Abstract
Background
Trauma systems improve outcome; however, it is unclear how geographic organization of trauma system resources (TSR) affects outcome. Our objective was to evaluate the relationship of fatal motor vehicle collisions (MVC) rates and the distance from individual MVC locations to the nearest TSR as a measure of the geographical organization of trauma systems, as well as how theoretical changes in the distribution of TSR may affect fatal MVC rates.
Methods
All fatal MVC in Pennsylvania 2013–14 were mapped from the FARS database. Deaths on scene were excluded. TSR including trauma centers and helicopter bases were mapped. Distance between each fatal MVC and nearest TSR was calculated. The primary outcome was fatal MVC rate per 100million vehicle miles traveled (VMT). Empiric Bayes Kriging and hotspot analysis were performed to evaluate geographic patterns in fatal MVC rates. Association between fatal MVC rate and distance to the nearest TSR was evaluated with linear regression. Spatial lag regression evaluated this association while controlling for MVC and county-level characteristics.
Results
We identified 886 fatalities from 863 fatal MVC. Median fatal MVC rate was 0.187 per 100million VMT. Higher fatal MVC rates and fatality hotspots occur in locations farther from TSR. The fatal MVC rate increased 0.141 per 100million VMT for every 10 miles farther from the nearest TSR (p<0.01). When controlling for confounders, the fatal MVC rate increased by 0.089 per 100million VMT for every 10 miles farther from the nearest TSR (p<0.01). If 2 helicopters stationed at trauma centers were relocated into the highest fatality regions, our model predicts a 12.3% relative reduction in the overall MVC fatality rate.
Conclusions
Increasing distance to the nearest TSR is associated with increasing fatal MVC rate. The geographic organization of trauma systems may impact outcome, and geospatial analysis can allow data-driven changes to potentially improve outcome.
Keywords: Geographic information systems, helicopter, trauma center, outcomes, motor vehicle collision
BACKGROUND
Regionalization of trauma care and development of trauma systems have significantly improved mortality and morbidity following injury in the United States (US).1–3 Timely access to trauma care is a critical component; however, access and outcomes among US trauma systems are not geographically uniform.4–9 Further, there is significant variation in the geographic organization of trauma systems which may play a role in outcomes.10
Our group has previously shown that the geographic distribution of trauma centers at the state-level is correlated with injury fatality rates.11 Motor vehicle collisions (MVC) have been shown to be particularly influenced by geographical factors, as several have shown that mortality from MVC is influenced by geographic region, population density, and vehicle miles traveled.12–15 Further, MVC events are dispersed throughout a trauma system and have a wide range of injury severity that mobilizes the full range of prehospital and trauma center resources.16
Some have also demonstrated that geospatial analysis can aid trauma system design and enhance resource allocation.17, 18 Thus, it remains unclear what relationship exists between the geographic organization of trauma system resources (TSR), outcomes after injury such as MVC, and the potential to influence outcomes through optimal distribution of TSR.
To explore this, our objective was to evaluate the relationship of fatal MVC rates and the distance from individual MVC locations to the nearest TSR as a measure of the geographical organization of trauma systems. We further sought to evaluate how theoretical changes in the distribution of TSR may affect fatal MVC rates. We hypothesized that increasing distance between MVC location and the nearest TSR would be associated with higher fatal MVC rates, and redistribution of TSR would have the potential to reduce fatal MVC rates.
METHODS
Data Sources
All fatal MVC in Pennsylvania from 2013 to 2014 reported to the National Highway Traffic Safety Administration (NHTSA) Fatality Analysis Reporting System (FARS) database were collected. The FARS database contains detailed information on accident, vehicle, and occupant characteristics for any MVC that results in the death of a person within 30 days of the event.19 Collisions in which all occupants were killed at the scene were excluded, as these represent non-survivable events in which the geospatial organization of trauma system resources would not influence outcome.
Pennsylvania county characteristics including population density, educational attainment, unemployment rate, poverty rate, and median household income were obtained from the US census bureau. The daily vehicle miles traveled (VMT) and number of MVC with any injury for each county were obtained from the Pennsylvania Department of Transportation. County level characteristics were obtained for 2013 and 2014 and averaged over the two-year study period. Level I and II trauma center locations in Pennsylvania during 2014 were obtained from the American Trauma Society Trauma Information Exchange Program. The 2015 Atlas and Database of Air Medical Services was used to determine the location of helicopter emergency medical services (HEMS) bases within Pennsylvania during 2014.
Geospatial Analysis
The location of each fatal MVC was geocoded and mapped based on latitude and longitude coordinates provided in the FARS database to obtain an incident-level map of fatal MVC events. Trauma system resources for purposes of this study were defined as trauma centers and HEMS bases. Trauma center and HEMS base locations were geocoded and mapped based on street addresses. The straight-line Euclidean distance in miles between each fatal MVC and the nearest TSR was calculated. Distance was also calculated to the nearest trauma center and nearest HEMS base separately for each fatal MVC.
