Abstract
Background
To this day, there is no data concerning guideline adherence on P2Y12-inhibitors in Austria. Prasugrel and ticagrelor have been shown to be superior to clopidogrel in the treatment of acute coronary syndromes (ACS). However, recent data from European registries showed a reluctant prescription policy with rates of clopidogrel at discharge ranging from 35 to 55%.
Methods
In this prospective, multi-centre registry we assessed prescription rates of P2Y12-inhibitors in patients with ACS in four Austrian PCI centres. Parameters associated with the use of clopidogrel have been evaluated in multivariate logistic regression.
Results
Between January and June 2015, 808 patients with ACS undergoing PCI were considered for further analysis. 416 (51.5%) presented with STEMI and 392 (48.5%) with NSTE-ACS. Mean age was 65.7 ± 12.4 and 240 (30.9%) were female. Twenty-eight (3.5%) died during the hospital stay. At discharge, 212 (27.2% of all patients) received clopidogrel, 260 (32.2%) prasugrel and 297 (36.8%) ticagrelor, while 11 (1.4%) did not receive any P2Y12-inhibitor. Of those patients, who were discharged with clopidogrel, 117 (55.2%) had no absolute contraindication against a more potent P2Y12-inhibitor. Diagnosis of NSTE-ACS (p<0.001), COPD (p = 0.049), and age (p<0.001) next to factors contributing to absolute contraindication were positively associated with the use of clopidogrel.
Conclusions
Despite a high level of care, a considerable number of patients were not treated with the more potent P2Y12-inhibitors. Parameters associated with a presumably higher risk of bleeding and side-effects against the more effective P2Y12 inhibitors were the most prominent factors for the prescription of clopidogrel.
Introduction
Cardiovascular disease is the most common cause of death in the western world, with coronary artery disease making up its greatest proportion. [1] Considerable time and effort has been invested to improve acute and chronic medical treatment with positive effects on various outcome parameters. [2,3] The introduction of two additional oral P2Y12-inhibitors, prasugrel and ticagrelor, extended the armamentarium of this drug class in addition to clopidogrel, and further improved outcome in patients presenting with acute coronary syndrome (ACS).[4,5] Both substances have been adopted into European treatment guidelines, which both recommend the use of these novel P2Y12-inhibitors over clopidogrel for all patients presenting with ACS without overt contraindications.[6–8]
Recent data from different national registries examining the usage of the novel agents in patients with ACS showed a rather reluctant prescription policy, with rates of clopidogrel prescription at discharge ranging from approximately 35 to 55%.[9–14] Hence, a significant percentage of patients presenting with ACS are not treated according to current guidelines in Europe.
In this registry, we sought to assess the prescription rate of the more effective P2Y12-inhibitors prasugrel and ticagrelor in patients presenting with ACS undergoing percutaneous coronary intervention (PCI) and its predictive parameters in four major Austrian tertiary hospitals with acute PCI facilities.
Methods
Our study complies with the Declaration of Helsinki of 1975, was approved by the local ethics committee (EK-14-220-VK) and informed and written consent has been obtained from all subjects. The “3rd Department of Medicine with Cardiology and Intensive Care Medicine of the Wilhelminenhospital” served as the coordinating and data analysis centre.
Study population
This prospective, multicentre, observational registry aimed to evaluate the prescription policy of dual antiplatelet therapy in consecutive patients presenting with ACS undergoing PCI in Austria between January and June 2015. Patients were included at four Austrian PCI centres. ACS patients presented either with persistent ST-segment elevation myocardial infarction (STEMI) or non ST-elevation acute coronary syndromes (NSTE-ACS). STEMI and NSTE-ACS were defined and diagnosed according to the current ESC guidelines available at that time.[6–8] According to the respective prescribing information, absolute contraindications against novel P2Y12-inhibitors were: History of stroke or transient ischemic attack (TIA) for prasugrel, history of intracranial haemorrhage for ticagrelor, presence of active bleeding and the indication for a chronic anticoagulation for both agents. [4,5,15] Age above 75 years and body weight below 60 kilograms for prasugrel, and comorbidities linked with severe dyspnea and predisposition for bradyarrhythmia for ticagrelor were defined as relative contraindications. [4,5,16]
Endpoints
As primary endpoint, the prescription rate of clopidogrel at discharge was investigated. As secondary endpoint, the association of clinical parameters on prescription patterns of clopidogrel were analysed at admission and at hospital discharge.
