Abstract
Objective
To examine the association between healthcare provider communication quality and child obesity status, and the role of parent obesity and child race/ethnicity regarding this association
Methods
We conducted a cross-sectional secondary data analysis with the 2011–2013 Medical Expenditures Panel Survey of parents with children ages 6–12 (n = 5,390). We used multivariable logistic regression to examine the association of parent-reported healthcare provider communication quality (explaining well, listening carefully, showing respect, and spending enough time) with child obesity status, and effect modification by parent obesity and child race/ethnicity.
Results
Parents of obese children were more likely to report that their child’s healthcare provider listened carefully (OR=1.41, p=0.002) and spent enough time (OR=1.33, p=0.022) than parents of non-obese children. Non-obese parents of obese children experienced better communication in the domains of listening carefully (p<0.001) and spending enough time (p=0.007). Parents of obese non-Hispanic Asian children and non-Hispanic Black children were more likely to report that providers explained things well (p=0.043) and listened carefully (p=0.012), respectively.
Conclusion
Parents of obese children experienced better communication if parents were non-obese or children were non-Hispanic Black or Asian.
Practice implications
Healthcare providers should ensure effective communication with obese parents of obese children.
Keywords: parent-reported pediatric provider communication, obesity, health disparities
1. Introduction
In the last few decades, rates of childhood obesity have increased substantially. Approximately 18% of elementary school aged children (ages 6 to 11) are now obese [1], compared to 7% in 1980 [2]. Children with obesity typically have greater medical needs as they are more likely to have adverse health conditions as a result of their excess body weight [3] such as dyslipidemia and impaired glucose tolerance [4]. Healthcare providers play an important role in preventing and managing child weight gain [5] by helping parents identify and understand the risks of their child’s weight [6].
Given the key role healthcare provider play for children with obesity, high-quality communication is particularly important for parents of children who are obese. High-quality, patient-centered healthcare provider communication has been linked to weight loss in both adults [7] and children [8, 9] with obesity. Additionally, in adult patients with obesity, the quality of patient-healthcare provider communication is associated with increased patient satisfaction [10], motivation to eat better and exercise regularly [11], and consumption of fruits and vegetables [12]. However, it is possible that healthcare providers may have biases against pediatric patients with obesity and their parents that result in negative provider interactions and impaired communication quality. Prior research among adults suggests that patients’ body weight may negatively affect the relationship and communication with their own healthcare providers [13–19]. Some studies have found that obese adult patients feel that by physicians and nurses stigmatize them because of their weight [13, 14], and experience negative interactions with their primary healthcare providers [15–18].
Less is known about how a child’s weight can influence healthcare provider communication. The limited research that does exist has focused specifically on weight-related discussions [20–23]. These studies have found that parents often experience negative interactions with their child’s healthcare provider during weight counseling sessions, including a lack of sympathy and insensitive or offensive comments from healthcare providers [20, 22]. Parents of overweight (defined by body mass index > 25), or obese children (as informed by child’s healthcare provider), or who had concerns about their child’s weight report feeling that their child’s healthcare providers blamed them for their child’s weight [20, 23]. They express feeling stigmatized by healthcare providers as inadequate in understanding and unable to address their child’s weight [24]. As a result, some have avoided consulting their child’s healthcare provider on weight management because of fear of judgment from their child’s healthcare provider [23]. However, some parents note more positive experiences where healthcare providers listened, were empathetic, and provided helpful advice [20].
Absent from the literature on child weight and healthcare provider communication are studies of parent-healthcare provider communication during routine pediatric office visits. Understanding interactions during routine visits is important because negative experiences of children with obesity and their parents may result in reduced quality of care during these encounters [19] and avoidance of future routine care [25, 26].
Additionally, existing studies have not considered whether other parent or child characteristics might potentially influence and even exacerbate issues with communication quality among parents of children with obesity. Two potentially important characteristics are parent obesity status and child race/ethnicity. First, parent behaviors towards food consumption and physical activity influence their child’s weight and dietary and activity behaviors [27–29]. Healthcare providers may perceive parents to be more responsible or at fault for their child’s weight if they are themselves obese, or anticipate greater difficulty in addressing weight management among their children. As a result, pediatric healthcare providers may also have weight-related biases towards parents with obesity that affect how they communicate with parents about their child. However, no study has examined whether parent obesity influences parent-healthcare provider communication. Second, research in adults has found differences in patient-healthcare provider communication quality among adults when both patient weight and race/ethnicity are considered, where obese Non-Hispanic (NH) Black patients experience worse communication quality [30]. Similarly, parents of obese minority children may also experience poor healthcare provider communication quality. To our knowledge, only one study has examined the healthcare provider communication experiences of parents of minority children with obesity during weight management conversations. This study, conducted among Latino parents, found that pediatricians frequently use stigmatizing terms like “fat” to describe the child’s body and rarely discuss culturally relevant dietary recommendations [31].
Our primary objective was to examine the association between child obesity status with four domains of parent-healthcare provider communication quality (how frequently healthcare providers explained things well, listened carefully, showed respect, and spent enough time) reported after routine pediatric care among parents of children 6 to 12 years of age. We hypothesized that parents of children with obesity would be more likely to report worse communication quality with their child’s healthcare provider in all four domains compared to parents of children who are not obese. We had 2 secondary objectives. First, we aimed to determine whether parent obesity status modified the association between child weight and parent-healthcare provider communication quality. We hypothesized that if either parent or child were obese, parents would report worse communication quality compared to non-obese parents of non-obese children, and that obese parents of obese children would report the worst communication quality. Second, we aimed to determine whether child race/ethnicity modified the association between child weight and parent-healthcare provider communication quality. We hypothesized that parents of obese Hispanic, NH Asian, and NH Black children would report worse healthcare provider communication quality compared to parents of non-obese NH White children.
2. Methods
2.1 Data Source
For this secondary data analysis, we pooled 2011 to 2013 data from the Medical Expenditure Panel Survey’s (MEPS) Household Component to increase power in our cross-sectional analysis. MEPS, which is conducted by the Agency for Healthcare Research and Quality (AHRQ), collects data from a nationally representative sample of U.S. non-institutionalized and non-military families and individuals. Our study sample included parents with a child aged 6–12 who had at least one visit with their healthcare provider in the past 12 months. For each child, one parent, identified as the head of the household, responded to survey questions about communication quality with the child’s healthcare provider. We limited our study sample to parents of pre-adolescents, as healthcare providers direct more of their communication towards parents of younger children, while they may communicate more directly with adolescent pediatric patients [32]. We excluded parents of underweight children from our analysis due to significant heterogeneity in the underlying reason for their child’s weight status (e.g., underweight due to illness) (n=693).
