Supplemental Digital Content is available in the text
Keywords: gait, lateral wedge arch support insoles, meta-analysis, osteoarthritis
Abstract
Objective:
The aim of this study was to evaluate the immediate effects of lateral wedge arch support insoles (LWAS) on reducing the knee joint load in patients with medial knee osteoarthritis (OA) compared with an appropriate control.
Methods:
Databases including Medline, EMBASE, Web of Science, Wiley Online Library, Cochrane library, and Google Scholar were searched with no limits on study date or language, from the earliest available date to October 31, 2016. The included studies had to have the aim of reducing knee load and have an appropriate control. The main measured values were the first and second peak external knee adduction moments (EKAM) and the knee adduction angular impulse (KAAI). The random-effects model was used for analyzing the eligible studies.
Results:
Nine studies met the inclusion criteria with a total of 356 participants of whom 337 received LWAS treatment. The risk of methodological bias scores (quality index) ranged from 21 to 27 of 32. Treatment with LWAS resulted in statistically significant reductions in the first peak EKAM (P = .005), the second peak EKAM (P = .01), and the KAAI (P = .03). However, among trials in which the control treatment was control shoes, the LWAS showed no associations on the first peak EKAM (P = .10) or the KAAI (P = .06); among trials in which the control treatment was neutral insoles, the LWAS showed no associations on the second peak EKAM (P = .21) or the KAAI (P = .23). At the same time, the LWAS showed no statistically significant reduction on the first peak EKAM (P = .39) when compared with flat insoles.
Conclusion:
Although meta-analysis outcomes of all studies indicated statistically significant associations between LWAS and reductions of the first peak EKAM, second peak EKAM and KAAI in people with medial knee OA while walking, different results existed in subgroups using various control conditions for comparison. These findings do not support the use of LWAS insoles for reducing knee load. An optimal LWAS treatment should provide the appropriate height of arch support and amount of lateral wedging. Further research should investigate the best combination of these 2 parameters to achieve efficacy without altered comfort.
1. Introduction
Knee osteoarthritis (OA) is a leading cause of knee pain and disability with substantial personal and economic burden in the elderly population and is one of the most common musculoskeletal disorders in the world.[1–4] Knee OA typically affects the medial tibiofemoral joint compartment[5,6] with a 10-fold propensity compared with the lateral compartment of the knee.[7] This discrepancy has been attributed to the higher loads[8] which the medial compartment carries, approximately 60% to 91% of the total knee load.[9–11] The unequal distribution of the transmitted load is because the line of force acting at the foot passes medially to the knee joint, producing the external knee adduction moment (EKAM).[12] As a commonly reported gait outcome measure in studies in the population with knee OA, the EKAM has consistently emerged as a valid surrogate to assess dynamic load on the medial compartment.[13–18] However, although limitations exist,[19,20] together with knee adduction angular impulse (KAAI), the first peak EKAM and second peak EKAM have been the main variables investigated in recent studies[20–22] owing to their relationship with medial contact force at the knee joint and OA progression.[13,19]
Unfortunately, there is currently no cure for this mechanically induced disease. Therefore, nonsurgical conservative management is of vital importance for this disease. Given that gait biomechanics have been associated with knee OA progression,[14–17] there has been much focus on modifying the gait biomechanical parameters mentioned previously with conservative interventions, such as varied orthotics directly influencing foot, ankle, and knee relationships with lower limb mechanics. Compared to surgical strategies such as high tibial osteotomy (HTO), unicompartmental knee replacement or total knee replacement aiming to alter static lower extremity alignment, orthotic treatment like knee braces or foot insoles can alter loading to the knee in the hope of reducing symptoms and disease progression.[23] The lateral wedge insole (LWI) is a wedge placed under the sole of the foot and angulated so that it is thicker at the lateral part than the medial edge, transferring loading from the medial to the lateral knee joint during weight bearing. Although different groups have promulgated different recommendations,[24–26] biomechanical studies have demonstrated an effect size in reduction of EKAM ranging from 4% to 12% with an LWI of at least 5 degrees.[20,27–35] However, the LWI can be uncomfortable for patients with knee OA[36] owing to the more pronated position.
The LWAS are lateral wedge insoles with added medial arch support (also called lateral wedge arch support insoles) aimed at minimizing the increase in the subtalar valgus angle to make patients more comfortable while maintaining their ability to reduce the EKAM during the late stance phase of gait. Recent studies have tested the effect on EKAM of adding an arch support to the LWI during gait but showed inconsistent findings.[21,23,29,37–46] Some authors found a reduction in the EKAM during the stance phase of gait using a lateral wedge and an arch support.[21,39–42,44–46] However, in some patients, no reductions[23,28] or smaller reductions[46] on the EKAM were observed. There is a lack of consensus on whether this kind of device should be recommended.
A recent meta-analysis evaluating the effect of LWI on biomechanical risk factors for knee OA progression reported small reductions, but the authors did not discuss the effect of the LWAS by distinguishing different types of interventions.[47] However, the LWAS played an important role and became more common in the conservative treatment of knee OA. The objective of this review was to assess the effects of LWAS on reductions of knee load in patients with knee OA by measuring biomechanical outcomes during gait analysis.
2. Materials and methods
2.1. Literature search
This review protocol has been published on the International Prospective Register of Systematic Reviews (PROSPERO, CRD 42017056749). The meta-analysis was programed on the basis of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement guidelines.[48] Several electronic databases were searched from the earliest available date to October 31, 2016, including Medline (via Pubmed), EMBASE (via OvidSP), Web of Science (via ISI Web of Knowledge), the Wiley Online Library, and Cochrane library. To cover any missing data, Google Scholar was also searched and screened with no limitation on study dates or any language restrictions. To improve the specificity and sensitivity of searching, we used Boolean logic operators “AND or OR” to combine the key words as a search strategy as follows: (“lateral wedge∗” OR “medial arch∗”) AND osteoarthritis. In the Wiley Online Library and Google Scholar, we used the search strategy: “lateral wedge∗” AND “medial arch∗,” AND osteoarthritis AND gait. Before initiating the screening, each database was searched by 2 independent researchers (F.X. and B.L.) to achieve agreement on the number of search hits achieved in each database.
2.2. Inclusion criteria
Studies considered eligible must have met certain criteria. First, study design: randomized controlled trials (RCTs), quasi-RCTs, and prospective cohort studies. For prospective studies, only baseline data inferring the immediate effects of LWAS were used. Second, population: adults with symptomatic diagnosed medial knee OA according to the clinical[49,50] and radiological[51] criteria. Third, intervention: LWAS, generally defined as an in-shoe orthotic device with an angle of inclination toward the lateral border of the foot with an added arch support at the medial side. Fourth, comparator: control shoe (standard or patient's own shoes) with a flat insole or neutral insole (with medial arch). Fifth, outcomes: the first or second peak EKAM or the KAAI, Sixth, test condition: walking stably on the ground.