Empiric Bayes kriging was used to generate a map of MVC fatality rates across Pennsylvania using individual MVC events as the unit of analysis. Kriging is a geospatial interpolation technique that fits a mathematical function to a specified number of points to determine the outcome values at all locations between the points.20 This technique assumes the distance between known outcome values at sample points reflects spatial correlation related to the variation in outcome values in space. Ordinary kriging techniques involve selection an empiric model of spatial autocorrelation for prediction, requiring some knowledge of the underlying spatial relationship and manual adjustment of model parameters for accurate results. Empiric Bayes kriging can estimate the underlying spatially dependent relationship empirically using sub-setting and simulations of the known outcome values. This allows kriging techniques to be used when the underlying relationship is not well known, and better accounts for the variance in the spatial relationship rather than assume a single empiric underlying spatial relationship.21 This technique ultimately allowed creation of a continuous surface of MVC fatality rates by interpolating the geospatial pattern of fatalities based on individual fatal MVC locations in Pennsylvania.
Additionally, a hotspot analysis was performed, again with individual MVC as the unit of analysis. Hot spot analysis identifies areas of spatially clustered high and low outcome values. This technique calculated the Getis-Ord Gi* statistic for each fatal MVC in the dataset. The Gi* statistic is a z-score that evaluates the outcome values for each feature within the context of the outcome values of neighboring features.22 The outcome values in a local area must be significantly higher (hot spot) or lower (cold spot) than would be expected if the outcome was randomly distributed in space. Based on the Gi* statistic, p-values are calculated, with hot and cold spots identified at the 99%, 95%, and 90% confidence levels. This technique allows identification of spatially clustered areas of high or low MVC fatality rates. All geospatial MVC fatality outcomes were normalized as a fatality rate per 100 million VMT to give an exposure-based rate that accounts for traffic volume and the related risk of being exposed to an MVC across the state. Geospatial analysis was performed using ArcGIS v10.2 (ESRI; Redlands, CA).
Statistical Analysis
The primary outcome was the exposure-based fatal MVC rate, defined as the proportion of fatal MVC among all MVC with injury per 100 million VMT. This outcome was aggregated at the county-level using all injury related crashes and VMT by county. The mean distance of all fatal MVC events within the county also calculated to allow the county to serve as the unit of analysis.
Linear regression was used to determine the association between the fatal MVC rate per 100 million VMT and the mean distance to the nearest TSR at the county-level. This model was repeated for trauma centers and HEMS bases separately. Linear models were weighted for the total number of MVC occurring in each county. Spatial-lag regression was also performed to evaluate this relationship while adjusting for MVC event and county characteristics. This included the proportion of fatal MVC occurring in adverse weather, rural locations, at night-time, in which speeding was a contributing factor, alcohol was involved, at least one occupant was unrestrained, at least one occupant was ejected, extrication from the vehicle was required, the mean age of fatalities, the mean estimated travel speed, the mean emergency medical services notification, response, scene, and transport times, as well as the county median household income, population density, proportion living in poverty, unemployment rate, and proportion achieving a bachelor’s degree. Spatial-lag regression accounts for the dependence between an outcome value at any given geographic location and the outcome value at neighboring geographic locations.23
To evaluate the potential impact of redistributing TSR, two scenarios were considered. First, a sample of helicopter bases located at existing trauma centers were theoretically moved within the geospatial analysis to alternate locations within the highest MVC fatality areas based on the empiric Bayes kriging results. This evaluates an increase in the geographic coverage of TSR, as the helicopters are moved into new regions while the trauma centers remain at the same location. Non-trauma center hospitals near the center of high fatality regions were selected as new potential bases and the distance to the nearest TSR was recalculated for the entire dataset using the alternate base sites. The predicted fatal MVC rate per 100 million VMT for each county from the model above were obtained. The model was then repeated using the alternate HEMS base locations and the predicted fatal MVC rates per 100 million VMT again calculated. The predicted fatal MVC rates from both models were averaged and the relative reduction in fatal MVC rates calculated under the alternate HEMS base locations. For the second scenario, this process was repeated after moving independent HEMS bases into the high fatality regions. Thus, no TSR remained at the prior HEMS base location and this scenario evaluates a true redistribution of TSR where resources move out of one location for another.
Data analysis was conducted using Stata v13 (StataCorp; College Station, TX). Continuous data are presented as median (interquartile range [IQR]) or mean. Continuous data were compared using Wilcoxon rank-sum tests, and categorical data compared using Chi-square. Spatial lag regression was conducted using GeoDa v1.6 (Arizona State University; Tempe, AZ). A two-tailed p value ≤0.05 was considered significant.
RESULTS
In 2013 and 2014 there were 863 fatal MVC events with 886 fatalities in Pennsylvania. The median fatal MVC rate across Pennsylvania was 0.187 per 100 million VMT (IQR 0.049, 0.348 per 100 million VMT). Table 1 describes the fatal MVC characteristics across the state. Figure 1 depicts the locations of each fatal MVC, as well as the distribution of fatal MVC rates across the state. The lowest fatal MVC rates occur in Allegheny (located in southwestern Pennsylvania) and Philadelphia (located in southeastern Pennsylvania) counties with the highest density of TSR. Areas of higher fatal MVC rates occur in the central, north-central, and north-eastern parts of the state, where there are geographic gaps in TSR availability.