2.2 Measures
Our dependent variables were four validated measures of parent-healthcare provider communication quality from the health plan version of the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey. CAHPS is a family of AHRQ-sponsored survey instruments designed to measure patient perspectives on the quality of their health care. These questions asked how frequently in the past 12 months parents thought that their child’s healthcare provider 1) explained things so that the parent understood, 2) listened carefully, 3) showed respect, and 4) spent enough time during visits. Responses were on a 4-point scale of never, sometimes, usually, and always. We dichotomized the responses to each question into always versus less than always, which is consistent with public reports of other CAHPS measures [33].
Our primary independent variable was child obesity status. Body mass index (BMI) was calculated from parent-report of child’s height and weight. We classified children as being obese if they were at or above the 95th percentile among children of the same age and sex, as defined by Center for Disease Control and Prevention [34].
Two effect modifiers, parent obesity status and child race/ethnicity, were examined. Parents were classified as being obese or not obese based on BMI calculated from their self-reported height and weight, which we classified according to standard NIH categories; parents were considered obese if their BMI was 30kg/m2 or above [35]. Parent-reported child race/ethnicity was categorized as NH White, NH Black, Hispanic, NH Asian, and NH other.
2.3 Statistical Analysis
For our primary objective, we conducted multivariate logistic regression to examine the association between child obesity status with each of the four healthcare provider communication quality domains, controlling for child and parent confounders. Our reference group for this analysis was parents of non-obese children. We controlled for the confounding effects of several child characteristics: age, sex, race/ethnicity, insurance coverage, number of visits in the past 12 months, perceived health status, whether child had a usual source of care, and geographic region. We also controlled for parent characteristics including: obesity status, sex, educational attainment, household income, and whether English was the most common language spoken at home. Parent race/ethnicity demonstrated high concordance with child race/ethnicity (percent agreement = 89%) and was excluded.
For our secondary objectives, we examined whether parent obesity and child race/ethnicity modified these associations by including interaction terms between child obesity status and parent obesity status, and child obesity status and child race/ethnicity in separate models. We did not control for adult obesity status or child race/ethnicity, respectively, in these models, as we were interested in exploring their role as effect modifiers. These models controlled for all remaining parent and child confounders listed above. We calculated the predicted probabilities of parents reporting high-quality communication for each of the 4 domains.
We accounted for the MEPS’s complex survey design by using specified survey weights to produce nationally representative estimates of the 2011–2013 U.S. non-institutionalized civilian population. All analyses were conducted in Stata/IC 14.1 (College Station, TX).
3. Results
Table 1 presents our study sample characteristics overall and stratified by child obesity status. 5,390 parents of children between the ages of 6–12 were included in the analysis. Approximately one-quarter of children were obese. The mean age for all children was 9.25 years. Non-obese children were more likely to be NH White, have excellent or very good health and have private insurance coverage compared to obese children. Obese children were more likely to be Hispanic or NH Black. Approximately one-third of all parents were obese and 63% were female. While 70% of non-obese children had non-obese parents, only 54% of obese children had non-obese parents. Parents of obese children were less educated, had a lower household income, were less likely to be born in the U.S., and were less likely to report English as the most commonly spoken language at home. A large proportion of parents reported high-quality communication with their child’s healthcare providers: “always” responses ranged from 76% for healthcare providers spending enough time to 83% for always showing respect to parents. The proportion of parents responding that they always experienced high-quality healthcare provider communication was similar for both obese and non-obese children in all 4 communication domains.
Table 1.
Sample characteristics by child obesity status
| Overall (n = 5,390) | Not obese (n = 3,736) | Obese (n = 1,654) | p-value | |
|---|---|---|---|---|
| Child Characteristics | ||||
| Age in years, mean (SD) | 9.25 (1.95) | 9.37 (1.87) | 8.92 (2.13) | < 0.001 |
| Gender, % | ||||
| Female | 49.34 | 50.27 | 46.6 | 0.109 |
| Race/ethnicity, % | ||||
| NH White | 60.62 | 64.63 | 48.7 | < 0.001 |
| NH Black | 11.8 | 10.06 | 16.97 | |
| Hispanic | 18.1 | 15.56 | 25.62 | |
| NH Asian | 4.51 | 4.6 | 4.25 | |
| NH Other | 4.97 | 5.15 | 4.46 | |
| Insurance Coverage, % | ||||
| Any private | 65.99 | 70.15 | 53.65 | < 0.001 |
| Public | 31.12 | 27.08 | 43.11 | |
| Uninsured | 2.89 | 2.78 | 3.24 | |
| Number of visits in the past 12 months, % | ||||
| 1 | 37.03 | 36.22 | 39.43 | 0.278 |
| 2 | 24.88 | 25.19 | 23.95 | |
| > 2 | 38.11 | 38.59 | 36.62 | |
| Perceived health status, % | ||||
| Excellent/very good | 81.63 | 83.5 | 76.07 | < 0.001 |
| Good/fair/poor | 18.37 | 16.50 | 23.94 | |
| Has usual source of care, % | 95.96 | 95.88 | 96.2 | 0.699 |
| Region, % | ||||
| Northeast | 19.86 | 20.09 | 19.16 | 0.500 |
| Midwest | 22.4 | 22.53 | 22.03 | |
| South | 37.9 | 37.01 | 40.55 | |
| West | 19.84 | 20.37 | 18.26 | |
| Parent Characteristics | ||||
| Obesity status, % | ||||
| Obese | 33.75 | 29.56 | 46.24 | < 0.001 |
| Parent sex, % | ||||
| Female | 62.7 | 62.0 | 62.2 | 0.893 |
| Educational attainment, % | ||||
| < HS degree | 9.34 | 7.44 | 15.02 | < 0.001 |
| HS or GED degree | 5.15 | 49.76 | 56.7 | |
| College degree or higher | 39.17 | 42.8 | 28.28 | |
| HH income, mean (SD) | 81,100 (63,500) | 84,700 (63,720) | 64,400 (56,800) | < 0.001 |
| US born, % | 80.9 | 82.3 | 76.6 | < 0.001 |
| English most common language spoken at home, % | ||||
| Yes | 87.81 | 89.58 | 82.54 | < 0.001 |
| Parent-Reported Healthcare Provider Communication Quality | ||||
| Explain Well | ||||
| Always | 80.15 | 80.21 | 79.96 | 0.876 |
| Listen Carefully | ||||
| Always | 80.36 | 79.72 | 82.28 | 0.094 |
| Shows Respect | ||||
| Always | 83.1 | 83.38 | 82.24 | 0.446 |
| Enough Time | ||||
| Always | 76.38 | 75.85 | 77.94 | 0.290 |
Notes:
Estimates calculated using survey weights.