2.3. Exclusion criteria
Studies considered ineligible contained one of the following features: allowing greater than a 1-month period of wear. (As mentioned in other studies, this is the longest time period where effects are not shown to decline with continued wear[27,52]); enrolling healthy participants; using footwear as a comparator, which is known independently to alter knee biomechanics; testing “variable stiffness” shoes whose features could vary across the test;[53,54] testing the condition of walking on a slope, upstairs, or downstairs.
2.4. Study inclusion
After importing the articles from the search of the aforementioned databases into the reference management software (Endnote X7), duplicate references were first removed. The eligibility criteria were applied to the title and abstract by 4 independent researchers (F.X., B.L., MJ.K., and JX.M.), with the retained articles cross-checked once more. Nineteen articles were retrieved in full-text and screened by reading the whole article; finally, 9 articles remained and formed the basis of this systematic review. Reference lists of previous related reviews were also screened and searched to prevent any missing data. Any differences of opinion between the 4 independent researchers were resolved by discussion initially; the opinion of the other researcher (Y.W.) was considered if consensus was not reached.
2.5. Quality assessment
Two independent reviewers (F.X. and B.L.) assessed each individual study using the Quality Index,[55] which contained 27 items relevant to a range of study designs and was still applicable to randomized studies. Each study was scored according to the scale with each item graded as yes (1 point), no (0 points), or unable to determine (0 points) to give a total score out of 32. The 27 items assessed not only the quality of reporting, internal validity (bias and confounding) and power but also the external validity.[55]
2.6. Data extraction
Two reviewers (F.X. and B.L.) independently extracted relevant data from the eligible literature including the title, publication year, first author and country, demographics of the patients, sample size, features of interventions, and descriptive (means, standardized differences) and inferential (P values and confidence intervals) statistical information. Once adequate data were reported, standardized mean differences (SMDs) were calculated as the mean difference of the biomechanical outcomes (peak EKAMs and KAAI) between interventions and control groups, divided by the pooled SD, with adjustment for small sample sizes (Hedges).[56] All data needed for calculations could be extracted directly from eligible articles. Corresponding authors of the included studies were contacted by E-mail if more information was required or needed to be confirmed.
2.7. Data synthesis and statistical methods
Review Manager Software for Windows (RevMan version 5.3., 2014) was used to perform the meta-analysis and present the results, using the inverse variance method.
Study heterogeneity was estimated through the I2 statistic test, subsequent χ2, and Cochran Q test in accordance with the values of I2 and P. Heterogeneity was interpreted by Guidelines from the Cochrane Collaboration, according to which, 25%, 50%, and 75% represent low, moderate, and high heterogeneity, respectively.[57] A fixed-effects model could be used if I2 <50% and P > .1. However, significant heterogeneity across studies was anticipated because of differences in comparators and the distribution of participant characteristics (i.e., severity of OA); therefore, a random-effects model was used to more conservatively estimate the pooled effect of the interventions.
For continuous outcomes, SMDs and 95% confidence intervals (95% CIs) were used to weigh the effect size. Effect sizes were interpreted as 0.2 (small), 0.5 (medium), and 0.8 (large).[58] To contextualise the effect sizes, the overall pooled estimates were back-transformed into original units using reference data from the largest study[44] (n = 70) with mean ± SD 0.39 ± 0.16 (Nm/kg) for the first peak EKAM, 0.33 ± 0.14 (Nm/kg) for the second peak EKAM, and 0.16 ± 0.07 (Nm/kg∗s) for the KAAI.
If a neutral insole or flat insole was present, a subgroup analysis was also performed to assess the effects of these different comparators on altering the biomechanical differences, as their use previously has been shown to influence clinical outcomes.[47,59] Publication bias was assessed using funnel plots with Begg and Egger regression test using STATA (version 12).
3. Results
3.1. Search results
A total of 845 records were identified according to the search strategy and abstracts (Fig. 1). Two related articles not published in English (1 Korean and 1 Iraqi) were excluded because they did not meet our criteria. Nine studies were considered eligible, after reading the full text, and included in the final review. Reference lists of several review articles were searched with no additional studies found. Two authors of 3 studies provided some useful information about the researches and 2 related studies,[39,60] which confirmed parts of another larger research study were excluded eventually.
Figure 1.
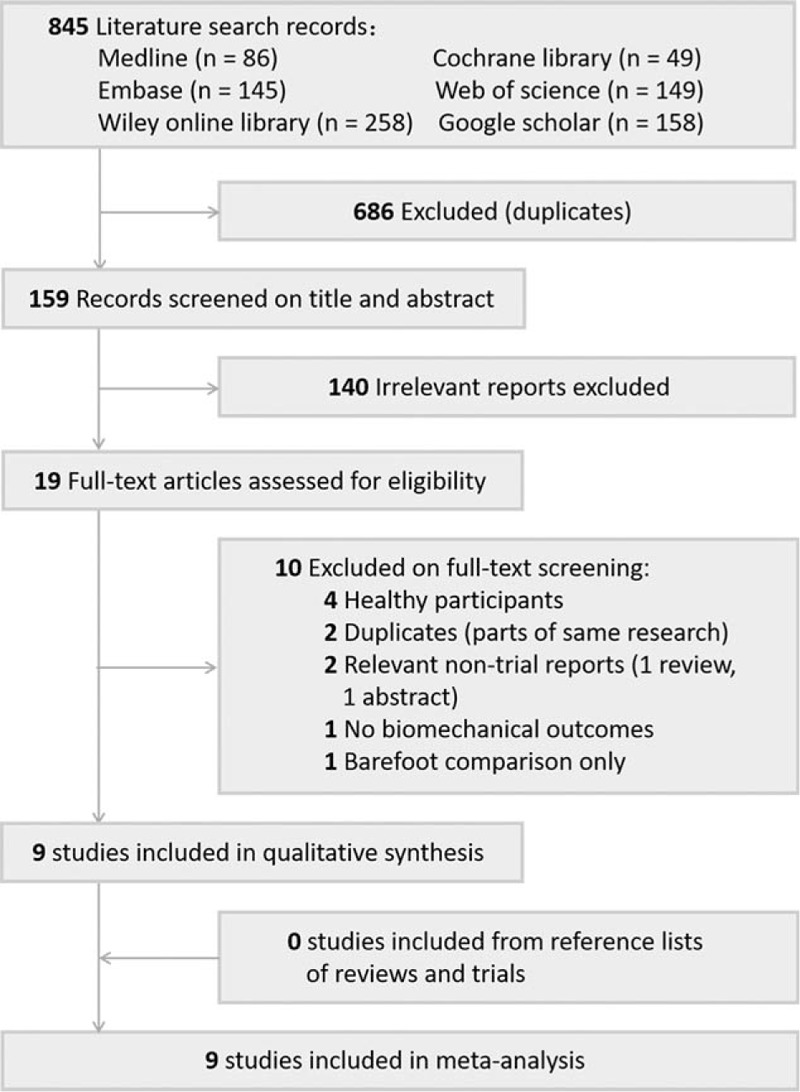
Review flow chart.
