Abstract
Background
Ankle fractures associated with syndesmotic injury have a poorer prognosis than those without such an injury. Anatomic reduction of the distal tibiofibular joint restores joint congruency and minimizes contact pressures, yet operative fixation of syndesmotic ankle injuries is frequently complicated by malreduction of the syndesmosis. Current methods of assessing reduction have been shown to be inadequate. As such, additional methods to judge the accuracy of syndesmotic reduction are required.
Questions/Purposes
The purposes of our study were (1) to determine the anatomic axis of the syndesmosis, or the trans-syndesmotic angle (TSA), and (2) to describe the intraoperative fluoroscopic appearance of syndesmotic clamp reduction oriented along the anatomic syndesmotic angle.
Methods
Computed tomography (CT) scans of 45 uninjured adult ankles were analyzed to measure the TSA, defined as the angle between the plane of a lateral ankle radiograph and a line drawn perpendicular to the fibular incisura. Three-dimensional reconstructions of CT scans were then used to demonstrate clamp placement collinear with the TSA as would be seen on an intraoperative lateral ankle radiograph.
Results
The average TSA measured 21±5 degrees anterior to the plane of a lateral radiograph. When a simulated reduction clamp tine was placed on the fibular ridge and the clamp oriented along the TSA, the medial tine, as seen on a lateral radiograph, was within the anterior one-third of the tibia 93% of the time. It was, on average, 23±7% of the distance from the anterior to the posterior tibial cortex, with tine placement occurring in this range in 73% of ankles. The medial tine rested 53±17% of the distance between the anterior cortices of the tibia and fibula, with 71% of tines placed in this range.
Conclusions
Reduction clamp placement oriented along the TSA has a predictable appearance on lateral ankle imaging and can guide clamp positioning during syndesmotic reduction. With one tine placed on the fibular ridge, placing the medial clamp tine in the anterior third of the tibia, or halfway between the anterior cortices of the tibia and fibula is the most accurate position for reduction in line with the TSA.
Level of Evidence
2 (Retrospective diagnostic)
Keywords: Syndesmosis, Anatomic, Reduction, Intraoperative Fluoroscopy, Trans-Syndesmotic Angle
Introduction
Ankle fractures are one of the most common operatively managed lower extremity injuries in orthopaedics, and 11 to 20% of unstable ankle fractures will have concomitant syndesmotic disruption [10, 11, 30]. Anatomic reduction of the syndesmosis and ankle mortise is critical to restore normal joint biomechanics and tibiotalar contact forces in order to optimize outcomes [2, 19, 22, 27, 29]. Numerous studies indicate that syndesmotic injuries portend poorer prognosis in pain and function scores both short- and long-term, and anatomic syndesmotic reduction has been implicated in improved functional outcomes [5, 13, 29].
One of the most common techniques employed to address syndesmotic injuries utilizes reduction forceps to obtain reduction, followed by fluoroscopic assessment of reduction accuracy. Despite recognizing the importance of restoring anatomic relationships following these injuries, reports of syndesmotic malreduction range from 12 to 52% [3, 6, 7, 12, 29]. Additionally, many authors have demonstrated the unreliability of radiographic assessment of syndesmotic reduction in the coronal and sagittal planes and have cautioned on the high rates of malreduction [1, 3, 7]. Prior studies indicate that, outside of fibular fracture malreduction or intra-articular fragments, malreduction of the fibula within the incisura, whether by translation, rotation, or a combination thereof, is often caused by eccentric clamp or screw placement [16, 18, 20]. This highlights the importance of preventing clamp-generated malreduction of the fibula within the incisura by ensuring the vector created by the reduction clamp’s tines is in line with the trans-syndesmotic angle. However, there is a paucity of literature describing the tibiofibular anatomic relationship that should be recreated.
Given the high incidence of malreduction and the importance of restoring native anatomic relationships to improve patient prognosis, this study measured the anatomic syndesmotic angle in uninjured ankles. When the operative appearance of a clamp spanning the syndesmosis at the angle specific to each patient was simulated, the medial tine was positioned at a predictable location along the anterior tibia on lateral imaging. The reproducibility of this position on intraoperative fluoroscopy can help guide surgeon placement of reduction clamp tines across the syndesmosis.
