Abstract
Objective:
To examine the effects of a new wearable type of lumbosacral support on low back pain.
Methods:
A total of 121 healthcare workers participated in this study. They were randomly allocated into the experimental and control groups and the former wore the support with signals of compression on the back by poor posture for the first 3 months. The control group remained on a waiting list for the first 3 months. Medical history, musculoskeletal symptoms, feeling in good posture, sleep habits, psychological distress, Roland-Morris Disability Questionnaire, and Somatosensory Amplification Scale (SSAS) were evaluated. The range of motion (ROM) in the shoulder and hip joints as well as spinal alignment were evaluated. Our primary concern was the difference in the change of low back pain measured by visual analog scale (VAS) between the two groups.
Results:
A total of 54 participants in the experimental and 53 participants in the control groups were analyzed. VAS and SSAS scores as well as lumbar spinal ROM in the experimental group significantly decreased. Low back pain (OR=0.401, 95% CI=0.168-0.954) and neck pain in the experimental group (OR=0.198, 95% CI=0.052-0.748) significantly decreased.
Conclusions:
The new lumbar support reduced VAS and SSAS scores, lumbar spinal ROM, low back pain, and neck pain. This new type of lumbar support reduced low back pain among healthcare workers.
Keywords: Healthcare workers, Low back pain, Lumbar support, Posture, Somatosensory Amplification Scale, Spinal alignment
Introduction
Work-related musculoskeletal disorders are a major contribution to the cost of work-related illness in developed countries1,2). Low back pain has influences on quality of life, work absenteeism, and medical expenses3), including in nurses4). Working people (25-60 years) are affected by low back pain at least once in their lifetime5).
Various ergonomic aids are marketed for the prevention of low back pain. Lumbar supports are frequently used to prevent low back pain among workers with a reduced trunk motion for flexion-extension and lateral bending6,7). Furthermore, it reduces intradiscal pressure on the lumbar vertebrae8) as well as load on the trunk9). A history of low back pain was a strong predictor for the incidence of new episodes of low back pain10). Homecare workers with frequent episodes of low back pain reported an adherence rate of 61% to 81% with lumbar supports and 45% decreases in pain intensity when using lumbar supports11). However, their effectiveness is still unclear7) and no type of lumbar support is specifically recommended for low back pain12).
Nurses have a risk of low back pain from being in awkward postures, carrying and repositioning patients, prolonged standing, and working without sufficient breaks13). Flexion, rotation, and awkward positions of the lumbar spine have a strong association with low back pain14). Lifting in-bed patients is a major risk factor of low back pain among nurses13). These situations are limited not only to nurses but also to other hospital workers.
A neutral posture is composed of an amalgamation of the position of multiple joints, bones, and muscles along the longitudinal axis of the body with equilibrium15). However, continuous poor posture, defined as increased forward head, greater thoracic kyphosis, and a more anterior shoulder position, can lead to musculoskeletal imbalances and pain, which might cause stresses on ligaments and intervertebral discs of the lumbar region16). Furthermore, poor posture affects scapular kinematics, which causes shoulder problems17).
Low back pain is defined as a "bio-psycho-socially induced disease" 18). Feelings of helplessness and hopelessness are important predictors of the onset and persistence of psychosomatic disorders19). Working status and subjective economic hardship were significantly associated with new onset of low back pain for survivors of the Great East Japan Earthquake20,21). Poor sleep is known to cause a range of physiological and psychological effects22). Postures associated with dominance and power affect how people experience pain23). Low back pain could be affected by multiple factors.
This study aimed to evaluate a new wearable type of lumbosacral support on the musculoskeletal symptoms, postural changes, psychological distress, sleep disturbance, somatosensory amplification, and range of motion (ROM) in the major joints.
Methods
Participants
The protocols of this study were approved by the institutional review board of Takeda General Hospital (approval number: H25-004) and all participants consented to join this study. The recruitment period was set from July 26 to October 30, 2013, and this study was conducted from November 19, 2013 to July 20, 2014. A total of 121 workers (5 males and 116 females) at Takeda General Hospital participated in this study and were 20 years old or older. They included nurses (98, 81%), care workers (9, 7.4%), medical assistants (11, 9.1%), and physical therapists (3, 2.5%). Inclusion criteria was a low back pain rating score (0-10 numerical rating scale: NRS) of 3 or more for the worst low back pain at least once a week for the previous 3 months at the recruitment period24). Exclusion criteria were as follows: (1) sensory disturbance in lower extremities; (2) history of surgery for lumbar disorders; (3) psychiatric disorders; and (4) mental disorders.
Randomization and masking
Participants were assigned consecutive numbers upon recruitment based on consent forms. They were randomly allocated into the experimental and control groups in a 1:1 ratio according to block randomization with a randomly selected block size of 4 or 6, generated by R3.0.1.