Table 1.
Characteristics of fatal motor vehicle collisions in Pennsylvania 2013–2014
| Total fatalities | 886 |
| Age of fatalities, years, median (IQR) | 51 (28, 70) |
| Adverse weather, n (%) | 129 (14.8) |
| Rural location, n (%) | 425 (48.0) |
| Night time, n (%) | 365 (41.2) |
| Speeding a factor, n (%) | 352 (39.7) |
| Alcohol a factor, n (%) | 196 (22.1) |
| Unrestrained or unhelmeted, n (%) | 403 (45.5) |
| Ejected, n (%) | 116 (13.1) |
| Extrication required, n (%) | 344 (39.0) |
| Travel speed, mph, median (IQR) | 45 (35, 55) |
| EMS notification time, mins, median (IQR) | 2 (1, 5) |
| EMS response time, mins, median (IQR) | 7 (5, 11) |
| EMS scene and transport time, mins, median (IQR) | 30 (21, 44) |
IQR, interquartile range; EMS, emergency medical services; mph, miles per hour
Figure 1.
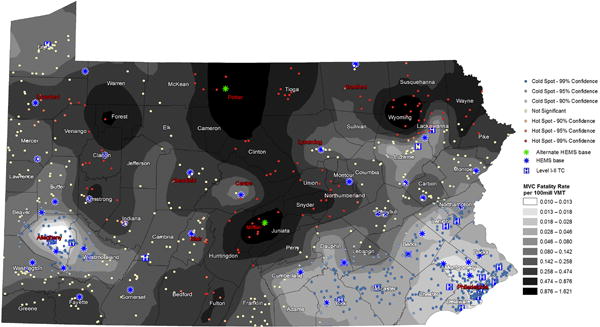
Fatal motor vehicle collisions (MVC) in Pennsylvania 2013 to 2014. Gray scale color ramp represents fatal MVC rate per 100 million vehicle miles traveled from empiric Bayes kriging interpolation. Individual MVC event locations are represented by color dot corresponding to hotspot analysis. Red represents hot spots with spatially clustered high fatal MVC rates per 100 million VMT at the indicated confidence level. Blue represents cold spots with spatially clustered low fatal MVC rates per 100 million VMT at the indicated confidence level. Level I/II trauma center locations are represented by the blue hospital symbols. Helicopter emergency medical services (HEMS) base locations are represented by the blue stars. Proposed alternate HEMS base locations for evaluation of the potential impact of trauma system resource redistribution are represented by the green stars. Counties are labeled, red county names indicate counties referred to in the Results section.
Hotspot analysis demonstrates clustering of high fatal MVC rates in the central and north-east portion of the state, farthest from TSR (Fig. 1.) Cold spots cluster in areas with proximity to TSR locations. Further, some MVC events near TSR locations in areas of moderate to high overall fatal MVC rates are not significant hot spots, such as seen in northern Bradford county (located in northeastern Pennsylvania), western Crawford county (located in northwestern Pennsylvania), and central Clearfield county (located in central Pennsylvania) (Fig. 1). This suggests proximity to TSR even in areas of higher fatality rates may be protective against clustering of fatal MVC events.
Linear regression demonstrated the fatal MVC rate increased 0.141 per 100 million VMT for every 10 miles farther from the nearest TSR (95%CI 0.140—0.143, p<0.001, Fig. 2). Similarly, the fatal MVC rate increased 0.072 per 100 million VMT for every 10 miles farther from the nearest trauma center (95%CI 0.071—0.073, p<0.001, Fig. 3) and 0.094 per 100 million VMT for every 10 miles farther from the nearest HEMS base (95%CI 0.093—0.095, p<0.001, Fig. 4).
Figure 2.
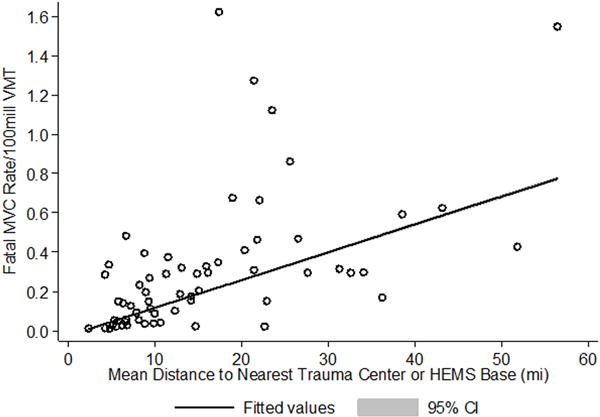
Plot of fatal MVC rate per 100 million vehicle miles traveled by mean distance to the nearest trauma system resource. Each open circle represents a Pennsylvania county. Distance in miles represents mean of all fatal MVC events occurring within the county. Line represents fitted linear regression values with 95% confidence interval.
Figure 3.