3.2. Study characteristics
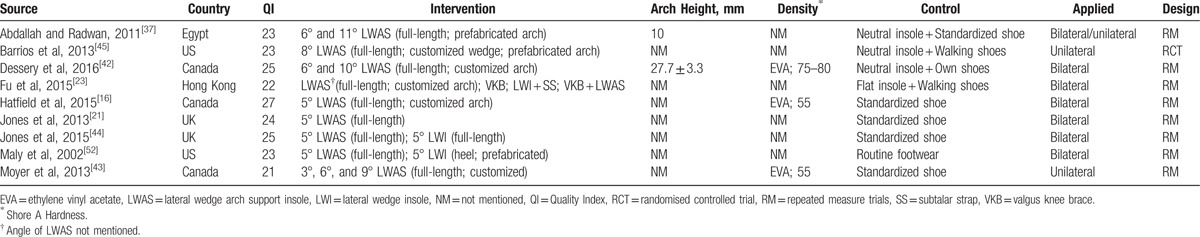
Eventually, 9 eligible studies were enrolled. Eight studies had repeated-measures designs and 1 was a RCT.[45] Full-length insoles were used in 8 studies and 1 study included both heel and full-length insoles.[49] The inclination angles of insoles ranged from 3 degrees[43] to 11 degrees[37] and the most common angle was 5 degrees.[21,44,46,52] With regard to the medial arch support, 5 used a custom design based on patient comfort,[16,21,23,42,43] and 3 studies used prefabricated arch supports.[37,45,52] The remaining study did not report these data.[44] Only 1 study used a flat insole as the comparison condition,[23] 3 studies used neutral insoles,[37,42,45] and 5 studies[16,21,43,44,52] used standardized footwear or patients’ usual shoes. Only 2 studies reported the height of the arch support[37,42] and 3 studies reported the density of the lateral wedge[42,43,46] (Table 1).[16,21,23,37,42–45,52]
Table 1.
Characteristics of included researches.
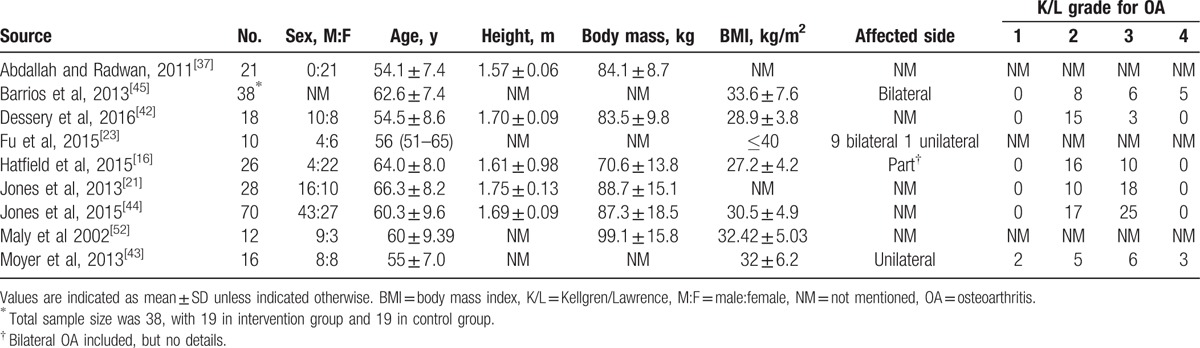
Totally, 337 participants were included. To represent the severity of knee pain, visual analogue scale (VAS) was used in 4 articles (mostly >3/10)[23,37,42,45] and the WOMAC (Western Ontario and McMaster Universities) OA index pain subscale was used in another 4 articles (mostly >30/100).[21,23,42,49] It is worth mentioning that, in different articles, pain level was recorded during level walking,[44,45] during moderate activities,[42] and on most days of the last week,[16] last 2 weeks,[21] or last 1 month.[23,37] Moreover, the Kellgren/Lawrence grade was used as radiographic assessment in most studies with a result as below: grade 2 or grade 3 in 4 articles[21,37,42,44], grade ≥2 in another 4 articles.[16,23,43,45] And criteria of the ACR (American College of Rheumatology) were used in 4 studies.[23,37,42,45] Three articles reported that the medial joint space was narrower than the lateral joint[21,42–45] and the varus knee alignment was also reported in several studies[23,37,42,43,49] (Table 2).[16,21,23,37,42–45,52]
Table 2.
Demographics of included studies.
3.3. Results of risk bias
The Quality Index scores of included studies ranged from 21 to 27 of 32 (Table 1). Agreement was finally reached by 2 reviewers (F.X. and B.L.). Only 1 study[42] described their interventions completely (item 4), whereas most studies failed to report the arch height and the density of the material used. Most studies also failed to report the sampling methods for recruitment (item 11) and the proportion of participants who agreed to participate from the initial recruitment (item 12). Few studies had adequate reports on these 2 items.[21,44] All studies failed to report whether assessors were masked during the analysis of primary outcome measures (item 15). And a few studies[16,42,45] reported that they performed an adequate allocation but did not report the sequence (item 24) (see Supplemental Table 1, which demonstrates full scoring results).
3.4. Results of meta-analysis
3.4.1. First peak EKAM
Effect of LWAS on the first peak EKAM was reported in 9 studies. Among these studies, 5 used a shoe-only comparison, 2 used a neutral insole (with arch support), 1 used a flat insole (without arch support), and 1 used both the neutral insole and flat insole. Data synthesis included data from 15 comparisons (7 shoe-only comparisons, 7 neutral insole comparisons, and 1 flat insole comparison); however, some studies made multiple comparisons with different insole angles (Table 3).[16,21,23,37,42–45,52]
Table 3.
Summary of comparisons in the analysis of parameters.