Methods
After obtaining Institutional Review Board approval, adult patients with unilateral syndesmotic injury requiring fixation were prospectively identified. Postoperatively, patients received bilateral lower extremity CT scans to assess the accuracy of syndesmotic reduction. For purposes of this study, only the uninjured extremities were used to measure the native TSA and simulate reduction clamp positioning; the injured extremities were not included in this study. Although history of prior injury or instability was not documented, none of the uninjured extremities had evidence of prior surgery.
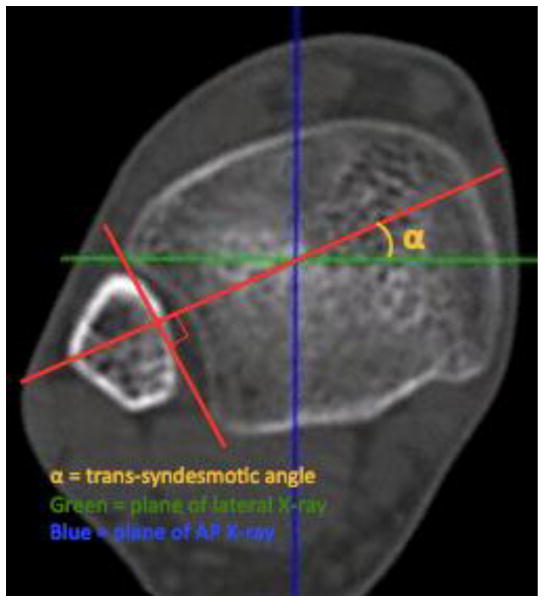
The TSA was defined as the angle between the plane of the true lateral ankle radiograph (in which the medial and lateral talar domes are superimposed) and a line drawn perpendicular to the tangent of the anterior and posterior borders of the fibular incisura (Figure 1). The reliability of the described measurements was assessed with use of an interclass correlation coefficient (ICC). The ICC was calculated between two independent observers who performed measurements at separate dates. The ICC was rated as poor (<0.2), fair (0.21 to 0.4), moderate (0.41 to 0.6), good (0.61 to 0.8), or very good (0.81 to 1). Measurements of the syndesmotic angle were made on an axial CT slice one centimeter proximal to the tibial plafond. Three-dimensional (3D) reconstructions of the CT scans were generated using Vitrea Core software (Vital Images, Minnetonka, MN). The 3D renderings were then used to create virtual two-dimensional (2D) images comparable to a true lateral ankle radiograph in which the medial and lateral ridges of the talar dome were superimposed. The plane of this 2D lateral representation was noted on the axial CT slice and provided the reference for the TSA. A line tangential to the anterior and posterior processes of the fibular incisura was made, and a line was then drawn perpendicular to this to measure the TSA.
Figure 1.
The trans-syndesmotic angle (TSA) was measured by drawing a line perpendicular to the incisura on an axial CT at 1 cm proximal to the tibial plafond, referenced from the plane of a talar dome lateral view of the ankle joint.