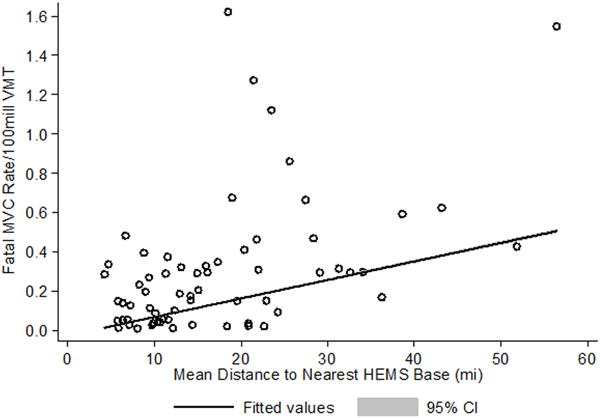
Plot of fatal MVC rate per 100 million vehicle miles traveled by mean distance to the nearest trauma center. Each open circle represents a Pennsylvania county. Distance in miles represents mean of all fatal MVC events occurring within the county. Line represents fitted linear regression values with 95% confidence interval.
Figure 4.
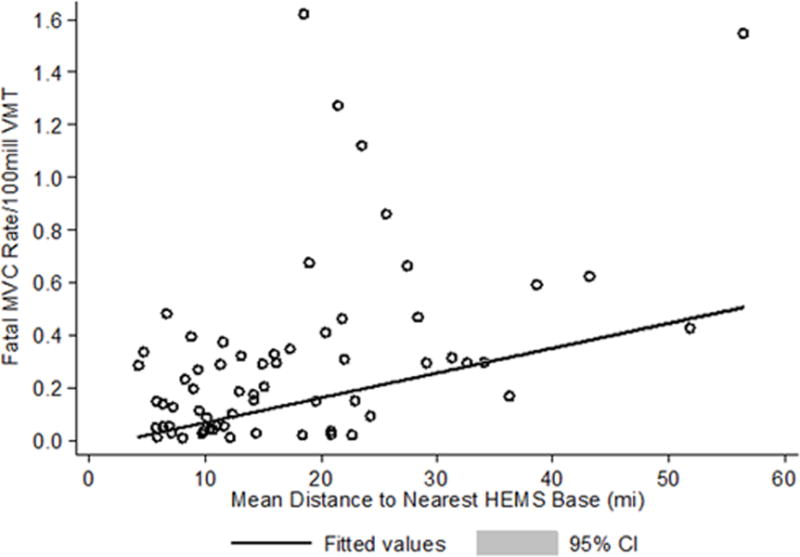
Plot of fatal MVC rate per 100 million vehicle miles traveled by mean distance to the nearest helicopter emergency medical services (HEMS) base. Each open circle represents a Pennsylvania county. Distance in miles represents mean of all fatal MVC events occurring within the county. Line represents fitted linear regression values with 95% confidence interval.
Spatial-lag regression adjusting for MVC and county characteristics again demonstrated a significant increase in the fatal MVC rate as distance increased from the nearest TSR (0.089 per 100 million VMT for each 10-mile increase, p=0.006). The fatal MVC rate also increased significantly as the distance to the nearest HEMS base increased (0.080 per 100 million VMT for each 10-mile increase, p=0.006). After adjustment in spatial lag regression, the fatal MVC rate was not associated with distance to the nearest trauma center (0.036 per 100 million VMT for each 10-mile increase, p=0.127).
Since HEMS bases appear to have the most influence over fatal MVC rates based on distance, two HEMS bases located at existing trauma centers were selected to evaluate the potential change in fatal MVC rates if redistributed to the highest fatality regions in Mifflin and Potter counties. The helicopter located at Robert Packer Guthrie Hospital in northern Bradford county (located in northeastern Pennsylvania) was moved to Cole Memorial Hospital in Potter county (located in northcentral Pennsylvania). Additionally, the helicopter located at University of Pittsburgh Medical Center Altoona in Blair county (located in southcentral Pennsylvania) was moved to Geisinger-Lewistown Hospital in Mifflin county (located in southcentral Pennsylvania). This redistribution of HEMS bases affected outcomes in seven counties, with a decrease in the average distance to the nearest TSR ranging from 0.1 miles to 50.2 miles. All seven counties had a decrease in the predicted fatal MVC rate ranging from 0.002 to 0.710 per 100 million VMT. The state-wide mean predicted fatal MVC rate from the model using current TSR locations was 0.199 per 100 million VMT. Under the proposed redistribution of two HEMS bases to high fatality areas, the state-wide mean predicted fatal MVC rate decreased to 0.174 per 100 million VMT. This translates to a 12.3% relative reduction in the fatal MVC rate overall across Pennsylvania.
