Abstract
AIM
To review current literature on types of distal triceps injury and determine diagnosis and appropriate management.
METHODS
We performed a systematic review in PubMed, Cochrane and EMBASE using the terms distal triceps tears and snapping triceps on the 10th January 2017. We excluded all animal, review, foreign language and repeat papers. We reviewed all papers for relevance and of the papers left we were able to establish the types of distal triceps injury, how these injuries are diagnosed and investigated and the types of management of these injuries including surgical. The results are then presented in a review paper format.
RESULTS
Three hundred and seventy-nine papers were identified of which 65 were relevant to distal triceps injuries. After exclusion we had 47 appropriate papers. The papers highlighted 2 main distal triceps injuries: Distal triceps tears and snapping triceps. Triceps tear are more common in males than females occurring in the 4th-5th decade of life and often due to a direct trauma but are also strongly associated with weightlifting and American football. The tears are diagnosed by history and clinically with a palpable gap. Diagnosis can be confirmed with the use of ultrasound (US) and magnetic resonance imaging. Treatment depends on type of tear. Partial tears can be treated conservatively with bracing and physio whereas acute tears need repair either open or arthroscopic using suture anchor or bone tunnel techniques with similar success. Chronic tears often need augmenting with tendon allograft or autograft. Snapping triceps are also seen more in men than women but at a mean age of 32 years. They are characterized by a snapping sensation mostly medially and can be associated with ulna nerve subluxation and ulna nerve symptoms. US is the diagnostic modality of choice due to its dynamic nature and to differentiate between snapping triceps tendon or ulna nerve. Treatment is conservative initially with activity avoidance and if that fails surgical management includes resection of triceps edge or transposition of the tendon plus or minus ulna nerve transposition.
CONCLUSION
Distal triceps injuries are uncommon. This systematic review examines the evidence base behind diagnosis, imaging and treatment options of distal triceps injuries including tears and snapping triceps.
Keywords: Triceps, Distal, Tear, Rupture, Snapping, Partial thickness, Biomechanical, Anatomy
Core tip: The anatomy, demographics, associations and mechanisms of triceps injuries are presented from the evidence base in the literature. Partial thickness tears and snapping triceps can be difficult to diagnose and appropriate assessment and imaging is essential. The surgical management available in the literature is presented for these uncommon injuries.
INTRODUCTION
Triceps injuries are relatively rare in comparison to other tendons around the elbow and found to be present on 3.8% of elbow magnetic resonance imaging (MRI) studies following elbow injury[1]. Lateral and medial epicondylitis being the most commonly encountered pathology and distal biceps ruptures presenting more frequently[2]. However, triceps pathology can cause significant symptoms and due to its less common nature can cause problems with diagnosis and treatment. The aim of this study was to review all current literature and present the best evidence for the management of distal triceps injuries.
MATERIALS AND METHODS
A systematic review was conducted using three search strategies (distal [All Fields] AND triceps [All Fields] AND (“1996/12/31” [PDAT]: “2017/01/10” [PDAT]), (triceps [All Fields] AND tear [All Fields] AND (“1996/12/31” [PDAT]: “2017/01/10” [PDAT]) and (snapping [All Fields] AND triceps [All Fields] AND (“1996/12/31” [PDAT]: “2017/01/10” [PDAT]) in PubMed on January 10th 2017. EMBASE and Cochrane databases were also searched with the same strategy. Additional references were looked for in the citations of the selected studies.
Inclusion criteria
Clinical studies investigating distal triceps injuries in English.
Exclusion criteria
Review articles; studies in foreign languages; animal studies; double publication of data; letters to authors.
Forty-seven studies were eligible for review and a further three studies were found from citations within the selected studies (Figure 1).
Figure 1.
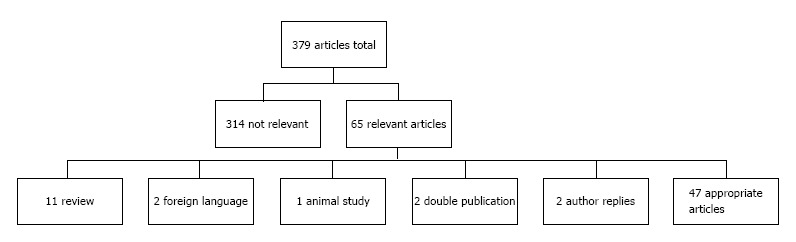
Flow diagram of systematic review process.