Statistical analysis
Data are presented as mean ± standard deviation for normally distributed continuous variables unless depicted otherwise. Continuous variables were compared by the t-test or the Mann-Whitney-U-test, where appropriate. For the detection of disparities in the distributions of categorical data Pearson’s χ2-test was used.
The association of clinical parameters on the prescription rate at admission and at hospital discharge of clopidogrel was analysed using a binary logistic regression model with step-wise back elimination using a likelihood-ratio test with a p-level for entry of 0.05 and a p-value for removal of 0.2. When more than two categories were present, dummy variables were introduced to define a reference group. The final models considered the following variables: Clinical presentation (STEMI or NSTE-ACS), age, gender, weight, presence of diabetes mellitus, presence of arterial hypertension, presence of hyperlipidaemia, familiar history of coronary heart disease (CHD), current or prior smoking, history of chronic obstructive pulmonary disease (COPD), site of antiplatelet loading therapy, presence of atrial fibrillation, active bleeding at admission, history of stroke or transient ischemic attack (TIA), history of intracranial haemorrhage, planned operation and peri-interventional anticoagulation treatment regimen regimen (only at discharge). In all statistical tests performed, a two-sided alpha level of p < 0.05 was regarded as statistically significant. Statistical analyses were performed using the IBM® SPSS® Statistics 23.0 (IBM Corp., Armonk, USA) software package.
Results
Between January and June 2015, we enrolled 990 patients presenting with an ACS, of whom 808 (81.6%) underwent PCI with stent implantation, 53 (5.4%) were referred for coronary artery bypass grafting and 129 (13.0%) were treated conservatively. Only patients undergoing PCI were considered for the primary analysis. Of those, 416 (51.5%) presented with STEMI and 392 (48.5%) with NSTE-ACS. Mean age was 65.7 ± 12.4 years and 250 (30.9%) were female. Baseline characteristics are summarised in Table 1.
Table 1. Baseline characteristics, comorbidities and treatment stratified for all patients, STEMI and NSTE-ACS.
| Variable | All | STEMI | NSTE-ACS | p-Value |
|---|---|---|---|---|
| n = 808 | n = 416 | n = 392 | ||
| Age, years (mean±SD) | 65.7±12.4 | 64.3±12.4 | 67.1±12.2 | 0.001 |
| Female, n (%) | 250 (30.9%) | 132 (31.7%) | 118 (30.1%) | 0.617 |
| Weight, kg (mean±SD) | 82.1 ± 16.9 | 81.4±16.0 | 82.8±17.8 | 0.236 |
| Hyperlipidaemia, n (%) | 488 (60.8%) | 255 (61.9%) | 233 (59.6%) | 0.504 |
| Hypertension, n (%) | 573 (70.9%) | 257 (61.8%) | 316 (80.6%) | <0.001 |
| Familiar history of CHD, n (%) | 56 (7.0%) | 32 (7.8%) | 24 (6.1%) | 0.365 |
| Diabetes mellitus, n (%) | 184 (22.8%) | 84 (20.2%) | 100 (25.5%) | 0.072 |
| Current or prior smoking, n (%) | 284 (35.4%) | 150 (36.4%) | 134 (34.3%) | 0.527 |
| COPD, n (%) | 54 (6.7%) | 21 (5.0%) | 33 (8.4%) | 0.055 |
| Prior stroke or TIA, n (%) | 37 (4.6%) | 17 (4.1%) | 20 (5.1%) | 0.490 |
| Intracranial haemorrhage, n (%) | 8 (1.0%) | 7 (1.7%) | 1 (0.3%) | 0.041 |