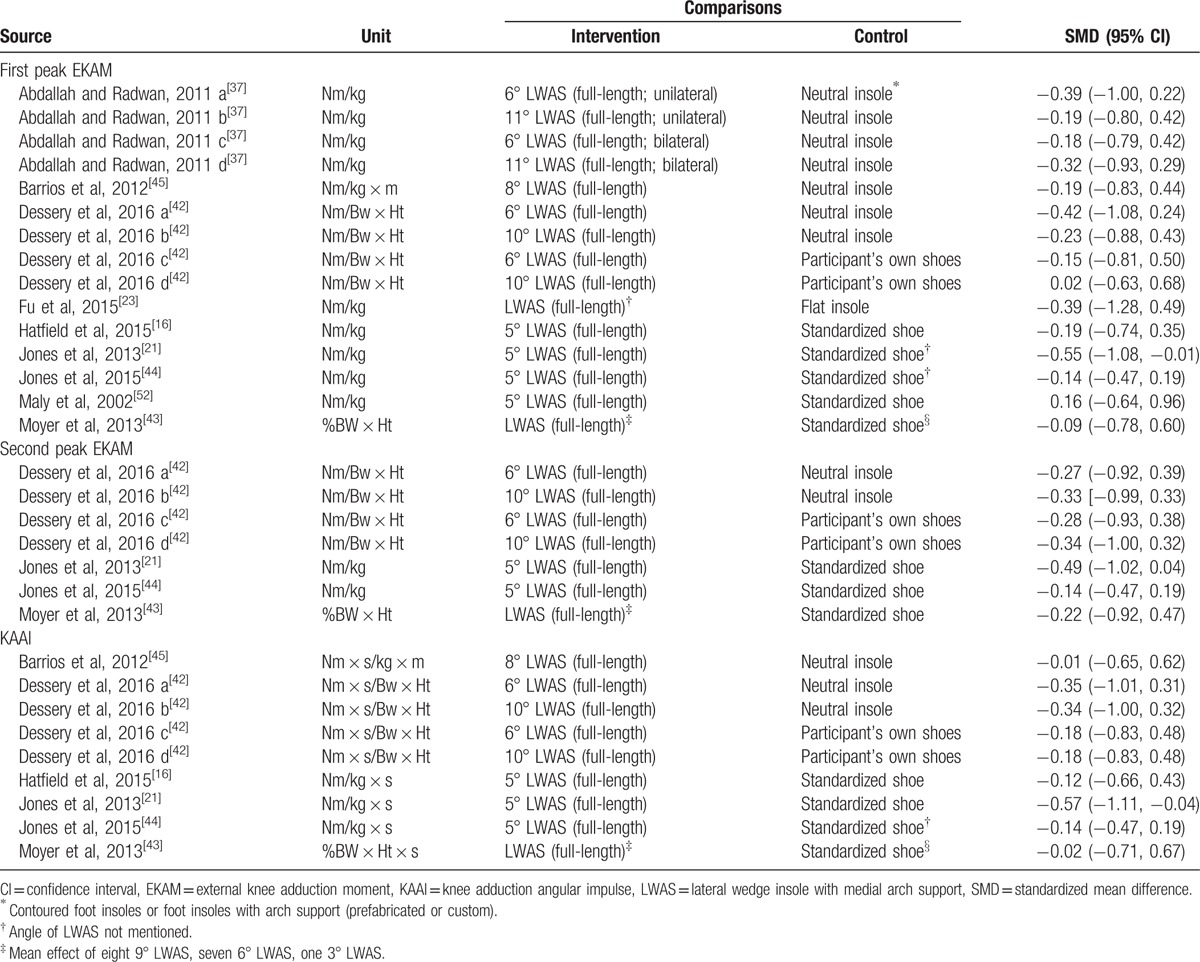
The overall pooled-effect estimate demonstrated that LWAS significantly reduced the first peak EKAM (SMD −0.22; 95% CI, −0.37 to −0.07; P = .005). This represents a small effect size and translates into an absolute change in the first peak EKAM of approximately −0.03 Nm/kg. Low statistical heterogeneity was found (χ2 = 1.30, P = .97, I2 = 0%) (Fig. 2).
Figure 2.
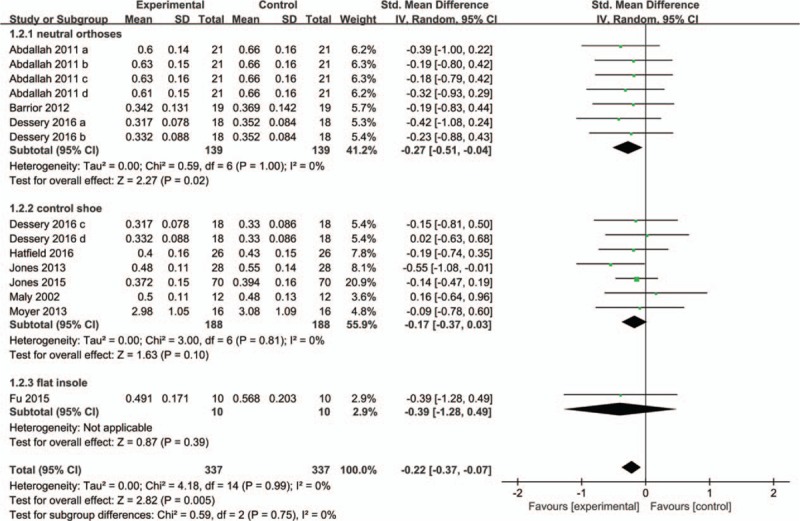
Forest plot of synthetic data for the first peak external knee adduction moment. The green squares indicate the effect size of every study. The transverse lines show the 95% CI. Black diamond represents the pooled estimate of every subgroup and the total effect. CI = confidence interval, SD = standardized errors.
Subgroup comparisons yielded different pooled effects. Among trials in which the control treatment was neutral insoles, the LWAS resulted in a statistically significant reduction on the first peak EKAM (SMD, −0.27; 95% CI, −0.51 to −0.04; P = .02; I2 = 0%; n = 7). However, the LWAS showed no associations on the first peak EKAM compared to both the shoe-only condition (SMD, −0.17; 95% CI, −0.37 to 0.03; P = .10; I2 = 0%; n = 7) and the flat insole condition (SMD −0.39; 95% CI, −1.28 to 0.49; n = 1). Begg test (P = .921, see Supplemental Figure 1, which shows the Begg funnel plot) and Egger test (SE = 0.63, P = .880, see Supplemental Figure 2, which demonstrates the Egger publication bias plot) for funnel plot asymmetry were not statistically significant, indicating weak evidence of publication bias for the first peak EKAM.
3.4.2. Second peak EKAM
Effect of LWAS on the second peak EKAM was reported in 4 studies, among which 3 studies used a shoe-only comparison, 1 study reported both neutral insole comparison and shoe-only comparison. Data synthesis included data from a total of 7 comparisons (Table 3).
The overall pooled-effect estimate demonstrated that LWAS significantly reduced the second peak EKAM (SMD −0.26; 95% CI, −0.47 to −0.06; P = .01). This represents a small effect size and translates into an absolute change in the first peak EKAM of approximately −0.02 Nm/kg. Low statistical heterogeneity was found (χ2 = 1.30, P = .97, I2 = 0%) (Fig. 3).
