Abstract
AIM
To investigate the effectiveness of a two-stage surgical procedure for the treatment of septic forearm non-union.
METHODS
Septic non-unions are rare complications of forearm fractures. When they occur, they modify the relationship between forearm bones leading to a severe functional impairment. Treatment is challenging and surgery and antibiotic therapy are required to achieve infection resolution. It is even harder to obtain non-union healing with good functional results. The aim of this study is to present a two stages surgical treatment for septic forearm non-union with revision and temporary stabilization of the non-union until infection has cleared and subsequently perform a new synthesis with plate, opposite bone graft strut and intercalary graft. We retrospectively reviewed 18 patients with a mean age at the time of primary injury of 34.5 years (19-57 years) and a mean follow-up of 6 years (2-10 years). All patients presented an atrophic non-union with a mean length of the bone defect of 1.8 cm (1.2-4 cm). Complications and clinical results after surgical treatment were recorded.
RESULTS
Mean time to resolution of the infectious process was 8.2 wk (range 4-20 wk) after the first surgery and specific antibiotic therapy. All the non-union healed with an average time of 5 mo (range 2-10 mo) after the second step surgery. Cultures on intraoperative samples were positive in all cases. No major intraoperative complications occurred. Two patients developed minor complications and one needed a second surgical debridement for infection resolution. At the last follow-up functional results were excellent in 5 (27.8%) patients, satisfactory in 10 (55.5%) and unsatisfactory in 3 (16.7%) patients. No activities of daily living (ADLs) limitations were reported by 12 (66.6%) patients, slight by 3 (16.6%) and severe limitation by 3 (16.6%) patients. Mean visual analog scale at the last follow-up was 1 (0-3).
CONCLUSION
The two-step technique has proven to be effective to achieve resolution of the infectious process and union with good functional results and low rate of complications.
Keywords: Forearm fractures, Non-union, Delayed union, Infection, Open fracture, External fixation, Bone graft
Core tip: Forearm non-union represent a challenging condition for the orthopaedic surgeon. Septic forms are even more difficult to overcome. However, in the present study we found that good clinical results can be achieved using a dual stage surgical technique with the first aim to resolve the infection process and subsequently achieve bone union.
INTRODUCTION
Septic non-union are defined as the absence of evidence of fracture healing and persistence of infection at the fracture site for 6 to 8 mo[1,2]. Current fixation techniques in forearm fractures with the application of the AO principles have proven to be quite effective to achieve healing with a reported non-union rate below 5%[3-6], and infection rate following open reduction and internal fixation (ORIF) for diaphyseal forearm fractures ranges between 2% and 6%[7-10].
Forearm non-unions generally occur as a consequence of inadequate initial reduction, unstable fixation or too early limb mobilization. Whereas in case of septic non-union multiple others factors like open injuries, significant soft tissue trauma, highly comminuted fractures, inadequate surgical fixation, patient characteristics and infection may be involved[7,11-13].
Forearm has the function to support and guide the hand movements through the pronation and the supination at the radio-humeral joint, and at the proximal and the distal radio-ulnar joints. A non-union of one or both the forearm bones modifies their relationships evolving towards proximal and/or distal joints impairment and forearm dysfunction. Furthermore, segmental bone defects in radius, ulna, or both may worsen functional impairment of the elbow and wrist with also difficulties in positioning the hand in space. Finally, a forearm non-union may compromise the strength in lifting objects and gripping.
Surgical treatment of septic forearm non-union may present many difficulties in addition to the well-known difficulties related to the treatment of bone infection, because of the poor bone quality resulting from the septic process, the bone necrosis and the scar adhesion of the soft tissue due to multiple previous surgeries[7,9]. Septic non-unions of the forearm are mostly atrophic non-unions, presenting both mechanical failure and severe biological impairment, and in these cases the bone gap and the bad trophic conditions make the surgical restoration of the shape and the function of the forearm even harder. Proper planning of the treatment should consider first to eradicate the infection, then to promote bone healing, restoring as much as possible bone length and shape, with the aim to restore a physiologic function of the upper limb, minimizing possible impairment of elbow and wrist range of motion, forearm pronation and supination and grip strength.