Experimental protocol
The wearable type of lumbosacral support (Spinal Underwear, Alcare, Tokyo, Japan) has been developed to correct posture using signals of compression on the skin of the back from poor posture. It uses NANO FRONT® (Teijin, Osaka, Japan) on the back (gray area, Fig. 1), which stimulates a tactile sense on the skin of the back while in poor posture. These stimuli can affect the erector spinae muscles to correct into a better posture24). The experimental group wore the support for the first 3 months except bathing and sleeping. Participants in the control group remained on a waiting list and were informed that they would wear the Spinal Underwear after 3 months had passed in the same manner.
Fig. 1.
Appearance of Spinal Underwear.
Asterisk: Textile fabrics for stimulating the back while in poor posture.
Measurement and Outcome
Evaluations were performed at the beginning and end of the program by the same blinded examiner for both groups. This questionnaire included medical history, subjective musculoskeletal symptoms (shoulder discomfort, knee pain, feeling numbness (not sensory disturbance), shoulder pain, neck pain, back pain, pain in extremities, and headache)20,21), sleep habits (Athens Insomnia Scale)25), psychological distress (K6)26), Roland-Morris Disability Questionnaire (RDQ, Japanese version)27), and Somatosensory Amplification Scale (SSAS)28). Subjective "feeling in good posture" was also inquired to evaluate postural changes of participants. ROM, including the shoulder joints in a standing position (forward flexion, external rotation with the arm at the side), the hip joints in a supine position (straight leg raising test, flexion, internal rotation), were evaluated with a goniometer and standing sagittal spinal alignment (flexion, neutral, and extension) with a Spinal Mouse® (Idiag, Volketswil, Switzerland). The spinal curvature (C7-S3) was measured 3 times and the mean angle was calculated12). Susceptibility of sleep disturbance was defined as greater than or equal to 6/24 points on the Athens Insomnia Scale. Psychological distress was defined as greater than or equal to 10/24 points on K6. Psychosomatic disease was suspected to be greater than or equal to 31/50 points on SSAS. Only low back pain was measured using a visual analog scale (VAS) ranging from 0 cm for no pain to 10 cm for unbearable pain29) from immediately before starting this study to the final follow-up. Age, gender, height, body weight, sleep disturbance, psychological distress, and somatosensory amplification were considered as confounding factors. Our primary outcome was determined to be the difference in the change of low back pain measured by VAS between the two groups. We also considered the following as a secondary outcome: Presence of subjective musculoskeletal symptoms, feeling in good posture, Athens Insomnia Scale, K6, RDQ, SSAS, and ROM of the shoulder joints, hip joints, and spine. The compliance of wearing the Spinal Underwear was checked by a diary in which participants had to write every day.
Statistical analysis
All statistical analyses were planned in an intention-to-treat manner. For the continuous variable, analysis of variance for repeated measures was used to estimate the intergroup difference over time. When the P value of the interaction term of allocation (x) time was <0.05, we considered the difference as statistically significant. As effect size, we calculated partial η2 using type III sum of squares. No covariate was put into the regression model. For the binary variable (presence of subjective musculoskeletal symptoms), for which we used a logistic regression model, allocation and baseline information of symptoms present were put into as predictive variables. All analyses were performed using R3.0.1. and P value of <0.05 was set for statistical significance. No adjustments for multi-hypothesis tests were conducted.
