Abstract
Background/Objectives
Hospitalization in community-dwelling elderly is often accompanied by functional loss, increasing the risk for continued functional decline and future institutionalization. The primary objective of our study was to examine the hospital-level variation in rates of new institutionalizations among Medicare beneficiaries.
Design
Retrospective cohort study.
Setting
Hospitals and nursing homes.
Participants
Medicare fee-for-service beneficiaries discharged from 4,469 hospitals in 2013 (N=4,824,040).
Measurements
New institutionalization, defined as new long term care nursing home residence (not skilled nursing facility) of at least 90 days duration within six months of hospital discharge.
Results
The overall observed rate of new institutionalizations was 3.6% (N=173,998). Older age, white race, Medicaid eligibility, longer hospitalization, and having a skilled nursing facility stay over the six months before hospitalization were associated with higher adjusted odds. Observed rates ranged from 0.9–5.9% across states. The variation in rates attributable to the hospital after adjusting for case-mix and state was 5.1%. Odds were higher for patients treated in smaller (OR=1.36, 95% CI: 1.27–1.45, ≤50 vs >500 beds), government owned (OR=1.15, 95% CI: 1.09–1.21 compared to for-profit), limited medical school affiliation (OR=1.13, 95% CI: 1.07–1.19 compared to major) hospitals and lower for patients treated in urban hospitals (OR=0.79, 95% CI: 0.76–0.82 compared to rural). Higher Summary Star ratings (OR=0.75, 95% CI: 0.67–0.93, five vs one stars) and Overall Hospital Rating (OR=0.62, 95% CI: 0.57–0.67, ratings of 9–10 vs 0) were associated with lower odds of institutionalization.
Conclusion
Hospitalization may be a critical period for preventing future institutionalization among elderly patients. The variation in rates across hospitals and its association with hospital quality ratings suggest some of these institutionalizations are avoidable and may represent targets for care improvement.
Keywords: elderly, nursing home, quality of care, hospital ratings, functional status
Introduction
Hospitalization is a vulnerable period for older adults.1–4 Older adults hospitalized for an acute illness or injury usually spend most of their stay in bed.5–7 Short-term bed rest in this population results in a loss of lean muscle mass, as well as declines in strength and aerobic capacity.8,9 Notably, functional decline occurs during hospitalization,1,2,4,10,11 even among previously healthy older adults.11
The adverse effects of hospitalization can extend beyond hospital discharge, resulting in continued care needs. Many different potential pathways following hospitalization exist; however, they typically start with discharge to post-acute care or directly to the community. Regardless of initial discharge setting, hospitalization may precipitate a trajectory of continued decline and subsequent institutionalization.2,3,10–14 Among Medicare beneficiaries, a majority of new institutionalizations in long term care nursing homes are preceded by a hospitalization.3 Therefore, hospitalization may represent a critical period for preventing the trajectory of decline leading to institutionalization.
Recognizing the vulnerability of hospitalized elderly patients, some hospitals have implemented specialized geriatric care in the form of hospital-wide programs or designated units.15–17 Programs, such as the Hospital Elder Life Program (HELP) and Nurses Improving the Care of Healthsystem Elders (NICHE), provide care targeted to the unique needs of hospitalized older patients within the existing hospital structure.17,18 Specialized units, such as Geriatric Evaluation and Management Units and Acute Care for the Elderly (ACE) units, focus on maintaining function through patient-centered care delivered by an interdisciplinary team in a specially structured environment.15,19,20 Averting within stay functional loss may place older adults on a healthier post-hospital trajectory and perhaps prevent the continued decline that places the patient at-risk for institutionalization.21
Given that hospital cultures and care processes vary across facilities, it is likely that patient risk of future institutionalization varies across facilities, as well. This has not been studied in a national cohort. The primary objective of our study was to examine the hospital-level variation in rates of new institutionalizations among Medicare fee-for-service beneficiaries. We hypothesized that rates of future institutionalizations would vary across hospitals, even after adjustment for case-mix and state.
Institutionalization has been defined various ways in the literature, with the term referring to settings with differing degrees of permanence. We defined “new institutionalization” as residence in a long term care nursing home for at least 90 days, within six months of hospital discharge, among patients who had not resided in long term care at any point over the six months prior to hospitalization. Patients could spend time as short-stay residents in skilled nursing facilities (SNF) over this time period, but these days were not included in the long term care day count. Compared to SNF stays for short-term rehabilitative services,22 long term care nursing home stays more likely represent an irreversible point in the trajectory of decline.23
Methods
Data Sources
The following 100% Medicare files from 2012–2014 were used to address the study objective: Medicare Provider Analysis and Review (MedPAR) and Resident Assessment Instrument Minimum Date Set 3.0 (MDS). Beneficiary demographic and enrollment data were extracted from Medicare Denominator Files and hospital characteristics from Provider of Service (POS) files24 and Hospital Compare Datasets.25 The 2011 Medicaid Long Term Care file from Texas was used to validate the outcome of a long term stay, as defined below. The study was approved by the University Institutional Review Board, and a Data Use Agreement was completed following the Centers for Medicare & Medicaid Services (CMS) requirements.