Obese: at or above the 95th percentile among children of the same age and sex; Not obese: less than the 95th percentile among children of the same age and sex
Other race includes: Pacific Islander, American Indian, Aleut, Eskimo
Association between parent-reported healthcare provider communication and child obesity status
Table 2 presents adjusted associations between each of the 4 communication domains and child obesity status as well as parent obesity status and child race/ethnicity. After controlling for parent and child confounders, parents of obese children were significantly more likely to report that their healthcare providers always listened carefully (OR = 1.41, 95% CI: 1.14, 1.74) and spent enough time with them (OR = 1.33, 95% CI: 1.04, 1.69). We did not find associations between child obesity status with parent reports of healthcare providers explaining well or showing respect. Full results of associations between parent-reported communication quality and all covariates are available in Appendix Table A1.
Table 2.
Adjusted associations between parent-reported communication quality and child obesity status, parent obesity status, and child race/ethnicity
| Explain Well | Listen Carefully | Show Respect | Enough Time | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| OR | 95% CI | p- value | OR | 95%CI | p- value | OR | 95% CI | p- value | OR | 95% CI | p- value | |
| Child Obesity Status | ||||||||||||
| Not obese | Ref | -- | -- | Ref | -- | -- | Ref | -- | -- | Ref | -- | -- |
| Obese | 1.10 | (0.88,1. 39) | 0.395 | 1.41 | (1.14,1. 74) | 0.002 | 1.09 | (0.87,1. 35) | 0.438 | 1.33 | (1.04,1. 69) | 0.022 |
| Parent Obesity Status | ||||||||||||
| Not obese | Ref | -- | -- | Ref | -- | -- | Ref | -- | -- | Ref | -- | -- |
| Obese | 1.02 | (0.79,1. 31) | 0.888 | 0.93 | (0.74,1. 18) | 0.568 | 0.92 | (0.72,1. 17) | 0.509 | 0.97 | (0.77,1. 27) | 0.916 |
| Child race/ethnicity | ||||||||||||
| NH White | Ref | -- | -- | Ref | -- | -- | Ref | -- | -- | Ref | -- | -- |
| NH Black | 0.92 | (0.70,1. 23) | 0.582 | 1.00 | (0.76,1. 31) | 0.993 | 1.08 | (0.80,1. 47) | 0.607 | 1.00 | (0.75,1. 31) | 0.973 |
| Hispanic | 0.93 | (0.66,1. 30) | 0.651 | 0.95 | (0.72,1. 25) | 0.701 | 0.99 | (0.70,1. 40) | 0.940 | 0.87 | (0.63,1. 20) | 0.384 |
| NH Asian | 0.68 | (0.36,1. 26) | 0.215 | 0.66 | (0.39,1. 13) | 0.131 | 0.58 | (0.33,1. 03) | 0.061 | 0.65 | (0.38,1. 11) | 0.112 |
| NH Other | 0.84 | (0.51,1.37) | 0.477 | 1.13 | (0.62,2. 07) | 0.683 | 0.85 | (0.51,1. 43) | 0.551 | 0.83 | (0.47,1. 46) | 0.516 |
Notes:
Bold text indicates significance at p<0.05.
ORs calculated using multivariate logistic regression. Model controls for child variables (age, sex, race/ethnicity, insurance coverage, # of visits to the doctor in past year, health status, geographic region), parent variables (educational attainment, race/ethnicity, obesity status, house hold income, US born, and language spoken at home), and survey year. Full results for all covariates are available in Appendix Table A1
Estimates calculated using survey weights.
Child Obese: at or above 95th percentile among children of the same age and sex. Child non-obese: less than 95th percentile among children of the same age and sex.
Parent Obese: BMI ≥ 30 kg/m2. Parent non-obese: BMI < 30 kg/m2
Other race includes: Pacific Islander, American Indian, Aleut, Eskimo.
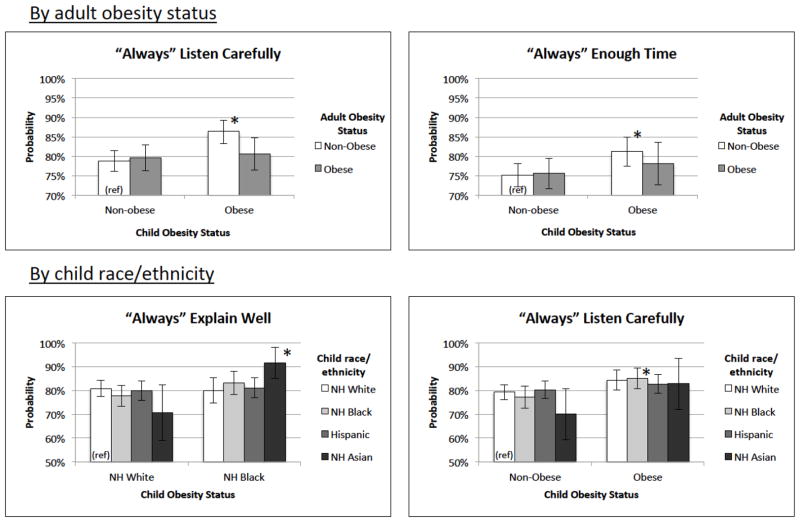
Differences by parent obesity status
Non-obese parents of obese children (86%) were more likely than non-obese parents of non-obese children (79%) to report that healthcare providers always listened to them (p < 0.001) (Figure 1). Similarly, non-obese parents of obese children (81%) were more likely than non-obese parents of non-obese children (75%) to report that healthcare providers always spent enough time with them (p = 0.007).
Figure 1.
Predicted probabilities of parent-reported healthcare provider communication quality by child obesity status and parent obesity status or child race/ethnicity
Note:
* denotes statistical significance at p < 0.05.
Figure presents models that had significant interactions with parent obesity status or child race/ethnicity. Predicted probabilities from all models are available in the Appendix Figure A1 and A2.
For interactions with adult obesity status, the non-obese child/non-obese parent category was the reference group. For interactions with child race/ethnicity, parents of non-obese NH White children was the reference group.
All models controlled for child variables (age, sex, insurance coverage, # of visits to the doctor in the past year, health status, and geographic region), parent variables (sex, educational attainment, household income, US born status, and language spoken at home), and survey year. Additionally, models by parent obesity status also controlled for child race/ethnicity, and models by child race/ethnicity also controlled for parent obesity status.
Estimates calculated using survey weights.
Differences by child race/ethnicity
Parents of NH Asian obese children were more likely to report that healthcare provider explained things well (Figure 1). In predicted probabilities from the adjusted models, 91% of parents of obese NH Asian children reported that healthcare providers always explained things compared to 81% of parents of non-obese NH White children (p = 0.043). Parents of obese NH Black children were more likely (86%) than parents of non-obese NH White children (79%) to report that healthcare providers always listened carefully (p = 0.012).