RESULTS
Appraisal of literature
All studies identified by the above search were case series and case reports. Inclusion criteria in the series was generally poorly described. Study number were small with the largest series being only 37 patients[3]. The tears were assessed by a number of modalities with no standard assessment utilised. Patient reported outcome measures were inconsistently used. As a consequence of this heterogeneity of patient groups, imaging and outcomes reported, reliable synthesis of data is not possible. As such the data is reported in a descriptive manner. Four distinct entities were identified. Acute tears, chronic tears, partial tears (either acute of chronic) and snapping triceps.
Anatomy
The triceps brachii is composed of three muscle bellies. The long head arises off the infraglenoid tubercle of the scapula, the medial head off the posterior aspect of the distal to the spiral groove and the lateral head off the lateral intermuscular septum and the posterolateral aspect of the humerus above the spiral groove. The triceps inserts as a bilaminate tendon over a wide area onto the tip of the olecranon. The average triceps width at its distal insertion, including the tendon and lateral expansion, has been reported as 40.6 mm[4]. With the tendon being a mean width of 30.6 mm and the distance from its medial edge to the ulna nerve at 10.2 mm[4]. Its footprint has a mean length of 22.5 mm and a width of 22.7 mm, giving the footprint an area of 466.2 mm2[4]. In around half of specimens a discrete tendinous portion of the medial triceps deep to the long and lateral head has been reported in cadaveric dissection, with the long and lateral portion forming a tendon superficial to it[5]. The mean dimensions of this medial head insertion were 16 mm × 4 mm, with a mean area of insertion of 44 mm2[5]. This study also demonstrated a second variant in the other half of specimens. This had a common combined tendon insertion, but still with the medial fibres deep to the long and lateral head.
Partial tears can be located on the superficial tendon only (combined lateral or long head)[6-8] but have also been described for the deep portion of the tendon in isolation (medial head)[5,9,10] the central one third of the tendon in isolation[10], the lateral portion in isolation[10], the lateral and central portion combined[10] or involving the medial and long head insertions with the lateral portion intact[10,11].
Demographics
Triceps tendon ruptures most commonly affect men in the 4th and 5th decades of life. From our pooled results we observed the mean age at rupture to be 47.5 years with a range from 12 to 75 years[1,3,5,8-28]. There was an 11:1 ratio of males to females (n = 170)[1,3,5,8-29]. Three paediatric cases have been reported in the literature in 12 and 16 year olds[11,22,26].
Associations
Triceps tendon ruptures are reported to be more common in systemic disease or entities such as chronic renal failure with secondary hypo-parathyroidism, rheumatoid arthritis and diabetes[8]. Localised infection has also been reported as a cause of rupture[1]. Interestingly chronic pre-existing posterior elbow pain may be present in up to a third of the patients[25] and with histology demonstrating chronic tendinopathy features in patients with pre-existing pain[17]. In traumatic ruptures, one study observed intra-articular fractures or collateral ligament ruptures in 3 of 6 patients (50%) and advised arthroscopic assessment of the joint at the same time as repair[12]. Concurrent olecranon fractures[16] and ulna neuropathy secondary to haematoma[23] have also been observed with traumatic ruptures. Bilateral tears have been reported in patients with a history of anabolic steroid use[26-28].
Mechanism of injury
The two described mechanisms for acute tears of the triceps are direct contact trauma, such as a fall or hitting fixed resistance with the posterior elbow[5,14,19,21,25]. Weightlifting[1,5,17,19,23-25,27,30] was the most common sport associated with acute tears and was often associated with a history of steroid use[1,23,30]. American football[3,29] and general sports injuries[8], as well as direct lacerations[10] have all also been reported as mechanisms.
Investigation
History and examination form the mainstay of diagnosis. Patients typically present with ecchymosis, pain, swelling, extension lag and a decreased active range of motion[10,19,21,22,31]. Palpable defects are commonly found and present in up to 80% of patients[10,21,22,31]. Partial tears may be easily missed as patients may have a good range of active motion, but do typically present with reduced power on extension of the elbow[5,6,9,15,18,20,31].