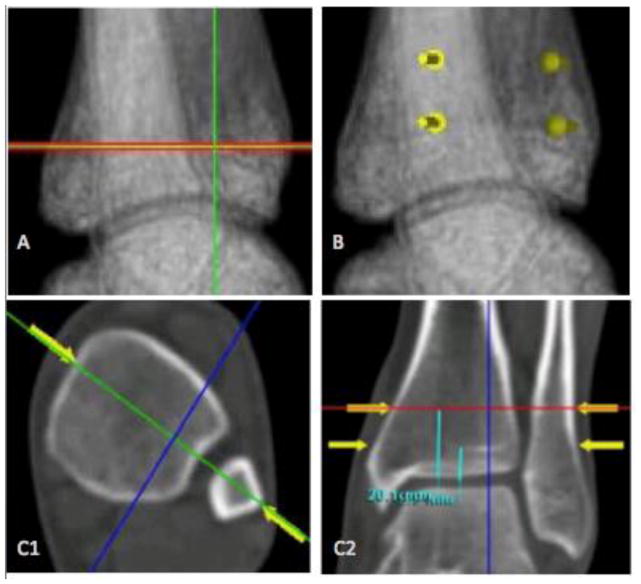
The 3D reconstructions were used to demonstrate clamp placement collinear with each patient’s TSA at one centimeter proximal to the tibiotalar joint line, starting with the lateral clamp tine placed on the lateral fibular ridge (Figure 2). The 3D reformats with anatomically based clamp placement were used to study clamp appearance as would be seen on intraoperative lateral ankle fluoroscopy. The anterior to posterior tibial diameter was measured on the 2D lateral reconstructions at one centimeter proximal to the plafond, and the location of the medial clamp tine was measured as a percentage of the distance from the anterior to posterior tibial cortex. Next, the distance from the anterior tibial cortex to the anterior fibular cortex was measured on the lateral 2D reconstructions, again one centimeter proximal to the plafond, and the location of the medial tine as a percentage of the distance from the anterior tibial cortex to the anterior fibular cortex was calculated. All measurements were then repeated at a distance two centimeters proximal to the plafond.
Figure 2.
To visualize clamp placement, three-dimensional CT reconstructions were reformatted to two-dimensional representations of radiographic images. (A) A talar dome lateral image was used to determine the plane for calculating the TSA. (B) Clamp positioning of the medial and lateral tines in line with the TSA as visualized on the simulated talar dome lateral image. (C1, C2) Axial and sagittal CT images demonstrating clamp placement collinear to the calculated TSA at 1 cm and 2 cm proximal to the tibial plafond, starting with the lateral clamp tine positioned on the fibular ridge.
The average medial clamp location was calculated with reference to (a) the anteroposterior tibial cortical diameter, and (b) the distance from the anterior tibial cortex to the anterior fibular cortex. For the anteroposterior tibial diameter calculations, the number of times the medial tine was positioned within the anterior one-third of the diameter was noted, and the number of times it fell within the middle one-third from the anterior tibial cortex to the anterior fibular cortex was determined.
Results
Measurement of the TSA
CT scans of 45 adult patients were available for analysis, ranging in age from 18 to 79 years (mean 40). There were 19 females and 26 males included in the study. The average trans-syndesmotic angle measured 21±5 degrees (range 12 to 30, median 20) anterior to the plane of a true lateral radiograph, with no statistical difference noted between males and females (TSA 20 and 22, respectively [p=0.49]). Interclass correlation coefficient for measurement of the TSA was 0.876, indicating very good reliability between independent observers.
Intraoperative Fluoroscopic Visualization of Clamp Placement
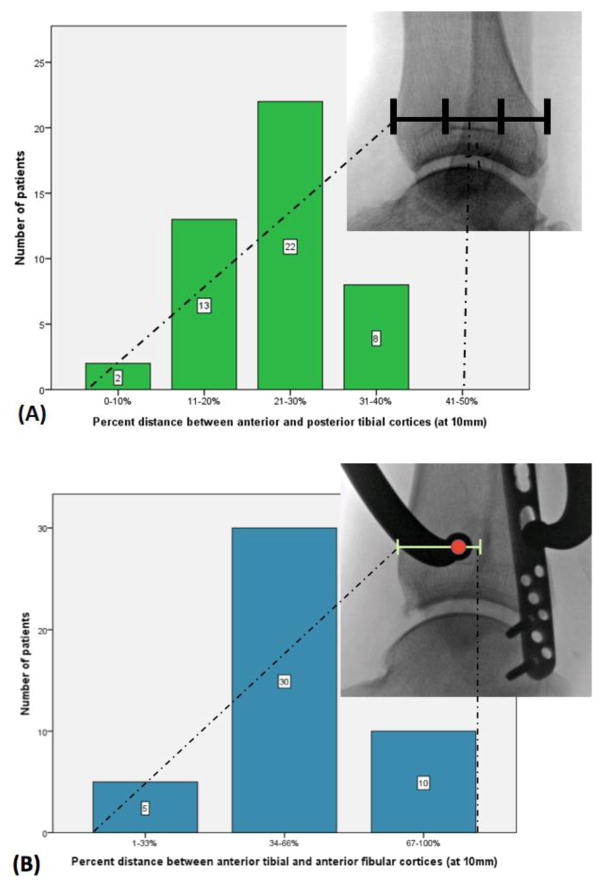