4. Discussion and Conclusion
4.1 Discussion
This study examined parent-healthcare provider communication during general pediatric care experiences. Contrary to our hypothesis, we found that, parents of obese children reported better communication quality with their child’s healthcare provider in the domains of healthcare providers listening carefully and spending enough time with them compared to parents of non-obese children. However, among parents of obese children, higher communication quality seemed to be limited to parents who were not obese. Communication quality among obese parents of obese children was similar to non-obese parents of non-obese children. Contrary to our hypothesis, we found that parents of obese minority children did not experience worse communication. In fact, parents of obese NH Black and Asian children were more likely to report that that healthcare providers listened carefully and explained things well, respectively.
To our knowledge, our study is the first to examine whether a child’s obesity status is associated with parent-healthcare provider communication quality during routine pediatric care. Our results suggest that the relationship between obesity status and healthcare provider communication quality may differ for pediatric and adults patients. Research among adults has reported that the communication and relationships of obese patients with their healthcare providers are either similar [30, 36], or worse when compared to their healthy weight counterparts [14, 15, 18, 37]. One possible explanation for this difference is that healthcare providers may be more sympathetic towards parents of obese children because they perceive a higher likelihood of successfully addressing weight issues compared to obese adult patients.
Our findings also differ from experiences documented between parents of obese children specifically within the context of pediatric weight-related discussions. Although previous studies have found that some parents experience positive and helpful interactions with their healthcare providers during these encounters, most report negative experiences [20, 22, 23]. The poor experiences during weight loss conversations might stem from healthcare providers discomfort with weight management discussions, rather than being driven by weight stigma. Previous studies have often documented healthcare providers’ limited training and confidence in delivering weight loss counseling [38, 39]. In contrast, our analysis, which focused on more general clinical interactions, suggest that these negative experiences may occur less frequently when the child’s weight is not necessarily the central focus. In fact, healthcare providers may actually be more conscious of how they communicate with parents of obese children, resulting in these parents reporting comparable or better communication quality compared to parents of non-obese children.
To our knowledge, no other study has considered whether parent obesity status modifies the association between healthcare provider communication quality and child obesity status. While among parents of obese children, non-obese parents experienced better communication, obese parents experienced similar communication as non-obese parents of non-obese children. It is possible that healthcare providers may be more sympathetic towards and willing to listen to non-obese parents of obese children, because they perceive these parents as less likely to engage in obesity-promoting behaviors, and less culpable for their child’s weight gain. It is also possible that non-obese parents of obese children are more willing to partner with their child’s healthcare provider and, in fact, may initiate clinical communication about their child’s weight and health. They may be more motivated and engaged in discussions about their child’s health because they recognize the health risks of obesity. They may also be less likely to feel stigmatized for their own weight.
Our finding that parents of obese NH Asian children were more likely to report that explain things well is surprising. Prior research has consistently found that parents of NH Asian children with limited English proficiency report worse interactions with their child’s healthcare provider, while English proficient parents of NH Asian children report similar experiences compared to parents of NH White children [40–42]. However, in multivariable regression analyses that controlled for parental socioeconomic status and whether English was spoken at home, we found that parents of obese NH Asian children reported better communication quality compared to parents of non-obese NH White children. There was no difference for parents of non-obese NH Asian children. One possible explanation for this unexpected finding is that since NH Asian children have the lowest prevalence of obesity [1], healthcare providers may be more inclined to explain things well to parents when they do encounter an obese child in this subpopulation. Given the complicated relationships among language, child obesity status, and parent-healthcare provider interactions in this subgroup, more research on parent-healthcare provider communication among NH Asians is needed.
Our finding that parents of obese NH Black children were more likely to report that healthcare providers always listened carefully compared to parents of non-obese NH White differs from a previous study among adults, which found that obese NH Black patients experience worse communication quality than non-obese NH Whites [30]. Taken together, these findings suggest that relationships among race, weight, and healthcare provider communication quality differ in pediatric and adult patient populations. While healthcare providers may have biases against NH Black overweight and obese adult patients that results in these patients experiencing worse healthcare provider communication quality, NH Black race does not seem to negatively impact healthcare provider communication in pediatric populations. We are encouraged by this finding because NH Black children are at a higher risk for childhood obesity [1], and obesity-related chronic diseases in adulthood [43]. High-quality communication with these pediatric patients can yield significant future health benefits.
Our results that parents of obese children did not report worse parent-healthcare provider communication is encouraging. Healthcare providers have a key role in addressing childhood obesity, so it is important that they communicate effectively with these patients. However, our findings highlight the need to consider parent-healthcare provider communication quality in a particularly high-risk group: obese children whose parents are also obese. High quality communication may be especially important for this group. Since parental behaviors can strongly influence child weight status [27–29], healthcare providers may need to foster stronger partnerships with these parents to address behavior changes for both child and parents. Care should be taken to ensure that healthcare providers provide high-quality communication with parents of obese children, regardless of parent weight. Additionally, there are substantial racial/ethnic disparities in childhood obesity [1]. Healthcare providers can potentially play a role in addressing these disparities through high quality communication with parents of obese children from subgroups disproportionally affected by obesity.
Gaps still exist, though, in the communication experienced by obese children and their parents. Since obese children are more likely to have suboptimal health [3], these patients can benefit from consistent high-quality of care, including effective communication in all four domains. We found that parents of obese children experience better communication in some but not all domains. Studies among parents of overweight Latino children and during sick-child visits, have noted that during weight-management sessions, parents would like healthcare providers to give specific, easy-to-follow guidance on healthy diet and family lifestyle changes and clearly explain weight-related health-issues [23, 44]. Furthermore, other gaps in quality of care for obese children remain, including a failure to diagnose obesity [45], and the need for consistent follow-up [46].
Our study had a number of limitations. Our analysis relied upon parent-reported height and weight for their child and themselves, which may underestimate both child [47] and parent BMI [48]. Our analysis was cross-sectional, making us unable to make conclusions about causality. We used report of healthcare provider communication quality from one parent, the head of the household, but it is possible that the other parent’s rating of communication quality may differ. We were also unable to control for healthcare provider characteristics that have previously been found to influence healthcare provider communication quality, such as healthcare provider weight and race/ethnicity [49–51]. We also could not determine which healthcare provider parents considered or the setting in which children received care when parents rated healthcare provider communication quality. If children saw multiple healthcare providers over the course of the year, their parents may have experienced different communication quality among healthcare providers. Our analysis only considered parent reported experiences of communication. However, previous studies in adults have found that healthcare providers and patients may differ in their expectations for quality of care, including communication [52]. Our analysis was only conducted among parents of children age 6 to 12, and our results may not be generalizable to parents of children in other age groups.