A series of patients affected by septic forearm non-union who underwent surgical treatment was retrospectively reviewed as part of this study with the aim of presenting a protocol for treatment of septic forearm non-union in two surgical steps: (1) revision of the non-union and temporary stabilization with external fixation, followed by antibiotic therapy until healing of the infection; and (2) new synthesis with plate and opposite bone graft strut, with interposition of intercalary bone graft to fill the bone gap. Results and complications at mid to long-term follow-up are reported.
MATERIALS AND METHODS
From January 2002 to December 2015 a total of 34 patients presenting septic forearm non-union were treated in our institution and retrospectively reviewed. Inclusion criteria of this study were: (1) patients with septic diaphyseal forearm non-union; (2) patients with a complete clinical and radiologic documentation of the whole treatment; and (3) patients with at least 2 years’ follow-up. Exclusion criteria were as follow: (1) presence of other fractures in the same limb at the time of the primary forearm injury; and (2) patients with neurological impairment on the same side of the non-union. Sixteen patients did not satisfy the inclusion criteria and were therefore excluded from the study. This left a total of 18 patients eligible for this retrospective review.
There were 15 men and 3 women with a mean age at the time of our observation and treatment of 34.5 years (range 19-57 years). The initial trauma was caused by road accident in 13 cases, injuries by machines in 4 and accidental fall in 1 case. The fracture involved the radius alone in 5 patients, the ulna alone in 11 patients and both the radius and the ulna in 2 patients.
The dominant limb was involved in 12 cases. An open fracture was present in 6 cases. The initial treatment consisted in ORIF with plate and screws in 10 patients, 3 of them presenting a Gustilo I open fracture treated within 24 h from the trauma, one of these treated with also intramedullary nailing (ulna) along with plate and screws (radius); fixation with intramedullary rod in 4 patients; external fixation in 3 patients and close reduction in 1 patient. Fourteen of the 18 patients underwent to further surgery after initial treatment, before our observation.
All patients were evaluated clinically in terms of pain and functional impairment, with blood tests including ESR and C-reaction protein (CRP), and with standard X-rays of the forearm in orthogonal projections. Septic non-union was considered on the basis of the absence of bone healing on radiographs after at least 6 mo from the initial treatment in presence of septic signs such as altered blood test with increase of white blood cell and/or ESR and/or CRP, presence of fistula or obvious soft tissue damage over the non-union site, positive specimens available from previous surgery. All patients presented an atrophic non-union with a mean length of the bone defect of 1.8 cm (range 1.2-4 cm) measured on radiographs.
The performed surgical treatment included two stages. The initial treatment consisted in the removal of the fixation devices, debridement and freshening of the non-union site removing fibrous and necrotic tissue in order to obtain healthy bone ends. The scar of the previous surgery was used to perform the skin incision when possible. Otherwise radius exposure was performed through dorsal Thompson approach, while ulna was exposed through direct posterior approach. The medullary canal of the bones was opened to allow good blood supply to the non-union site. Segmental bone defect up to 3 cm after the debridement were left free; conversely, in cases of bone loss greater than 3 cm and large infectious outbreak, a gentamicin-loaded cement spacer was applied. Samples of infected tissue from the wound, the bone and the deep soft tissue adjacent the non-union were cultured and bone specimens were sent to the pathology for analysis. New synthesis with mono-axial external fixator was performed in order to keep the length of the bone segment and the shape and the function of the forearm.
A targeted antibiotic therapy based on the culture performed on intraoperative samples was set, each patients received a specific antibiotic therapy according to the sensibility of the culture to the antibiotic therapy. Dosage, duration and any drug changes were discussed and decided by our infectious diseases consultant considering the patient’s comorbidities, liver and kidney function and response to therapy. Monthly, all patients were evaluated clinically, radiographically and with blood tests, these repeated every two weeks. When normal values of ESR and CRP were observed, antibiotic therapy was interrupted and after 4-6 wk without antibiotic therapy, if ESR and CRP were still normal, and there weren’t clinical signs of infection, resolution of the infection was considered.