Results
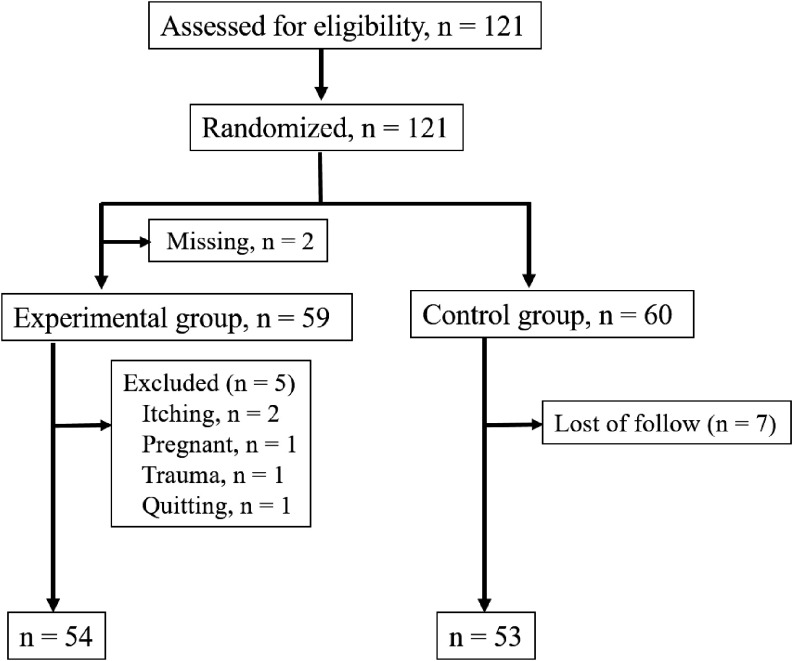
One hundred and twenty-one participants were randomly assigned to the experimental (n=61) and control groups (n=60) (Fig. 2). Baseline characteristics of participants (N=121) immediately after recruitment were shown in Table 1. Participants with severe low back pain (n=79, VAS ≥3) had significantly higher VAS (p=0.0005), RDQ scores (p<0.0001), rate of feeling numbness (p=0.011), and the right shoulder flexion (p=0.015) as compared with those having moderate low back pain (n=40, VAS <3). There were no significant differences in the other criteria. There was no significant difference between the experimental and control groups in every criterion, including VAS, immediately after randomization (data not shown). In the experimental group, 2 participants were excluded because of a misunderstanding in their group. Furthermore, in the same group, 5 participants were lost due to itching (n=2), pregnant (n=1), trauma (n=1), and quitting (n=1). In the waiting control group (n=60), 7 participants were lost. A total of 54 participants in the experimental group (2 males and 52 females) and 53 participants in the control group (1 male and 52 females) were analyzed in the final follow-up (Fig. 2). There was no significant difference in the spinal alignment. VAS scores at baseline characteristics of the experimental (n=54) and control groups (n=53) were homogenous at the beginning of this protocol (Table 2). However, VAS was significantly lower in the experimental group as compared with the control group (p=0.038) because of the two missing participants. The experimental group exhibited significant improvement over time as compared with the control group with regard to VAS (F=4.53, df=1; 105, p=0.036, partial η2=0.04) and SSAS scores (F=5.72, df=1; 105, p=0.019, partial η2=0.05). The lumbar spinal ROM in the experimental group significantly decreased as compared with the control group (F=4.15, df=1; 103, p=0.044, partial η2=0.04) (Table 3). There were no significant differences between the two groups with regard to the remaining variables. With regard to subjective symptoms, low back pain (OR=0.401, 95% CI=0.168-0.954, p=0.039) and neck pain (OR=0.198, 95% CI=0.052-0.748, p=0.017) in the experimental group significantly decreased as compared with the control group (Table 4). There were no significant differences between the two groups with regard to the remaining musculoskeletal symptoms.
Fig. 2.
Selection of study participants.
Table 1.
Baseline characteristics of the participants
| Low back pain | P | ||
|---|---|---|---|
| Moderate (n=40) | Severe (n=79) | ||
| SLR*: Straight leg raising test | |||
| Age | 44.2±10.4 | 44.7±9.8 | 0.798 |
| Gender (Female, %) | 38 (95%) | 78 (98.7%) | 0.261 |
| Height | 158.3±6.2 | 157.8±5.4 | 0.637 |
| Body weight | 56.0±9.4 | 57.3±9.6 | 0.481 |
| VAS | 2.00±1.77 | 3.43±2.20 | 0.0005 |
| RDQ | 0.98±1.44 | 3.25±2.91 | <0.0001 |
| K6 | 4.2±3.3 | 3.9±3.8 | 0.775 |
| Athens | 5.1±2.8 | 4.8±2.8 | 0.530 |
| SSAS | 28.6±5.6 | 29.0±5.8 | 0.734 |
| Feeling in good posture | 2 (5%) | 8 (10.1%) | 0.492 |
| Shoulder discomfort | 25 (62.5%) | 52 (65.8%) | 0.839 |
| Knee pain | 11 (27.5%) | 20 (25.3%) | 0.827 |
| Numbness | 1 (2.5%) | 15 (19%) | 0.011 |
| Shoulder pain | 12 (30%) | 12 (15.2%) | 0.089 |
| Neck pain | 9 (22.5%) | 13 (32.5%) | 0.459 |
| Back pain | 8 (20%) | 10 (12.7%) | 0.294 |
| Pain in extremities | 3 (7.5%) | 6 (7.6%) | 1.000 |
| Headache | 7 (17.5%) | 23 (29.1%) | 0.188 |
| Spinal Mouse ® | |||
| Flexion (Th) | 50.8±11.9 | 47.6±20.8 | 0.366 |
| Flexion (L) | 38.2±16.5 | 42.1±19.3 | 0.281 |
| Flexion (S) | 42.8±20.5 | 43.1±16.2 | 0.928 |
| Extension (Th) | 21.8±19.6 | 22.1±21.5 | 0.950 |
| Extension (L) | –37.0±11.7 | –32.6±11.4 | 0.052 |
| Extension (S) | –2.1±10.2 | –2.2±8.4 | 0.967 |