At one centimeter proximal to the tibial plafond, with the lateral tine placed on the fibular ridge and the clamp oriented along the TSA, the medial tine was, on average, 23±7% of the distance from the anterior tibial cortex to the posterior tibial cortex (range 7 to 39%, median 24%). In 33 (73%) ankles, the medial tine rested within this distribution of 23±7%. The medial tine was positioned within the anterior one-third of the tibia in 42 (93%) ankles (Figure 3), and fell within the second quartile 49% of the time. When referencing the anterior cortex of the fibula, the medial tine rested 53±17% of the distance between the anterior cortex of the tibia and the anterior cortex of the fibula (range 15 to 86%, median 52%), and 32 (71%) ankles fell into this distribution of 53±17%. The medial tine was within the central one-third of the space between the anterior tibial cortex and anterior fibular cortex 71% of the time (Figure 3) (Table 1). At two centimeters proximal to the tibial plafond, the medial tine was an average of 27±9% of the distance from the anterior to the posterior tibial cortices (range 8 to 47%, median 27%), and was within the anterior one-half in 45 (100%) ankles. The medial tine was in the anterior one-third of the anteroposterior tibial diameter in 36 (80%) ankles and within the second quartile 62% of the time. The medial tine was positioned at 50±17% of the distance between the anterior cortices of the tibia and fibula (range 13 to 83%, median 52%). The tine was within the central third of this space 73% of the time (Table 1).
Figure 3.
Using three-dimensional reconstructions, the lateral tine of a reduction forceps was positioned on the fibular ridge, and, with the clamp positioned along the TSA, the location of the medial tine on a simulated lateral fluoroscopy image was noted with respect to its position (A) from anterior to posterior along the tibia and (B) in the space between the anterior cortices of the tibia and fibula.
Table 1.
Percentage of ankles in which the medial tine fell into each third between the anterior tibial cortex and anterior fibular cortex at 10 mm and 20 mm proximal to the distal tibial joint line.
| Anterior Tibial to Anterior Fibular Cortices
| |||
|---|---|---|---|
| N=45 | Anterior 1/3 | Middle 1/3 | Posterior 1/3 |
| 10 mm | 9% | 71% | 20% |
| 20 mm | 11% | 73% | 16% |
Discussion
Ankle fractures with disruption of the distal tibiofibular ligaments are associated with poorer outcomes than injuries without syndesmotic instability [5, 13, 24, 29]. These injuries are at increased risk of progressing to early post-traumatic ankle arthritis, resulting in further pain and disability to patients [2, 19, 27, 29]. Despite the importance of anatomic reduction of the syndesmosis, malreduction is common [3, 7]. Given this disparity, there is a need to define better ways to judge the adequacy of reduction intraoperatively. In this study, we determined the anatomic TSA in uninjured ankles using CT imaging and then simulated syndesmotic clamp reduction along the TSA of each ankle. We found that when the lateral tine is first positioned on the fibular ridge and the clamp is oriented along the TSA, the medial tine predictably lies in the anterior one-third of the anteroposterior tibial diameter as visualized on a talar dome lateral radiograph, and within the central one-third of the distance from the anterior tibial cortex to the anterior fibular cortex.