The second surgical stage consisted into removal of the external fixator and new synthesis with plate and opposite homologous bone graft strut with intercalary graft inserted between the bone ends to restore proper bone length. Intraoperative specimens from the surgical site were taken again and cultured to further confirm the resolution of the infection. Segmental bone defects were quantified and length of the bones were measured using the image intensifier according to Szabo and Weber[14]. The mean length of the intercalary graft was 2.3 cm (range 1.5-5 cm). In case of both bone non-union, fixation of the ulna was performed first in order to properly restore length and alignment of the forearm[15]. No antibiotic therapy was performed after the second surgical stage because all the patients were considered cured from infection. Standard prophylaxis at anaesthetic induction was performed according to the guideline of our hospital.
A long-arm cast with elbow 90° flexed and forearm in intermediate rotation was applied after surgery and maintained for 3 wk. Subsequently an articulate elbow brace was applied for another 3 wk allowing flexion-extension of the elbow and physiotherapy was prescribed. Patients were checked monthly until there was radiographic evidence of bone healing, and thereafter, yearly for a mean postoperative follow-up of 6 years (range 2-10 years).
A combined clinical and radiographic evaluation was used to assess the healing of the non-union. Clinical parameters of healing were: (1) absence of pain or tenderness on palpation; (2) painless grip strength recovery; and (3) painless recovery of elbow and wrist range of motion. Whereas radiographic criteria were: (1) bridging of the non-union seen at three cortices; and (2) obliteration of the non-union line or cortical continuity.
The forearm, elbow and wrist flexion, extension, supination, and pronation were assessed using the Anderson system which classifies results as excellent, satisfactory and unsatisfactory. Excellent result was considered in case of united fracture with loss of less than 10° of elbow or wrist flexion-extension or less than 25% of forearm pronation-supination; satisfactory result was considered in case of healed fracture with loss of less than 20° of elbow or wrist flexion-extension or less than 50% of forearm pronation-supination; unsatisfactory was considered in case of healed fracture with a loss greater than 20° of elbow or wrist flexion-extension or greater than 50% of forearm pronation-supination whereas persistent non-union or malunion was considered a failure[3].
The return to activities of daily living (ADLs) and to job was evaluated in terms of time to return and possible limitation (no limitation, slight and severe limitation). Visual analog scale (VAS) was used to evaluate any residual pain.
RESULTS
The average follow-up was 6 years (range 2-10 years). At the last follow-up all non-unions healed with evidence of graft integration and bone remodelling (Figure 1).
Figure 1.
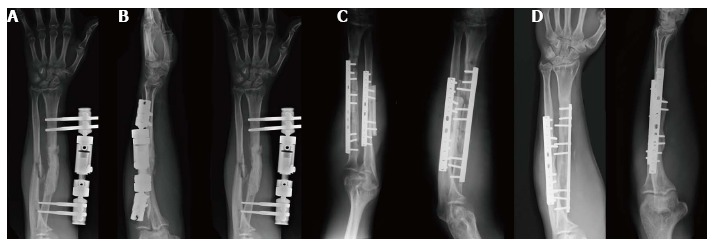
Radiographic aspect of a both radius and ulna non-union in a 25-year-old man. A: Occurred after a Gustilo I open fracture undergone open reduction and internal fixation by plate and screws and intramedullary nailing; B: Once a septic non-union was diagnosed, removal of fixation devices and surgical debridement were performed and an external fixator was applied; C: Eight weeks after the surgical toilette the infection has resolved and thus new synthesis with plate, opposite strut and intercalary bone graft was performed; D: At follow-up both non-unions appear healed with noticeable remodelling of the bone graft.