4.2 Conclusion
Our analysis of a large nationally representative dataset of the U.S. suggests that parents of obese children experience better communication quality, specifically in healthcare providers listening carefully and spending enough time with them. However, these benefits for parents of obese children were higher when parents themselves were not obese. Contrary to the adult literature, we did not find impaired healthcare provider communication among parents of obese minority children; in fact for obese NH Black and NH Asian children, parents actually reported better communication quality compared to parents of non-obese NH White children.
4.3 Practice Implications
High-quality communication between parents and their child’s healthcare provider is important for maintaining a strong relationship with parents, achieving high-quality patient care, and improving parent satisfaction. Based on our finding that overall, parents of children with obesity experience high-quality communication, healthcare providers should continue to maintain high-quality communication with parents of children with obesity. However, among parents of children with obesity, higher communication quality seemed to be limited to parents who were not obese, emphasizing the need for healthcare providers to be cognizant of potential biases towards parents with obesity and aim to communicate effectively with all parents regardless of parent obesity status. While efforts have been made to make healthcare providers aware of biases towards obese adult patients and improve communication (e.g., motivational interviewing), these same efforts with pediatric healthcare providers can improve communication quality with obese parents of obese children. These patients likely have greater medical need and require strong healthcare provider-parents collaboration to manage the child’s weight and obesity-related comorbidities.
Healthcare provider communication quality does not appear to contribute to documented disparities in obesity prevalence among Hispanic and NH Black children. Healthcare providers should continue to maintain high-quality communication with parents of minority obese children in all four communication domains. Additionally, Hispanic children have the highest risk of obesity and may require additional attention and partnership, so healthcare provider training on culturally appropriate communication may help to improve communication quality.
Future research should examine why communication quality differs by parental obesity status among parents of obese children, and the complex relationships between child race/ethnicity, weight, and parent-healthcare provider communication. Future studies can also further examine the role of parent language among parents of NH Asian obese children in their assessment of healthcare provider communication.
I confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
Highlights.
Child obesity status did not negatively impact parent-provider communication
Non-obese parents of obese children reported better provider communication
Parent-provider communication better among obese NH Black and NH Asian children
Providers should be cognizant of potential biases towards obese parents
Acknowledgments
Funding:
This work was supported by the Agency for Healthcare Research and Quality [Award Number #T32HS000029] and National Institute Of Diabetes And Digestive And Kidney Diseases of the National Institutes of Health [Award Number T32DK062707]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or Agency for Healthcare Research and Quality.
Appendix
Table A1.
Full results of adjusted associations for parents reporting high-quality healthcare provider communication by child adjusted status adjusted for all covariates
| Explain Well | Listen Carefully | Show Respect | Enough Time | |||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| OR | 95% CI | OR | 95%CI | OR | 95% CI | OR | 95% CI | |
| Child Obesity Status | ||||||||
| Not obese | Ref | -- | Ref | -- | Ref | -- | Ref | -- |
| Obese | 1.11 | (0.88,1.39) | 1.40 | (1.14,1.73) | 1.09 | (0.87,1.36) | 1.32 | (1.03,1.69) |
| Parent Obesity Status | ||||||||
| Not obese | Ref | -- | Ref | -- | Ref | -- | Ref | -- |
| Obese | 1.00 | (0.78,1.28) | 0.93 | (0.74,1.17) | 0.91 | (0.71,1.15) | 0.97 | (0.75,1.24) |
| Child race/ethnicity | ||||||||
| NH White | Ref | -- | Ref | -- | Ref | -- | Ref | -- |
| NH Black | 0.93 | (0.69,1.25) | 0.93 | (0.70,1.23) | 1.08 | (0.79,1.49) | 0.94 | (0.71,1.25) |
| Hispanic | 0.97 | (0.68,1.36) | 1.01 | (0.74,1.36) | 1.11 | (0.78,1.57) | 0.92 | (0.66,1.28) |
| NH Asian | 0.72 | (0.38,1.36) | 0.63 | (0.36,1.11) | 0.59 | (0.32,1.08) | 0.66 | (0.38,1.15) |
| NH Other | 0.84 | (0.52,1.37) | 1.12 | (0.61,2.06) | 0.87 | (0.52,1.46) | 0.82 | (0.47,1.43) |
| Child age | 0.99 | (0.94,1.04) | 1.05 | (1.00,1.11) | 1.02 | (0.97,1.07) | 1.03 | (0.99,1.07) |