In the second theoretical redistribution of TSR, two helicopters not located at a trauma center were selected to be moved to the same locations in Potter and Mifflin counties. The helicopter in Lycoming county (located in northeastern Pennsylvania) was moved to Cole Memorial Hospital in Potter county (located in northcentral Pennsylvania), while the helicopter in Centre county (located in central Pennsylvania) was moved to Geisinger-Lewistown Hospital in Mifflin county (located in southcentral Pennsylvania). This redistribution of HEMS bases affected outcomes in eleven counties, with seven counties seeing improvements while four counties had worsening of outcomes. In the seven counties positively affected, there was a decrease in the average distance to the nearest TSR ranging from 0.1 miles to 50.2 miles. These seven counties had a decrease in the predicted fatal MVC rate ranging from 0.027 to 0.708 per 100 million VMT. In the four counties adversely affected, there was an increase in the average distance to the nearest TSR ranging from 4.2 miles to 18.2 miles. These four counties had an increase in the predicted fatal MVC rate ranging from 0.037 to 0.230 per 100 million VMT. Under this proposed redistribution of two HEMS bases to high fatality areas, the state-wide mean predicted fatal MVC rate decreased to 0.181 per 100 million VMT. This translates to a 9.1% relative reduction in the fatal MVC rate overall across Pennsylvania.
DISCUSSION
This analysis demonstrated that fatal MVC rates are higher in geographic areas with fewer TSR nearby. Hotspot analysis confirmed that fatal MVC events cluster in areas farthest from TSR. Analysis at the county-level also shows that as the mean distance of fatal MVC events increases, the fatal MVC rate increases. This finding persists after controlling for county-level demographics, MVC characteristics, and the spatial correlation of outcomes. It also appears that this relationship is largely driven by the distance to the nearest HEMS base.
While these findings could be considered intuitive, perhaps the more salient finding is the use of incident level data to drive potential changes in TSR allocation has the potential to improve outcome. By redistributing only two HEMS bases into high MVC fatality areas identified in our geospatial analysis, predicted mortality was significantly reduced through optimizing the geospatial organization of the trauma system and reducing the distance to the nearest TSR. As would be expected, moving helicopters away from a current trauma center and effectively increasing the overall geographic coverage of TSR showed the most potential improvement, while redistributing TSR from one area to another showed a smaller gain as some areas lost TSR coverage. This issue is important, and geospatial modeling such as this may help to assess both the positive and negative potential impact of redistributing TSR in a system where it may only be possible to move resources from one area to another.
Two NHTSA research reports also evaluated the association of fatal MVC as reported in FARS and proximity to level I or II trauma centers and HEMS bases, reporting a similar relationship between MVC fatalities and distance to these TSR. When looking at distance to the nearest trauma center, patients with a 45 to 60 minute and those with a >60 minutes transport time to a level I or II trauma center had a 13% and 23% respective increase in the odds of dying on scene compared to non-fatal injury after MVC.24 Evaluation of proximity to HEMS bases revealed that 64% of fatally injured MVC occupants died on scene when outside of a HEMS 20 minute response area, while 55% died on scene when within a HEMS 20 minute response area.25
Several groups have examined the effect of geography on MVC outcomes. Increased MVC mortality in rural areas is a consistent finding, and many suggest a lack of proximity to emergency medical services and hospitals partly underlies this.12, 26–28 Clark and Cushing developed models of regional variation in MVC mortality.13 They were able to explain 74% of the variation in MVC mortality rates among US states using population density, mean distance between hospitals, and whether the state was in the southern US or not. The inter-hospital distance explained the most variation in mortality in their models, leading the authors to conclude improved organization and transport of MVC patients would likely have the greatest impact on outcomes, particularly in rural areas. Goldstein et al evaluated 1,754 US counties, finding the deaths per injury rate after MVC accounted for the greatest variation in MVC mortality and drove the rural-urban disparity.15 The authors conclude that dispersion of emergency medical resources and hospitals in rural areas like accounts for their findings of disproportionately higher case-fatality rates in rural areas. Our data take these groups’ work a step further by evaluating transporting HEMS resources as a component of the trauma system, and supports the concept that optimizing geographic organization and transport of MVC patients has the potential to improve outcome.
Clark and Cushing in an evaluation of MVC mortality rates in urban and rural areas found population density was associated with MVC mortality at the state-level even when controlling for VMT; however the presence of a state trauma system did not affect mortality.14 The authors analyzed trauma systems as a binary indicator of the presence or absence of a state trauma system, as well as restricted to those meeting seven or eight of the essential criteria published by Bass et al.29 Nathens and colleagues demonstrated a lag of 13 years before the presence of a state trauma system improved MVC outcomes, suggesting this represented the time necessary to optimize organization of system and transport resources.16 Taken with the current data, it appears that the formal presence of a trauma system alone may not reduce MVC mortality, but the geographic organization of resources within that system is an important component to potentially reduce mortality.