Cultures on intra-operative samples (harvested during the first surgery) were positive in all patients finding S. aureus in 9 patients, S. epidermidis in 4 patients, P. aeruginosa in 2 patients, both S. aureus and P. aeruginosa in one patient, both S. aureus and P. acnes in one patient and both S. hominis and K. pneumoniae in one patient. The mean time to resolution of the infectious process was 8.2 wk (range 4-20 wk) after the first surgery and specific antibiotic therapy. Average time of healing of the non-union was 5 mo (range 2-10 mo) after the second surgery (Table 1).
Table 1.
Patient and fracture data and treatment
| Patient | Age (yr) | Bones involved | Open/ closed | Initial treatment | Speciments | Time to infection resolution (wk) | Bone defect and intercalary graft size (cm) | Time to healing (mo) |
| 1 | 27 | Radius | Closed | Intramedullary rod | S. epidermidis | 6 | 2.2 | 5 |
| 2 | 31 | Ulna | Open | ORIF | S. aureus | 4 | 1.8 | 4 |
| 3 | 41 | Radius | Closed | ORIF | S. aureus | 6 | 1.5 | 2 |
| 4 | 24 | Ulna | Closed | ORIF | S. hominis + K. pneumoniae | 8 | 2.0 | 4 |
| 5 | 19 | Ulna | Closed | Intramedullary rod | S. epidermidis | 6 | 1.8 | 3 |
| 6 | 42 | Ulna | Closed | ORIF | P. aeruginosa | 8 | 2.0 | 6 |
| 7 | 39 | Ulna | Open | ORIF | S. aureus | 6 | 1.6 | 3 |
| 8 | 34 | Radius | Closed | ORIF | S. aureus1 + P. aeruginosa | 20 | 2.2 | 4 |
| 9 | 45 | Ulna | Closed | Intramedullary rod | S. aureus | 8 | 1.7 | 3 |
| 10 | 25 | Radius + Ulna | Open | ORIF + intram. rod | S. aureus + P. acnes | 8 | 2.2 | 8 |
| 11 | 57 | Ulna | Open | External fixator | S. aureus | 10 | 4.0 | 7 |
| 12 | 38 | Ulna | Closed | ORIF | S. epidermidis | 6 | 1.8 | 4 |
| 13 | 20 | Radius + Ulna | Open | External fixator | S. aureus | 6 | 2.8 | 8 |
| 14 | 31 | Ulna | Closed | Close reduction | S. aureus | 10 | 2.0 | 4 |
| 15 | 52 | Radius | Closed | ORIF | S. aureus | 12 | 2.5 | 5 |
| 16 | 40 | Ulna | Open | External fixator | S. epidermidis | 6 | 5.0 | 10 |
| 17 | 22 | Ulna | Closed | Intramedullary rod | S. aureus | 6 | 1.8 | 4 |
| 18 | 34 | Radius | Closed | ORIF | P. aeruginosa | 12 | 2.5 | 6 |
Bacterial resistant strain, second debridement performed. ORIF: Open reduction and internal fixation.
No major intraoperative complications occurred. In three patients skin wound healed by secondary intention and one of them required a skin graft. One patient suffered an incomplete transient palsy of posterior interosseous nerve that completely resolved 6 mo after surgery. One patient developed radio-ulnar impingement with prono-supination impairment and underwent further removal of the hardware with functional improvement. After first surgery one patient needed a second surgical debridement and to change the antibiotic therapy due to resumption of infection seen clinically and through blood tests.
At the last follow-up forearm functional results according to the Anderson scale were excellent in 5 (27.8%) patients, satisfactory in 10 (55.5%) and unsatisfactory in 3 patients (16.7%), no failures were recorded. Patients resumed ADLs at a mean of 3 mo after surgery. No limitations were reported by 12 (66.6%) patients, slight limitation by 3 (16.6%) and severe by 3 (16.6%). The original work activity was resumed at a mean of 5 mo after surgery, without limitations in 9 (50%) cases, slight limitation in 6 (33.3%), and with severe limitation that required to change the type of activity in 3 cases (16.6%). At the last available follow-up mean value of pain according to VAS was 1 (range 0-3) (Table 2).