A bony fleck proximal to the olecranon is commonly identified on lateral radiographs[10,12,17,23,25,27] and is strongly suggestive of a triceps avulsion injury The bony fleck may also be demonstrated on ultrasound (US)[7,8]. This radiological sign reflects the intra-operative observation that 33%-73% of patients have avulsion fractures off the olecranon. The remainder of patients have a rupture at the bone tendon junction[19,25]. Triceps ruptures can be missed on X-ray[22,25] and both US and magnetic resonance imaging (MRI) have been used to diagnosis complete tears and partial tears[7,17,19,25,27]. US has been reported to be as accurate as MRI for both complete and partial ruptures, including identifying the location of partial rupture[8,22].
Treatment
Partial tears: Good results of non-operative treatment even in patients with high functional demands have been reported for the treatment of partial tears. Treatment involves physiotherapy, bracing and avoidance of heavy lifting, pushing or resisted extension for a period of up to 12 wk[27,31]. Harris et al[27] reported good results in a single high demand patient with bilateral tears treated with a conservative regime. Platelet rich plasma (PRP) injection has also been advocated for the treatment of partial tears[18,29]. Cheatham et al[18] reported the results of a single patient treated with PRP with resolution of pain and return to gym 4 mo after a PRP and physiotherapy regime.
Complete tears
Acute tears: Early primary repair is indicated for complete acute ruptures. Surgery is preferably preformed within the first three weeks of injury. Numerous surgical techniques have been reported. These include suture anchors in the triceps footprint[5,6,21,25,32], bone tunnels[10,14,20,22,31,33] or a combination of both tunnels and anchors[15,19,33]. Suture anchors repairs have also been performed arthroscopically[5,6,32].
Bava et al[21] reported the results of 5 male patients treated with an open suture anchor technique. They reported a mean American Shoulder and Elbow Surgeons elbow score of 99.2 at an average of 32 mo follow-up[21]. Lempainen et al[25] also reported excellent results in three athletes treated with an open suture anchor technique for acute tendon rupture. van Reit and Neuerman[10] report on the largest series of open bone tunnel repairs. van Reit et al[10] reported the results of 14 patients treated for acute tendon rupture with a bone tunnel technique. Triceps strength was noted to be 4/5 or 5/5 on manual testing in all examined subjects post operatively. Isokinetic testing of ten patients showed that peak strength was, on the average, 82% of that of the untreated extremity. Three re-ruptures were reported in their series[10]. van Riet et al[10] reported the results of six patients treated with a bone tunnel technique and reported good to excellent results at 12 mo post op with no cases of re-rupture. Kokkalis et al[19], Paniago et al[15] and Paci et al[33], all report good results utilising a combined bone tunnel and suture anchor technique in three separate case reports with no adverse advents reported.
Techniques utilising arthroscopic repairs for acute injuries have been reported by Athwal et al[5] and Ng et al[32]. Athwal et al[5] reported good results for the arthroscopic repair of two acute tears treated with an arthroscopic technique at 2 years’ follow-up with respect DASH and Mayo elbow scores. Ng et al[32] did not report outcomes for their technique.
Because of the heterogeneity of types of tear, repair techniques, and outcome measures it is impossible to determine superiority of one technique over another. Generally surgery has been reported to give good improvement in the Morrey score, Mayo, ASES, Oxford elbow scores and DASH[6,9,14,21,29]. It is reported to significantly reduce pain and improve muscle strength[6,10,19]. Our pooled results have demonstrated that in three studies, all patients achieved full extension in some studies with flexion to at least 110 degrees[10,14,15], whereas others achieve an average loss of 7-10 degrees of extension[10,19]. Three of 14 (21%) re-ruptures were reported in van Reit[10]’s study, one suture anchor pullout was been reported and needed revision[14], and one asymptomatic partial re-rupture was detected on post-operative MRI[6]. Otherwise no re-ruptures were reported or commented on.
Chronic tears: The management of chronic tendon ruptures is a challenge. Occasionally it is possible to repair the tendon using one of the techniques described above. For chronic ruptures with significant tendon retraction, reconstruction with a graft may be required. Grafts include achilles allograft[11,13] or ipsilateral semi-tendinous tendon[10,15], aconeus[10,11], Latisimus Dorsi[10], plantaris[10] and palmaris longus[10]. Aconeus[26] and palmaris longus have also been used in augmentation of primary repairs[20]. Sanchez-Sotelo et al[11] reports the largest case series of chronic rupture reconstruction from the Mayo clinic. They utilised an achilles tendon allograft in three cases or an anconeus muscle flap in four cases. One rotation flap failed six months after operation. At an average of 33 mo follow-up the remaining six patients had no or slight pain, restoration of a functional arc of movement and normal or slightly decreased power of extension[11].
