Colau M-M, Rannou F, et al. Relation of inflammatory modic changes to intradiscal steroid injection outcome in chronic low back pain. Eur Spine J. 2007;16:925–931. doi: 10.1007/s00586-006-0301-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jensen OK, Nielsen CV, Sørensen JS, Stengaard-Pedersen K. Type 1 Modic changes was a significant risk factor for 1-year outcome in sick-listed low back pain patients: a nested cohort study using magnetic resonance imaging of the lumbar spine. Spine J. 2014;14:2568–2581. doi: 10.1016/j.spinee.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 30.Lurie JD, Moses RA, Tosteson ANA, et al. Magnetic resonance imaging predictors of surgical outcome in patients with lumbar intervertebral disc herniation. Spine (Phila Pa 1976) 2013;38:1216–1225. doi: 10.1097/BRS.0b013e31828ce66d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ohtori S, Inoue G, Ito T, et al. Tumor necrosis factor-immunoreactive cells and PGP 9.5-immunoreactive nerve fibers in vertebral endplates of patients with discogenic low back Pain and Modic Type 1 or Type 2 changes on MRI. Spine (Phila Pa 1976) 2006;31:1026–1031. doi: 10.1097/01.brs.0000215027.87102.7c. [DOI] [PubMed] [Google Scholar]
- 32.Fields AJ, Liebenberg EC, Lotz JC. Innervation of pathologies in the lumbar vertebral end plate and intervertebral disc. Spine J. 2014;14:513–521. doi: 10.1016/j.spinee.2013.06.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eskola JP, Männikkö M, Samartzis D, Karppinen J. Genome-wide association studies of lumbar disc degeneration—are we there yet? Spine J. 2014;14:479–482. doi: 10.1016/j.spinee.2013.07.437. [DOI] [PubMed] [Google Scholar]
- 34.Schmid G, Witteler A, Willburger R, et al. Lumbar disk herniation: correlation of histologic findings with marrow signal intensity changes in vertebral endplates at MR imaging. Radiology. 2004;231:352–358. doi: 10.1148/radiol.2312021708. [DOI] [PubMed] [Google Scholar]
- 35.Perilli E, Parkinson IH, Truong L-H, et al. Modic (end-plate) changes in the lumbar spine: bone microarchitecture and remodelling. Eur Spine J. 2014;24:1926–1934. doi: 10.1007/s00586-014-3455-z. [DOI] [PubMed] [Google Scholar]
- 36.Kuisma M, Karppinen J, Haapea M, et al. Modic changes in vertebral endplates: a comparison of MR imaging and multislice CT. Skeletal Radiol. 2009;38:141–147. doi: 10.1007/s00256-008-0590-9. [DOI] [PubMed] [Google Scholar]
- 37.Lecka-Czernik B. Marrow fat metabolism is linked to the systemic energy metabolism. Bone. 2012;50:534–539. doi: 10.1016/j.bone.2011.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weiner BK, Vilendecic M, Ledic D, et al. Endplate changes following discectomy: natural history and associations between imaging and clinical data. Eur Spine J. 2014;24:2449–2457. doi: 10.1007/s00586-014-3734-8. [DOI] [PubMed] [Google Scholar]
- 39.Kerttula LI, Serlo WS, Tervonen OA, et al. Post-traumatic findings of the spine after earlier vertebral fracture in young patients. Spine (Phila Pa 1976) 2000;25:1104–1108. doi: 10.1097/00007632-200005010-00011. [DOI] [PubMed] [Google Scholar]
- 40.Dudli S, Ferguson SJ, Haschtmann D. Severity and pattern of post-traumatic intervertebral disc degeneration depend on the type of injury. Spine J. 2014;14:1256–1264. doi: 10.1016/j.spinee.2013.07.488. [DOI] [PubMed] [Google Scholar]
- 41.Mok FPS, Samartzis D, Karppinen J, et al. ISSLS prize winner: prevalence, determinants, and association of Schmorl nodes of the lumbar spine with disc degeneration: a population-based study of 2449 individuals. Spine (Phila Pa 1976) 2010;35:1944–1952. doi: 10.1097/BRS.0b013e3181d534f3. [DOI] [PubMed] [Google Scholar]
- 42.Yoganandan N, Larson SJ, Gallagher M, et al. Correlation of microtrauma in the lumbar spine with intraosseous pressures. Spine (Phila Pa 1976) 1994;19:435–440. doi: 10.1097/00007632-199402001-00009. [DOI] [PubMed] [Google Scholar]