Figure 3.
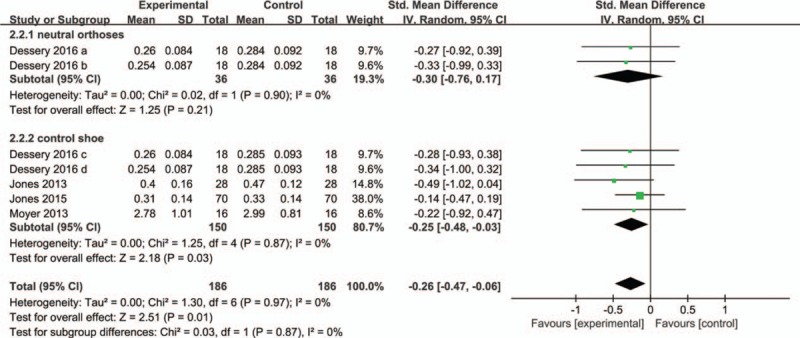
Forest plot of synthetic data for the second peak external knee adduction moment. The green squares indicate the effect size of every study. The transverse lines show the 95% CI. Black diamond represents the pooled estimate of every subgroup and the total effect. CI = confidence interval, SD = standardized errors.
Subgroup comparisons also yielded different pooled effects. Among trials in which the control treatment was a shoe-only condition, the LWAS significantly reduced the second peak EKAM (SMD, −0.25; 95% CI, −0.48 to 0.17; P = .03; I2 = 0%; n = 5). However, the LWAS showed no associations on the second peak EKAM compared to the neutral insole condition (SMD, −0.30; 95% CI, −0.76 to 0.17; P = .21; I2 = 0%; n = 2). Begg test (P = .764, see Supplemental Figure 3, which demonstrates the Begg funnel plot) and Egger test (SE = 0.56, P = 0.165, see Supplemental Figure 4, which demonstrates the Egger publication bias plot) for funnel plot asymmetry were not statistically significant, indicating weak evidence of publication bias for the second peak EKAM.
3.5. KAAI
Six studies including 9 comparisons were reported for the effect of the LWAS on the KAAI: 4 studies with a shoe-only comparison, 1 study with a neutral insole comparison, and 1 study reported both neutral insole comparison and shoe-only comparison (Table 3).
The overall pooled estimate demonstrated a significant reduction in the KAAI using LWAS (SMD −0.21; 95% CI −0.39 to −0.02; P = .03). The pooled-effect size translated to an absolute change in the KAAI of approximately −0.02 Nm/kg∗s. Low statistical heterogeneity was found (χ2 = 3.04, P = .93, I2 = 0%) (Fig. 4).
Figure 4.
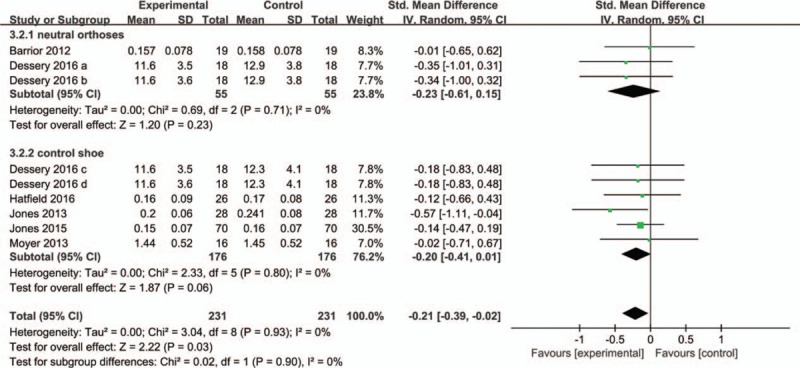
Forest plot of synthetic data for the knee adduction angular impulse. The green squares indicate the effect size of every study. The transverse lines show the 95% CI. Black diamond represents the pooled estimate of every subgroup and the total effect. CI = confidence interval, SD = standardized errors.
Subgroup comparisons also yielded different pooled effects. The LWAS showed no associations with KAAI compared to both the shoe-only condition (SMD, −0.20; 95% CI, −0.41 to 0.01; P = .06; I2 = 0%; n = 6) and the neutral insole condition (SMD −0.23; 95% CI, −0.61 to 0.15; P = .23; I2 = 0%; n = 3). Begg test (P = .602, see Supplemental Figure 5, which demonstrates the Begg funnel plot) and Egger test (SE = 0.87, P = 0.779, see Supplemental Figure 6, which demonstrates the Egger publication bias plot) for funnel plot asymmetry was not statistically significant, indicating weak evidence of publication bias for the KAAI.
4. Discussion
The LWAS played a positive role in conservative treatment for people with medial knee OA. Biomechanical parameters related with the medial compartment load of the knee joint including EKAMs and KAAI were reduced with the use of the LWAS without distinguishing between the comparators. However, it should be noted that the results were different when compared with the varied controlled conditions.
To the best of our knowledge, no previous reviews quantitatively evaluated the effect of LWAS. A systematic review evaluated the literature for the effect of different orthotics or footwear on the peak EKAMs and drew the conclusion that LWI was associated with decreased peak EKAM in participants with medial knee OA. The authors also found that there was evidence for increased peak EKAMs with the use of arch supports or medial wedges, indicating increased joint loading at the knee, although medial arch supports have an effect on reducing the amount of foot pronation caused by the LWI.[61] However, this comprehensive review did not mention the effect of the LWAS in detail. The latest meta-analysis[47] regarding this topic did not focus on the different interventions, especially the condition with the medial arch support, to which an increasing number of investigators have recently paid attention. Therefore, our study is the most definitive analysis to clarify the effects of the LWAS alone on reducing knee load in people with knee OA.
The mechanism of the effects of the LWI for the medial osteoarthritic knee was first studied by Yasuda and Sasaki[62] and proved effective for conservative treatment of knee OA; they found that a higher degree of wedging may lead to higher reductions in the first peak EKAM. However, the LWI also has its limitations. Butler et al[63] suggested that the use of lateral wedges may increase rear foot eversion, which is traditionally considered to place individuals at risk of injury and Abdallah and Radwan[37] revealed significant negative correlations between the subtalar eversion and knee adduction moments. Recently, foot orthoses with arch supports have often been prescribed by clinicians to optimize patients’ comfort[42] and medial arch support was also added to the LWI in many studies to increase comfort; its effect on reducing the amount of foot pronation has been proved.[64] Hatfield et al[46] suggested that the ankle eversion angle peak and frontal plane excursion were significantly reduced in treatment with the lateral wedge plus arch support compared to the lateral wedge alone condition. However, it should be noted that a medially applied arch support might have interfered with the effect of LWI in producing foot pronation. A recent review has found laboratory-based evidence that the medial arch may be associated with increased EKAM, indicating increased joint loading at the knee.[61] Therefore, in the clinical setting, practitioners may face a dilemma when prescribing footwear for people with medial knee OA. In view of this condition, we decided to evaluate whether LWAS was effective in reducing knee loading in patients with medial knee OA compared with an appropriate control.