Table 2.
Results
| Patient | Age (yr) | Follow-up (yr) | Anderson | ADLs limitations | Job limitations | VAS |
| 1 | 27 | 6 | Excellent | No | No | 0 |
| 2 | 31 | 4 | Satisfactory | No | No | 0 |
| 3 | 41 | 8 | Satisfactory | No | No | 0 |
| 4 | 24 | 3 | Satisfactory | Slight | Slight | 1 |
| 5 | 19 | 10 | Satisfactory | No | No | 0 |
| 6 | 42 | 4 | Satisfactory | Slight | Slight | 2 |
| 7 | 39 | 10 | Satisfactory | No | Slight | 1 |
| 8 | 34 | 8 | Excellent | No | No | 0 |
| 9 | 45 | 4 | Excellent | No | No | 0 |
| 10 | 25 | 6 | Satisfactory | No | Slight | 2 |
| 11 | 57 | 4 | Unsatisfactory | Severe | Severe | 2 |
| 12 | 38 | 5 | Excellent | No | No | 0 |
| 13 | 20 | 8 | Satisfactory | Slight | Slight | 2 |
| 14 | 31 | 8 | Satisfactory | No | No | 0 |
| 15 | 52 | 2 | Unsatisfactory | Severe | Severe | 3 |
| 16 | 40 | 4 | Unsatisfactory | Severe | Severe | 3 |
| 17 | 22 | 6 | Excellent | No | No | 0 |
| 18 | 34 | 8 | Satisfactory | No | Slight | 1 |
VAS: Visual analog scale.
DISCUSSION
In this study a two-step protocol for surgical treatment of septic forearm non-unions is presented including: (1) extensive surgical debridement of the non-union and temporary external fixation followed by targeted antibiotic therapy; and (2) new synthesis of the non-union with plate and screws, opposite homologous bone graft strut and intercalary allograft after the healing of infection. This technique allowed to achieve good radiographic and clinical outcome, healing of all non-unions with 83.3% of excellent and satisfactory results, and low rate of complications.
The treatment of septic forearm non-unions must consider first the resolution of the infectious process and then the achievement of the fracture union providing a proper reconstruction of the fractured bones and hence adequate function of the forearm. Septic forearm non-unions are mainly atrophic with severe biologic impairment of the bone and the soft tissues. Commonly there may be a various amount of bone gap characterized by scarring, bone sclerosis and absorption, and poor blood supply. All these problems make more challenging to achieve bone healing and good clinical outcomes. Various surgical options are reported in the literature for the treatment of aseptic forearm non-unions[6,7,9,11-13], but there is paucity of studies concerning the treatment of the septic ones. Baldy dos Reis et al[16] using autologous bone graft and compression plate reported a high rate of good functional results (29 cases out of 31), but their study included mixed cohorts of patients with both septic and aseptic non-unions and a direct comparison with our study is difficult. In a retrospective review of 35 patients presenting forearm non-unions, 11 septic, Ring et al[9] reported a success rate of 100% using plate fixation and autologous cancellous bone-grafting, recovering a mean bone defect of 2.2 cm. The results reported by Ring et al[9] limited to the 11 septic non-unions seem to confirm the results presented in this paper with a 100% of union rate, however Ring et al[9] study lacks of an adequate description of the surgical procedure and of the treatment of the infection. Similar results are reported by Prasarn et al[7] in a retrospective analysis of 15 infected forearm non-unions. Prasarn et al[7] achieved union in all patients using a two-stage surgical procedure with extensive debridement followed by plate and screws fixation with autologous iliac crest bone graft. Differently to the protocol detailed in this paper, Prasarn et al[7] repeated surgical debridement every 48-72 h: It’s the authors’ opinion that this procedure could be considered hard and painful to bear for the patient and expensive in terms of overall cost of the whole treatment. Furthermore, Prasarn et al[7] used an autologous iliac crest bone grafting that presents high morbidity on the donor site and it increases the surgical time. It’s the authors’ belief that the homologous bone graft may present more advantages than the autologous one, mainly consisting in: (1) short surgical time; (2) possibility to customize the graft according to the patient’s characteristics; and (3) neglectable differences in terms of osteoinductive and osteoconductive properties compared to autologous bone graft[6,17]. Furthermore, a cortical strut graft may provide additional stability than a metal plate alone, and thus improvement of the non-union healing may be postulated. Moreover, a stable fixation usually allows earlier recovery of active motion of the limb.