| Child sex | ||||||||
| Male | Ref | -- | Ref | -- | Ref | -- | Ref | -- |
| Female | 1.08 | (0.88,1.32) | 0.86 | (0.71,1.04) | 0.96 | (0.78,1.19) | 0.97 | (0.79,1.19) |
| Child Insurance Status | ||||||||
| Any private | Ref | -- | Ref | -- | Ref | -- | Ref | -- |
| Public | 1.03 | (0.77,1.39) | 0.98 | (0.74,1.31) | 1.02 | (0.74,1.41) | 0.87 | (0.63,1.21) |
| Uninsured | 1.82 | (0.96,3.46) | 1.53 | (0.88,2.69) | 2.04 | (1.05,3.95) | 1.21 | (0.64,2.28) |
| Number of visits in the past 12 months | ||||||||
| 1 | Ref | -- | Ref | -- | Ref | -- | Ref | -- |
| 2 | 0.96 | (0.75,1.22) | 0.89 | (0.70,1.13) | 0.84 | (0.67,1.06) | 0.78 | (0.62,0.98) |
| 3 | 0.62 | (0.46,0.82) | 0.74 | (0.54,1.02) | 0.72 | (0.53,0.98) | 0.65 | (0.49,0.85) |
| 4 | 0.73 | (0.51,1.04) | 0.77 | (0.53,1.12) | 0.81 | (0.55,1.21) | 0.78 | (0.55,1.12) |
| 5 - 9 | 0.59 | (0.39,0.88) | 0.55 | (0.38,0.79) | 0.48 | (0.32,0.74) | 0.61 | (0.41,0.91) |
| 10+ | 0.39 | (0.23,0.67) | 0.41 | (0.26,0.66) | 0.34 | (0.19,0.58) | 0.39 | (0.22,0.68) |
| Perceived Health Status | ||||||||
| Excellent/very good | Ref | -- | Ref | -- | Ref | -- | Ref | -- |
| Good | 0.66 | (0.51,0.84) | 0.57 | (0.44,0.74) | 0.58 | (0.46,0.73) | 0.55 | (0.44,0.70) |
| Fair/poor | 0.55 | (0.32,0.92) | 0.51 | (0.31,0.83) | 0.48 | (0.28,0.82) | 0.59 | (0.35,1.00) |
| Has usual source of care | ||||||||
| Yes | Ref | -- | Ref | -- | Ref | -- | Ref | -- |
| No | 0.50 | (0.29,0.84) | 0.41 | (0.20,0.84) | 0.47 | (0.27,0.83) | 0.54 | (0.26,1.14) |
| Region | ||||||||
| Northeast | Ref | -- | Ref | -- | Ref | -- | Ref | -- |
| Midwest | 1.14 | (0.78,1.66) | 0.98 | (0.69,1.39) | 1.11 | (0.75,1.65) | 1.17 | (0.80,1.71) |
| South | 1.10 | (0.73,1.68) | 1.27 | (0.86,1.88) | 0.98 | (0.66,1.46) | 1.35 | (0.91,1.99) |
| West | 0.92 | (0.66,1.30) | 0.93 | (0.66,1.31) | 0.78 | (0.56,1.09) | 0.93 | (0.66,1.31) |
| Parent Educational Attainment | ||||||||
| < HS degree | Ref | -- | Ref | -- | Ref | -- | Ref | -- |
| HS or GED degree | 1.01 | (0.73,1.39) | 0.95 | (0.73,1.24) | 0.89 | (0.66,1.21) | 1.13 | (0.86,1.50) |
| College degree or higher | 1.02 | (0.63,1.64) | 0.94 | (0.61,1.45) | 0.97 | (0.59,1.58) | 1.07 | (0.70,1.65) |
| HH income, mean (SD) | 1.02 | (1.00, 1.05) | 1.02 | (0.99, 1.05) | 1.05 | (1.02, 1.08) | 1.01 | (0.99, 1.04) |
| Parent US Birth status | ||||||||
| Born in US | Ref | -- | Ref | -- | Ref | -- | Ref | -- |
| Born outside of US | 0.70 | (0.39,1.26) | 0.65 | (0.40,1.07) | 0.73 | (0.43,1.22) | 0.76 | (0.48,1.18) |
| Parent report of language most commonly spoken at home | ||||||||
| English | Ref | -- | Ref | -- | Ref | -- | Ref | -- |
| Spanish | 0.85 | (0.54,1.35) | 0.82 | (0.54,1.25) | 0.88 | (0.56,1.41) | 0.89 | (0.58,1.36) |
| Other | 0.80 | (0.40,1.58) | 1.10 | (0.58,2.12) | 1.05 | (0.52,2.12) | 0.96 | (0.54,1.71) |
| Year | ||||||||
| 2011 | Ref | -- | Ref | -- | Ref | -- | Ref | -- |
| 2012 | 1.12 | (0.86, 1.47) | 1.25 | (0.96, 1.64) | 1.2 | (0.91, 1.58) | 1.38 | (1.09, 1.74) |
| 2013 | 1.36 | (1.02, 1.82) | 1.45 | (1.11, 2.12) | 1.55 | (1.12, 2.15) | 1.54 | (1.18, 2.02) |
Notes:
Bold text indicates significance at p<0.05.
ORs calculated using multivariate logistic regression. Model controls for child variables (age, sex, race/ethnicity, insurance coverage, # of visits to the doctor in past year, health status, geographic region), parent variables (educational attainment, race/ethnicity, obesity status, house hold income, US born, and language spoken at home), and survey year. Estimates calculated using survey weights.
Child Obese: at or above 95th percentile among children of the same age and sex. Child non-obese: less than 95th percentile among children of the same age and sex.
Parent Obese: BMI ≥ 30 kg/m2. Parent non-obese: BMI < 30 kg/m2
Other race includes: Pacific Islander, American Indian, Aleut, Eskimo.
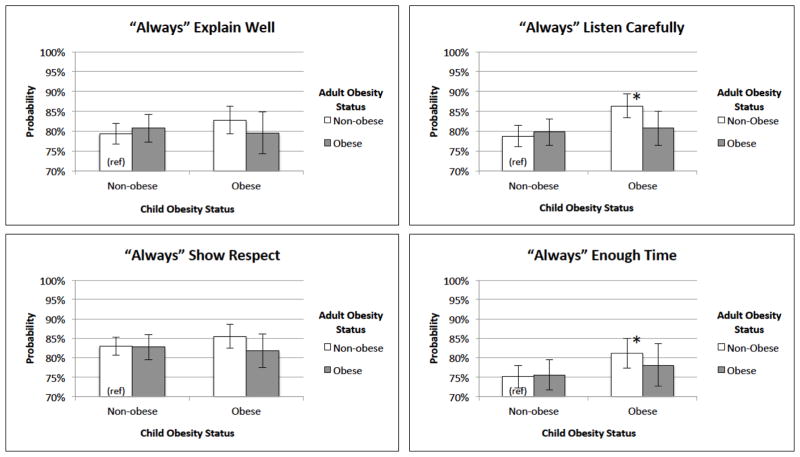
Figure A1.
Predicted probabilities of parent-reported healthcare provider communication in all 4 domains by child and parent obesity status
Note: Non-obese child/non-obese parent category was the reference group for all models.
* denotes statistical significance at p < 0.05.
Models controlled for child variables (age, sex, race/ethnicity, insurance coverage, # of visits to the doctor in the past year, health status, and geographic region), parent variables (educational attainment, household income, US born status, and language spoken at home), and survey year.
Estimates calculated using survey weights.
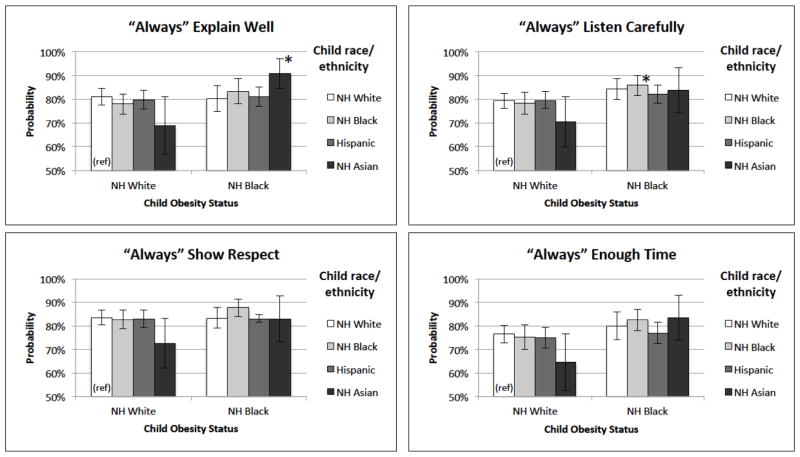
Figure A2.
Predicted probabilities of parent-reported healthcare provider communication quality in all 4 domains by child weight and race/ethnicity
Note: Non-obese NH White child category was the reference group for all models.
* denotes statistical significance p < 0.05.
Results from NH Other race/ethnicity group not shown due to significant heterogeneity in this group.