The reported high frequency of syndesmotic malreduction can partly be attributed to the anatomy of the distal tibiofibular joint. The incisura is a shallow, concave surface in 75% of ankles, with the remainder being slightly convex or irregular [9]. The fibula typically lies asymmetrically within the incisura. In a study by Lepojarvi et al [12], 97% of the fibulas were positioned anteriorly or centrally. As such, any reduction vector that is not collinear with the true axis of the syndesmosis has the potential to malreduce the fibula within the incisura [11, 12, 16, 18, 20]. Coronal and sagittal alignment is readily measured on plain radiographs, and coronal malalignment has been the most frequently cited and measured in previous studies [16, 18, 20]. Malrotation has not been as well studied as translation with regards to syndesmotic reduction [16]. Significant displacement, rotation, and over-compression of the syndesmosis based on eccentric positioning of a reduction clamp has previously been demonstrated in a cadaveric model [16]. Conversely, reduction with a clamp oriented along the anatomic angle of the syndesmosis is unlikely to result in rotation or translation of the fibula, and should minimize the risk of over-compression of the syndesmosis [16, 26].
While numerous studies have examined cadaveric models of syndesmotic disruption and various methods of reduction, there has yet to be a description of the anatomy of the trans-syndesmotic angle [4, 14, 21, 20]. This information is crucial given prior studies that emphasize the importance of anatomic syndesmotic reduction. Classically, syndesmotic screws are placed at 30 degrees from the coronal plane [11, 30]. In this study, we determined the anatomic TSA in 45 uninjured adult ankles and found that the average syndesmotic angle was less than this historically accepted value, averaging 21±5 degrees anterior to the plane of a lateral radiograph.
As noted in prior literature, current radiographic measurements are unreliable for final assessment of reduction [1, 3, 14, 21]. A study by Gardner et al [7] noted a 52% rate of malreduction of the syndesmosis, only half of which were identified postoperatively on plain radiographic imaging alone. Furthermore, even direct visualization of the syndesmosis via open reduction resulted in up to a 16% malreduction rate on postoperative imaging [17, 24]. These studies are illustrative of the necessity to develop innovative means to judge reduction intraoperatively. However, there are few studies that describe such techniques to prevent malreduction. Several authors have investigated the use of intraoperative CT, which, while improving intraoperative detection of malreduction, does not eliminate its occurrence and adds cost and time to the operative procedure [3, 4, 6, 23].
Intraoperative fluoroscopy is familiar and frequently utilized by surgeons. The current study directly measured the trans-syndesmotic angle in uninjured ankles and used those individualized measurements to radiographically position a simulated clamp along that axis. This method enabled us to visualize the appearance of an anatomically positioned clamp on a true lateral radiograph as would be seen intraoperatively. By first calculating the TSA, our study was able to demonstrate that an anatomically directed reduction clamp will have a predictable appearance on lateral radiographs.
At one centimeter proximal to the plafond, the medial tine was 23±7% of the distance from the anterior to the posterior tibial cortex. The medial tine was positioned in this range in 33 of 45 (73%) ankles in this study and was positioned in the anterior one-third of the tibia in 42 of 45 (93%) ankles. With reference to the anterior fibular cortex, the medial tine was positioned 53±17% of the distance between the anterior cortices of the tibia and fibula, and 32 of 45 (71%) ankles demonstrated placement of the medial tine within this range. As tine placement moved from one to two centimeters proximal to the plafond, the medial tine trended more toward the fibula. While the exact value of the TSA will frequently not be known intraoperatively, these numbers suggest that clamp positioning during syndesmotic reduction can be guided by careful attention to clamp tine location on lateral ankle fluoroscopy. By using this method, care must be taken to ensure accurate initial clamp placement laterally and that the lateral tine does not shift anteriorly or posteriorly during placement of the medial tine. Importantly, the position of the clamp should be assessed on a true lateral radiograph of the ankle, or one in which the medial and lateral ridges of the talar dome are superimposed, as rotation will affect the appearance of clamp location on a two-dimensional image.
Prior studies that have evaluated clamp placement as it relates to syndesmotic reduction have used cadaveric specimens to recreate syndesmotic injuries followed by clamp application at various vectors across the syndesmosis. Phisitkul et al placed clamps at three predetermined orientations across the syndesmosis and obtained CT scans to evaluate the reduction [20]. Miller et al performed a similar experiment, although the lateral tine was maintained on the fibular ridge and the medial tine was placed at three different positions [16]. Similarly to the study by Phisitkul et al, reduction adequacy was determined by assessing axial CT scans. While the studies effectively demonstrated that clamp placement affects reduction, the positioning of the clamps was arbitrary and without an anatomical basis. Furthermore, the axial CT scans were not standardized based on lateral fluoroscopy, limiting the ability to determine intraoperative correlation to their results.