- 43.Dudli S, Haschtmann D, Ferguson SJ. Persistent degenerative changes in the intervertebral disc after burst fracture in an in vitro model mimicking physiological post-traumatic conditions. Eur Spine J. 2014;24:1901–1908. doi: 10.1007/s00586-014-3301-3. [DOI] [PubMed] [Google Scholar]
- 44.Ishihara H, McNally DS, Urban JP, Hall AC. Effects of hydrostatic pressure on matrix in different regions of the intervertebral synthesis disk. J Appl Physiol. 1996;80:839–846. doi: 10.1152/jappl.1996.80.3.839. [DOI] [PubMed] [Google Scholar]
- 45.Lotz J, Chin JR. Intervertebral Disc Cell Death Is Dependent on the Magnitude and Duration of Spinal Loading. Spine (Phila Pa 1976) 2000;25:1477–1483. doi: 10.1097/00007632-200006150-00005. [DOI] [PubMed] [Google Scholar]
- 46.Rajasekaran S, Babu JN, Arun R, et al. ISSLS prize winner: A study of diffusion in human lumbar discs: a serial magnetic resonance imaging study documenting the influence of the endplate on diffusion in normal and degenerate discs. Spine (Phila Pa 1976) 2004;29:2654–2667. doi: 10.1097/01.brs.0000148014.15210.64. [DOI] [PubMed] [Google Scholar]
- 47.Adams MA, Freeman BJ, Morrison HP, et al. Mechanical initiation of intervertebral disc degeneration. Spine (Phila Pa 1976) 2000;25:1625–1636. doi: 10.1097/00007632-200007010-00005. [DOI] [PubMed] [Google Scholar]
- 48.Ferguson SJ, Ito K, Nolte LP. Fluid flow and convective transport of solutes within the intervertebral disc. J Biomech. 2004;37:213–221. doi: 10.1016/s0021-9290(03)00250-1. [DOI] [PubMed] [Google Scholar]
- 49.Brown DB, Glaiberman CB, Gilula LA, Shimony JS. Correlation between preprocedural MRI findings and clinical outcomes in the treatment of chronic symptomatic vertebral compression fractures with percutaneous vertebroplasty. AJR Am J Roentgenol. 2005;184:1951–1955. doi: 10.2214/ajr.184.6.01841951. [DOI] [PubMed] [Google Scholar]
- 50.Wagner AL, Murtagh FR, Arrington JA, Stallworth D. Relationship of Schmorl’s nodes to vertebral body endplate fractures and acute endplate disk extrusions. AJNR Am J Neuroradiol. 2000;21:276–281. [PMC free article] [PubMed] [Google Scholar]
- 51.Takahashi K, Miyazaki T, Ohnari H, et al. Schmorl’s nodes and low-back pain. Analysis of magnetic resonance imaging findings in symptomatic and asymptomatic individuals. Eur Spine J. 1995;4:56–59. doi: 10.1007/BF00298420. [DOI] [PubMed] [Google Scholar]
- 52.Ma X-L, Ma J-X, Wang T, et al. Possible role of autoimmune reaction in Modic Type I changes. Med Hypotheses. 2011;76:692–694. doi: 10.1016/j.mehy.2011.01.035. [DOI] [PubMed] [Google Scholar]
- 53.Albert HB, Kjaer P, Jensen TS, et al. Modic changes, possible causes and relation to low back pain. Med Hypotheses. 2008;70:361–368. doi: 10.1016/j.mehy.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 54.Stirling A, Worthington T, Rafiq M, et al. Association between sciatica and Propionibacterium acnes. Lancet. 2001;357:2024–2025. doi: 10.1016/S0140-6736(00)05109-6. [DOI] [PubMed] [Google Scholar]
- 55.Bhanji S, Williams B, Sheller B, et al. Transient bacteremia induced by toothbrushing a comparison of the Sonicare toothbrush with a conventional toothbrush. Pediatr Dent. 2002;24:295–299. [PubMed] [Google Scholar]
- 56.Wedderkopp N, Thomsen K, Manniche C, et al. No evidence for presence of bacteria in modic type I changes. Acta Radiol. 2009;50:65–70. doi: 10.1080/02841850802524485. [DOI] [PubMed] [Google Scholar]
- 57.Burke JG, Watson GRW, Conhyea D, et al. Human nucleus pulposis can respond to a pro-inflammatory stimulus. Spine (Phila Pa 1976) 2003;28:2685–2693. doi: 10.1097/01.BRS.0000103341.45133.F3. [DOI] [PubMed] [Google Scholar]
- 58.Rannou F, Ouanes W, Boutron I, et al. High-sensitivity C-reactive protein in chronic low back pain with vertebral end-plate Modic signal changes. Arthritis Rheum. 2007;57:1311–1315. doi: 10.1002/art.22985. [DOI] [PubMed] [Google Scholar]