One of the limit of the present study is related to the supposed risk of disease transmission with homologous graft, but bacterial infection due to contaminated bone have been rarely reported in literature with an overall risk similar to other major orthopaedic procedures[17]. It’s the authors’ opinion that the biomechanic advantages related to the homologous graft are greater than its estimated risk of disease transmission, even if the authors are also aware that a case-control study would be necessary to establish the real advantages from an autologous graft rather than a homologous. Another limit of this study is related to the relatively small average length of the bone defect of 2.2 cm, so the authors are not able to determine if our protocol could bring the same good results also in case of massive bone defect. In these cases the use of vascularized fibular graft has been described with successfully results[18-21], reporting though major disadvantages related to the risk of infection and thrombosis of the graft vessels[22], technical difficulties of the procedure and comorbidity on the donor site[23]. Recently Zhang et al[24] retrospectively analysed the results of a series of 16 patients affected by septic forearm non-union treated with external fixation and bone transport. The union in all patients was achieved with average good clinical results, nevertheless this technique requires high patient’s compliance due to the demanding and long treatment and moreover some concerns about the effectiveness of this treatment may still be raised when it is applied on likely avascular post-infected tissue[18-20]. Others limitations of this study are mainly related to be retrospective, to the relatively small number of patients, the non-homogeneous series and the absence of a control group.
In the authors’ experience some technical precautions must be respected. First, placing the plate and the opposite graft too close to the interosseous membrane must be avoided in order to prevent impingement between radius and ulna and prono-supination impairment. Second, care should be taken to ensure adequate coverage of the bone and the graft by muscles with the aim to enhance blood supply and surgical wound healing. Third, adequate extensive debridement should be performed in order to expose healthy bone ends and to promote biological stimulation. Finally, the new synthesis must be performed only after complete resolution of the infection, documented by clinic and radiographic signs and blood tests.
Septic forearm non-unions are rare and challenging to treat. The infection represents an obstacle to the healing process that frequently requires prolonged treatment, deferred therapeutic interventions and good patient’s compliance.
The two steps technique for the treatment of septic forearm non-unions based on revision of the non-union and temporary stabilization with external fixation, targeted antibiotic therapy and finally new synthesis with plate and homologous bone graft has proven to be effective in achieving union. Good clinical results have been obtained in the majority of cases with low rate of significant complications. Despite the unsatisfactory functional results in 16.7% of the patients according to the Anderson scale, the study presented in this paper obtained resolution of the infectious process and healing of the non-unions in all cases. Accurate debridement and postoperative targeted antibiotic therapy are mandatory to eradicate the infection and thus to allow bone healing. The synthesis with plate and opposite bone graft strut, with intercalary graft, can ensure both stability and biological enhancement so as to promote healing of the non-union and restore good function of the forearm. Despite the average good results of the present study, considering its aforementioned limitations, prospective randomized controlled trial would be desirable to better define the best strategy for treatment of septic forearm non-unions.
COMMENTS
Background
Septic non-union of the forearm represent a challenging condition because of the poor bone quality due to the septic process and the forearm function impairment. Septic non-unions of the forearm are mostly atrophic non-unions, presenting both mechanical failure and severe biological impairment, and in these cases the bone gap and the bad trophic conditions make the surgical restoration of the shape and the function of the forearm even harder. Only few reports are available in literature on this topic because of its infrequence.
Research frontiers
Aim of this study was to evaluate the effectiveness of a two-stage surgical procedure for the treatment of septic non-union of the forearm.