Biomechanical studies
Petre et al[34] reported the intact triceps tendon has a peak load to failure of 1741N, in comparision to peak load to failure of 317N, and 593N for a direct repair, and augmented repair tendons respectively. Comparison made between peak load to failure for a trans-osseous cruciate suture technique[10] and a two bone tunnel and knotless sutures technique[33], showed a significant difference of 510N for the knotless technique and 283N for the cruciate technique[35]. A similar peak load to failure of 317N was found for the same trans-osseous cruciate suture technique[10], but found to be less than the peak load of 593N when the repair was augmented with interwoven flexor carpi radialis[34]. Interestingly Yeh et al[4] observed no significant difference in the peak load to failure for an “anatomic” double row trans-osseous repair[4], the trans-osseous cruciate suture technique[10] and a 2 suture anchor with Krakow-type whip-stitch technique[4].
Snapping triceps
The snapping triceps occurs in a younger population than triceps tendon rupture with a mean age of 32 years (n = 30), ranging from 14-65 years[36-42] and slightly reduced male to female ratio of 6.5:1[36-42].
Snapping triceps is a dynamic condition occurring during flexion or extension[43] of the elbow and is characterised by a snap on both active and passive movement[43]. The triceps can dislocate on either the medial or lateral side, but is much more common medially[41]. It can be asymptomatic, cause snapping, elbow pain or ulna neuropathy if dislocating medially[42-44]. Snapping triceps has been demonstrated to be bilateral in some patients, but is not necessarily symptomatic on both sides[42]. On the medial side, the snapping can be attributed to the ulna nerve, but snapping may still occur despite ulna nerve transposition[36]. Snapping triceps may be associated with dislocation of the ulna nerve[43]. Spinner et al[42] reported all 17 patients in his series (100%) having concurrent dislocation of the ulna nerve with the snapping triceps. Spinner postulated that a snapping ulna nerve and snapping triceps could be differentiated by the angle at which the snapping occurred. The ulna nerve is thought to snap at 70-90 degrees of flexion, whereas the triceps is thought to snap at around 115 degrees of flexion[43].
Aetiology
Snapping triceps is thought to be due to the medial vector placed on triceps that can occur in cubitus varus and is not thought to be associated with rotational deformities[44] or muscle activation patterns[40]. This medial vector is a function of the T angle where the T angle is the angle between the subtended line of pull of triceps (humeral shaft with extended elbow) and the longitudinal line of proximal ulna[44].
On the medial side snapping triceps can be a complication of displaced supracondylar fractures[36,45], inherited as an accessory medial triceps or abnormal insertion[43,46], due to hypertrophy of the medial triceps in athletes[43,47], associated with hypermobility of the ulna nerve[42], associated with osseous abnormalities[42] and as a complication of ulna nerve transposition[48,49]. On the lateral side it has been associated with a widened triceps tendon inserting more laterally and is treated with resection of the lateral edge[41].
Diagnosis
US, MRI, CT and sonoelastography have been used for diagnosis[37-39,43,50]. Ultrasound is the imaging modality of choice of some as can be used as a dynamically to differentiate between a snapping medial triceps and a subluxing medial nerve[37].
Treatment
Initially conservative treatment can be attempted with NSAIDS and avoidance of provoking activities for 3-6 mo[43]. If this is unsuccessful surgery can be considered[36]. Surgery can include resection of the triceps edge, transposition of the tendon, transposing an associated ulnar nerve and correction of cubitus varus[43,45]. Transposition involves transferring the medial third of the tendon to the lateral position[36,47].