There are several potential reasons for our findings. It is not surprising that increasing distance from a fatal MVC to the nearest TSR was associated with higher mortality rates. This population clearly had severe injury ultimately resulting in death and many were likely time-sensitive. Increasing distance to TSR translates to longer delays to definitive care and poor outcome. HEMS base location appears to be a primary driver of this relationship. This is likely due in part to the greater number of HEMS bases relative to trauma centers, and thus for most MVC events a HEMS base was the closest TSR and point of potential entry into the trauma system. Several groups have demonstrated HEMS transport can significantly improve mortality, particularly in severely injured patients.30–33 Given this, we evaluated redistribution of HEMS bases into the two highest MVC fatality regions in the state. One can argue that placement of HEMS bases at a trauma center may not be the optimal geographic distribution of TSR. This limits the effective range of the helicopter and increases prehospital time compared to a system configured with HEMS bases located distant from trauma centers, in areas where they are more frequently utilized to transport patients. Thus, this simple optimization of TSR was predicted to reduce mortality across the state from MVC. Further, our second redistribution scenario shows that moving TSR from one area to another positively impacts some areas while potentially creating new areas of need. Techniques such as those used in this study may help to define the balance to ensure any proposed changes to the organization of TSR has an overall benefit while minimizing potential adverse effects in the trauma system.
Others have also used geospatial analysis to optimize TSR allocation and demonstrate the potential to improve outcomes. Branas et al developed the Trauma Resource Allocation Model for Ambulances and Hospitals, utilizing a spatial model of injured patients in Maryland to develop an algorithm that optimizes trauma center and HEMS base geographic distribution.17 This algorithm demonstrated optimal placement of TSR resulted in an improvement in access to trauma care within 30 minutes, demonstrating applicability of the model to mature trauma systems as well as the potential to aid less well developed systems. The Geospatial Evaluation of Systems of Trauma Care (GEOS) model was developed by Jansen and colleagues to optimize national TSR allocation in Scotland.34 The GEOS model incorporates prehospital triage guidelines to guide patient flow, models constraints based on center resources, bed capacities, and HEMS availability. This group has also demonstrated the utility of incident-level geospatial profiling in trauma system planning and development.35 Geospatial evaluation of TSR has also been used to optimize the time benefits of HEMS versus ground transport of trauma patients.36, 37
This study has several implications. First, it demonstrates the power of geographic information systems to provide insight to injury patterns across trauma systems. Second, it highlights the potential importance of the geospatial organization of TSR and their impact on outcomes. Finally, it demonstrates the ability to make data-driven changes to TSR allocation to potentially improve outcomes. We altered only two helicopter bases and demonstrated a potential reduction in MVC fatality rates under both redistribution scenarios. This is also helpful to allow prediction of realistic changes in the organization of TSR, as redistributing trauma centers in a mature trauma system such as Pennsylvania is likely not feasible.
There are several limitations for consideration. First, this is a retrospective study, linking data from several sources. This also results in limited data available for interactions among factors related to MVC mortality. Further, FARS data does not include detailed data regarding type or severity of injuries. County-level analysis precludes the complexities of individual patient responses and outcomes. As noted above, analysis was at the county-level; however regional trauma systems catchment areas may cross several county lines and include portions of neighboring states. In addition to the geospatial configuration of trauma centers and HEMS bases, appropriate triage and utilization of these resources varies geographically and impacts outcomes. We also did not include the contribution of ground EMS resources as their precise distribution and availability is more dynamic; nevertheless, these also factor into outcomes in the trauma system.
We only narrowly interrogated our model in terms of redistributing TSR, while there are many possible iterations. We chose to only move two HEMS bases for two main reasons. First, there were two obvious large areas of high fatal MVC regions identified in the geospatial analysis clearly lacking any TSR in proximity. Second, we sought to determine if small changes in the organization of TSR could potentially impact outcomes, as large scale redistribution of TSR in mature trauma systems is likely not feasible. Our two redistribution scenarios were meant to evaluate increasing TSR coverage and redistribution of TSR coverage, demonstrating the later can potentially harm areas losing these resources. We used the same new HEMS base locations to allow for comparison across the scenarios. There are multiple other possibilities that were not considered given the scope and constraints of this study, but certainly deserve further investigation. Finally, the specific results of this study are highly specific to the geography of Pennsylvania and cannot be applied elsewhere. Despite this, the application of these techniques is generalizable to other geographic areas to potentially help optimize the geospatial organization of TSR.
CONCLUSION
Increasing distance to the nearest TSR is associated with increasing fatal MVC rate in Pennsylvania. This finding persists when adjusting for MVC and local characteristics, suggesting geographic organization of trauma systems influences outcome. Importantly, geospatial analysis of incident level data can target problem areas to allow data-driven changes to the geospatial organization of trauma system resources with the potential to improve outcomes.
Acknowledgments
Air medical data obtained August 4, 2016 from the Atlas and Database of Air Medical Services (ADAMS), compiled by and under license from CUBRC’s Public Safety & Transportation Group in alliance with the Association of Air Medical Services (AAMS) and the air medical industry. This publication is solely the responsibility of the authors and does not necessarily represent the official views of either CUBRC Inc., or AAMS.
No funding or support was directly received to perform the current study. Dr. Brown receives support from an institutional T32 Ruth L. Kischstein National Research Service Award training grant (5T32GM008516-20) from the National Institutes of Health.
Footnotes
There are no conflicts of interest for the current study
This paper was presented as an oral podium presentation at the 30th Annual Scientific Assembly of the Eastern Association for the Surgery of Trauma, January 10–14th, 2017; Hollywood, FL.