| Active bleeding, n (%) | 9 (1.1%) | 4 (1.0%) | 5 (1.3%) | 0.671 |
| Atrial fibrillation, n (%) | 79 (9.8%) | 38 (9.1%) | 41 (10.5%) | 0.526 |
| Peri-interventional anticoagulation and antiplatelet therapy | ||||
| UFH, n (%) | 580 (71.8%) | 259 (62.3%) | 32 (81.9%) | <0.001 |
| UFH + GPI, n (%) | 102 (12.6%) | 78 (18.8%) | 24 (6.1%) | |
| Bivalirudin, n (%) | 95 (11.8%) | 57 (13.7%) | 38 (9.7%) | |
| Othera, n (%) | 22 (2.7%) | 17 (4.1%) | 5 (1.3%) | |
| Vessel Intervention, n (%) | ||||
| 1 | 603 (79.3%) | 318 (82.0%) | 285 (76.6%) | 0.045 |
| 2 | 136 (17.9%) | 57 (14.7%) | 79 (21.2%) | |
| 3 | 21 (2.8%) | 13 (3.4%) | 8 (2.2%) | |
| Use of DES, n (%) | 795 (98.4%) | 405 (97.4%) | 390 (99.4%) | 0.178 |
| Site of antiplatelet loading therapy | ||||
| Ambulance, n (%) | 168 (20.8%) | 137 (32.9%) | 31 (7.9%) | <0.001 |
| Emergency ward, n (%) | 181 (22.4%) | 109 (26.2%) | 72 (18.4%) | |
| Cardiology ward, n (%) | 153 (18.9%) | 66 (15.9%) | 87 (22.2%) | |
| Cath lab, n (%) | 220 (27.2%) | 67 (16.1%) | 153 (39.0%) | |
| Other wards, n (%) | 15 (1.9%) | 8 (1.9%) | 7 (1.8%) | |
| Maintenance, n (%) | 18 (2.2) | 2 (0.5%) | 16 (4.1%) | |
Data are presented as mean ± SD or %. CHD = coronary heart disease; COPD = chronic obstructive pulmonary disease; DES = drug-eluting stent; GPI = glycoprotein IIb/IIIa inhibitor; NSTE-ACS = non-ST-elevation acute coronary syndrome; STEMI = ST-elevation myocardial infarction; UFH = unfractionated heparin.
a Other refers to peri-interventional monotherapies or combinations of low-molecular weight heparins, fondaparinux and glycoprotein inhibitors.
As expected, patients presenting with NSTE-ACS were older (67.1±12.2 vs. 64.3±12.4; p = 0.001) and received multi-vessel PCI more frequently compared to STEMI patients (p = 0.045). Also, arterial hypertension (80.6% vs. 61.8%; p<0.001) was more frequently observed in the NSTE-ACS population. Moreover, STEMI and NSTE-ACS patients differed significantly in regard to peri-interventional anticoagulation and antiplatelet therapy (p<0.001) with higher rates of glycoprotein-inhibitors (18.8% vs. 6.1%) and bivalirudin (13.7% vs. 9.7%) in patients presenting with STEMI. There was no significant difference between both patient groups concerning the use of drug-eluting stents (405 (97.4%) vs. 390 (99.4%); p = 0.178).
Of all patients, 122 (15.1%) had an indication for chronic anticoagulation or at least one absolute contraindication against the use of a novel agent at admission (Table 1).
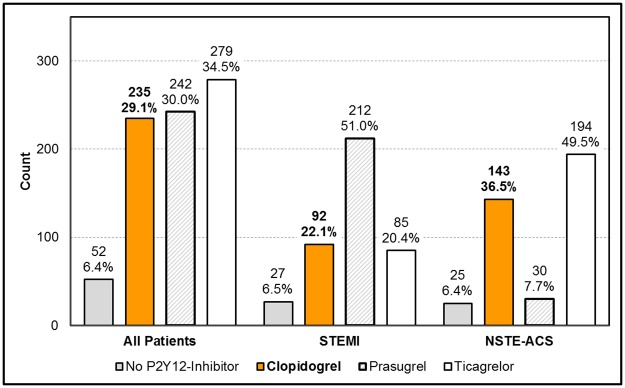
Antiplatelet therapy at admission
Of 808 patients included into the final analysis, 235 (29.1%) received clopidogrel, 242 (30.0%) prasugrel and 279 (34.5%) ticagrelor at admission, while 52 (6.4%) did not receive any P2Y12-inhibitor (Fig 1). In total, 803 patients (99.4%) received acetylsalicylic acid (ASA). Prescription rates of P2Y12-inhibitors for patients presenting with STEMI and NSTE-ACS are also depicted in Fig 1.
Fig 1. Prescription rates for P2Y12-inhibitors at admission in absolute numbers and percent stratified for the whole cohort, for STEMI patients and NSTE-ACS patients.