DISCUSSION
The distal insertion of the triceps anatomy is presented and relates to the different types of tears seen in clinical practice. Distal triceps tears can present in a wide age group, but are much more common in males. They can be associated with a history of steroid use and sports injuries, especially weightlifting. Full thickness tears are usually easily diagnosed on clinical examination, but partial thickness tears can be missed and require imaging with either MRI or US. They can be associated with intra-articular fractures and collateral ligament injuries around the elbow. Some partial thickness tears can be managed with nonsurgical treatment, and full thickness tears can be treated with reattachment via anchors or transosseous sutures. Chronic tears may require augmentation with tendinous allograft or autograft. Snapping triceps presents in a younger age group, but still with predominance in males. It is much more common on the medial side and can present with an array of symptoms apart from snapping. It can be misdiagnosed as an ulnar nerve subluxation and can be a cause of persistent symptoms after surgery for this. Treatment initially is non-surgical, but can involve resection of the thickened edge of the tendon, transposition of the tendon and management of the ulnar nerve.
COMMENTS
Background
Distal triceps injuries are rare and therefore can be misdiagnosed and poorly managed. The purpose of the systematic review of distal triceps injuries was to identify the main injuries that occur and how to diagnose these as well as to identify if there was a consensus or how to manage these.
Research frontiers
The main hotspot identified in this review is the best type of fixation for distal triceps ruptures and if these injuries are being better diagnosed then hopefully there will be larger numbers of cases to investigate clinically with regards to superiority of fixation.
Innovations and breakthroughs
The systematic review has shown that magnetic resonance imaging is superior at confirming the diagnosis of distal triceps tears when there is clinical doubt whereas snapping triceps are better diagnosed using ultrasound due to its dynamic nature. Partial tears of the distal triceps can be initially treated conservatively but full tears need to be treated surgically. Snapping triceps can also be treated conservatively initially but failure to resolve symptoms can be treated surgically with resection of the snapping edge of triceps and/or transposition.
Applications
The systematic review will hopefully make readers more aware of distal triceps injuries and the differential diagnosis of snapping triceps when faced with a subluxing ulna nerve. The authors hope that as there is no gold standard for distal triceps tear fixation that future research can investigate these in the clinical setting as opposed to the cadaveric setting to identify which fixation is superior.
Peer-review
This is a review article on the topic of distal triceps lesions. The authors perform a systematic review of the literature and present their conclusions based only in original data form the search. This is a well written paper that is interesting to read and will be of help to the readers of the journal.
Footnotes
Conflict-of-interest statement: There are no conflicts of interests for any of the authors with regards to this paper.
Data sharing statement: N/A.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): E
Peer-review started: February 9, 2017
First decision: March 27, 2017
Article in press: May 19, 2017
P- Reviewer: Cui Q, Gao BL, Iban MAR, Kodde IF S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
References
- 1.Koplas MC, Schneider E, Sundaram M. Prevalence of triceps tendon tears on MRI of the elbow and clinical correlation. Skeletal Radiol. 2011;40:587–594. doi: 10.1007/s00256-010-1043-9. [DOI] [PubMed] [Google Scholar]