Recently, Grenier et al described the anteroposterior tibiofibular ratio as an intraoperative assessment of syndesmotic reduction [8]. This method states the anterior fibular cortex crosses the tibial physeal scar at the midpoint of a line crossing that point and the anterior tibial cortex at the level of the physeal scar. While they showed good reproducibility in its measurement, the ratio does not take into account the syndesmotic axis, nor does it provide guidance for positioning a clamp during reduction. Summers et al described using intraoperative true talar dome lateral radiographs of the contralateral uninjured extremity to assess the anteroposterior alignment of the fibula with respect to the anterior and posterior tibial cortices [25]. However, while this method is a useful adjunct to assist with the final anterior to posterior fibular position with respect to the tibia, it cannot be utilized when bilateral lower extremities are injured, and, again, does not aid with clamp positioning.
Our study has limitations. One of the weaknesses lies in the study being entirely radiographic. The simulated intraoperative clamp positions were created by generating 2D images from 3D CT reconstructions. Furthermore, all of the ankles analyzed were uninjured. Extremity trauma results in injury to both the skeletal structures as well as to the soft tissue envelope that aids in bony stabilization. Clinical studies will be necessary to validate the presented methodology in pathologic ankles.
Care must be taken in cases where the syndesmosis is widely displaced. In such situations, clamp placement, even if oriented along the TSA, may still result in malreduction. In the majority of injury patterns, however, the fibula is mildly displaced within the incisura with residual diastasis evident on imaging. Further, there may be small changes in the radiographic clamp tine position depending on depth of tine penetration into bone due to poor bone quality or type of reduction clamp used.
While our study provides insight into obtaining an anatomic syndesmotic reduction, it does not provide information on patient outcomes. There has not been a study to date that satisfactorily addresses the effects of syndesmotic malreduction on patient outcomes, or even whether the poorer outcomes associated with syndesmotic injuries are a result of high malreduction rates or are due to the injury itself. Additional studies are necessary to determine whether functional outcomes are correlated with anatomic reduction, and if so, to what degree and whether there is a difference in patient outcome between translational or rotational malreductions. It is possible that syndesmotic fixation with a suture button construct may be more lenient than screw fixation and allow greater laxity and forgiveness, although cost and rotational control of a suture-button construct remain concerns.
In conclusion, this study determined the anatomic TSA in uninjured ankles and then simulated syndesmotic clamp reduction along the TSA of each ankle. The results demonstrate that regardless of variability in the anatomy of the ankle syndesmosis between patients, routine intraoperative use of a true lateral fluoroscopic view can guide clamp placement, and thereby potentially minimize the risk of clamp-generated malreduction. Placing the medial clamp tine in the anterior third of the anteroposterior tibial diameter, or half way between the anterior tibial cortex and anterior fibular cortex on a lateral ankle radiograph appears to be the most accurate position for reduction based on the trans-syndesmotic angle.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Beumer A, van Hemert WL, Niesing R, Entius CA, Ginai AZ, Mulder PG, et al. Radiographic measurement of the distal tibiofibular syndesmosis has limited use. Clinical orthopaedics and related research. 2004;(423):227–34. doi: 10.1097/01.blo.0000129152.81015.ad. [DOI] [PubMed] [Google Scholar]