Models controlled for child variables (age, sex, insurance coverage, # of visits to the doctor in the past year, health status, and geographic region), parent variables (obesity status, educational attainment, household income, US born status, and language spoken at home), and survey year.
Estimates calculated using survey weights.
Footnotes
Conflict of Interest
Authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the united states, 2011–2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. [accessed September 16, 2016];Childhood Obesity Facts. 2015 < https://http://www.cdc.gov/healthyschools/obesity/facts.htm%3E.
- 3.Turer CB, Lin H, Flores G. Health status, emotional/behavioral problems, health care use, and expenditures in overweight/obese US children/adolescents. Acad Pediatr. 2013;13:251–8. doi: 10.1016/j.acap.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 4.Yanovski JA. Pediatric obesity. An introduction. Appetite. 2015;93:3–12. doi: 10.1016/j.appet.2015.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown CL, Halvorson EE, Cohen GM, Lazorick S, Skelton JA. Addressing Childhood Obesity: Opportunities for Prevention. Pediatr Clin North Am. 2015;62:1241–1261. doi: 10.1016/j.pcl.2015.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hernandez RG, Cheng TL, Serwint JR. Parents healthy weight perceptions and preferences regarding obesity counseling in preschoolers: Pediatricians matter. Clin Pediatr (Phila) 2010;49:790–798. doi: 10.1177/0009922810368288. [DOI] [PubMed] [Google Scholar]
- 7.Pollak KI, Alexander SC, Coffman CJ, Tulsky JA, Lyna P, Dolor RJ, James IE, Brouwer RJN, Manusov JRE, Østbye T. Physician Communication Techniques and Weight Loss in Adults: Project CHAT. Am J Prev Med. 2010;39:321–328. doi: 10.1016/j.amepre.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schwartz RP, Hamre R, Dietz WH, et al. Office-based motivational interviewing to prevent childhood obesity: A feasibility study. Arch Pediatr Adolesc Med. 2007;161:495–501. doi: 10.1001/archpedi.161.5.495. [DOI] [PubMed] [Google Scholar]
- 9.Resnicow K, Taylor R, Baskin M, McCarty F. Results of go girls: A weight control program for overweight African-American adolescent females. Obes Res. 2005;13:1739–1748. doi: 10.1038/oby.2005.212. [DOI] [PubMed] [Google Scholar]
- 10.Pollak KI, Nagy P, Bigger J, Bilheimer A, Lyna P, Gao X, Lancaster M, Watkins RC, Johnson F, Batish S, Skelton JA, Armstrong S. Effect of teaching motivational interviewing via communication coaching on clinician and patient satisfaction in primary care and pediatric obesity-focused offices. Patient Educ Couns. 2016;99:300–303. doi: 10.1016/j.pec.2015.08.013. [DOI] [PubMed] [Google Scholar]
- 11.Jay M, Gillespie C, Schlair S, Sherman S, Kalet A. Physician’s use of the 5As in counseling obese patients: is the quality of counseling associated with patients’ motivation and intention to lose weight? BMC Health Serv Res. 2010;10 doi: 10.1186/1472-6963-10-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baumann M, Tchicaya A, Lorentz N, Le Bihan E. Impact of Patients’ Communication with the Medical Practitioners, on Their Adherence Declared to Preventive Behaviours, Five Years after a Coronary Angiography, in Luxembourg. PLoS One. 2016;11:e0157321. doi: 10.1371/journal.pone.0157321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9:788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 14.Puhl RM, Brownell KD. Confronting and coping with weight stigma: an investigation of overweight and obese adults. Obesity (Silver Spring) 2006;14:1802–15. doi: 10.1038/oby.2006.208. [DOI] [PubMed] [Google Scholar]
- 15.Gudzune KA, Beach MC, Roter DL, Cooper LA. Physicians build less rapport with obese patients. Obesity. 2013;21:2146–2152. doi: 10.1002/oby.20384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gudzune KA, Bennett WL, Cooper LA, Bleich SN. Patients who feel judged about their weight have lower trust in their primary care providers. Patient Educ Couns. 2014;97:128–131. doi: 10.1016/j.pec.2014.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hebl M, Xu J, Mason M. Weighing the care: patients’ perceptions of physician care as a function of gender and weight. Int J Obes. 2003;27:269–275. doi: 10.1038/sj.ijo.802231. [DOI] [PubMed] [Google Scholar]
- 18.Richard P, Ferguson C, Lara AS, Leonard J, Younis M. Disparities in physician-patient communication by obesity status. Inquiry. 2014 doi: 10.1177/0046958014557012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev. 2015;16:319–326. doi: 10.1111/obr.12266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Edmunds L. Parents’ perceptions of health professionals’ responses when seeking help for their overweight children. Fam Pract. 2005;22:287–292. doi: 10.1093/fampra/cmh729. [DOI] [PubMed] [Google Scholar]
- 21.Sealy YM, Zarcadoolas C, Dresser M, Wedemeyer L, Short L, Silver L. Using public health detailing and a family-centered ecological approach to promote patient-provider-parent action for reducing childhood obesity. Childhood Obesity. 2012;8:132–146. doi: 10.1089/chi.2011.0025. [DOI] [PubMed] [Google Scholar]
- 22.Toftemo I, Glavin K, Lagerløv P. Parents’ views and experiences when their preschool child is identified as overweight: a qualitative study in primary care. Fam Pract. 2013;30:719–723. doi: 10.1093/fampra/cmt056. [DOI] [PubMed] [Google Scholar]
- 23.Turner KM, Salisbury C, Shield JPH. Parents’ views and experiences of childhood obesity management in primary care: A qualitative study. Fam Pract. 2012;29:476–481. doi: 10.1093/fampra/cmr111. [DOI] [PubMed] [Google Scholar]
- 24.Hamlington B, Ivey LE, Brenna E, Biesecker LG, Biesecker BB, Sapp JC. Characterization of courtesy stigma perceived by parents of overweight children with bardet-biedl syndrome. PLoS One. 2015:10. doi: 10.1371/journal.pone.0140705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amy NK, Aalborg A, Lyons P, Keranen L. Barriers to routine gynecological cancer screening for White and African-American obese women. Int J Obes Relat Metab Disord. 2005;30:147–155. doi: 10.1038/sj.ijo.0803105. [DOI] [PubMed] [Google Scholar]
- 26.Alegria Drury CA, Louis M. Exploring the Association Between Body Weight, Stigma of Obesity, and Health Care Avoidance. J Am Acad Nurse Pract. 2002;14:554–561. doi: 10.1111/j.1745-7599.2002.tb00089.x. [DOI] [PubMed] [Google Scholar]
- 27.Fogelholm M, Nuutinen O, Pasanen M, Myohanen E, Saatela T. Parent-child relationship of physical activity patterns and obesity. Int J Obes Relat Metab Disord. 1999;23:1262–8. doi: 10.1038/sj.ijo.0801061. [DOI] [PubMed] [Google Scholar]
- 28.Patrick H, Nicklas TA. A review of family and social determinants of children’s eating patterns and diet quality. J Am Coll Nutr. 2005;24:83–92. doi: 10.1080/07315724.2005.10719448. [DOI] [PubMed] [Google Scholar]
- 29.Fogelholm M, Nuutinen O, Pasanen M, Myöhänen E, Säätelä T. Parent-child relationship of physical activity patterns and obesity. Int J Obes. 1999;23:1262–1268. doi: 10.1038/sj.ijo.0801061. [DOI] [PubMed] [Google Scholar]
- 30.Wong M, Gudzune KA, Bleich SN. Provider communication quality: Influence of patients’ weight and race. Patient Educ Couns. 2015 doi: 10.1016/j.pec.2014.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Turer CB, Montaño S, Lin H, Hoang K, Flores G. Pediatricians’ Communication About Weight With Overweight Latino Children and Their Parents. Pediatrics. 2014;134:892–899. doi: 10.1542/peds.2014-1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Dulmen AM. Children’s contributions to pediatric outpatient encounters. Pediatrics. 1998;102:563. doi: 10.1542/peds.102.3.563. [DOI] [PubMed] [Google Scholar]
- 33.Agency for Healthcare Research and Quality. [accessed 19 August 2016];Comparative Data. 2016 < http://www.ahrq.gov/cahps/cahps-database/comparative-data/index.html%3E.