Study population
The cohort was Medicare fee-for-service beneficiaries discharged from an acute care hospital. Cohort selection is presented in Figure 1. We first identified all hospital discharges in the 2013 100% national MedPAR claims data for beneficiaries over age 65 with continuous Medicare Part A coverage (no HMO) over the 12 months prior to, and six months following, hospitalization. The windows surrounding hospitalization allowed for assessment of comorbidities (12-month look back) and identification of the outcome. Patients also had to survive for nine months following discharge (N=5,475,229). Because we were interested in “new” institutionalizations, patients who resided in long term care at any point over the six months prior to hospitalization were excluded. Discharges with outlier hospital lengths of stay were also excluded. Outliers were defined as lengths of stay >2 geometric standard deviations from the geometric mean, calculated separately for each diagnosis-related group major diagnostic category (DRG-MDC). Discharges from hospitals with <25 claims were excluded, as were discharges from hospitals with missing data in the Provider of Service (POS) file. Finally, for analyses including hospital-level factors, discharges from hospitals with missing data in the Hospital Compare Datasets for Summary Star Ratings (n=116,910) and Overall Hospital Rating (n=331,807) were excluded.
Figure 1.
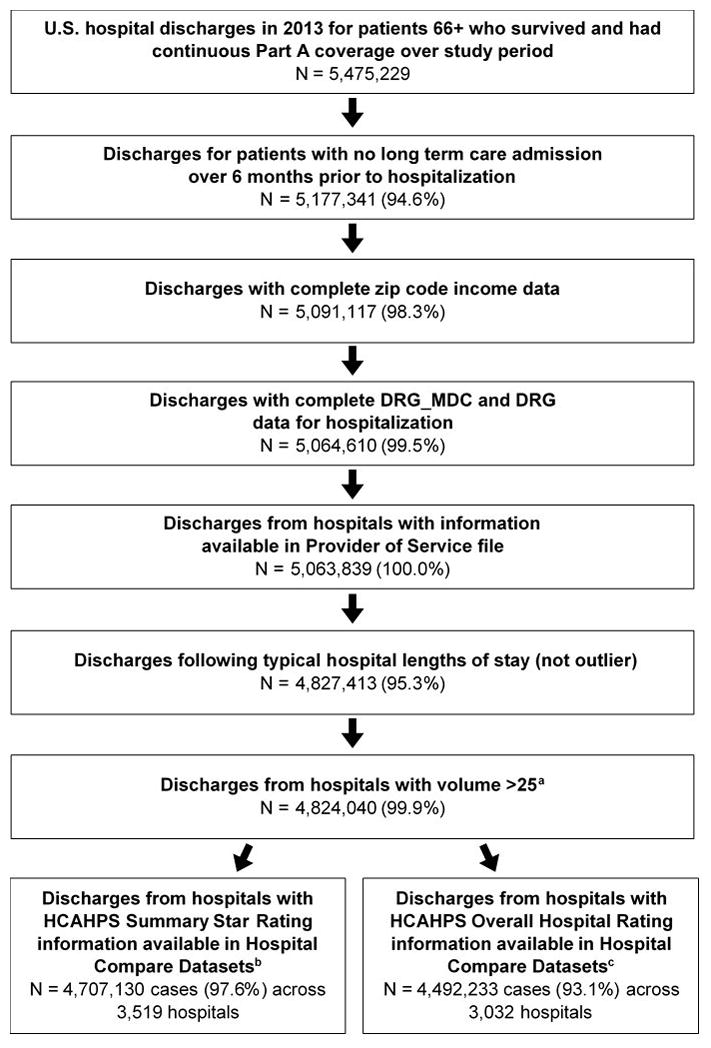
Cohort selection. Discharges remaining (N) at each step as the sample criteria are applied. Percentages are the percent remaining from previous step. Final cohorts for a) patient and state-level analyses, b) hospital-level analyses including HCAHPS Summary Star Rating, c) hospital-level analyses including HCAHPS Overall Hospital Rating item. Abbreviations: DRG, diagnosis-related group; MDC, major diagnostic category; HCAHPS, Hospital Consumer Assessment of Healthcare Providers and Systems
Predictors
Patient characteristics
Beneficiary age, sex, race/ethnicity (White, Black, Hispanic, Other), and Medicaid eligibility were extracted from Medicare Denominator Files. Income level at the beneficiary’s zip code of residence was obtained from the 2013 American Community Survey estimates of the U.S. Census Bureau.26 Elixhauser comorbidities were identified by reviewing all discharge diagnoses associated with MedPAR hospital claims for the index hospitalization and those over the prior 12 months.27 The Elixhauser approach was developed for use with administrative datasets and identifies 31 comorbid conditions, defined as diagnoses that may impact healthcare utilization and/or mortality.27 Because our outcome was new institutionalization, we added two comorbidities: dementia and delirium. MedPAR claims for the index hospitalization were used to determine the MDC-DRG, Intensive Care Unit (ICU) utilization, and length of stay.
Hospital characteristics
Information on hospital bed size, location (urban/rural), type (for-profit, nonprofit, government), and medical school affiliation (major, limited, graduate, no affiliation) was extracted from Provider of Service files. Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey Summary Star Ratings were obtained from Hospital Compare files.28 The star ratings are composite scores, ranging from one to five, calculated by CMS based on measures of patient experiences, including: nurse communication, doctor communication, responsiveness of hospital staff, pain management, communication about medicines, discharge information, care transition, cleanliness of hospital environment, quietness of hospital environment, overall hospital rating, and willingness to recommend the hospital.29 Higher star ratings are associated with lower readmission and mortality rates; however, the association between star ratings and rates of new institutionalizations has not been investigated.30,31 Performance on the Overall Hospital Rating item of the HCAHPS survey was extracted, as well. The item reads “Using any number from 0 to 10, where 0 is the worst hospital possible and 10 is the best hospital possible, what number would you rate this hospital during your stay?”32–34 Patient experience is a “unique and vital aspect of hospital quality”,33 and hospital scores on the HCAHPS survey are used in the Hospital Value-Based Purchasing Program.35 The survey is not administered to those residing in nursing homes.