- 59.Albert HB, Lambert P, Rollason J, et al. Does nuclear tissue infected with bacteria following disc herniations lead to Modic changes in the adjacent vertebrae? Eur Spine J. 2013;22:690–696. doi: 10.1007/s00586-013-2674-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kaneyama S, Nishida K, Takada T, et al. Fas ligand expression on human nucleus pulposus cells decreases with disc degeneration processes. J Orthop Sci. 2008;13:130–135. doi: 10.1007/s00776-007-1204-4. [DOI] [PubMed] [Google Scholar]
- 61.Wang F, Jiang J-M, Deng C-H, et al. Expression of Fas receptor and apoptosis in vertebral endplates with degenerative disc diseases categorized as Modic type I or II. Injury. 2011;42:790–795. doi: 10.1016/j.injury.2011.01.034. [DOI] [PubMed] [Google Scholar]
- 62.Geiss A, Larsson K, Junevik K, et al. Autologous nucleus pulposus primes T cells to develop into interleukin-4-producing effector cells: an experimental study on the autoimmune properties of nucleus pulposus. J Orthop Res. 2009;27:97–103. doi: 10.1002/jor.20691. [DOI] [PubMed] [Google Scholar]
- 63.Virri J, Grönblad M, Seitsalo S, et al. Comparison of the prevalence of inflammatory cells in subtypes of disc herniations and associations with straight leg raising. Spine (Phila Pa 1976) 2001;26:2311–2315. doi: 10.1097/00007632-200111010-00004. [DOI] [PubMed] [Google Scholar]
- 64.Shamji MF, Allen KD, So S, et al. Gait abnormalities and inflammatory cytokines in an autologous nucleus pulposus model of radiculopathy. Spine (Phila Pa 1976) 2009;34:648–654. doi: 10.1097/BRS.0b013e318197f013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gertzbein SD, Tait JH, Devlin SR. The stimulation of lymphocytes by nucleus pulposus in patients with degenerative disk disease of the lumbar spine. Clin Orthop Relat Res. 1976;123:149–154. [PubMed] [Google Scholar]
- 66.Kanerva A, Kommonen B, Grönblad M, et al. Inflammatory cells in experimental intervertebral disc injury. Spine (Phila Pa 1976) 1997;22:2711–2715. doi: 10.1097/00007632-199712010-00002. [DOI] [PubMed] [Google Scholar]
- 67.Park J-B, Chang H, Kim Y-S. The pattern of interleukin-12 and T-helper types 1 and 2 cytokine expression in herniated lumbar disc tissue. Spine (Phila Pa 1976) 2002;27:2125–2128. doi: 10.1097/01.BRS.0000025687.56098.54. [DOI] [PubMed] [Google Scholar]
- 68.Yamamoto J, Maeno K, Takada T, et al. Fas ligand plays an important role for the production of pro-inflammatory cytokines in intervertebral disc nucleus pulposus cells. J Orthop Res. 2013;31:608–615. doi: 10.1002/jor.22274. [DOI] [PubMed] [Google Scholar]
- 69.Murai K, Sakai D, Nakamura Y, et al. Primary immune system responders to nucleus pulposus cells: evidence for immune response in disc herniation. Eur Cell Mater. 2010;19:13–21. doi: 10.22203/ecm.v019a02. [DOI] [PubMed] [Google Scholar]
- 70.Bárdos T, Szabó Z, Czipri M, et al. A longitudinal study on an autoimmune murine model of ankylosing spondylitis. Ann Rheum Dis. 2005;64:981–987. doi: 10.1136/ard.2004.029710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Burke J, Watson R, McCormack D, et al. Endplate changes are associated with increased disc inflammatory mediator production. J Bone Joint Surg Br. 2003;85-B(SUPP II):164. [Google Scholar]
- 72.Torkki M, Majuri M-L, Wolff H, et al. Osteoclast activators are elevated in intervertebral disks with Modic changes among patients operated for herniated nucleus pulposus. Eur Spine J. 2015 Mar 27; doi: 10.1007/s00586-015-3897-y. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 73.Klawitter M, Hakozaki M, Kobayashi H, et al. Expression and regulation of toll-like receptors (TLRs) in human intervertebral disc cells. Eur Spine J. 2014;23:1878–1891. doi: 10.1007/s00586-014-3442-4. [DOI] [PubMed] [Google Scholar]
- 74.Wuertz K, Vo N, Kletsas D, Boos N. Inflammatory and catabolic signalling in intervertebral discs: the roles of NF-κB and MAP kinases. Eur Cell Mater. 2012;23:103–19. doi: 10.22203/ecm.v023a08. (discussion 119–20) [DOI] [PubMed] [Google Scholar]