The loading dose was given to 168 patients (20.8%) in the ambulance (pre-hospital loading), to 181 (22.4%) in the emergency room, to 153 (18.9%) at the cardiology ward, to 220 (27.2%) in the cath-lab, and to 15 (1.9%) at another ward and 18 (2.2%) were already on a maintenance dose (Table 1).
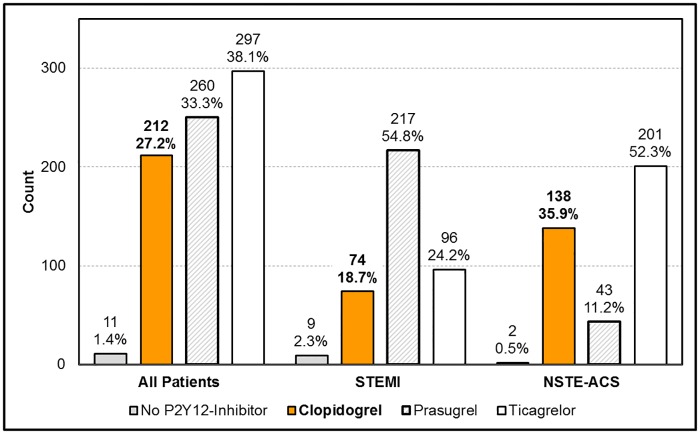
Antiplatelet therapy at discharge
During the hospital stay 28 patients (3.5%) died. Of the remaining patients, 212 (26.2% of all) received clopidogrel, 260 (32.2%) prasugrel and 297 (36.8%) ticagrelor, while 11 (1.4%) did not receive any P2Y12-inhibitor at discharge (Fig 2). Differences between STEMI-patients and NSTE-ACS patients are depicted in Fig 2.
Fig 2. Prescription rates for P2Y12-inhibitors at discharge in absolute numbers and percent stratified for the whole cohort, for STEMI patients and NSTE-ACS patients.
Switching from the initial P2Y12-inhibitor occurred in 14.7% of all patients—64 (7.9% of all) of those patients treated initially with clopidogrel were switched, 25 to prasugrel (3.1%) and 30 to ticagrelor (3.7%), respectively.
Of the 212 patients, who were discharged with clopidogrel, 117 (55.2%—15.2% of all patients) had no absolute contraindication against a new P2Y12-inhibitor. Of all patients discharged with a novel agent, twenty (2.6%) patients were discharged despite the presence of an absolute contraindication or the indication for chronic anticoagulation.
Predictors of use of clopidogrel
In descending order of relative odds, the presence of following characteristics was associated positively with clopidogrel use at admission: Diagnosis of NSTE-ACS (OR 2.334 [95%CI 1.575–3.460]) and age (OR 1.030 per 1-year increase [95%CI 1.013–1.048]), next to factors contributing to absolute contraindication (Table 2).
Table 2. Predictors of clopidogrel use at admission after stepwise backward elimination in a multivariate binary logistic regression analysis model.
Variables that were entered into the model prior to elimination were: Main diagnosis, age, gender, weight, presence of diabetes, presence of hypertension, presence of hyperlipidaemia, familiar history of coronary heart disease (CHD), current or prior smoking, history of COPD, site of antiplatelet loading therapy, presence of atrial fibrillation, active bleeding at admission, history of stroke or TIA, history of intracranial haemorrhage and planned operation.
| Predictors of clopidogrel use at admission. | ||||
|---|---|---|---|---|
| OR | 95% CI | p-value | ||
| Age | 1.030 | 1.013 | 1.048 | 0.001 |
| Weight | 0.990 | 0.979 | 1.002 | 0.096 |
| NSTE-ACS | 2.334 | 1.575 | 3.460 | <0.001 |
| Familiar history of coronary heart disease | 1.592 | .807 | 3.144 | 0.180 |
| Loading in the ambulance | 0.383 | 0.122 | 1.206 | 0.101 |
| Loading in the emergency room | 0.233 | 0.074 | 0.736 | 0.013 |
| Loading at the cath-lab | 0.199 | 0.063 | 0.622 | 0.006 |
| Loading at the cardiology ward | 0.339 | 0.108 | 1.068 | 0.065 |
| Active Bleeding | 18.163 | 2.182 | 151.202 | 0.007 |
| History of intracranial haemorrhage | 8.735 | 1.434 | 53.226 | 0.019 |
| History of stroke or TIA | 2.411 | 1.056 | 5.509 | 0.037 |
| Presence of atrial fibrillation | 4.254 | 2.317 | 7.811 | <0.001 |
OR: odds ratio; CI: confidence interval; CHD = coronary heart disease; COPD = chronic obstructive pulmonary disease; NSTE-ACS = non-ST-elevation acute coronary; syndrome; TIA = transient ischemic attack.