Residence in long term care
Long term care stays were identified using MDS assessment records for residence in nursing homes, after excluding SNF stays using claims for SNF services in the MedPAR file, based on the method of Intrator, et al.36 This approach allowed us to distinguish long term care stays from SNF stays. For patients who transitioned from SNF care to long term care within the same facility, the date the SNF claim ended was considered the admission date to long term care. We validated our approach of using MedPAR claims and MDS records to identify long term care residence (≥90 days), using Medicaid long term care claims as the gold standard, in a subsample of dual eligible beneficiaries (sensitivity 93.1%; positive predictive value 85.7%).
Outcome
The outcome was “new institutionalization”, which we defined as a new residence in a long term care nursing home for at least 90 consecutive days starting within six months of hospital discharge.23 Long term care nursing home stays that were interrupted by a hospitalization with or without a SNF stay were considered a single episode if the individual returned to long term care within seven days of hospital or SNF discharge.37
Statistical analysis
Hospital rates of new institutionalizations were estimated from a multilevel logistic regression model adjusted for case-mix and state. States vary in 1) funding for long term care and provision of community alternatives to nursing homes38 and 2) availability and occupancy of nursing home beds.39 Multilevel logistic regression allowed us to model a dichotomous outcome (new institutionalization, yes/no) while controlling for the clustering of patients within hospitals. The adjusted rates were used to examine the variation in rates remaining if every facility treated the average case-mix (patient-level factors presented in Table 1 and Supplementary Table S1) and the influences of state were removed.38 The adjusted rates and corresponding 95% confidence intervals (CI) were ranked and plotted. Hospitals with 95% confidence intervals for adjusted rates entirely above or below the average adjusted rate were identified on the plot. To describe the facility-level variation, Intraclass Correlation Coefficients (ICC) were calculated from multilevel logistic regression models.40 First, the ICC for an empty model including only a facility identifier was calculated. We then calculated the ICC for the model adjusted for case-mix and state. Sensitivity analyses examining facility-level variation in rates of new institutionalizations were performed for the following subgroups: patients hospitalized for pneumonia, COPD or congestive heart failure; patients hospitalized following a hip fracture; and patients hospitalized for any medical DRG. We also tested the mortality effect by examining facility-level variation in a cohort that did not exclude those who died and adjusting for death. SAS version 9.4 (SAS Institute, Cary, NC) was used for all statistical analyses.
Table 1.
Patient-level predictors of new institutionalization
| N (%) | Observed Rates | Odds Ratioa (95% CI) | |
|---|---|---|---|
| All | 4,824,040 | 3.6% | |
| Age (years) | |||
| 66 – 70 | 1,088,294 (22.6) | 1.4% | Reference |
| 71 – 75 | 1,019,135 (21.1) | 2.0% | 1.42 (1.38, 1.46) |
| 76 – 80 | 941,903 (19.5) | 3.0% | 2.00 (1.94, 2.05) |
| 81 – 85 | 855,966 (17.7) | 4.6% | 2.95 (2.87, 3.03) |
| 86 – 90 | 607,622 (12.6) | 6.7% | 4.25 (4.13, 4.36) |
| ≥91 | 311,120 (6.5) | 9.9% | 6.57 (6.38, 6.76) |
| Sex | |||
| Female | 2,786,145 (57.8) | 4.3% | Reference |
| Male | 2,037,895 (42.2) | 2.7% | 0.98 (0.96, 0.99) |
| Race/Ethnicity | |||
| White | 4,058,115 (84.1) | 3.6% | Reference |
| Black | 389,400 (8.1) | 4.5% | 0.79 (0.77, 0.81) |
| Hispanic | 228,961 (4.8) | 3.3% | 0.56 (0.54, 0.58) |
| Others | 147,564 (3.1) | 3.3% | 0.68 (0.65, 0.71) |
| Medicaid eligibility | |||
| No | 4,020,084 (83.3) | 2.5% | Reference |
| Yes | 803,956 (16.7) | 9.3% | 4.35 (4.29, 4.42) |
| Income quartileb | |||
| <40,696 | 1,205,843 (25.0) | 4.1% | Reference |
| 40,696 – 50,810 | 1,205,851 (25.0) | 3.8% | 1.06 (1.03, 1.08) |
| 50,810 – 66,898 | 1,206,331 (25.0) | 3.4% | 1.07 (1.04, 1.09) |
| >66,898 | 1,206,015 (25.0) | 3.1% | 1.09 (1.07, 1.12) |
| SNF prior 6 monthsc | |||
| No | 4,382,120 (90.8) | 2.5% | Reference |
| Yes | 441,920 (9.2) | 14.2% | 4.51 (4.44, 4.58) |
| Type of DRG | |||
| Medical | 3,298,379 (68.4) | 4.4% | Reference |
| Surgical | 1,525,661 (31.6) | 1.8% | 0.55 (0.54, 0.56) |
| Length of hospital stayd | |||
| Quartile 1 | 1,693,688 (35.1) | 1.5% | Reference |
| Quartile 2 | 1,258,153 (26.1) | 3.7% | 2.05 (2.01, 2.09) |
| Quartile 3 | 886,713 (18.4) | 4.7% | 2.38 (2.33, 2.44) |
| Quartile 4 | 985,486 (20.4) | 6.1% | 3.05 (2.99, 3.11) |
| ICUe | |||
| No | 3,598,522 (74.6) | 3.6% | Reference |
| Yes | 1,225,518 (25.4) | 3.5% | 0.95 (0.94, 0.97) |
Abbreviations: SNF, skilled nursing facility; DRG, diagnostic-related group; ICU, intensive care unit
Odds ratios are from a multilevel model adjusted for all characteristics presented in the table, as well as patients’ comorbidities and diagnostic group (DRG_MDC) (Supplementary Table S1) and hospital state.