| Thoracic spinal ROM | 29.1±18.2 | 25.4±31.3 | 0.495 |
| Lumbar spinal ROM | 74.6±20.6 | 74.5±18.4 | 0.966 |
| Sacral spinal ROM | 45.1±20.3 | 45.3±17.2 | 0.953 |
| Neutral (Th) | 39.1±13.0 | 34.0±25.8 | 0.239 |
| Neutral (L) | –21.8±10.1 | –19.1±11.4 | 0.212 |
| Neutral (S) | 6.8±8.4 | 10.2±41.9 | 0.612 |
| Flexion-Neutral (Th) | 11.4±14.8 | 13.6±36.1 | 0.708 |
| Flexion-Neutral (L) | 60.1±15.8 | 60.9±14.4 | 0.800 |
| Flexion-Neutral (S) | 36.2±18.8 | 33.0±45.5 | 0.676 |
| Neutral-Extension (Th) | 17.7±19.3 | 11.9±33.3 | 0.318 |
| Neutral-Extension (L) | 14.9±9.7 | 13.4±9.6 | 0.419 |
| Neutral-Extension (S) | 8.8±10.2 | 12.4±41.2 | 0.599 |
| Range of motion | |||
| Rt. SLR* | 72.1±12.1 | 73.3±11.6 | 0.619 |
| Rt. Hip flexion | 120.0±9.9 | 119.1±9.4 | 0.631 |
| Rt. Hip internal rotation | 43.4±11.6 | 41.7±10.5 | 0.438 |
| Rt. Shoulder flexion | 160.9±14.8 | 166.7±10.4 | 0.015 |
| Rt. Shoulder external rotation | 69.6±13.7 | 71.3±15.9 | 0.575 |
| Lt. SLR* | 71.0±14.1 | 73.2±10.8 | 0.348 |
| Lt. Hip flexion | 120.6±7.9 | 118.4±8.0 | 0.152 |
| Lt. Hip internal rotation | 43.1±12.7 | 42.6±11.5 | 0.81 |
| Lt. Shoulder flexion | 162.1±14.7 | 164.1±16.4 | 0.506 |
| Lt. Shoulder external rotation | 69.8±14.2 | 71.4±13.1 | 0.56 |
Table 2.
Baseline characteristics of the participants after the randomization
| Experimental group (n=54) | Control group (n=53) | P | |
|---|---|---|---|
| SLR*: Straight leg raising test | |||
| Age | 44.7±10.0 | 44.7±9.6 | 0.994 |
| Gender (Female, %) | 52/54 | 52/53 | >0.99 |
| Height | 157.7±5.7 | 158.6±5.3 | 0.414 |
| Body weight | 57.1±10.2 | 57.0±9.0 | 0.940 |
| VAS | 2.48±2.09 | 3.35±2.16 | 0.038 |
| RDQ | 2.26±2.44 | 2.83±3.17 | 0.298 |
| K6 | 3.9±3.8 | 4.3±3.2 | 0.549 |
| Athens | 4.6±2.3 | 5.2±3.2 | 0.268 |
| SSAS | 30.0±5.9 | 28.0±5.0 | 0.063 |
| Feeling in good posture | 5 (9.26%) | 5 (9.43%) | >0.99 |
| Low back pain | 35 (64.8%) | 36 (67.9%) | 0.838 |
| Shoulder discomfort | 33 (61.1%) | 37 (68.5%) | 0.418 |
| Knee pain | 12 (22.2%) | 16 (30.2%) | 0.385 |
| Numbness | 8 (14.8%) | 8 (15.1%) | >0.99 |
| Shoulder pain | 13 (24.1%) | 11 (20.8%) | 0.817 |
| Neck pain | 11 (20.4%) | 9 (17%) | 0.805 |
| Back pain | 9 (16.7%) | 6 (11.3%) | 0.579 |
| Pain in extremities | 3 (5.56%) | 5 (9.43%) | 0.489 |
| Headache | 10 (18.5%) | 15 (28.3%) | 0.260 |
| Spinal Mouse ® | |||
| Flexion (Th) | 49.7±16.6 | 50.3±10.5 | 0.808 |
| Flexion (L) | 42.7±18.0 | 39.5±18.2 | 0.352 |
| Flexion (S) | 41.0±17.7 | 44.0±17.7 | 0.383 |
| Extension (Th) | 21.9±21.8 | 22.4±21.0 | 0.898 |
| Extension (L) | –34.0±10.8 | –34.1±12.3 | 0.980 |
| Extension (S) | –2.0±9.0 | –2.1±7.6 | 0.962 |
| Thoracic spinal ROM | 27.9±27.4 | 28.0±21.1 | 0.988 |
| Lumbar spinal ROM | 76.5±20.9 | 73.0±16.9 | 0.353 |
| Sacral spinal ROM | 43.1±18.9 | 46.3±17.8 | 0.380 |
| Neutral (Th) | 33.0±29.8 | 39.3±11.1 | 0.151 |
| Neutral (L) | –18.6±10.2 | –20.5±11.5 | 0.362 |
| Neutral (S) | 12.0±50.3 | 6.2±9.5 | 0.412 |
| Flexion-Neutral (Th) | 16.7±37.2 | 10.8±12.3 | 0.269 |
| Flexion-Neutral (L) | 61.0±16.6 | 59.8±12.8 | 0.669 |
| Flexion-Neutral (S) | 29.1±54.5 | 37.9±16.0 | 0.262 |
| Neutral-Extension (Th) | 11.4±37.8 | 16.9±19.8 | 0.348 |
| Neutral-Extension (L) | 15.4±9.2 | 13.3±9.5 | 0.269 |
| Neutral-Extension (S) | 14.0±49.7 | 8.3±7.6 | 0.420 |
| Range of motion | |||
| Rt. SLR* | 73.1±11.9 | 73.3±12.2 | 0.947 |
| Rt. Hip flexion | 120.4±8.6 | 120.0±9.7 | 0.835 |
| Rt. Hip internal rotation | 42.2±10.8 | 42.6±10.2 | 0.837 |
| Rt. Shoulder flexion | 166.2±11.2 | 164.5±11.2 | 0.442 |
| Rt. Shoulder external rotation | 70.5±13.9 | 71.0±17.0 | 0.849 |
| Lt. SLR* | 71.5±12.2 | 72.9±12.7 | 0.549 |
| Lt. Hip flexion | 118.7±7.4 | 120.8±7.4 | 0.156 |
| Lt. Hip internal rotation | 42.7±11.7 | 42.6±12.3 | 0.985 |
| Lt. Shoulder flexion | 166.1±11.4 | 161.8±19.3 | 0.167 |
| Lt. Shoulder external rotation | 72.1±14.0 | 70.2±12.7 | 0.455 |
Table 3.