At hospital discharge, the following variables were associated positively with clopidogrel use: Diagnosis of NSTE-ACS (OR 2.197 [95%CI 1.350–3.574]), presence of COPD (OR 2.212 [95%CI 1.037–4.718]), and age (OR per 1-year increase 1.049 [95%CI 1.026–1.072]), next to factors contributing to absolute contraindication (Table 3).
Table 3. Predictors of clopidogrel use at discharge after stepwise backward elimination in a multivariate binary logistic regression analysis model.
Variables that were entered into the model prior to elimination were: Main diagnosis, age, gender, weight, presence of diabetes, presence of hypertension, presence of hyperlipidaemia, familiar history of coronary heart disease (CHD), current or prior smoking, presence of COPD, site of antiplatelet loading therapy, switching of P2Y12-inhibitor during hospital stay, presence of atrial fibrillation, active bleeding at admission, history of stroke or TIA, history of intracranial haemorrhage, planned surgery and peri-interventional anticoagulation and antiplatelet treatment regimen.
| Predictors of clopidogrel use at discharge. | ||||
|---|---|---|---|---|
| OR | 95% CI | p-value | ||
| Age | 1.049 | 1.026 | 1.072 | <0.001 |
| Weight | 0.991 | 0.977 | 1.005 | 0.185 |
| NSTE-ACS | 2.197 | 1.350 | 3.574 | 0.002 |
| Hypertension | 1.653 | 0.931 | 2.934 | 0.086 |
| Familiar history of coronary heart disease | 2.105 | 0.911 | 4.861 | 0.081 |
| Loading in the ambulance | 0.174 | 0.048 | 0.638 | 0.008 |
| Loading in the emergency room | 0.178 | 0.050 | 0.641 | 0.008 |
| Loading at the cath-lab | 0.170 | 0.048 | 0.603 | 0.006 |
| Loading at the cardiology ward | 0.172 | 0.047 | 0.628 | 0.008 |
| Presence of COPD | 2.212 | 1.037 | 4.718 | 0.040 |
| Active bleeding | 35.197 | 3.787 | 327.095 | 0.002 |
| History of intracranial haemorrhage | 22.347 | 3.312 | 150.761 | 0.001 |
| History of stroke or TIA | 4.611 | 1.759 | 12.088 | 0.002 |
| Presence of atrial fibrillation | 19.785 | 8.727 | 44.857 | <0.001 |
| Peri-interventional unfractionated heparin | 0.348 | 0.087 | 1.384 | 0.134 |
| Peri-interventional bivalirudin | 0.254 | 0.058 | 1.118 | 0.070 |
| Peri-interventional LMWH | 0.132 | 0.015 | 1.151 | 0.067 |
OR: odds ratio; CI: confidence interval; CHD = coronary heart disease; COPD = chronic obstructive pulmonary disease; LMWH = low-molecular weight heparin; NSTE-ACS = non-ST-elevation acute coronary syndrome; TIA = transient ischemic attack.
Discussion
The main findings of our study investigating the use of P2Y12-inhibitors in a population of subjects with acute coronary syndrome undergoing invasive revascularization exhibited a clopidogrel use in 29.2% of our patients at admission and in 27.2% at hospital discharge.