Income level at the beneficiary’s zip code of residence obtained from the 2013 American Community Survey (ACS) estimates of the U.S. Census Bureau.
Received care in a skilled nursing facility in the six months prior to hospitalization.
Length of stay quartiles based on expected length of stay for the admitting diagnosis-related group major diagnostic category (DRG-MDC).
Admitted to ICU during index hospitalization.
Results
Distributions of patient characteristics across the 4,824,040 hospital discharges are presented in Table 1. The overall observed rate of new institutionalization was 3.6% (N=173,998). Long term care length of stay was assessed in a subgroup discharged during the first six months of 2013, allowing at least one year of follow-up. In this subgroup of newly institutionalized patients (N=85,559), 67.5% had long term care stays lasting at least 365 days. As expected, older age and race/ethnicity were associated with institutionalization.41,42 Hispanics had lower rates (3.3% vs. 3.6%) and adjusted odds (odds ratio (OR)=0.56, 95% CI: 0.54–0.58) of institutionalization compared to whites. Blacks had higher observed rates than whites (4.5 vs. 3.6%); however, in adjusted analyses black race (OR=0.79, 95% CI: 0.77–0.81) had a protective effect compared to white race. Medicaid eligibility at hospital discharge was associated with higher adjusted odds (OR=4.35, 95% CI: 4.29–4.42) of institutionalization. Further analyses not shown indicated that differences in Medicaid eligibility explained the differences between the unadjusted rates and adjusted OR values for black race. Patients with longer hospital stays were at increased risk for institutionalization, as were those who had a SNF stay in the six months prior to hospitalization. Refer to Table 1 for a complete listing of observed rates and ORs adjusted for all variables listed in the table, as well as for patients’ comorbidities and hospital diagnostic group (DRG_MDC) (Supplementary Table S1).
State-level variation in observed rates of new institutionalizations is presented in Figure 2. Lower rates were observed in western states, while higher rates were observed in the Midwest. Rates were ≤1.0% in Arizona and Alaska and ≥5.0% in North and South Dakota, Iowa, Kansas, and Nebraska.
Figure 2.
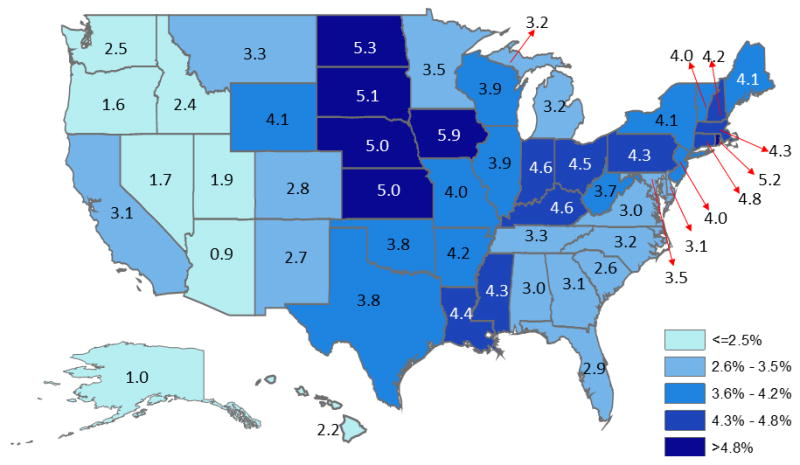
State-level variation in the observed rates of new institutionalizations following discharge from an acute care hospital. N = 4,824,040.
Hospital-level variation
Based on the ICC for the empty multilevel model, 11.4% of the variation in rates of new institutionalizations was attributable to the hospital. After adjusting for case-mix (all patient-level factors in Table 1 and Supplementary Table S1) and state, the variation attributable to the hospital was 5.1%. Figure 3 presents hospital rates of new institutionalizations adjusted for case-mix and state. There were 390 (8.7%) hospitals that performed significantly better than average and 811 (18.2%) hospitals that performed significantly worse. If hospitals with adjusted rates higher than the 25th percentile improved to the 25th percentile, 32,738 (28%) new institutionalizations would be avoided. In sensitivity analyses, after adjusting for case-mix and state, the variation attributable to the hospital was 4.8% among patients hospitalized for pneumonia, COPD or congestive heart failure; 2.8% among patients hospitalized following a hip fracture; and 4.6% among patients hospitalized for any medical DRG. In a cohort that included those who died over the nine months following hospitalization, the hospital-level variation was 5.0%. The adjusted rates of new institutionalizations for hospitals generated from that multilevel model were very close to those generated from the multilevel model presented in Figure 3, with a Pearson correlation coefficient of 0.97 (p <0.001).
Figure 3.
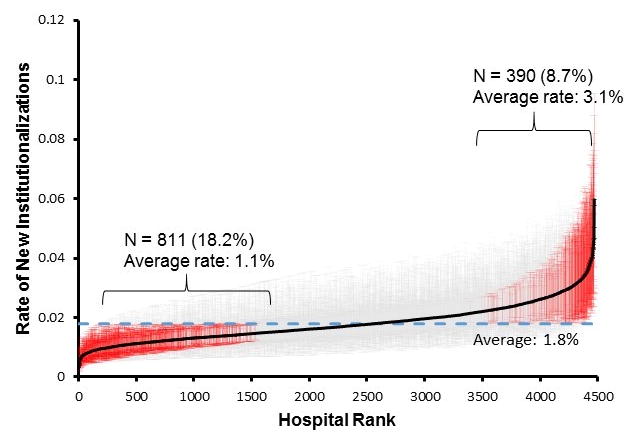
Variation among hospitals in adjusted rates of new institutionalizations. Hospitals were ranked based on rates from a multilevel model adjusted for state and case-mix (patient characteristics in Table 1 and Supplementary Table S1). The dotted line represents the overall average adjusted rate. Hospitals with 95% confidence intervals for rates entirely above or below the average adjusted rate are indicated in red. Results are presented for 4,469 hospitals and 4,824,040 discharges. Note: The average adjusted rate of institutionalization, 1.8%, is considerably lower than the overall rate of 3.6%. This is because the average adjusted rate is derived from a multilevel model that assumes every facility treated the average case-mix (patient-level factors presented in Table 1 and Supplementary Table S1) and removes the influences of state.