Changes after the intervention
| Experimental group (n=54) | Control group (n=53) | P | |
|---|---|---|---|
| Mean, SD | Mean, SD | ||
| SLR*: Straight leg raising test SD: Standard deviation | |||
| Height | –0.0, 0.5 | –0.1, 0.5 | 0.794 |
| Body weight | 0.2, 1.3 | 0.1, 1.0 | 0.440 |
| VAS | –1.1, 1.8 | –0.3, 1.9 | 0.036 |
| RDQ | –0.6, 2.3 | –0.5, 3.0 | 0.815 |
| K6 | –0.37, 3.26 | –0.70, 2.62 | 0.568 |
| Athens | –0.57, 2.69 | –1.55, 2.85 | 0.072 |
| SSAS | –2.80, 5.39 | –0.53, 4.35 | 0.019 |
| Spinal Mouse ® | |||
| Flexion (Th) | –0.9, 18.4 | –8.3, 33.2 | 0.160 |
| Flexion (L) | –17.3, 19.4 | –11.1, 19.3 | 0.103 |
| Flexion (S) | 9.2, 21.2 | 6.1, 16.3 | 0.395 |
| Extension (Th) | 5.0, 20.1 | 0.1, 18.8 | 0.195 |
| Extension (L) | –6.5, 12.5 | –6.5, 12.1 | 0.990 |
| Extension (S) | 6.5, 11.0 | 5.1, 10.1 | 0.503 |
| Thoracic spinal ROM | –5.9, 29.9 | –6.8, 37.0 | 0.892 |
| Lumbar spinal ROM | –10.6, 19.1 | –3.1, 18.9 | 0.044 |
| Sacral spinal ROM | 2.6, 19.1 | 1.2, 19.7 | 0.742 |
| Neutral (Th) | 1.7, 33.5 | –2.3, 13.0 | 0.424 |
| Neutral (L) | –8.4, 13.6 | –7.8, 11.4 | 0.812 |
| Neutral (S) | –0.4, 50.8 | 6.2, 9.0 | 0.355 |
| Flexion-Neutral (Th) | –2.3, 39.2 | –5.7, 38.5 | 0.648 |
| Flexion-Neutral (L) | –8.8, 17.0 | –3.3, 18.7 | 0.117 |
| Flexion-Neutral (S) | 9.5, 57.4 | –0.4, 16.7 | 0.233 |
| Neutral-Extension (Th) | –3.8, 40.8 | –2.9, 20.6 | 0.884 |
| Neutral-Extension (L) | –1.8, 11.1 | –0.7, 12.3 | 0.646 |
| Neutral-Extension (S) | –6.9, 47.8 | 1.0, 8.9 | 0.242 |
| Range of motion | |||
| Rt. SLR* | –1.1, 12.6 | –1.7, 12.7 | 0.811 |
| Rt. Hip flexion | –2.2, 11.5 | 0.6, 9.4 | 0.174 |
| Rt. Hip internal rotation | –6.3, 11.5 | –5.3, 9.6 | 0.621 |
| Rt. Shoulder flexion | 0.6, 11.9 | –2.0, 15.5 | 0.326 |
| Rt. Shoulder external rotation | 0.6, 10.6 | –4.5, 20.0 | 0.097 |
| Lt. SLR* | –0.2, 12.7 | –1.9, 13.2 | 0.498 |
| Lt. Hip flexion | –1.9, 10.9 | –2.0, 7.6 | 0.943 |
| Lt. Hip internal rotation | –4.1, 11.2 | –4.7, 11.2 | 0.768 |
| Lt. Shoulder flexion | –2.5, 12.4 | 0.4, 17.5 | 0.321 |
| Lt. Shoulder external rotation | 0.5, 10.3 | –2.6, 10.9 | 0.132 |
Table 4.