- 2.Safran MR, Graham SM. Distal biceps tendon ruptures: incidence, demographics, and the effect of smoking. Clin Orthop Relat Res. 2002;40:275–283. [PubMed] [Google Scholar]
- 3.Finstein JL, Cohen SB, Dodson CC, Ciccotti MG, Marchetto P, Pepe MD, Deluca PF. Triceps Tendon Ruptures Requiring Surgical Repair in National Football League Players. Orthop J Sports Med. 2015;3:2325967115601021. doi: 10.1177/2325967115601021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yeh PC, Stephens KT, Solovyova O, Obopilwe E, Smart LR, Mazzocca AD, Sethi PM. The distal triceps tendon footprint and a biomechanical analysis of 3 repair techniques. Am J Sports Med. 2010;38:1025–1033. doi: 10.1177/0363546509358319. [DOI] [PubMed] [Google Scholar]
- 5.Athwal GS, McGill RJ, Rispoli DM. Isolated avulsion of the medial head of the triceps tendon: an anatomic study and arthroscopic repair in 2 cases. Arthroscopy. 2009;25:983–988. doi: 10.1016/j.arthro.2009.02.020. [DOI] [PubMed] [Google Scholar]
- 6.Heikenfeld R, Listringhaus R, Godolias G. Endoscopic repair of tears of the superficial layer of the distal triceps tendon. Arthroscopy. 2014;30:785–789. doi: 10.1016/j.arthro.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Downey R, Jacobson JA, Fessell DP, Tran N, Morag Y, Kim SM. Sonography of partial-thickness tears of the distal triceps brachii tendon. J Ultrasound Med. 2011;30:1351–1356. doi: 10.7863/jum.2011.30.10.1351. [DOI] [PubMed] [Google Scholar]
- 8.Tagliafico A, Gandolfo N, Michaud J, Perez MM, Palmieri F, Martinoli C. Ultrasound demonstration of distal triceps tendon tears. Eur J Radiol. 2012;81:1207–1210. doi: 10.1016/j.ejrad.2011.03.012. [DOI] [PubMed] [Google Scholar]
- 9.Khiami F, Tavassoli S, De Ridder Baeur L, Catonné Y, Sariali E. Distal partial ruptures of triceps brachii tendon in an athlete. Orthop Traumatol Surg Res. 2012;98:242–246. doi: 10.1016/j.otsr.2011.09.022. [DOI] [PubMed] [Google Scholar]
- 10.van Riet RP, Morrey BF, Ho E, O’Driscoll SW. Surgical treatment of distal triceps ruptures. J Bone Joint Surg Am. 2003;85-A:1961–1967. doi: 10.2106/00004623-200310000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Sanchez-Sotelo J, Morrey BF. Surgical techniques for reconstruction of chronic insufficiency of the triceps. Rotation flap using anconeus and tendo achillis allograft. J Bone Joint Surg Br. 2002;84:1116–1120. doi: 10.1302/0301-620x.84b8.12902. [DOI] [PubMed] [Google Scholar]
- 12.Gharanizadeh K, Mazhar FN, Molavy N, Bagherifard A, Shariatzadeh H. Avulsions of Triceps Brachii : associated injuries and surgical treatment; a case series. Acta Orthop Belg. 2016;82:197–202. [PubMed] [Google Scholar]
- 13.Aunon-Martin I, Prada-Canizares A, Jimenez-Diaz V, Vidal-Bujanda C, Leon-Baltasar JL. Treatment of a Complex Distal Triceps Tendon Rupture With a New Technique: A Case Report. Arch Trauma Res. 2016;5:e32221. doi: 10.5812/atr.32221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Neumann H, Schulz AP, Breer S, Faschingbauer M, Kienast B. Traumatic Rupture of the Distal Triceps Tendon (A Series of 7 Cases) Open Orthop J. 2015;9:536–541. doi: 10.2174/1874325001509010536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paniago AF, Storti TM, Faria RS, Morais DC, Souza MP. Reconstruction of chronic tearing of the distal triceps using the double-row configuration: technical note. Rev Bras Ortop. 2015;50:596–600. doi: 10.1016/j.rboe.2015.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tarallo L, Zambianchi F, Mugnai R, Costanzini CA, Catani F. Distal triceps tendon repair using Krakow whipstitches, K wires, tension band and double drilling technique: a case report. J Med Case Rep. 2015;9:36. doi: 10.1186/s13256-014-0504-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mangano T, Cerruti P, Repetto I, Trentini R, Giovale M, Franchin F. Chronic Tendonopathy as a Unique Cause of Non Traumatic Triceps Tendon Rupture in a (Risk Factors Free) Bodybuilder: A Case Report. J Orthop Case Rep. 2015;5:58–61. doi: 10.13107/jocr.2250-0685.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheatham SW, Kolber MJ, Salamh PA, Hanney WJ. Rehabilitation of a partially torn distal triceps tendon after platelet rich plasma injection: a case report. Int J Sports Phys Ther. 2013;8:290–299. [PMC free article] [PubMed] [Google Scholar]