Hospital characteristics
Distributions of hospital characteristics across the 3,519 facilities are presented in Table 2. Observed rates of new institutionalizations and ORs adjusted for patient and facility characteristics are also presented in Table 2. Rates and adjusted odds increased as hospital size decreased (OR=1.36, 95% CI: 1.27–1.45, ≤50 vs >500 beds). Odds were also increased following care in government-owned (OR=1.15, 95% CI: 1.09–1.21) and nonprofit hospitals (OR=1.11, 95% CI: 1.07–1.16) compared for-profit hospitals. Care in limited (OR=1.13, 95% CI: 1.07–1.19) or no (OR=1.09, 95% CI: 1.04–1.14) medical school affiliation hospitals was associated with increased odds compared to care in hospitals with a major medical school affiliation. Patients treated in urban hospitals had lower odds of institutionalization (OR=0.79, 95% CI: 0.76–0.82).
Table 2.
Hospital-level predictors of new institutionalizationa
| N (%) | Observed rate | Odds ratio (95% CI)b | |
|---|---|---|---|
| All | 4,707,130 | 3.5% | |
| Bed Size | |||
| > 500 | 1,303,245 (27.7) | 3.0% | Reference |
| 401 – 500 | 510,919 (10.9) | 3.4% | 1.03 (0.96, 1.10) |
| 301 – 400 | 763,042 (16.2) | 3.4% | 1.04 (0.98, 1.10) |
| 201 – 300 | 876,486 (18.6) | 3.6% | 1.09 (1.03, 1.15) |
| 101 – 200 | 774,050 (16.4) | 4.0% | 1.18 (1.12, 1.24) |
| 51 – 100 | 294,387 (6.3) | 4.3% | 1.29 (1.21, 1.37) |
| ≤ 50 | 185,001 (3.9) | 4.7% | 1.36 (1.27, 1.45) |
| Location | |||
| Rural | 655,151 (13.9) | 4.8% | Reference |
| Urban | 4,051,979 (86.1) | 3.3% | 0.79 (0.76, 0.82) |
| Type of provider | |||
| For-profit | 703,533 (15.0) | 3.3% | Reference |
| Government | 582,037 (12.4) | 3.6% | 1.15 (1.09, 1.21) |
| Nonprofit | 3,421,560 (72.7) | 3.6% | 1.11 (1.07, 1.16) |
| Medical School Affiliation | |||
| Major | 1,109,932 (23.6) | 3.2% | Reference |
| Limited | 875,144 (18.6) | 3.6% | 1.13 (1.07, 1.19) |
| Graduate | 223,415 (4.8) | 3.2% | 1.05 (0.97, 1.13) |
| No affiliation | 2,498,639 (53.1) | 3.7% | 1.09 (1.04, 1.14) |
| HCAHPS Summary Star Ratingc | |||
| 1 star | 97,820 (2.1) | 4.7% | Reference |
| 2 stars | 838,468 (17.8) | 3.8% | 1.00 (0.92, 1.09) |
| 3 stars | 2,255,893 (47.9) | 3.5% | 0.94 (0.86, 1.02) |
| 4 stars | 1,417,653 (30.1) | 3.3% | 0.88 (0.81, 0.96) |
| 5 stars | 97,296 (2.1) | 3.0% | 0.75 (0.67, 0.93) |
Abbreviations: HCAHPS, Hospital Consumer Assessment of Healthcare Providers and Systems
Discharges from hospitals with missing data in the Hospital Compare Datasets were excluded (N=116,887). Results presented for 4,706,267 discharges across 3,519 hospitals.
Odds ratios are from a multilevel model adjusted for all patient characteristics presented in Table 1 and Supplementary Table S1, as well as hospital characteristics presented in this table.
HCAHPS Summary Star Rating from Hospital Compare website (https://www.medicare.gov/hospitalcompare/Data/HCAHPS-Star-Ratings.html).
There was a clear association between new institutionalizations and hospital quality ratings. Patients’ odds for institutionalization was decreased at facilities with four and five star ratings on the HCAHPS Summary Star Rating. Compared to those discharged from hospitals with only one star, patients discharged from hospitals with four stars had 12% lower adjusted odds of new institutionalization and five stars 25% lower odds. To further explore the association between quality and new institutionalization, we repeated analyses using the HCAHPS “Overall Rating of Hospital” item. These analyses included 4,492,233 discharges across 3,032 hospitals. Adjusted odds of new institutionalization decreased as hospital rating increased. Compared to patients treated in hospitals with a rating of 0, ORs are as follows: 0.95 (95% CI: 0.92–0.99) for ratings 1–2, 0.91 (95% CI: 0.88–0.95) for ratings 3–4, 0.88 (95% CI: 0.84–0.92) for ratings 5–6, 0.80 (95% CI: 0.75–0.85) for ratings 7–8, and 0.62 (95% CI: 0.57–0.67) for ratings 9–10.