Innovations and breakthroughs
In this study, a two-step protocol for surgical treatment of septic forearm non-unions is presented including: (1) extensive surgical debridement of the non-union and temporary external fixation followed by targeted antibiotic therapy; and (2) new synthesis of the non-union with plate and screws, opposite homologous bone graft strut and intercalary allograft after the healing of infection. Good radiographic and clinical results have been recorded with an average follow-up of six years. Only limited studies are reported in literature on the same topic, moreover with various limitations such as: Groups heterogeneity and lack of information on the technique used. In the present study, we tried to focalize attention on a homogeneous group of patients and to carefully report the technique used exploring its advantages and disadvantages.
Applications
This study suggests a new surgical technique for septic forearm non-union treatment. Readers may use it as a stimulus to change their clinical practice or to assess new research frontiers.
Terminology
Septic non-union are defined as the absence of evidence of fracture healing and persistence of infection at the fracture site for 6 to 8 mo.
Peer-review
This is a well written paper.
Footnotes
Institutional review board statement: This study received the ethical approval from the institutional review board statement of the Rizzoli Orthopaedic Institute of Bologna (No. 0021967).
Informed consent statement: All patients involved in this study gave their written informed consent prior to study inclusion.
Conflict-of-interest statement: The authors declare no conflicts of interest.
Data sharing statement: Authors agreed to share data with the editor.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Peer-review started: February 5, 2017
First decision: March 28, 2017
Article in press: May 15, 2017
P- Reviewer: Cui Q, Emara KM S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
References
- 1.Meyer S, Weiland AJ, Willenegger H. The treatment of infected non-union of fractures of long bones. Study of sixty-four cases with a five to twenty-one-year follow-up. J Bone Joint Surg Am. 1975;57:836–842. [PubMed] [Google Scholar]
- 2.Struijs PA, Poolman RW, Bhandari M. Infected nonunion of the long bones. J Orthop Trauma. 2007;21:507–511. doi: 10.1097/BOT.0b013e31812e5578. [DOI] [PubMed] [Google Scholar]
- 3.Anderson LD. Treatment of ununited fractures of the long bones; compression plate fixation and the effect of different types of internal fixation on fracture healing. J Bone Joint Surg Am. 1965;47:191–208. [PubMed] [Google Scholar]
- 4.Chapman MW, Gordon JE, Zissimos AG. Compression-plate fixation of acute fractures of the diaphyses of the radius and ulna. J Bone Joint Surg Am. 1989;71:159–169. [PubMed] [Google Scholar]
- 5.Kloen P, Wiggers JK, Buijze GA. Treatment of diaphyseal non-unions of the ulna and radius. Arch Orthop Trauma Surg. 2010;130:1439–1445. doi: 10.1007/s00402-010-1071-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Faldini C, Traina F, Perna F, Borghi R, Nanni M, Chehrassan M. Surgical treatment of aseptic forearm nonunion with plate and opposite bone graft strut. Autograft or allograft? Int Orthop. 2015;39:1343–1349. doi: 10.1007/s00264-015-2718-6. [DOI] [PubMed] [Google Scholar]
- 7.Prasarn ML, Ouellette EA, Miller DR. Infected nonunions of diaphyseal fractures of the forearm. Arch Orthop Trauma Surg. 2010;130:867–873. doi: 10.1007/s00402-009-1016-4. [DOI] [PubMed] [Google Scholar]