Besides the shoe-only condition, we also took the neutral insole and flat insole into consideration separately, for there is no consensus as to whether flat insoles are biomechanically inert.[47,59] The reported effects of the neutral insole are not consistent in recent studies.[38,65] Although meta-analysis pooling of all studies showed statistically significant associations between the use of LWAS and reductions of the first peak EKAM, second peak EKAM and KAAI during walking for people with medial knee OA, different results were observed when comparing with various control conditions. With regard to the first peak EKAM, the use of LWAS results in a small but statistically significant reduction when the control group is the neutral insole, whereas no significant difference existed in the shoe-only or flat insole condition. The neutral insole is described as a foot orthosis made with arch support[37,42] (prefabricated or custom) or contoured foot orthoses[45] in related studies, which have reported increasing EKAM in the early or late stance phase of the gait,[42,66] that is, less pronation along with larger EKAM caused by the neutral insole. This could explain why the reduction of the first peak EKAM seemed greater in this condition. In other words, the overall effect size is not as large as that found in the neutral group when considered in the shoe-only condition. The one and only article[23] including the flat insole comparison also suggested no significant reduction. Another explanation for the minimal reduction of the shoe-only group is the larger vertical ground reaction forces caused by the higher wedge inclination. As we know, knee external adduction moment is proportional to the combination of ground reaction force and its moment arm.[9] Because medial arch support tends to displace the center of pressure medially, the extent of the reduction of the knee lever arm by LWI zooms out. Furthermore, the vertical ground reaction force increases during walking with the use of a higher lateral wedge, which has also been discussed in a related article.[42] These 2 conditions may display a correlation with the inconspicuous reduction in the first peak EKAM.
Different results also appear in the subgroup analysis of the effects on the second peak EKAM. When compared with shoe-only conditions, the reductions caused by the LWAS were small but significant. However, contrary to our assumption, the neutral insole group showed insignificant reduction on the second peak EKAM, which was unexpected. According to Jones et al,[21] during mid and terminal stance, effect of the lateral wedge can be counteracted by multiple foot structures contacting with more ground and the articulations between them. Furthermore, the ground reaction force is likely to be strongly influenced by the fact that the body mass moves toward the contralateral limb before it making ground contact.[21] If so, the LWI should mainly affect the first peak EKAM with less influence on the second peak EKAM, which is inconsistent with our result (shoe-only condition). We call this characteristic the buffer effect hereafter. Although it is difficult to find a rational explanation for this result, we can ensure that it is the arch support, which caused this eccentric discrepancy. Initially, we only considered that the medial arch support may have opposite effects on the center position of pressure with the LWI, and ignored the fact that it made the LWI more comfortable (especially the custom ones). In view of the fact that appropriate medial arch support results in less tension or pressure than the flat insole on the medial and sole of the foot,[37,66] we speculate that the appropriate height of the medial arch support could weaken the buffer effect by fitting closely between foot arch and insole when used with the LWI simultaneously. Therefore, we find the LWAS has a significant effect on the second peak EKAM, although a insignificant effect on the first peak EKAM in the shoe-only group. At the same time, in the neutral insole group, such effect of the medial arch support is neutralized. The hypothesis above needs to be further studied, emphasizing the importance of coordination between the lateral wedge and medial arch. It is worth mentioning that we have not analyzed the participants’ different responses and individual variations, which could be conspicuous as Hinman et al[38] observed. In addition, there are only 2 comparisons included in the neutral insole group for the second EKAM.
Differences also exist with regard to the KAAI, which has been proposed as a more useful measure to account for both the duration and magnitude of loading in knee OA. In both neutral insole and shoe-only conditions, the LWAS had no significant effect on KAAI. This result implied that the lateral wedge inclination is not large enough or the medial arch support is not appropriate. Few researchers have discussed how to combine these 2 parts.
As with any study, our review also has its limitations. First, our meta-analysis consists of 8 repeated measure studies and only 1 RCT. And most studies only test the instant effect of insoles. Long-term effect of LWAS needs to be studied. However, funnel plots revealed low publication bias supporting our inferences. Second, it should be mentioned that the measurement method and the walking speed of patients reported in the articles were not exactly the same and their roles in this research may need to be studied further. Third, inferring knee load with EKAM is also contentious since the contribution of muscle forces[47] and the external knee flexion moment to joint load are not considered. However, by studying outcomes related with disease progression,[14] clinical relevance was maintained in this review. Finally, only 2 articles reported the height of the arch support, which is a barrier for analyzing the combination of the LWI and the medial arch support. Although we searched the data in many ways and updated previous related reviews, only few trials were found. Because of the few comparisons included in some subgroups, the validity of our results might be threatened by the inability to extrapolate the findings to a larger population.
5. Conclusions
Considering the 9 trials together, this meta-analysis suggested a favorable effect of the LWAS insoles for reducing the biomechanical parameters (peak EKAMs and KAAI) related to knee load in patients with medial knee OA compared with a control. However, when we focused on the group of trials in which LWAS insoles were compared directly with shoe-only or flat insoles, we found no association with the first peak EKAM. We found no association with the second peak EKAM either, when comparing the LWAS with the neutral insole. No heterogeneity was found across all trial findings. These results suggest that compared with control interventions, the LWAS insoles were not more efficacious for reducing the knee load in patients with medial knee OA. An optimal LWAS should provide the appropriate arch support height and amount of lateral wedging. Further research should investigate the best combination of these 2 parameters to achieve appropriate benefit without altered comfort.
Supplementary Material
Acknowledgment
The authors acknowledge all authors who provided information about their researches.
Footnotes
Abbreviations: ACR = American College of Rheumatology, CIs = confidence intervals, EKAM = external knee adduction moment, HTO = high tibial osteotomy, KAAI = knee adduction angular impulse, LWAS = lateral wedge arch support insole, LWI = lateral wedge insole, OA = osteoarthritis, PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses, RCT = randomized controlled trial, SD = standard deviation, SMDs = standard mean differences, VAS = visual analog scale, WOMAC = Western Ontario and McMaster Universities.
F.X. and B.L. contributed equally to this study.
J-X.M. and X-L.M.are the corresponding authors who contributed equally.
This study received funding from National Natural Science Foundation of China (No. 81102607), Tianjin Health Bureau Science and Technology Foundation (No. 2014KY31) and Key Project of Tianjin Science and Technology (No. 13ZCZDSY01700).