Discussion
Improving care and reducing costs are the goals of current healthcare reforms.43 CMS is at the forefront of these reforms and has implemented several initiatives to “transform Medicare from a passive payer of claims to an active purchaser of quality healthcare for its beneficiaries”.44 CMS is transitioning to quality metrics predominantly focused on patient experiences and outcomes.44 Institutionalization is an undesirable outcome of hospitalization3,41 associated with poorer patient experiences and increased healthcare costs,45 supporting its value as a potential quality indicator. Our findings further support its value. We examined new institutionalizations in a national cohort of hospital discharges and observed a significant variation in rates among hospitals.
In our cohort, patients discharged from hospitals with higher HCAHPS Summary Star Ratings or Overall Rating of Hospital scores had lower adjusted odds of a new institutionalization. Compared to quality metrics based on processes of care, the HCAHPS survey captures patient experiences.32 The association between number of stars and post-discharge outcomes is similar to findings from a study by Wang, et al.30 We observed an association between the number of stars and odds of institutionalization, and they observed an association between number of stars and rates of mortality and hospital readmissions.30
Recovery from an illness or injury often does not end at hospital discharge, resulting in complex trajectories of continued care. A few examples of these trajectories include discharge to a SNF and then the community; discharge to a SNF with a transition to long term care; and discharge to the community with a hospital readmission and eventual long term care residence. Complex trajectories are also observed with established quality metrics, such as 30-day readmissions and mortality. Like other quality measures, the variation in rates of new institutionalizations suggests the potential for improvement. Although the variation attributable to the hospital is only 5.1%, this value is higher than the approximately 2% variation attributable to hospitals in 30-day readmission rates.46–48
Why do some hospitals have lower rates of new institutionalizations following discharge? A plausible hypothesis is that some hospitals better prevent the functional loss16,19,20 that contributes to risk of future institutionalization.2,3 Given the relationship between hospital-associated functional decline and future institutionalization, prevention of functional decline among hospitalized older adults appears to be a clear target for care improvement.2,3,12,13 Implementing standardized functional assessments in the hospital setting would allow providers to better monitor this outcome and facilitate discharge planning. Improving care transitions is a goal of healthcare reforms.43,49 Incentivizing providers to reduce rates of future institutionalization may encourage greater coordination across care transitions, as well as better discharge and follow-up care.
Limitations
There are limitations associated with our outcome. First, we defined institutionalization as residence in a long term care nursing home for a minimum of 90 days. A standardized definition of institutionalization has not been established. However, this length of stay is representative of a fairly permanent placement.23 It should also be noted that not all institutionalizations represent a “bad” outcome. Long term care will be the most appropriate living setting for some individuals. Additionally, as with 30-day readmissions, some institutionalizations occurring within six months of discharge will be unrelated to the prior hospitalization.
Another limitation is that we do not account for post-hospital care trajectories. New institutionalizations will be preceded by varying degrees of healthcare utilization, including SNF stays and hospital readmissions. Future research is needed examining these complex pathways. However, an important first step is determining that rates vary at the hospital-level.
A final consideration is the generalizability of our findings. Our study examined a cohort of Medicare fee-for-service beneficiaries with continuous enrollment over the study period. Findings may not apply to patients who are younger than 66 years or have a different payer source.
Conclusions
Preventing future institutionalization is a priority at the individual and societal levels. Hospitalizations may be a critical period for preventing the trajectory of functional decline leading to this undesirable outcome. Ninety-day long term care residence starting within six months of hospital discharge could be a potentially valuable quality measure. The metric can be obtained with existing data, accurately reported, and represents an outcome important to patients and their families. The variation in rates among hospitals and the association with hospital quality ratings suggest some of these new institutionalizations are avoidable. Future research is needed to examine the hospital processes that best prevent new institutionalizations among older patients.
Supplementary Material
New institutionalizations by patients’ comorbidities and hospital diagnostic group
Acknowledgments
FUNDING SOURCES:
The study was supported by the National Institutes of Health (R01 AG33134; K05 CA134923; R01 HD069443; K12 HD055929; and P30 AG024832) and the Agency for Healthcare Research and Quality (R24 HS22134).
Conflict of Interest
The authors have no financial or personal conflicts of interest to disclose.
Author Contributions
Study concept and design: All authors. Acquisition of data: Goodwin. Analysis and interpretation of data: All authors. Preparation of the manuscript: Middleton. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Zhou. Obtained funding: Goodwin. Study supervision: Goodwin.
Sponsor’s Role
The study was supported by the National Institutes of Health (R01 AG33134; K05 CA134923; R01 HD069443; K12 HD055929; and P30 AG024832) and the Agency for Healthcare Research and Quality (R24 HS22134). The funding organizations had no role in the design of the study; the collection, management, analysis, and interpretation of the data; or the preparation of the manuscript.