- 8.Schemitsch EH, Richards RR. The effect of malunion on functional outcome after plate fixation of fractures of both bones of the forearm in adults. J Bone Joint Surg Am. 1992;74:1068–1078. [PubMed] [Google Scholar]
- 9.Ring D, Allende C, Jafarnia K, Allende BT, Jupiter JB. Ununited diaphyseal forearm fractures with segmental defects: plate fixation and autogenous cancellous bone-grafting. J Bone Joint Surg Am. 2004;86-A:2440–2445. [PubMed] [Google Scholar]
- 10.Stern PJ, Drury WJ. Complications of plate fixation of forearm fractures. Clin Orthop Relat Res. 1983:25–29. [PubMed] [Google Scholar]
- 11.Moroni A, Rollo G, Guzzardella M, Zinghi G. Surgical treatment of isolated forearm non-union with segmental bone loss. Injury. 1997;28:497–504. doi: 10.1016/s0020-1383(97)00044-2. [DOI] [PubMed] [Google Scholar]
- 12.Faldini C, Pagkrati S, Nanni M, Menachem S, Giannini S. Aseptic forearm nonunions treated by plate and opposite fibular autograft strut. Clin Orthop Relat Res. 2009;467:2125–2134. doi: 10.1007/s11999-009-0827-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Faldini C, Miscione MT, Acri F, Chehrassan M, Bonomo M, Giannini S. Use of homologous bone graft in the treatment of aseptic forearm nonunion. Musculoskelet Surg. 2011;95:31–35. doi: 10.1007/s12306-011-0117-8. [DOI] [PubMed] [Google Scholar]
- 14.Szabo RM, Weber SC. Comminuted intraarticular fractures of the distal radius. Clin Orthop Relat Res. 1988:39–48. [PubMed] [Google Scholar]
- 15.Bronstein AJ, Trumble TE, Tencer AF. The effects of distal radius fracture malalignment on forearm rotation: a cadaveric study. J Hand Surg Am. 1997;22:258–262. doi: 10.1016/S0363-5023(97)80160-8. [DOI] [PubMed] [Google Scholar]
- 16.dos Reis FB, Faloppa F, Fernandes HJ, Albertoni WM, Stahel PF. Outcome of diaphyseal forearm fracture-nonunions treated by autologous bone grafting and compression plating. Ann Surg Innov Res. 2009;3:5. doi: 10.1186/1750-1164-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stevenson S. Enhancement of fracture healing with autogenous and allogeneic bone grafts. Clin Orthop Relat Res. 1998:S239–S246. doi: 10.1097/00003086-199810001-00024. [DOI] [PubMed] [Google Scholar]
- 18.Safoury Y. Free vascularized fibula for the treatment of traumatic bone defects and nonunion of the forearm bones. J Hand Surg Br. 2005;30:67–72. doi: 10.1016/j.jhsb.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 19.Allieu Y, Meyer zu Reckendorf G, Chammas M, Gomis R. Congenital pseudarthrosis of both forearm bones: long-term results of two cases managed by free vascularized fibular graft. J Hand Surg Am. 1999;24:604–608. doi: 10.1053/jhsu.1999.0604. [DOI] [PubMed] [Google Scholar]
- 20.Dell PC, Sheppard JE. Vascularized bone grafts in the treatment of infected forearm nonunions. J Hand Surg Am. 1984;9:653–658. doi: 10.1016/s0363-5023(84)80006-4. [DOI] [PubMed] [Google Scholar]
- 21.Han CS, Wood MB, Bishop AT, Cooney WP. Vascularized bone transfer. J Bone Joint Surg Am. 1992;74:1441–1449. [PubMed] [Google Scholar]
- 22.Minami A, Kasashima T, Iwasaki N, Kato H, Kaneda K. Vascularised fibular grafts. An experience of 102 patients. J Bone Joint Surg Br. 2000;82:1022–1025. doi: 10.1302/0301-620x.82b7.10332. [DOI] [PubMed] [Google Scholar]
- 23.Gore DR, Gardner GM, Sepic SB, Mollinger LA, Murray MP. Function following partial fibulectomy. Clin Orthop Relat Res. 1987:206–210. [PubMed] [Google Scholar]
- 24.Zhang Q, Yin P, Hao M, Li J, Lv H, Li T, Zhang H, Wang G, Zhang L, Tang P. Bone transport for the treatment of infected forearm nonunion. Injury. 2014;45:1880–1884. doi: 10.1016/j.injury.2014.07.029. [DOI] [PubMed] [Google Scholar]