The authors report no conflicts of interest.
Supplemental Digital Content is available for this article.
References
- [1].Badley EM. Arthritis in Canada: what do we know and what should we know? J Rheumatol 2005;72suppl:39–41. [PubMed] [Google Scholar]
- [2].Barber CE, Patel JN, Woodhouse L, et al. Development of key performance indicators to evaluate centralized intake for patients with osteoarthritis and rheumatoid arthritis. Arthritis Res Ther 2015;17:322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Guccione AA, Felson DT, Anderson JJ, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. A J Public Health 1994;84:351–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum 2008;58:26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Andriacchi TP. Dynamics of knee malalignment. Orthop Clin North Am 1994;25:395–403. [PubMed] [Google Scholar]
- [6].Ledingham J, Regan M, Jones A, et al. Radiographic patterns and associations of osteoarthritis of the knee in patients referred to hospital. Ann Rheum Dis 1993;52:520–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ahlback S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) 1968;Suppl 277:277–2. [PubMed] [Google Scholar]
- [8].Huch K, Kuettner KE, Dieppe P. Osteoarthritis in ankle and knee joints. Semin Arthritis Rheum 1997;26:667–74. [DOI] [PubMed] [Google Scholar]
- [9].Schipplein OD, Andriacchi TP. Interaction between active and passive knee stabilizers during level walking. J Orthop Res 1991;9:113–9. [DOI] [PubMed] [Google Scholar]
- [10].Kettelkamp DB, Chao EY. A method for quantitative analysis of medial and lateral compression forces at the knee during standing. Clin Orthop Rela Res 1972;83:202–13. [DOI] [PubMed] [Google Scholar]
- [11].Morrison JB. The mechanics of the knee joint in relation to normal walking. J Biomech 1970;3:51–61. [DOI] [PubMed] [Google Scholar]
- [12].Johnson F, Leitl S, Waugh W. The distribution of load across the knee. A comparison of static and dynamic measurements. J Bone Joint Surg 1980;62:346–9. [DOI] [PubMed] [Google Scholar]
- [13].Zhao D, Banks SA, Mitchell KH, et al. Correlation between the knee adduction torque and medial contact force for a variety of gait patterns. J Orthop Res 2007;25:789–97. [DOI] [PubMed] [Google Scholar]
- [14].Bennell KL, Bowles KA, Wang Y, et al. Higher dynamic medial knee load predicts greater cartilage loss over 12 months in medial knee osteoarthritis. Ann Rheum Dis 2011;70:1770–4. [DOI] [PubMed] [Google Scholar]
- [15].Chehab EF, Favre J, Erhart-Hledik JC, et al. Baseline knee adduction and flexion moments during walking are both associated with 5 year cartilage changes in patients with medial knee osteoarthritis. Osteoarthritis Cartilage 2014;22:1833–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hatfield GL, Stanish WD, Hubley-Kozey CL. Three-dimensional biomechanical gait characteristics at baseline are associated with progression to total knee arthroplasty. Arthritis Care Res 2015;67:1004–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Chang AH, Moisio KC, Chmiel JS, et al. External knee adduction and flexion moments during gait and medial tibiofemoral disease progression in knee osteoarthritis. Osteoarthritis Cartilage 2015;23:1099–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Birmingham TB, Hunt MA, Jones IC, et al. Test-retest reliability of the peak knee adduction moment during walking in patients with medial compartment knee osteoarthritis. Arthritis Rheum 2007;57:1012–7. [DOI] [PubMed] [Google Scholar]
- [19].Walter JP, D’Lima DD, Colwell CW, Jr, et al. Decreased knee adduction moment does not guarantee decreased medial contact force during gait. J Orthop Res 2010;28:1348–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Fantini Pagani CH, Hinrichs M, Bruggemann GP. Kinetic and kinematic changes with the use of valgus knee brace and lateral wedge insoles in patients with medial knee osteoarthritis. J Orthop Res 2012;30:1125–32. [DOI] [PubMed] [Google Scholar]
- [21].Jones RK, Nester CJ, Richards JD, et al. A comparison of the biomechanical effects of valgus knee braces and lateral wedged insoles in patients with knee osteoarthritis. Gait Posture 2013;37:368–72. [DOI] [PubMed] [Google Scholar]
- [22].Kumar D, Manal KT, Rudolph KS. Knee joint loading during gait in healthy controls and individuals with knee osteoarthritis. Osteoarthritis Cartilage 2013;21:298–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Fu HC, Lie CW, Ng TP, et al. Prospective study on the effects of orthotic treatment for medial knee osteoarthritis in Chinese patients: clinical outcome and gait analysis. Hong Kong Med J 2015;21:98–106. [DOI] [PubMed] [Google Scholar]
- [24].Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage 2008;16:137–62. [DOI] [PubMed] [Google Scholar]
- [25].Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res 2012;64:465–74. [DOI] [PubMed] [Google Scholar]
- [26].Osteoarthritis: National Clinical Guideline for Care and Management in Adults. London 2008. [PubMed] [Google Scholar]
- [27].Hinman RS, Bowles KA, Bennell KL. Laterally wedged insoles in knee osteoarthritis: do biomechanical effects decline after one month of wear? BMC Musculoskelet Disord 2009;10:146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Butler RJ, Marchesi S, Royer T, et al. The effect of a subject-specific amount of lateral wedge on knee mechanics in patients with medial knee osteoarthritis. J Orthop Res 2007;25:1121–7. [DOI] [PubMed] [Google Scholar]
- [29].Kakihana W, Akai M, Nakazawa K, et al. Inconsistent knee varus moment reduction caused by a lateral wedge in knee osteoarthritis. Am J Phys Med Rehabil 2007;86:446–54. [DOI] [PubMed] [Google Scholar]
- [30].Hinman RS, Payne C, Metcalf BR, et al. Lateral wedges in knee osteoarthritis: what are their immediate clinical and biomechanical effects and can these predict a three-month clinical outcome? Arthritis Rheum 2008;59:408–15. [DOI] [PubMed] [Google Scholar]
- [31].Hinman RS, Bowles KA, Payne C, et al. Effect of length on laterally-wedged insoles in knee osteoarthritis. Arthritis Rheum 2008;59:144–7. [DOI] [PubMed] [Google Scholar]
- [32].Hinman RS, Bennell KL. Advances in insoles and shoes for knee osteoarthritis. Curr Opin Rheumatol 2009;21:164–70. [DOI] [PubMed] [Google Scholar]
- [33].Kakihana W, Akai M, Nakazawa K, et al. Effects of laterally wedged insoles on knee and subtalar joint moments. Arch Phys Med Rehabil 2005;86:1465–71. [DOI] [PubMed] [Google Scholar]