Level of Evidence: III, epidemiologic
AUTHOR CONTRIBUTIONS: J.B.B., M.R.R., and J.L.S. designed the study and performed the literature search. J.B.B. performed the data collection. J.B.B performed the data analysis. J.B.B., M.R.R, and J.L.S. participated in initial manuscript preparation. All authors contributed to data interpretation and critical revision of the manuscript.
References
- 1.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 2.MacKenzie EJ, Weir S, Rivara FP, Jurkovich GJ, Nathens AB, Wang W, Scharfstein DO, Salkever DS. The value of trauma center care. J Trauma. 2010;69:1–10. doi: 10.1097/TA.0b013e3181e03a21. [DOI] [PubMed] [Google Scholar]
- 3.Nathens AB, Jurkovich GJ, Rivara FP, Maier RV. Effectiveness of state trauma systems in reducing injury-related mortality: a national evaluation. J Trauma. 2000;48:25–30. doi: 10.1097/00005373-200001000-00005. discussion 30–21. [DOI] [PubMed] [Google Scholar]
- 4.Branas CC, MacKenzie EJ, Williams JC, Schwab CW, Teter HM, Flanigan MC, Blatt AJ, ReVelle CS. Access to trauma centers in the United States. JAMA. 2005;293:2626–2633. doi: 10.1001/jama.293.21.2626. [DOI] [PubMed] [Google Scholar]
- 5.Gomez D, Haas B, Doumouras AG, Zagorski B, Ray J, Rubenfeld G, McLellan BA, Boyes DM, Nathens AB. A population-based analysis of the discrepancy between potential and realized access to trauma center care. Ann Surg. 2013;257:160–165. doi: 10.1097/SLA.0b013e31827b9649. [DOI] [PubMed] [Google Scholar]
- 6.Hsia RY, Wang E, Torres H, Saynina O, Wise PH. Disparities in trauma center access despite increasing utilization: data from California, 1999 to 2006. J Trauma. 2010;68:217–224. doi: 10.1097/TA.0b013e3181a0e66d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Minei JP, Schmicker RH, Kerby JD, Stiell IG, Schreiber MA, Bulger E, Tisherman S, Hoyt DB, Nichol G, Resuscitation Outcome Consortium I Severe traumatic injury: regional variation in incidence and outcome. Ann Surg. 2010;252:149–157. doi: 10.1097/SLA.0b013e3181df0401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown JB, Gestring ML, Stassen NA, Forsythe RM, Billiar TR, Peitzman AB, Sperry JL. Geographic Variation in Outcome Benefits of Helicopter Transport for Trauma in the United States. Annals of Surgery. 2015;1 doi: 10.1097/SLA.0000000000001047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hsia R, Shen YC. Possible geographical barriers to trauma center access for vulnerable patients in the United States: an analysis of urban and rural communities. Arch Surg. 2011;146:46–52. doi: 10.1001/archsurg.2010.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mann NC, MacKenzie E, Teitelbaum SD, Wright D, Anderson C. Trauma System Structure and Viability in the Current Healthcare Environment: A State-by-State Assessment. The Journal of Trauma: Injury, Infection, and Critical Care. 2005;58:136–147. doi: 10.1097/01.ta.0000151181.44658.0a. [DOI] [PubMed] [Google Scholar]
- 11.Brown JB, Rosengart MR, Billiar TR, Peitzman AB, Sperry JL. Geographic distribution of trauma centers and injury-related mortality in the United States. J Trauma Acute Care Surg. 2016;80:42–50. doi: 10.1097/TA.0000000000000902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clark DE. Effect of population density on mortality after motor vehicle collisions. Accid Anal Prev. 2003;35:965–971. doi: 10.1016/s0001-4575(02)00104-5. [DOI] [PubMed] [Google Scholar]
- 13.Clark DE, Cushing BM. Predicting regional variations in mortality from motor vehicle crashes. Acad Emerg Med. 1999;6:125–130. doi: 10.1111/j.1553-2712.1999.tb01050.x. [DOI] [PubMed] [Google Scholar]
- 14.Clark DE, Cushing BM. Rural and urban traffic fatalities, vehicle miles, and population density. Accid Anal Prev. 2004;36:967–972. doi: 10.1016/j.aap.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 15.Goldstein GP, Clark DE, Travis LL, Haskins AE. Explaining regional disparities in traffic mortality by decomposing conditional probabilities. Inj Prev. 2011;17:84–90. doi: 10.1136/ip.2010.029249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nathens AB, Jurkovich GJ, Cummings P, Rivara FP, Maier RV. The effect of organized systems of trauma care on motor vehicle crash mortality. JAMA. 2000;283:1990–1994. doi: 10.1001/jama.283.15.1990. [DOI] [PubMed] [Google Scholar]
- 17.Branas CC, MacKenzie EJ, Revelle CS. A Trauma Resource Allocation Model for Ambulances and Hospitals. Health Services Research. 2000;35:489–507. [PMC free article] [PubMed] [Google Scholar]
- 18.Carr B, Branas C. TraumaMaps.org Trauma Center Maps. University of Pennsylvania Cartographic Modeling Laboratory; Copyright © 2006 Trustees of the University of Pennsylvania. Available at: www.traumamaps.org. Accessed: 28, February 2014. [Google Scholar]
- 19.National Highway Traffic Safety Administration. Fatality Analysis Reporting System (FARS) Analytical User’s Manual 1975-2014. Available at: https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/812316. Accessed: March 23, 2016.