- 34.Center for Disease Control and Prevention (CDC) [accessed 2016 July 31];Defining Childhood Obesity. 2015 < http://www.cdc.gov/obesity/childhood/defining.html%3E.
- 35.L. National Institutes of Health National Heart, and Blood Institute. [accessed 2016 July 31];How are overweight and obesity diagnosed? 2012 < http://www.nhlbi.nih.gov/health/health-topics/topics/obe/diagnosis%3E.
- 36.Gudzune KA, Huizinga MM, Cooper LA. Impact of patient obesity on the patient provider relationship. Patient Educ Couns. 2011;85:e322–e325. doi: 10.1016/j.pec.2011.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huizinga MM, Cooper LA, Bleich SN, Clark JM, Beach MC. Physician respect for patients with obesity. J Gen Intern Med. 2009;24:1236–1239. doi: 10.1007/s11606-009-1104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Story MT, Neumark-Stzainer DR, Sherwood NE, Holt K, Sofka D, Trowbridge FL, Barlow SE. Management of child and adolescent obesity: attitudes, barriers, skills, and training needs among health care professionals. Pediatrics. 2002;110:210–4. [PubMed] [Google Scholar]
- 39.Nelson JM, Vos MB, Walsh SM, O’Brien LA, Welsh JA. Weight management-related assessment and counseling by primary care providers in an area of high childhood obesity prevalence: current practices and areas of opportunity. Child Obes. 2015;11:194–201. doi: 10.1089/chi.2014.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weech-Maldonado R, Morales LS, Spritzer K, Elliott M, Hays RD. Racial and ethnic differences in parents’ assessments of pediatric care in Medicaid managed care. Health Serv Res. 2001;36:575. [PMC free article] [PubMed] [Google Scholar]
- 41.Clemans-Cope L, Kenney G. Low income parents’ reports of communication problems with health care providers: effects of language and insurance. Public Health Rep. 2007;122:206–16. doi: 10.1177/003335490712200210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Seid M, Stevens GD, Varni JW. Parents’ perceptions of pediatric primary care quality: effects of race/ethnicity, language, and access. Health Serv Res. 2003;38:1009–31. doi: 10.1111/1475-6773.00160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liao Y, Bang D, Cosgrove S, Dulin R, Harris Z, Taylor A, White S, Yatabe G, Liburd L, Giles W. Surveillance of health status in minority communities-Racial and Ethnic Approaches to Community Health Across the US (REACH US) Risk Factor Survey, United States, 2009, MMWR. Surveillance summaries: Morbidity and mortality weekly report. Surveillance summaries/CDC. 2011;60:1–44. [PubMed] [Google Scholar]
- 44.Lupi JL, Haddad MB, Gazmararian JA, Rask KJ. Parental Perceptions of Family and Pediatrician Roles in Childhood Weight Management. The Journal of Pediatrics. 2014;165:99–103.e2. doi: 10.1016/j.jpeds.2014.02.064. [DOI] [PubMed] [Google Scholar]
- 45.O’Brien SH, Holubkov R, Reis EC. Identification, evaluation, and management of obesity in an academic primary care center. Pediatrics. 2004;114:e154–9. doi: 10.1542/peds.114.2.e154. [DOI] [PubMed] [Google Scholar]
- 46.Turer CB, Mehta M, Durante R, Wazni F, Flores G. Parental perspectives regarding primary-care weight-management strategies for school-age children. Maternal & Child Nutrition. 2016;12:326–338. doi: 10.1111/mcn.12131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lundahl A, Kidwell KM, Nelson TD. Parental underestimates of child weight: A meta-analysis. Pediatrics. 2014;133:e689–e703. doi: 10.1542/peds.2013-2690. [DOI] [PubMed] [Google Scholar]
- 48.Taylor AW, Dal Grande E, Gill TK, Chittleborough CR, Wilson DH, Adams RJ, Grant JF, Phillips P, Appleton S, Ruffin RE. How valid are self-reported height and weight? A comparison between CATI self-report and clinic measurements using a large cohort study. Aust N Z J Public Health. 2006;30:238–246. doi: 10.1111/j.1467-842x.2006.tb00864.x. [DOI] [PubMed] [Google Scholar]
- 49.Bleich SN, Gudzune KA, Bennett WL, Jarlenski MP, Cooper LA. How does physician BMI impact patient trust and perceived stigma? Preventive Medicine. 2013;57:120–124. doi: 10.1016/j.ypmed.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-Centered Communication, Ratings of Care, and Concordance of Patient and Physician Race. Annals of Internal Medicine. 2003;139:907–915+I34. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- 51.Brown TN, Ueno K, Smith CL, Austin NS, Bickman L. Communication patterns in medical encounters for the treatment of child psychosocial problems: does pediatrician-parent concordance matter? Health Commun. 2007;21:247–56. doi: 10.1080/10410230701307717. [DOI] [PubMed] [Google Scholar]
- 52.Levine R, Shore K, Lubalin J, Garfinkel S, Hurtado M, Carman K. Comparing physician and patient perceptions of quality in ambulatory care. Int J Qual Health Care. 2012;24:348–56. doi: 10.1093/intqhc/mzs023. [DOI] [PubMed] [Google Scholar]