Changes of musculoskeletal symptoms
| OR | 95% CI | P | |
|---|---|---|---|
| OR: Odds ratio | |||
| Feeling in good posture | 2.94 | 0.729, 11.80 | 0.130 |
| Low back pain | 0.401 | 0.168, 0.954 | 0.039 |
| Shoulder discomfort | 0.425 | 0.153, 1.180 | 0.102 |
| Knee pain | 0.688 | 0.205, 2.310 | 0.545 |
| Numbness | 1.32 | 0.295, 5.940 | 0.713 |
| Shoulder pain | 0.554 | 0.183, 1.680 | 0.296 |
| Neck pain | 0.198 | 0.052, 0.748 | 0.017 |
| Back pain | 0.492 | 0.149, 1.630 | 0.245 |
| Pain in extremities | 0.378 | 0.086, 1.670 | 0.199 |
| Headache | 0.884 | 0.309, 2.530 | 0.818 |
Discussion
The 12-month prevalence of low back pain has been estimated to be from 15% to 64% in developed countries30). Healthcare settings had high rates of work-related illness, such as low back pain, workplace violence, shift work, needle stick injuries, high physical work load, and job stress31). Low back pain is one of the main problems affecting quality of life and work productivity as well as absenteeism pattern and disabilities in nursing4). These situations are similar to those in other hospital workers besides nurses. About 78% hospital workers have experienced low back pain and over 47% of them had difficulty in their work in our pilot survey of this study prior to the recruiting period (data not shown).
Mechanical, psychological, social factors play an important role in symptom onset and maintenance of non-specific low back pain32). Among mechanical factors, posture is considered to be a risk factor for non-specific low back pain32). Poor posture is a common finding in patients with a musculoskeletal complaint33). Postural balance is controlled by coordination of multiple segments in the kinetic chain from foot to head15). Because low back pain originates from various factors, ROM in major joints, such as the hip and shoulder, and spinal alignment was measured in this study. However, there were no significant differences in the spinal ROM and ROM in the hip between participants with severe or moderate low back pain with baseline characteristics after the recruitment period (Table 1). Participants had severe low back pain at the recruitment period but there remained a possibility to reduce the pain while waiting for the start of this study. The right shoulder flexion in the severe low back pain group had a significant increase, which could be explained by most of them being right handed, and they make lordosis to reduce low back pain, which results in internal rotation of the right scapula17). This scapular kinematics seem to influence the shoulder ROM. There were no significant differences in the spinal motion, expect for the lumbar ROM, and ROM in the hip and shoulder between the experimental and control groups at the final follow-up. This seems to be explained by a small sample size and follow-up periods were limited. Not only the sagittal but also the coronal alignment should be considered in future analyses.
Lumbopelvic complex has ROM of 110° (40° in the lumbar spine and 70° in the hip joint) and participants with low back pain had more lumbar segment motion than the pelvis during forward bending of the trunk as compared with those without low back pain34). A repetitive and sustained flexed posture may lead to impaired spinal muscle control35). Thus, greater lumbar motion can induce overloading of the lumbar spine and consequently low back pain36). The decrease in the lumbar ROM at the final follow-up may have a positive effect on the experimental group.
Low back pain is influenced by several factors32). Indices of depression and somatization had strong correlations with functional limitation by low back pain34). It is comprehensible that participants with severe low back pain had significantly higher VAS scores at baseline characteristics at the recruitment period. However, there were no significant differences of psychological distress (K6) or Athens Insomnia Scale, which have a relationship with depression, between participants with severe and moderate low back pain. Somatization seems to affect those with severe low back pain, which could explain an increase of subjective numbness on them. VAS scores in the experimental group were significantly lower as compared with those in the control group because two participants failed to start. However, VAS scores in the experimental group significantly decreased at the final follow-up. Furthermore, these effects had continued after 3 months after completion in the experimental group (data not shown). The Spinal Underwear had an effect of reducing low back pain and a decrease of lumbar ROM seems to be continuing after taking it off. SSAS scores significantly decreased in the experimental group and they seem to have a relationship with low back pain. Further study is needed to clarify these phenomena.
At the beginning of this study, the rates of subjective feeling of good posture were estimated to increase in the experimental group, because the Spinal Underwear stimulates tactile sense on the skin of the back while in poor postures. However, there was no significant difference between the two groups. As the height in the experimental group was not changed at the final follow-up, effects of the Spinal Underwear seemed to be limited to restriction of the lumbar ROM. Follow-up periods were short and the sample size was quite small, which could make it difficult to detect the difference.
With regard to musculoskeletal symptoms, neck pain as well as low back pain significantly decreased in the experimental group. This phenomenon may also prove that musculoskeletal symptoms are influenced by several factors, such as postures and somatization34).