- [34].Hinman RS, Bowles KA, Metcalf BB, et al. Lateral wedge insoles for medial knee osteoarthritis: effects on lower limb frontal plane biomechanics. Clin Biomech 2012;27:27–33. [DOI] [PubMed] [Google Scholar]
- [35].Bennell KL, Bowles KA, Payne C, et al. Lateral wedge insoles for medial knee osteoarthritis: 12 month randomised controlled trial. Bmj 2011;342:d2912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Kerrigan DC, Lelas JL, Goggins J, et al. Effectiveness of a lateral-wedge insole on knee varus torque in patients with knee osteoarthritis. Arch Phys Med Rehabil 2002;83:889–93. [DOI] [PubMed] [Google Scholar]
- [37].Abdallah AA, Radwan AY. Biomechanical changes accompanying unilateral and bilateral use of laterally wedged insoles with medial arch supports in patients with medial knee osteoarthritis. Clin Biomech 2011;26:783–9. [DOI] [PubMed] [Google Scholar]
- [38].Hinman RS, Bardin L, Simic M, et al. Medial arch supports do not significantly alter the knee adduction moment in people with knee osteoarthritis. Osteoarthritis Cartilage 2013;21:28–34. [DOI] [PubMed] [Google Scholar]
- [39].Jones RK, Chapman GJ, Findlow AH, et al. A new approach to prevention of knee osteoarthritis: reducing medial load in the contralateral knee. J Rheumatol 2013;40:309–15. [DOI] [PubMed] [Google Scholar]
- [40].Nakajima K, Kakihana W, Nakagawa T, et al. Addition of an arch support improves the biomechanical effect of a laterally wedged insole. Gait Posture 2009;29:208–13. [DOI] [PubMed] [Google Scholar]
- [41].Yeh HC, Chen LF, Hsu WC, et al. Immediate efficacy of laterally wedged insoles with arch support on walking in persons with bilateral medial knee osteoarthritis. Arch Phys Med Rehabil 2014;95:2420–7. [DOI] [PubMed] [Google Scholar]
- [42].Dessery Y, Belzile E, Turmel S, et al. Effects of foot orthoses with medial arch support and lateral wedge on knee adduction moment in patients with medial knee osteoarthritis. Prosthet Orthot Int 2016;ISSN: 0309-3646. DOI: 10.1177/0309364616661254. PMID: 27555447. [DOI] [PubMed] [Google Scholar]
- [43].Moyer RF, Birmingham TB, Dombroski CE, et al. Combined effects of a valgus knee brace and lateral wedge foot orthotic on the external knee adduction moment in patients with varus gonarthrosis. Arch Phys Med Rehabil 2013;94:103–12. [DOI] [PubMed] [Google Scholar]
- [44].Jones RK, Chapman GJ, Parkes MJ, et al. The effect of different types of insoles or shoe modifications on medial loading of the knee in persons with medial knee osteoarthritis: a randomised trial. J Orthopaed Res 2015;33:1646–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Barrios JA, Butler RJ, Crenshaw JR, et al. Mechanical effectiveness of lateral foot wedging in medial knee osteoarthritis after 1 year of wear. J Orthop Res 2013;31:659–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Hatfield GL, Cochrane CK, Takacs J, et al. Knee and ankle biomechanics with lateral wedges with and without a custom arch support in those with medial knee osteoarthritis and flat feet. J Orthop Res 2016;34:1597–605. [DOI] [PubMed] [Google Scholar]
- [47].Arnold JB, Wong DX, Jones RK, et al. Lateral wedge insoles for reducing biomechanical risk factors for medial knee osteoarthritis progression: a systematic review and meta-analysis. Arthritis Care Res 2016;68:936–51. [DOI] [PubMed] [Google Scholar]
- [48].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–12. [DOI] [PubMed] [Google Scholar]
- [49].Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833–40. [PubMed] [Google Scholar]
- [50].Aletaha D, Neogi T, Silman AJ, et al. 2010 Rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 2010;62:2569–81. [DOI] [PubMed] [Google Scholar]
- [51].Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis 1957;16:494–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Maly MR, Culham EG, Costigan PA. Static and dynamic biomechanics of foot orthoses in people with medial compartment knee osteoarthritis. Clin Biomech 2002;17:603–10. [DOI] [PubMed] [Google Scholar]
- [53].Bennell KL, Kean CO, Wrigley TV, et al. Effects of a modified shoe on knee load in people with and those without knee osteoarthritis. Arthritis Rheum 2013;65:701–9. [DOI] [PubMed] [Google Scholar]
- [54].Erhart JC, Mundermann A, Elspas B, et al. A variable-stiffness shoe lowers the knee adduction moment in subjects with symptoms of medial compartment knee osteoarthritis. J Biomech 2008;41:2720–5. [DOI] [PubMed] [Google Scholar]
- [55].Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 1998;52:377–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Hedges LV. Distribution theory for Glass's estimator of effect size and related estimators. J Educ Stat 1981;6:107–28. [Google Scholar]
- [57].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. Bmj 2003;327:557–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Cohen J. A power primer. Psychol Bull 1992;112:155–9. [DOI] [PubMed] [Google Scholar]
- [59].Parkes MJ, Maricar N, Lunt M, et al. Lateral wedge insoles as a conservative treatment for pain in patients with medial knee osteoarthritis: a meta-analysis. Jama 2013;310:722–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Jones RK, Chapman GJ, Forsythe L, et al. The relationship between reductions in knee loading and immediate pain response whilst wearing lateral wedged insoles in knee osteoarthritis. J Orthop Res 2014;32:1147–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Radzimski AO, Mundermann A, Sole G. Effect of footwear on the external knee adduction moment—a systematic review. Knee 2012;19:163–75. [DOI] [PubMed] [Google Scholar]
- [62].Yasuda K, Sasaki T. The mechanics of treatment of the osteoarthritic knee with a wedged insole. Clin Orthop Relat Res 1987;162–72. [PubMed] [Google Scholar]
- [63].Butler RJ, Barrios JA, Royer T, et al. Effect of laterally wedged foot orthoses on rearfoot and hip mechanics in patients with medial knee osteoarthritis. Prosthet Orthot Int 2009;33:107–16. [DOI] [PubMed] [Google Scholar]
- [64].Levinger P, Menz HB, Fotoohabadi MR, et al. Foot posture in people with medial compartment knee osteoarthritis. J Foot Ankle Res 2010;3:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Franz JR, Dicharry J, Riley PO, et al. The influence of arch supports on knee torques relevant to knee osteoarthritis. Med Sci Sports Exerc 2008;40:913–7. [DOI] [PubMed] [Google Scholar]
- [66].Tsung BY, Zhang M, Mak AF, et al. Effectiveness of insoles on plantar pressure redistribution. J Rehabil Res Dev 2004;41:767–74. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