- 75.Piccinini AM, Midwood KS. DAMPening inflammation by modulating TLR signalling. Mediators Inflamm. 2010 doi: 10.1155/2010/672395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mills KHG. TLR-dependent T cell activation in autoimmunity. Nat Rev Immunol. 2011;11:807–822. doi: 10.1038/nri3095. [DOI] [PubMed] [Google Scholar]
- 77.Baum T, Yap SP, Karampinos DC, et al. Does vertebral bone marrow fat content correlate with abdominal adipose tissue, lumbar spine bone mineral density, and blood biomarkers in women with type 2 diabetes mellitus? J Magn Reson Imaging. 2012;35:117–124. doi: 10.1002/jmri.22757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Thomas GPL, Hemmrich K, Abberton KM, et al. Zymosan-induced inflammation stimulates neo-adipogenesis. Int J Obes (Lond) 2008;32:239–248. doi: 10.1038/sj.ijo.0803702. [DOI] [PubMed] [Google Scholar]
- 79.Monden M, Koyama H, Otsuka Y, et al. Receptor for advanced glycation end products regulates adipocyte hypertrophy and insulin sensitivity in mice: involvement of Toll-like receptor 2. Diabetes. 2013;62:478–489. doi: 10.2337/db11-1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lim YZ, Wang Y, Wluka AE, et al. Association of obesity and systemic factors with bone marrow lesions at the knee: a systematic review. Semin Arthritis Rheum. 2014;43:600–612. doi: 10.1016/j.semarthrit.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 81.Hassett G, Hart DJ, Manek NJ, et al. Risk factors for progression of lumbar spine disc degeneration: the Chingford Study. Arthritis Rheum. 2003;48:3112–3117. doi: 10.1002/art.11321. [DOI] [PubMed] [Google Scholar]
- 82.Gimble JM, Zvonic S, Floyd ZE, et al. Playing with bone and fat. J Cell Biochem. 2006;98:251–266. doi: 10.1002/jcb.20777. [DOI] [PubMed] [Google Scholar]
- 83.Schwartz AV, Sigurdsson S, Hue TF, et al. Vertebral bone marrow fat associated with lower trabecular BMD and prevalent vertebral fracture in older adults. J Clin Endocrinol Metab. 2013;98:2294–2300. doi: 10.1210/jc.2012-3949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ott C, Jacobs K, Haucke E, et al. Role of advanced glycation end products in cellular signaling. Redox Biol. 2014;2:411–429. doi: 10.1016/j.redox.2013.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Jazini E, Sharan AD, Morse LJ, et al. Alterations in T2 relaxation magnetic resonance imaging of the ovine intervertebral disc due to nonenzymatic glycation. Spine (Phila Pa 1976) 2012;37:E209–E215. doi: 10.1097/BRS.0b013e31822ce81f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Illien-Junger S, Grosjean F, Laudier DM, et al. Combined anti-inflammatory and anti-AGE drug treatments have a protective effect on intervertebral discs in mice with diabetes. PLoS One. 2013;8:e64302. doi: 10.1371/journal.pone.0064302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Fields AJ, Berg-Johansen B, Metz LN, et al. Alterations in intervertebral disc composition, matrix homeostasis and biomechanical behavior in the UCD-T2DM rat model of type 2 diabetes. J Orthop Res. 2015;33:738–746. doi: 10.1002/jor.22807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Liu-Bryan R. Synovium and the innate inflammatory network in osteoarthritis progression. Curr Rheumatol Rep. 2013;15:323. doi: 10.1007/s11926-013-0323-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rojas A, Delgado-López F, González I, et al. The receptor for advanced glycation end-products: a complex signaling scenario for a promiscuous receptor. Cell Signal. 2013;25:609–614. doi: 10.1016/j.cellsig.2012.11.022. [DOI] [PubMed] [Google Scholar]
- 90.Wan Y, Chong L-W, Evans RM. PPAR-gamma regulates osteoclastogenesis in mice. Nat Med. 2007;13:1496–1503. doi: 10.1038/nm1672. [DOI] [PubMed] [Google Scholar]