In the recent GRAPE registry by Alexopoulos et al. conducted in eight Greek hospitals and a study by Kudaravalli et al. conducted in the urban area around Pittsburgh, rates of clopidogrel upon admission were 67.7% and 80.2%, respectively. [9,13] At discharge, the rate was 38.7% in the GRAPE registry and 55.5% in the Italian EYESHOT registry by De Luca et al., whereas the rate in the study by Kudaravalli et al. remained high with 77.6%.[9,10,13] This prominent gap between the European and American cohorts at discharge reflects the different recommendation policies, with the European guidelines favouring the novel agents in contrast to the American guidelines, leaving the choice of agent to the physicians discretion.[6,17–19]
The clopidogrel prescription rate in our cohort was comparably lower to other recent European registries, both at admission and discharge. [9,10] However, besides this positive trend compared to international data, in our hands 55.2% of the patients discharged with clopidogrel had no absolute contraindication against a modern P2Y12-inhibitor or an indication for long-term antithrombotic therapy. The rate was lower compared to the GRAPE registry, where 76.2% of all patients discharged with clopidogrel had no contraindication against a novel agent, but still 14.4% of our total cohort were “undertreated” in regards to antiplatelet therapy. Potential system related factors might be physician´s inertia, thus, suboptimal guideline adherence, lack of resources, time constraints, and other local factors, as previously reported. [20] Moreover, patient related factors might have had a potential impact on the underuse of more effective antiplatelet agents: Higher age, known as a warning but no absolute contraindication for prasugrel treatment, was independently associated with the use of clopidogrel in our cohort, in line with previous studies showing reduced evidence-based therapy in ACS cohorts of elderly patients and with other registries.[9,10,12,21,22] Following a subgroup analysis of the PLATO-trial current European guidelines advise ticagrelor over clopidogrel also in the elderly. However, the evidence of superiority of ticagrelor compared to clopidogrel is weak and remains doubtful, as elderly patients were strikingly underrepresented in, both, the PLATO and TRITON-TIMI 38 trial. [4–8] Since this population has an especially high risk for bleeding complications, an overestimation of the net clinical benefit in this specific subgroup cannot be excluded.
Also, the presence of COPD was associated with clopidogrel prescription. Physicians seemed to be cautious to use ticagrelor with respect to dyspnoea as a frequent side effect, but in such patients prasugrel would have been an option. [4,5] Accordingly, in our hands the clinical presentation was associated with the use of clopidogrel, as seen also in other registries.[9,10,12,13] NSTE-ACS patients more frequently received clopidogrel compared to STEMI-patients (35.9% vs 18.7%), possibly reflecting the higher rate of comorbidities. [23] Interestingly, body weight was not associated with the prescription of clopidogrel.
Most importantly, antiplatelet therapy administered at the time of admission was infrequently switched during hospitalization (14.7%), even when contraindications against a more effective P2Y12 inhibitor were absent. In the EYESHOT registry the switching rate was comparably low, whereas in the GRAPE registry about one third of the all patients were switched to another agent. The higher switching rate in the GRAPE registry thereby most probably reflects the standard use of clopidogrel in the pre-hospital medical services.[9,10]
Similar to the results of the EYESHOT registry, DAPT was initiated in 26.3% of the NSTE-ACS patients already before PCI, although both, ticagrelor and clopidogrel, were never tested in randomized clinical trials addressing the question of pre-loading in NSTE-ACS before PCI, while prasugrel should not be used before coronary anatomy is known and PCI is performed. [10,24]
Limitations and strengths
These data are derived from four major tertiary hospitals in predominantly urban areas and might not represent all patients hospitalized for an ACS in rural areas of Austria. Nevertheless, in Austria most rural areas are covered by centralised cath-labs in urban areas and therefore, our registry probably provides a real-life picture of current guideline adherence regarding dual antiplatelet therapy and, therefore, is valuable in assessing the translation of scientific evidence to everyday practice in Central Europe. As the study was planned to address prescription policy of P2Y12-inhibtors in Austria, we did not investigate the clinical outcome for our patients and also the study was not powered to address clinical outcome.
Conclusion
In opposite to the recommendations of at that time valid ESC guidelines, a considerable number of patients were not treated with the more potent P2Y12-inhibitors in urban Austrian ACS networks, but received clopidogrel despite missing absolute contraindications against prasugrel or ticagrelor. Parameters associated with a presumably higher risk of bleeding and/or comorbidities and expected side-effects against the more effective P2Y12 inhibitors based on warnings (age, co-morbidities associated with dyspnea or bradycardia) were the most prominent factors for the initial prescription of clopidogrel. Moreover, we could demonstrate a relatively low willingness of cardiologists for switching clopidogrel if already initiated to one of the more effective P2Y12-inhibtiors as a topic future improvement.
Supporting information
Dataset is available from the Figshare database: https://doi.org/10.6084/m9.figshare.4903439.v4.