Previous studies have used various devices for postural monitoring having a problem with the trade-off between portability and accuracy of measurement37-39). The provision of constant postural feedback via audio feedback, such as the Spinal Underwear, decreased low back pain40). However, the Spinal Underwear has the advantage of keeping good posture through daily unconscious training without interference.
This study has several limitations. First, this study adopted prospective, randomized, open, blinded-endpoint method. Preferably, sham procedure (same underwear without NANO FRONT®) should be prepared. However, it was difficult to manufacture them. Further study with a strict blinded manner is needed. Second, ROM was measured only in the hip and shoulder. The other joints, such as the ankle, knee, and cervical ROM could be measured in further studies to prove the correlation between poor posture and low back pain. Third, evaluation of psychological factors was limited. Fourth, musculoskeletal symptoms were ambiguous. Fifth, the follow-up rate was not high. At last, we looked at the symptoms of low back pain, but the underlying pathology was not assessed.
Conclusion
This study demonstrated that a new wearable type lumbar support (Spinal Underwear) reduced VAS and SSAS scores, lumbar spinal ROM, low back pain, and neck pain. This lumbar support has a positive effect on reducing low back pain among healthcare workers.
Acknowledgments: The authors would like to acknowledge their valued help and efforts from nurse managers and the department of physical therapy staffs at Takeda General Hospital.
Conflicts of interest: The authors report no conflicts of interest.
References
- 1). Bernal D, Campos-Serna J, Tobias A, Vargas-Prada S, Benavides FG, Serra C. Work-related psychosocial risk factors and musculoskeletal disorders in hospital nurses and nursing aides: a systematic review and meta-analysis. Int J Nurs Stud 2015; 52 (2): 635-648. [DOI] [PubMed] [Google Scholar]
- 2). Waddell G. Biopsychosocial analysis of low back pain. Baillieres Clin Rheumatol 1992; 6 (3): 523-557. [DOI] [PubMed] [Google Scholar]
- 3). Roelofs PD, Bierma-Zeinstra SM, van Poppel MN, van Mechelen W, Koes BW, van Tulder MW. Cost-effectiveness of lumbar supports for home care workers with recurrent low back pain: an economic evaluation alongside a randomized-controlled trial. Spine (Phila Pa 1976) 2010; 35 (26): E1619-1626. [DOI] [PubMed] [Google Scholar]
- 4). Lipscomb J, Trinkoff A, Brady B, Geiger-Brown J. Health care system changes and reported musculoskeletal disorders among registered nurses. Am J Public Health 2004; 94 (8): 1431-1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5). Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord 2000; 13 (3): 205-217. [DOI] [PubMed] [Google Scholar]
- 6). Dillingham TR. Lumbar supports for prevention of low back pain in the workplace. JAMA 1998; 279 (22): 1826-1828. [DOI] [PubMed] [Google Scholar]
- 7). van Poppel MN, Hooftman WE, Koes BW. An update of a systematic review of controlled clinical trials on the primary prevention of back pain at the workplace. Occup Med (Lond) 2004; 54 (5): 345-352. [DOI] [PubMed] [Google Scholar]
- 8). Nachemson A, Morris JM. In vivo measurements of intradiscal pressure. Discometry, a method for the determination of pressure in the lower lumbar discs. J Bone Joint Surg Am 1964; 46: 1077-1092. [PubMed] [Google Scholar]
- 9). Nachemson A, Schultz A, Andersson G. Mechanical effectiveness studies of lumbar spine orthoses. Scand J Rehabil Med Suppl 1983; 9: 139-149. [PubMed] [Google Scholar]
- 10). Smedley J, Egger P, Cooper C, Coggon D. Prospective cohort study of predictors of incident low back pain in nurses. BMJ 1997; 314 (7089): 1225-1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11). Jellema P, Bierma-Zeinstra SM, Van Poppel MN, Bernsen RM, Koes BW. Feasibility of lumbar supports for home care workers with low back pain. Occup Med (Lond) 2002; 52 (6): 317-323. [DOI] [PubMed] [Google Scholar]
- 12). Saito H, Sekiguchi M, Yamada H, et al. Comparison of postural changes and muscle fatigue between two types of lumbar support: a prospective longitudinal study. Fukushima J Med Sci 2014; 60 (2): 141-148. [DOI] [PubMed] [Google Scholar]