- 19.Kokkalis ZT, Mavrogenis AF, Spyridonos S, Papagelopoulos PJ, Weiser RW, Sotereanos DG. Triceps brachii distal tendon reattachment with a double-row technique. Orthopedics. 2013;36:110–116. doi: 10.3928/01477447-20130122-03. [DOI] [PubMed] [Google Scholar]
- 20.Scolaro JA, Blake MH, Huffman GR. Triceps tendon reconstruction using ipsilateral palmaris longus autograft in unrecognized chronic tears. Orthopedics. 2013;36:e117–e120. doi: 10.3928/01477447-20121217-30. [DOI] [PubMed] [Google Scholar]
- 21.Bava ED, Barber FA, Lund ER. Clinical outcome after suture anchor repair for complete traumatic rupture of the distal triceps tendon. Arthroscopy. 2012;28:1058–1063. doi: 10.1016/j.arthro.2011.12.016. [DOI] [PubMed] [Google Scholar]
- 22.Kibuule LK, Fehringer EV. Distal triceps tendon rupture and repair in an otherwise healthy pediatric patient: a case report and review of the literature. J Shoulder Elbow Surg. 2007;16:e1–e3. doi: 10.1016/j.jse.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 23.Duchow J, Kelm J, Kohn D. Acute ulnar nerve compression syndrome in a powerlifter with triceps tendon rupture--a case report. Int J Sports Med. 2000;21:308–310. doi: 10.1055/s-2000-9468. [DOI] [PubMed] [Google Scholar]
- 24.Molloy JM, Aberle CJ, Escobar E. Triceps tendon tear in a middle-aged weightlifter. J Orthop Sports Phys Ther. 2013;43:848. doi: 10.2519/jospt.2013.0419. [DOI] [PubMed] [Google Scholar]
- 25.Lempainen L, Sarimo J, Rawlins M, Heikkilä J, Orava S. Triceps tears in athletes: different injury patterns and surgical treatment. Arch Orthop Trauma Surg. 2011;131:1413–1417. doi: 10.1007/s00402-011-1319-0. [DOI] [PubMed] [Google Scholar]
- 26.Sierra RJ, Weiss NG, Shrader MW, Steinmann SP. Acute triceps ruptures: case report and retrospective chart review. J Shoulder Elbow Surg. 2006;15:130–134. doi: 10.1016/j.jse.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 27.Harris PC, Atkinson D, Moorehead JD. Bilateral partial rupture of triceps tendon: case report and quantitative assessment of recovery. Am J Sports Med. 2004;32:787–792. doi: 10.1177/0363546503258903. [DOI] [PubMed] [Google Scholar]
- 28.Golshani B, Bindra J, Hunter JC. Bilateral triceps tendon tear. Radiol Case Rep. 2011;6:581. doi: 10.2484/rcr.v6i4.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mair SD, Isbell WM, Gill TJ, Schlegel TF, Hawkins RJ. Triceps tendon ruptures in professional football players. Am J Sports Med. 2004;32:431–434. doi: 10.1177/0095399703258707. [DOI] [PubMed] [Google Scholar]
- 30.Sollender JL, Rayan GM, Barden GA. Triceps tendon rupture in weight lifters. J Shoulder Elbow Surg. 1998;7:151–153. doi: 10.1016/s1058-2746(98)90227-0. [DOI] [PubMed] [Google Scholar]
- 31.Marinello PG, Peers S, Sraj S, Evans PJ. A treatment algorithm for the management of distal triceps ruptures. Tech Hand Up Extrem Surg. 2015;19:73–80. doi: 10.1097/BTH.0000000000000082. [DOI] [PubMed] [Google Scholar]
- 32.Ng T, Rush LN, Savoie FH. Arthroscopic Distal Triceps Repair. Arthrosc Tech. 2016;5:e941–e945. doi: 10.1016/j.eats.2016.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Paci JM, Clark J, Rizzi A. Distal triceps knotless anatomic footprint repair: a new technique. Arthrosc Tech. 2014;3:e621–e626. doi: 10.1016/j.eats.2014.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Petre BM, Grutter PW, Rose DM, Belkoff SM, McFarland EG, Petersen SA. Triceps tendons: a biomechanical comparison of intact and repaired strength. J Shoulder Elbow Surg. 2011;20:213–218. doi: 10.1016/j.jse.2010.08.017. [DOI] [PubMed] [Google Scholar]