References
- 1.Covinsky KE, Palmer RM, Fortinsky RH, et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc. 2003;51:451–8. doi: 10.1046/j.1532-5415.2003.51152.x. [DOI] [PubMed] [Google Scholar]
- 2.Gill TM, Allore HG, Holford TR, et al. Hospitalization, restricted activity, and the development of disability among older persons. JAMA. 2004;292:2115–24. doi: 10.1001/jama.292.17.2115. [DOI] [PubMed] [Google Scholar]
- 3.Goodwin JS, Howrey B, Zhang DD, et al. Risk of continued institutionalization after hospitalization in older adults. J Gerontol A Biol Sci Med Sci. 2011;66:1321–7. doi: 10.1093/gerona/glr171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sourdet S, Lafont C, Rolland Y, et al. Preventable Iatrogenic Disability in Elderly Patients During Hospitalization. J Am Med Dir Assoc. 2015;16:674–81. doi: 10.1016/j.jamda.2015.03.011. [DOI] [PubMed] [Google Scholar]
- 5.Brown CJ, Redden DT, Flood KL, et al. The underrecognized epidemic of low mobility during hospitalization of older adults. J Am Geriatr Soc. 2009;57:1660–5. doi: 10.1111/j.1532-5415.2009.02393.x. [DOI] [PubMed] [Google Scholar]
- 6.Pedersen MM, Bodilsen AC, Petersen J, et al. Twenty-four-hour mobility during acute hospitalization in older medical patients. J Gerontol A Biol Sci Med Sci. 2013;68:331–7. doi: 10.1093/gerona/gls165. [DOI] [PubMed] [Google Scholar]
- 7.Covinsky KE, Pierluissi E, Johnston CB. Hospitalization-associated disability: “She was probably able to ambulate, but I’m not sure”. JAMA. 2011;306:1782–93. doi: 10.1001/jama.2011.1556. [DOI] [PubMed] [Google Scholar]
- 8.Coker RH, Hays NP, Williams RH, et al. Bed rest promotes reductions in walking speed, functional parameters, and aerobic fitness in older, healthy adults. J Gerontol A Biol Sci Med Sci. 2015;70:91–6. doi: 10.1093/gerona/glu123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kortebein P, Ferrando A, Lombeida J, et al. Effect of 10 days of bed rest on skeletal muscle in healthy older adults. JAMA. 2007;297:1772–4. doi: 10.1001/jama.297.16.1772-b. [DOI] [PubMed] [Google Scholar]
- 10.Gill TM, Allore HG, Gahbauer EA, et al. Change in disability after hospitalization or restricted activity in older persons. JAMA. 2010;304:1919–28. doi: 10.1001/jama.2010.1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zisberg A, Shadmi E, Gur-Yaish N, et al. Hospital-associated functional decline: the role of hospitalization processes beyond individual risk factors. J Am Geriatr Soc. 2015;63:55–62. doi: 10.1111/jgs.13193. [DOI] [PubMed] [Google Scholar]
- 12.Helvik AS, Selbaek G, Engedal K. Functional decline in older adults one year after hospitalization. Arch Gerontol Geriatr. 2013;57:305–10. doi: 10.1016/j.archger.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 13.Fortinsky RH, Covinsky KE, Palmer RM, et al. Effects of functional status changes before and during hospitalization on nursing home admission of older adults. J Gerontol A Biol Sci Med Sci. 1999;54:M521–6. doi: 10.1093/gerona/54.10.m521. [DOI] [PubMed] [Google Scholar]
- 14.Gill TM, Allore HG, Gahbauer EA, et al. The role of intervening illnesses and injuries in prolonging the disabling process. J Am Geriatr Soc. 2015;63:447–52. doi: 10.1111/jgs.13319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Landefeld CS, Palmer RM, Kresevic DM, et al. A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients. N Engl J Med. 1995;332:1338–44. doi: 10.1056/NEJM199505183322006. [DOI] [PubMed] [Google Scholar]
- 16.Baztan JJ, Suarez-Garcia FM, Lopez-Arrieta J, et al. Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta-analysis. BMJ. 2009;338:b50. doi: 10.1136/bmj.b50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Inouye SK, Bogardus ST, Jr, Baker DI, et al. The Hospital Elder Life Program: a model of care to prevent cognitive and functional decline in older hospitalized patients. Hospital Elder Life Program. J Am Geriatr Soc. 2000;48:1697–706. doi: 10.1111/j.1532-5415.2000.tb03885.x. [DOI] [PubMed] [Google Scholar]
- 18.Capezuti EA, Bricoli B, Boltz MP. Nurses Improving the Care of Healthsystem Elders: creating a sustainable business model to improve care of hospitalized older adults. J Am Geriatr Soc. 2013;61:1387–93. doi: 10.1111/jgs.12324. [DOI] [PubMed] [Google Scholar]
- 19.Fox MT, Persaud M, Maimets I, et al. Effectiveness of acute geriatric unit care using acute care for elders components: a systematic review and meta-analysis. J Am Geriatr Soc. 2012;60:2237–45. doi: 10.1111/jgs.12028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Craen K, Braes T, Wellens N, et al. The effectiveness of inpatient geriatric evaluation and management units: a systematic review and meta-analysis. J Am Geriatr Soc. 2010;58:83–92. doi: 10.1111/j.1532-5415.2009.02621.x. [DOI] [PubMed] [Google Scholar]
- 21.Boyd CM, Landefeld CS, Counsell SR, et al. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. J Am Geriatr Soc. 2008;56:2171–9. doi: 10.1111/j.1532-5415.2008.02023.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Department of Health and Human Services. Centers for Medicare & Medicaid Services. Federal Register. Final Rule. 2015. Medicare Program; Prospective Payment System and Consolidated Billing for Skilled Nursing Facilities (SNFs) for FY 2016, SNF Value-Based Purchasing Program, SNF Quality Reporting Program, and Staffing Data Collection. [PubMed] [Google Scholar]
- 23.Gassoumis ZD, Fike KT, Rahman AN, et al. Who transitions to the community from nursing homes? Comparing patterns and predictors for short-stay and long-stay residents. Home Health Care Serv Q. 2013;32:75–91. doi: 10.1080/01621424.2013.779353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Medicare & Medicaid Services. [Accessed September 8, 2016];2013 Provider of Services Current Files (POS) Available at: https://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/Provider-of-Services/
- 25.Centers for Medicare & Medicaid Services. [Accessed May 23, 2016];Hospital Compare data archive. Available at https://data.medicare.gov/data/archives/hospital-compare.
- 26.United States Census Bureau. [Accessed May 23, 2016];American FactFinder. Available at: http://factfinder.census.gov/faces/nav/jsf/pages/index.xhtml.