- 91.Naveiras O, Nardi V, Wenzel PL, et al. Bone-marrow adipocytes as negative regulators of the haematopoietic microenvironment. Nature. 2009;460:259–263. doi: 10.1038/nature08099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Turner CH. Functional determinants of bone structure: beyond Wolff’s law of bone transformation. Bone. 1992;13:403–409. doi: 10.1016/8756-3282(92)90082-8. [DOI] [PubMed] [Google Scholar]
- 93.Nuttall ME, Shah F, Singh V, et al. Adipocytes and the regulation of bone remodeling: a balancing act. Calcif Tissue Int. 2014;94:78–87. doi: 10.1007/s00223-013-9807-6. [DOI] [PubMed] [Google Scholar]
- 94.Schellinger D, Lin CS, Hatipoglu HG, Fertikh D. Potential value of vertebral proton MR spectroscopy in determining bone weakness. AJNR Am J Neuroradiol. 2001;22:1620–1627. [PMC free article] [PubMed] [Google Scholar]
- 95.Albert HB, Sorensen JS, Christensen BS, Manniche C. Antibiotic treatment in patients with chronic low back pain and vertebral bone edema (Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy. Eur Spine J. 2013;22:697–707. doi: 10.1007/s00586-013-2675-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Korhonen T, Karppinen J, Paimela L, et al. The treatment of disc-herniation-induced sciatica with infliximab: one-year follow-up results of FIRST II, a randomized controlled trial. Spine (Phila Pa 1976) 2006;31:2759–2766. doi: 10.1097/01.brs.0000245873.23876.1e. [DOI] [PubMed] [Google Scholar]
- 97.Koivisto K, Kyllönen E, Haapea M, et al. Efficacy of zoledronic acid for chronic low back pain associated with Modic changes in magnetic resonance imaging. BMC Musculoskelet Disord. 2014;15:64. doi: 10.1186/1471-2474-15-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Carbone LD, Nevitt MC, Wildy K, et al. The relationship of antiresorptive drug use to structural findings and symptoms of knee osteoarthritis. Arthritis Rheum. 2004;50:3516–3525. doi: 10.1002/art.20627. [DOI] [PubMed] [Google Scholar]
- 99.Papuga MO, Proulx ST, Kwok E, et al. Chronic axial compression of the mouse tail segment induces MRI bone marrow edema changes that correlate with increased marrow vasculature and cellularity. J Orthop Res. 2010;28:1220–1228. doi: 10.1002/jor.21103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ulrich JA, Liebenberg EC, Thuillier DU, Lotz J. ISSLS prize winner: repeated disc injury causes persistent inflammation. Spine (Phila Pa 1976) 2007;32:2812–2819. doi: 10.1097/BRS.0b013e31815b9850. [DOI] [PubMed] [Google Scholar]
- 101.Malinin T, Brown MD. Changes in vertebral bodies adjacent to acutely narrowed intervertebral discs: observations in baboons. Spine (Phila Pa 1976) 2007;32:E603–E607. doi: 10.1097/BRS.0b013e31815574e7. [DOI] [PubMed] [Google Scholar]
- 102.Fields AJ, Han M, Krug R, Lotz JC. Cartilaginous end plates: quantitative MR imaging with very short echo times-orientation dependence and correlation with biochemical composition. Radiology. 2015;274:482–489. doi: 10.1148/radiol.14141082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Roemer FW, Frobell R, Hunter DJ, et al. MRI-detected subchondral bone marrow signal alterations of the knee joint: terminology, imaging appearance, relevance and radiological differential diagnosis. Osteoarthritis Cartilage. 2009;17:1115–1131. doi: 10.1016/j.joca.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 104.Felson DT, Niu J, Guermazi A, et al. Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum. 2007;56:2986–2992. doi: 10.1002/art.22851. [DOI] [PubMed] [Google Scholar]
- 105.Bendix T, Sorensen JS, Henriksson GAC, et al. Lumbar modic changes-a comparison between findings at low- and high-field magnetic resonance imaging. Spine (Phila Pa 1976) 2012;37:1756–1762. doi: 10.1097/BRS.0b013e318257ffce. [DOI] [PubMed] [Google Scholar]
- 106.Urquhart DM, Zheng Y, Cheng AC, et al. Could low grade bacterial infection contribute to low back pain? A systematic review. BMC Med. 2015;13:13. doi: 10.1186/s12916-015-0267-x. [DOI] [PMC free article] [PubMed] [Google Scholar]