- 2.Chissell HR, Jones J. The influence of a diastasis screw on the outcome of Weber type-C ankle fractures. The Journal of bone and joint surgery British volume. 1995;77(3):435–8. [PubMed] [Google Scholar]
- 3.Davidovitch RI, Weil Y, Karia R, Forman J, Looze C, Liebergall M, et al. Intraoperative syndesmotic reduction: three-dimensional versus standard fluoroscopic imaging. The Journal of bone and joint surgery American volume. 2013;95(20):1838–43. doi: 10.2106/JBJS.L.00382. [DOI] [PubMed] [Google Scholar]
- 4.Ebraheim NA, Lu J, Yang H, Mekhail AO, Yeasting RA. Radiographic and CT evaluation of tibiofibular syndesmotic diastasis: a cadaver study. Foot & ankle international. 1997;18(11):693–8. doi: 10.1177/107110079701801103. [DOI] [PubMed] [Google Scholar]
- 5.Egol KA, Pahk B, Walsh M, Tejwani NC, Davidovitch RI, Kovak KJ. Outcome after unstable ankle fracture: effect of syndesmotic stabilization. Journal of orthopaedic trauma. 24(1):7–11. doi: 10.1097/BOT.0b013e3181b1542c. [DOI] [PubMed] [Google Scholar]
- 6.Franke J, von Recum J, Suda AJ, Grutzner PA, Wendl K. Intraoperative three-dimensional imaging in the treatment of acute unstable syndesmotic injuries. The Journal of bone and joint surgery American volume. 2012;94(15):1386–90. doi: 10.2106/JBJS.K.01122. [DOI] [PubMed] [Google Scholar]
- 7.Gardner MJ, Demetrakopoulos D, Briggs SM, Helfet DL, Lorich DG. Malreduction of the tibiofibular syndesmosis in ankle fractures. Foot & ankle international. 2006;27(10):788–92. doi: 10.1177/107110070602701005. [DOI] [PubMed] [Google Scholar]
- 8.Grenier S, Benoit B, Rouleau DM, Leduc S, Laflamme G, Liew A. APTF: anteroposterior tibiofibular ratio, a new reliable measure to assess syndesmotic reduction. Journal of orthopaedic trauma. 2013;27(4):207–11. doi: 10.1097/BOT.0b013e31826623cc. [DOI] [PubMed] [Google Scholar]
- 9.Hocker K, Pachucki A. The fibular incisure of the tibia. The cross-sectional position of the fibula in distal syndesmosis. Der Unfallchirurg. 1989;92(8):401–6. [PubMed] [Google Scholar]
- 10.Huber T, Schmoelz W, Bolderl A. Motion of the fibula relative to the tibia and its alterations with syndesmosis screws: A cadaver study. Foot Ankle Surg. 2012;18(3):203–9. doi: 10.1016/j.fas.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 11.Kennedy MT, Carmody O, Leong S, Kennedy C, Dolan M. A computed tomography evaluation of two hundred normal ankles, to ascertain what anatomical landmarks to use when compressing or placing an ankle syndesmosis screw. Foot (Edinburgh, Scotland) 2014;24(4):157–60. doi: 10.1016/j.foot.2014.07.001. [DOI] [PubMed] [Google Scholar]
- 12.Lepojarvi S, Pakarinen H, Savola O, Haapea M, Sequeiros RB, Niinimaki J. Posterior translation of the fibula may indicate malreduction: CT study of normal variation in uninjured ankles. Journal of orthopaedic trauma. 2014;28(4):205–9. doi: 10.1097/BOT.0b013e3182a59b3c. [DOI] [PubMed] [Google Scholar]
- 13.Lubbeke A, Salvo D, Stern R, Hoffmeyer P, Holzer M, Assal M. Risk factors for post-traumatic osteoarthritis of the ankle: an eighteen year follow-up study. Int Orthop. 2012;36(7):1403–10. doi: 10.1007/s00264-011-1472-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Marmor M, Hansen E, Han HK, Buckley J, Matityahu A. Limitations of standard fluoroscopy in detecting rotational malreduction of the syndesmosis in an ankle fracture model. Foot & ankle international. 32(6):616–22. doi: 10.3113/FAI.2011.0616. [DOI] [PubMed] [Google Scholar]
- 15.McBryde A, Chiasson B, Wilhelm A, Donovan F, Ray T, Bacilla P. Syndesmotic screw placement: a biomechanical analysis. Foot & ankle international. 1997;18(5):262–6. doi: 10.1177/107110079701800503. [DOI] [PubMed] [Google Scholar]