- 20.Oliver M. Kriging: A method of interpolation for Geographical Information Systems. International J Geographic Information Systems. 1900;4:313–332. [Google Scholar]
- 21.Pilz J, Spock G. Why Do We Need and How Should We Implement Bayesian Kriging Methods. Stoch Environ Res Risk Assess. 2008;22:621–632. [Google Scholar]
- 22.Getis A, Ord JK. The analysis of spatial association by use of distance statistics. Geographical Analysis. 1992;24:189–206. [Google Scholar]
- 23.Ward MD, Skrede-Gleditsch K. Spatial Regression Models. Quantitative Applications in the Social Sciences. 2008;155 [Google Scholar]
- 24.National Highway Traffic Safety Administration. The Association Between Crash Proximity to Level 1 and 2 Trauma Centers and Crash Scene Mortality of Drivers Injured in Fatal Crashes. Available at: https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/811599. Accessed: November 14, 2016.
- 25.National Highway Traffic Safety Administration. Analysis of the Proximity of Fatal Motor Vehicle Crash Locations to the Availability of Helicopter Emergency Medical Service Response. Available at: https://crashstats.nhtsa.dot.gov/Api/Public/ViewPublication/811542. Accessed: November 14, 2016. [PubMed]
- 26.Travis LL, Clark DE, Haskins AE, Kilch JA. Mortality in rural locations after severe injuries from motor vehicle crashes. J Safety Res. 2012;43:375–380. doi: 10.1016/j.jsr.2012.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brodsky H, Hakkert AS. Highway fatal accidents and accessibility of emergency medical services. Soc Sci Med. 1983;17:731–740. doi: 10.1016/0277-9536(83)90261-7. [DOI] [PubMed] [Google Scholar]
- 28.Jones AP, Bentham G. Emergency medical service accessibility and outcome from road traffic accidents. Public Health. 1995;109:169–177. doi: 10.1016/s0033-3506(05)80049-6. [DOI] [PubMed] [Google Scholar]
- 29.Bass RR, Gainer PS, Carlini AR. Update on trauma system development in the United States. J Trauma. 1999;47:S15–21. doi: 10.1097/00005373-199909001-00005. [DOI] [PubMed] [Google Scholar]
- 30.Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Helicopters and the civilian trauma system: national utilization patterns demonstrate improved outcomes after traumatic injury. J Trauma. 2010;69:1030–1034. doi: 10.1097/TA.0b013e3181f6f450. discussion 1034–1036. [DOI] [PubMed] [Google Scholar]
- 31.Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Helicopters improve survival in seriously injured patients requiring interfacility transfer for definitive care. J Trauma. 2011;70:310–314. doi: 10.1097/TA.0b013e3182032b4f. [DOI] [PubMed] [Google Scholar]
- 32.Galvagno SM, Jr, Haut ER, Zafar SN, Millin MG, Efron DT, Koenig GJ, Jr, Baker SP, Bowman SM, Pronovost PJ, Haider AH. Association between helicopter vs ground emergency medical services and survival for adults with major trauma. JAMA. 2012;307:1602–1610. doi: 10.1001/jama.2012.467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sullivent EE, Faul M, Wald MM. Reduced mortality in injured adults transported by helicopter emergency medical services. Prehosp Emerg Care. 2011;15:295–302. doi: 10.3109/10903127.2011.569849. [DOI] [PubMed] [Google Scholar]
- 34.Jansen JO, Morrison JJ, Wang H, Lawrenson R, Egan G, He S, Campbell MK. Optimizing trauma system design: the GEOS (Geospatial Evaluation of Systems of Trauma Care) approach. J Trauma Acute Care Surg. 2014;76:1035–1040. doi: 10.1097/TA.0000000000000196. [DOI] [PubMed] [Google Scholar]
- 35.Jansen JO, Morrison JJ, Wang H, He S, Lawrenson R, Campbell MK, Green DR. Feasibility and utility of population-level geospatial injury profiling: prospective, national cohort study. J Trauma Acute Care Surg. 2015;78:962–969. doi: 10.1097/TA.0000000000000617. [DOI] [PubMed] [Google Scholar]
- 36.Shaw JJ, Psoinos CM, Santry HP. It’s All About Location, Location, Location: A New Perspective on Trauma Transport. Ann Surg. 2015 doi: 10.1097/SLA.0000000000001265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Widener MJ, Ginsberg Z, Schleith D, Floccare DJ, Hirshon JM, Galvagno S. Ground and Helicopter Emergency Medical Services Time Tradeoffs Assessed with Geographic Information. Aerosp Med Hum Perform. 2015;86:620–627. doi: 10.3357/AMHP.4173.2015. [DOI] [PubMed] [Google Scholar]