(SAV)
Acknowledgments
The study was planned and performed by the Association for the Promotion of Research in Arteriosclerosis, Thrombosis and Vascular Biology (ATVB), Vienna, Austria and partially financially supported by Astra Zeneca and Daiichi Sankyo. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Abbreviations
- ACS
acute coronary syndrome
- CHD
coronary heart disease
- CI
confidence interval
- COPD
chronic obstructive pulmonary disease
- DES
drug-eluting stent
- GPI
glycoprotein IIb/IIIa inhibito
- LMWH
low-molecular weight heparin
- NSTE-ACS
non-ST-elevation myocardial infarction
- OR
odds ratio
- PCI
percutaneous coronary intervention
- STEMI
ST-elevation myocardial infarction
- TIA
transient ischemic attack
- UFH
unfractionated heparin
Data Availability
All relevant data are within the paper and its Supporting Information file.
Funding Statement
The study was planned and performed by the Association for the Promotion of Research in Arteriosclerosis, Thrombosis and Vascular Biology (ATVB), Vienna, Austria and partially financially supported by Astra Zeneca and Daiichi Sankyo. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization. Health statistics and information systems. Cause-specific mortality. Estimates for 2000–2012. World Health Statistics 2012. 2012.
- 2.Rogers WJ, Frederick PD, Stoehr E, Canto JG, Ornato JP, Gibson CM, et al. Trends in presenting characteristics and hospital mortality among patients with ST elevation and non-ST elevation myocardial infarction in the National Registry of Myocardial Infarction from 1990 to 2006. Am Heart J. 2008;156: 1026–34. doi: 10.1016/j.ahj.2008.07.030 [DOI] [PubMed] [Google Scholar]
- 3.Bata IR, Gregor RD, Wolf HK, Brownell B. Trends in five-year survival of patients discharged after acute myocardial infarction. Can J Cardiol. 2006;22: 399–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, et al. Prasugrel versus Clopidogrel in Patients with Acute Coronary Syndromes. N Engl J Med. 2007;357: 2001–2015. doi: 10.1056/NEJMoa0706482 [DOI] [PubMed] [Google Scholar]
- 5.Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, et al. Ticagrelor versus Clopidogrel in Patients with Acute Coronary Syndromes. N Engl J Med. 2009;361: 1045–1057. doi: 10.1056/NEJMoa0904327 [DOI] [PubMed] [Google Scholar]
- 6.Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33: 2569–619. doi: 10.1093/eurheartj/ehs215 [DOI] [PubMed] [Google Scholar]
- 7.Windecker S, Kolh P, Alfonso F, Collet J-P, Cremer J, Falk V, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2014;35: 2541–2619. doi: 10.1093/eurheartj/ehu278 25173339 [Google Scholar]
- 8.Roffi M, Patrono C, Collet J-P, Mueller C, Valgimigli M, Andreotti F, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2015;32: 2999–3054. [Google Scholar]
- 9.Alexopoulos D, Goudevenos JA, Xanthopoulou I, Deftereos S, Sitafidis G, Kanakakis I, et al. Implementation of contemporary oral antiplatelet treatment guidelines in patients with acute coronary syndrome undergoing percutaneous coronary intervention: A report from the GReek AntiPlatelet rEgistry (GRAPE). Int J Cardiol. 2013;168: 5329–5335. doi: 10.1016/j.ijcard.2013.08.007 [DOI] [PubMed] [Google Scholar]
- 10.De Luca L, Leonardi S, Cavallini C, Lucci D, Musumeci G, Caporale R, et al. Contemporary antithrombotic strategies in patients with acute coronary syndrome admitted to cardiac care units in Italy: The EYESHOT Study. Eur Hear J Acute Cardiovasc Care. 2015;4: 441–52. [DOI] [PubMed] [Google Scholar]
- 11.Clemmensen P, Grieco N, Ince H, Danchin N, Goedicke J, Ramos Y, et al. MULTInational non-interventional study of patients with ST-segment elevation myocardial infarction treated with PRimary Angioplasty and Concomitant use of upstream antiplatelet therapy with prasugrel or clopidogrel—the European MULTIPRAC Registry. Eur Hear J Acute Cardiovasc Care. 2015;4: 220–9. [DOI] [PubMed] [Google Scholar]