- 35.Clark J, Obopilwe E, Rizzi A, Komatsu DE, Singh H, Mazzocca AD, Paci JM. Distal triceps knotless anatomic footprint repair is superior to transosseous cruciate repair: a biomechanical comparison. Arthroscopy. 2014;30:1254–1260. doi: 10.1016/j.arthro.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 36.Kontogeorgakos VA, Mavrogenis AF, Panagopoulos GN, Lagaras A, Koutalos A, Malizos KN. Cubitus varus complicated by snapping medial triceps and posterolateral rotatory instability. J Shoulder Elbow Surg. 2016;25:e208–e212. doi: 10.1016/j.jse.2016.03.012. [DOI] [PubMed] [Google Scholar]
- 37.Chuang HJ, Hsiao MY, Wu CH, Özçakar L. Dynamic Ultrasound Imaging for Ulnar Nerve Subluxation and Snapping Triceps Syndrome. Am J Phys Med Rehabil. 2016;95:e113–e114. doi: 10.1097/PHM.0000000000000466. [DOI] [PubMed] [Google Scholar]
- 38.Łasecki M, Olchowy C, Pawluś A, Zaleska-Dorobisz U. The Snapping Elbow Syndrome as a Reason for Chronic Elbow Neuralgia in a Tennis Player - MR, US and Sonoelastography Evaluation. Pol J Radiol. 2014;79:467–471. doi: 10.12659/PJR.891393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zbojniewicz AM. US for diagnosis of musculoskeletal conditions in the young athlete: emphasis on dynamic assessment. Radiographics. 2014;34:1145–1162. doi: 10.1148/rg.345130151. [DOI] [PubMed] [Google Scholar]
- 40.Boon AJ, Spinner RJ, Bernhardt KA, Ross SR, Kaufman KR. Muscle activation patterns in snapping triceps syndrome. Arch Phys Med Rehabil. 2007;88:239–242. doi: 10.1016/j.apmr.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 41.Spinner RJ, Goldner RD, Fada RA, Sotereanos DG. Snapping of the triceps tendon over the lateral epicondyle. J Hand Surg Am. 1999;24:381–385. doi: 10.1053/jhsu.1999.0381. [DOI] [PubMed] [Google Scholar]
- 42.Spinner RJ, Goldner RD. Snapping of the medial head of the triceps and recurrent dislocation of the ulnar nerve. Anatomical and dynamic factors. J Bone Joint Surg Am. 1998;80:239–247. doi: 10.2106/00004623-199802000-00011. [DOI] [PubMed] [Google Scholar]
- 43.Spinner RJ, Goldner RD. Snapping of the medial head of the triceps: diagnosis and treatment. Tech Hand Up Extrem Surg. 2002;6:91–97. doi: 10.1097/00130911-200206000-00008. [DOI] [PubMed] [Google Scholar]
- 44.Spinner RJ, An KN, Kim KJ, Goldner RD, O’Driscoll SW. Medial or lateral dislocation (snapping) of a portion of the distal triceps: a biomechanical, anatomic explanation. J Shoulder Elbow Surg. 2001;10:561–567. doi: 10.1067/mse.2001.118006. [DOI] [PubMed] [Google Scholar]
- 45.Spinner RJ, O’Driscoll SW, Davids JR, Goldner RD. Cubitus varus associated with dislocation of both the medial portion of the triceps and the ulnar nerve. J Hand Surg Am. 1999;24:718–726. doi: 10.1053/jhsu.1999.0718. [DOI] [PubMed] [Google Scholar]
- 46.Spinner RJ, Davids JR, Goldner RD. Dislocating medial triceps and ulnar neuropathy in three generations of one family. J Hand Surg Am. 1997;22:132–137. doi: 10.1016/S0363-5023(05)80193-5. [DOI] [PubMed] [Google Scholar]
- 47.Spinner RJ, Wenger DE, Barry CJ, Goldner RD. Episodic snapping of the medial head of the triceps due to weightlifting. J South Orthop Assoc. 1999;8:288–292. [PubMed] [Google Scholar]
- 48.Spinner RJ, Gabel GT. Latrogenic snapping of the medial head of the triceps after ulnar nerve transposition. J South Orthop Assoc. 2001;10:236–240. [PubMed] [Google Scholar]
- 49.Minami A, Kato H, Iwasaki N. Snapping of Triceps Tendon After Anterior Nerve Transposition for Recurrent Subluxation of the Ulnar Nerve. Hand Surg. 1999;4:193–196. doi: 10.1142/s0218810499000253. [DOI] [PubMed] [Google Scholar]
- 50.Jacobson JA, Jebson PJ, Jeffers AW, Fessell DP, Hayes CW. Ulnar nerve dislocation and snapping triceps syndrome: diagnosis with dynamic sonography--report of three cases. Radiology. 2001;220:601–605. doi: 10.1148/radiol.2202001723. [DOI] [PubMed] [Google Scholar]