- 16.Miller AN, Barei DP, Iaquinto JM, Ledoux WR, Beingessner DB. Iatrogenic syndesmosis malreduction via clamp and screw placement. Journal of orthopaedic trauma. 2013;27(2):100–6. doi: 10.1097/BOT.0b013e3182a70221. [DOI] [PubMed] [Google Scholar]
- 17.Miller AN, Carroll EA, Parker RJ, Boraiah S, Helfet DL, Lorich DG. Direct visualization for syndesmotic stabilization of ankle fractures. Foot & ankle international. 2009;30(5):419–26. doi: 10.3113/FAI.2009.0419. [DOI] [PubMed] [Google Scholar]
- 18.Nimick CJ, Collman DR, Lagaay P. Fixation orientation in ankle fractures with syndesmosis injury. The Journal of foot and ankle surgery : official publication of the American College of Foot and Ankle Surgeons. 2013;52(3):315–8. doi: 10.1053/j.jfas.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 19.Pettrone FA, Gail M, Pee D, Fitzpatrick T, Van Herpe LB. Quantitative criteria for prediction of the results after displaced fracture of the ankle. The Journal of bone and joint surgery American volume. 1983;65(5):667–77. [PubMed] [Google Scholar]
- 20.Phisitkul P, Ebinger T, Goetz J, Vaseenon T, Marsh JL. Forceps reduction of the syndesmosis in rotational ankle fractures: a cadaveric study. The Journal of bone and joint surgery American volume. 2012;94(24):2256–61. doi: 10.2106/JBJS.K.01726. [DOI] [PubMed] [Google Scholar]
- 21.Pneumaticos SG, Noble PC, Chatziioannou SN, Trevino SG. The effects of rotation on radiographic evaluation of the tibiofibular syndesmosis. Foot & ankle international. 2002;23(2):107–11. doi: 10.1177/107110070202300205. [DOI] [PubMed] [Google Scholar]
- 22.Ramsey PL, Hamilton W. Changes in tibiotalar area of contact caused by lateral talar shift. The Journal of bone and joint surgery American volume. 1976;58(3):356–7. [PubMed] [Google Scholar]
- 23.Richter M, Zech S. Intraoperative 3-dimensional imaging in foot and ankle trauma-experience with a second-generation device (ARCADIS-3D) Journal of orthopaedic trauma. 2009;23(3):213–20. doi: 10.1097/BOT.0b013e31819867f6. [DOI] [PubMed] [Google Scholar]
- 24.Sagi HC, Shah AR, Sanders RW. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. Journal of orthopaedic trauma. 26(7):439–43. doi: 10.1097/BOT.0b013e31822a526a. [DOI] [PubMed] [Google Scholar]
- 25.Summers HD, Sinclair MK, Stover MD. A reliable method for intraoperative evaluation of syndesmotic reduction. Journal of orthopaedic trauma. 2013;27(4):196–200. doi: 10.1097/BOT.0b013e3182694766. [DOI] [PubMed] [Google Scholar]
- 26.Tornetta P, 3rd, Spoo JE, Reynolds FA, Lee C. Overtightening of the ankle syndesmosis: is it really possible? The Journal of bone and joint surgery American volume. 2001;83-A(4):489–492. doi: 10.2106/00004623-200104000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Valderrabano V, Horisberger M, Russell I, Dougall H, Hintermann B. Etiology of ankle osteoarthritis. Clinical orthopaedics and related research. 2009;467(7):1800–6. doi: 10.1007/s11999-008-0543-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Verim O, Er MS, Altinel L, Tasgetiren S. Biomechanical evaluation of syndesmotic screw position: a finite-element analysis. Journal of orthopaedic trauma. 2014;28(4):210–5. doi: 10.1097/BOT.0b013e3182a6df0a. [DOI] [PubMed] [Google Scholar]
- 29.Weening B, Bhandari M. Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. Journal of orthopaedic trauma. 2005;19(2):102–8. doi: 10.1097/00005131-200502000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Zalavras C, Thordarson D. Ankle syndesmotic injury. The Journal of the American Academy of Orthopaedic Surgeons. 2007;15(6):330–9. doi: 10.5435/00124635-200706000-00002. [DOI] [PubMed] [Google Scholar]