- 12.Yudi MB, Clark DJ, Farouque O, Eccleston D, Andrianopoulos N, Duffy SJ, et al. Clopidogrel, prasugrel or ticagrelor in patients with acute coronary syndromes undergoing percutaneous coronary intervention. Intern Med J. 2016;46: 559–565. doi: 10.1111/imj.13041 [DOI] [PubMed] [Google Scholar]
- 13.Kudaravalli M, Althouse AD, Marroquin OC, Khandhar SJ, Sharbaugh MS, Toma C, et al. Assessment of P2Y12 inhibitor usage and switching in acute coronary syndrome patients undergoing percutaneous coronary revascularization. Int J Cardiol. 2016;223: 854–859. doi: 10.1016/j.ijcard.2016.08.144 [DOI] [PubMed] [Google Scholar]
- 14.Angerås O, Hasvold P, Thuresson M, Deleskog A, ÖBraun O. Treatment pattern of contemporary dual antiplatelet therapies after acute coronary syndrome: a Swedish nationwide population-based cohort study. Scand Cardiovasc J. 2016;50: 99–107. doi: 10.3109/14017431.2015.1119304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lip GYH, Windecker S, Huber K, Kirchhof P, Marin F, Ten Berg JM, et al. Management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous coronary or valve interventions: a joint consensus document of the European Society of Cardiology Cardiology Workin. Eur Heart J. 2014;35: 3155–3179. [DOI] [PubMed] [Google Scholar]
- 16.Scirica BM, Cannon CP, Emanuelsson H, Michelson EL, Harrington RA, Husted S, et al. The incidence of bradyarrhythmias and clinical bradyarrhythmic events in patients with acute coronary syndromes treated with ticagrelor or clopidogrel in the PLATO (Platelet Inhibition and Patient Outcomes) trial: Results of the continuous electrocardiogr. J Am Coll Cardiol. 2011;57: 1908–1916. [DOI] [PubMed] [Google Scholar]
- 17.Hamm CW, Bassand J-P, Agewall S, Bax JJ, Boersma E. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2011;32: 2999–3054. doi: 10.1093/eurheartj/ehr236 [DOI] [PubMed] [Google Scholar]
- 18.Jneid H, Anderson JL, Wright RS, Adams CD, Bridges CR, Casey DE Jr, Ettinger SM, Fesmire FM, Ganiats TG, Lincoff AM, Peterson ED, Philippides GJ, Theroux P, Wenger NK Z J. 2012 ACCF/AHA Focused Update of the Guideline for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction. J Am Coll Cardiol. 2012;60: 645–81. [DOI] [PubMed] [Google Scholar]
- 19.O’Gara PT, Kushner FG, Ascheim DD et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines Developed. J Am Coll Cardiol. 2013;62: e147–239.23747642 [Google Scholar]
- 20.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA R H. Why Don’t Physicians Follow Clinical Practice Guidelines? JAMA. 1999;282: 1458–65. [DOI] [PubMed] [Google Scholar]
- 21.Avezum A, Makdisse M, Spencer F, Gore JM, Fox KAA, Montalescot G, et al. Impact of age on management and outcome of acute coronary syndrome: observations from the Global Registry of Acute Coronary Events (GRACE). Am Heart J. 2005;149: 67–73. doi: 10.1016/j.ahj.2004.06.003 [DOI] [PubMed] [Google Scholar]
- 22.Alexander KP, Newby LK, Bhapkar M V, White HD, Hochman JS, Pfisterer ME, et al. International variation in invasive care of the elderly with acute coronary syndromes. Eur Heart J. 2006;27: 1558–64. doi: 10.1093/eurheartj/ehl067 [DOI] [PubMed] [Google Scholar]
- 23.Roe MT, Messenger JC, Weintraub WS, Cannon CP, Fonarow GC, Dai D, et al. Treatments, trends, and outcomes of acute myocardial infarction and percutaneous coronary intervention. J Am Coll Cardiol. 2010;56: 254–63. doi: 10.1016/j.jacc.2010.05.008 [DOI] [PubMed] [Google Scholar]
- 24.Montalescot G, Collet J-P, Ecollan P, Bolognese L, ten Berg J, Dudek D, et al. Effect of Prasugrel Pre-Treatment Strategy in Patients Undergoing Percutaneous Coronary Intervention for NSTEMI: The ACCOAST-PCI Study. J Am Coll Cardiol. 2014;64: 2563–2571. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Dataset is available from the Figshare database: https://doi.org/10.6084/m9.figshare.4903439.v4.
(SAV)
Data Availability Statement
All relevant data are within the paper and its Supporting Information file.