- 27.Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Centers for Medicare & Medicaid Services. [Accessed July 15, 2016];Hospital Compare. Available at: https://www.medicare.gov/hospitalcompare/search.html.
- 29.Centers for Medicare & Medicaid Services. [Accessed August 11, 2016];Survey of patients’ experiences (HCAHPS) star ratings. Available at: https://www.medicare.gov/hospitalcompare/Data/HCAHPS-Star-Ratings.html.
- 30.Wang DE, Tsugawa Y, Figueroa JF, et al. Association Between the Centers for Medicare and Medicaid Services Hospital Star Rating and Patient Outcomes. JAMA Intern Med. 2016;176:848–50. doi: 10.1001/jamainternmed.2016.0784. [DOI] [PubMed] [Google Scholar]
- 31.Centers for Medicare & Medicaid Services. [Accessed August 11, 2016];Hospital Compare Overall Rating. Available at: https://www.medicare.gov/hospitalcompare/About/Hospital-overall-ratings.html.
- 32. [Accessed May 23, 2016];HCAHPS Survey. Available at: http://www.hcahpsonline.org/files/March%202016_Survey%20Instruments_English_Mail.pdf.
- 33.Tefera L, Lehrman WG, Conway P. Measurement of the Patient Experience: Clarifying Facts, Myths, and Approaches. JAMA. 2016;315:2167–8. doi: 10.1001/jama.2016.1652. [DOI] [PubMed] [Google Scholar]
- 34.Department of Health and Human Services. Final Rule. Federal Register: Medicare Program; Inpatient Rehabilitation Facility Prospective Payment System for Federal Fiscal Year 2016. [PubMed] [Google Scholar]
- 35.Department of Health and Human Services. Medicare Program; Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the Long-Term Care Hospital Prospective Payment System and Fiscal Year 2015 Rates; Quality Reporting Requirements for Specific Providers; Reasonable Compensation Equivalents for Physician Services in Excluded Hospitals and Certain Teaching Hospitals; Provider Administrative Appeals and Judicial Review; Enforcement Provisions for Organ Transplant Centers; and Electronic Health Record (EHR) Incentive Program; Final Rule 2014.
- 36.Intrator O, Hiris J, Berg K, et al. The residential history file: studying nursing home residents’ long-term care histories(*) Health Serv Res. 2011;46:120–37. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Acumen LLC. Draft Specifications for the Medicare Spending Per Beneficiary-Post-Acute Care (MSPB-PAC) Resource Use Measures, Provided for Public Comment. Jan, 2016. [Google Scholar]
- 38.Eiken S, Sredl K, Burwell B, et al. [Accessed June 2, 2016];Medicaid Expenditure for Long-Term Services and Supports (LTSS) in FY 2014: Managed LTSS Reached 15 Percent of LTSS Spending. Available at: https://www.medicaid.gov/medicaid-chip-program-information/by-topics/long-term-services-and-supports/downloads/ltss-expenditures-2014.pdf.
- 39.Department of Health and Human Services. [Accessed September 14, 2016];Nursing Home Data Compendium 2015 Edition. Available at: https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/CertificationandComplianc/Downloads/nursinghomedatacompendium_508-2015.pdf.
- 40.Tom S, Roel B, editors. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. 2. Taylor & Francis Group, LLC; 2012. [Google Scholar]
- 41.Thomeer MB, Mudrazija S, Angel JL. How do race and Hispanic ethnicity affect nursing home admission? Evidence from the Health and Retirement Study. J Gerontol B Psychol Sci Soc Sci. 2015;70:628–38. doi: 10.1093/geronb/gbu114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gaugler JE, Duval S, Anderson KA, et al. Predicting nursing home admission in the U. S: a meta-analysis. BMC Geriatr. 2007;7:13. doi: 10.1186/1471-2318-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Burwell SM. Setting value-based payment goals--HHS efforts to improve U.S. health care. N Engl J Med. 2015;372:897–9. doi: 10.1056/NEJMp1500445. [DOI] [PubMed] [Google Scholar]
- 44.Department of Health and Human Services. Centers for Medicare & Medicaid Services. Final Rule. 2011. Federal Register. Medicare Program; Hospital Inpatient Value-Based Purchasing Program. [PubMed] [Google Scholar]
- 45.Feder J, Komisar HL, Niefeld M. Long-term care in the United States: an overview. Health Aff (Millwood) 2000;19:40–56. doi: 10.1377/hlthaff.19.3.40. [DOI] [PubMed] [Google Scholar]
- 46.Singh S, Lin YL, Kuo YF, et al. Variation in the risk of readmission among hospitals: the relative contribution of patient, hospital and inpatient provider characteristics. J Gen Intern Med. 2014;29:572–8. doi: 10.1007/s11606-013-2723-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Krumholz HM, Merrill AR, Schone EM, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circ Cardiovasc Qual Outcomes. 2009;2:407–13. doi: 10.1161/CIRCOUTCOMES.109.883256. [DOI] [PubMed] [Google Scholar]
- 48.Chin DL, Bang H, Manickam RN, et al. Rethinking Thirty-Day Hospital Readmissions: Shorter Intervals Might Be Better Indicators Of Quality Of Care. Health Aff (Millwood) 2016;35:1867–75. doi: 10.1377/hlthaff.2016.0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Anderson GF, Davis K, Guterman S. Issue Brief. The Commonwealth Fund; 2015. [Accessed August 5, 2016]. Medicare Payment Reform: Aligning Incentives for Better Care. Available at: http://www.commonwealthfund.org/~/media/files/publications/issue-brief/2015/jun/1826andersonmedicarepaymentreformaligningincentivesmcare50ibv3.pdf. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
New institutionalizations by patients’ comorbidities and hospital diagnostic group