- 13). Smedley J, Egger P, Cooper C, Coggon D. Manual handling activities and risk of low back pain in nurses. Occup Environ Med 1995; 52 (3): 160-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14). Heneweer H, Staes F, Aufdemkampe G, van Rijn M, Vanhees L. Physical activity and low back pain: a systematic review of recent literature. Eur Spine J 2011; 20 (6): 826-845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15). Dahl KD, Wang H, Popp JK, Dickin DC. Load distribution and postural changes in young adults when wearing a traditional backpack versus the BackTpack. Gait Posture 2016; 45: 90-96. [DOI] [PubMed] [Google Scholar]
- 16). Griegel-Morris P, Larson K, Mueller-Klaus K, Oatis CA. Incidence of common postural abnormalities in the cervical, shoulder, and thoracic regions and their association with pain in two age groups of healthy subjects. Phys Ther 1992; 72 (6): 425-431. [DOI] [PubMed] [Google Scholar]
- 17). Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys Ther 2000; 80 (3): 276-291. [PubMed] [Google Scholar]
- 18). Hagiwara Y, Yabe Y, Sugawara Y, et al. Influence of living environments and working status on low back pain for survivors of the Great East Japan Earthquake. J Orthop Sci 2016. [DOI] [PubMed] [Google Scholar]
- 19). Schmale AH. Giving up as a final common pathway to changes in health. Adv Psychosom Med 1972; 8: 20-40. [DOI] [PubMed] [Google Scholar]
- 20). Yabe Y, Hagiwara Y, Sekiguchi T, et al. Influence of living environment and subjective economic hardship on new-onset low back pain for survivors of the Great East Japan Earthquake. J Orthop Sci 2016. [DOI] [PubMed] [Google Scholar]
- 21). Hagiwara Y, Yabe Y, Sugawara Y, et al. Influence of living environments and working status on low back pain for survivors of the Great East Japan Earthquake. J Orthop Sci 2016; 21 (2): 138-142. [DOI] [PubMed] [Google Scholar]
- 22). Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep 2003; 26 (2): 117-126. [DOI] [PubMed] [Google Scholar]
- 23). Bohns VK, Wiltermuth SS. It hurts when I do this (or you do that): Posture and pain tolerance. Journal of Experimental Social Psychology 2012; 48 (1): 341-345. [Google Scholar]
- 24). Saito H, Sekiguchi M, Yamada H, et al. Comparison of postural changes and muscle fatigue between two types of lumbar support: a prospective longitudinal study. Fukushima J Med Sci 2014. [DOI] [PubMed] [Google Scholar]
- 25). Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res 2000; 48 (6): 555-560. [DOI] [PubMed] [Google Scholar]
- 26). Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 2002; 32 (6): 959-976. [DOI] [PubMed] [Google Scholar]
- 27). Suzukamo Y, Fukuhara S, Kikuchi S, et al. Validation of the Japanese version of the Roland-Morris Disability Questionnaire. J Orthop Sci 2003; 8 (4): 543-548. [DOI] [PubMed] [Google Scholar]
- 28). Nakao M, Tamiya N, Yano E. Gender and somatosensory amplification in relation to perceived work stress and social support in Japanese workers. Women Health 2005; 42 (1): 41-54. [DOI] [PubMed] [Google Scholar]
- 29). Huskisson EC, Jones J, Scott PJ. Application of visual-analogue scales to the measurement of functional capacity. Rheumatol Rehabil 1976; 15 (3): 185-187. [DOI] [PubMed] [Google Scholar]
- 30). Punnett L, Wegman DH. Work-related musculoskeletal disorders: the epidemiologic evidence and the debate. J Electromyogr Kinesiol 2004; 14 (1): 13-23. [DOI] [PubMed] [Google Scholar]
- 31). McNeely E. The consequences of job stress for nurses' health: time for a check-up. Nurs Outlook 2005; 53 (6): 291-299. [DOI] [PubMed] [Google Scholar]
- 32). Hopayian K, Notley C. A systematic review of low back pain and sciatica patients' expectations and experiences of health care. Spine J 2014. [DOI] [PubMed] [Google Scholar]
- 33). Hagiwara Y, Kanazawa K, Ando A, et al. Blood flow changes of the anterior humeral circumflex artery decrease with the scapula in internal rotation. Knee Surg Sports Traumatol Arthrosc 2014. [DOI] [PubMed] [Google Scholar]
- 34). Dionne CE. Psychological distress confirmed as predictor of long-term back-related functional limitations in primary care settings. J Clin Epidemiol 2005; 58 (7): 714-718. [DOI] [PubMed] [Google Scholar]
- 35). Parkinson RJ, Callaghan JP. The role of dynamic flexion in spine injury is altered by increasing dynamic load magnitude. Clin Biomech (Bristol, Avon) 2009; 24 (2): 148-154. [DOI] [PubMed] [Google Scholar]
- 36). Hasebe K, Sairyo K, Hada Y, et al. Spino-pelvic-rhythm with forward trunk bending in normal subjects without low back pain. Eur J Orthop Surg Traumatol 2014; 24 (Suppl 1): S193-199. [DOI] [PubMed] [Google Scholar]
- 37). Boocock MG, Jackson JA, Burton AK, Tillotson KM. Continuous measurement of lumbar posture using flexible electrogoniometers. Ergonomics 1994; 37 (1): 175-185. [DOI] [PubMed] [Google Scholar]
- 38). Holmes MW, Hodder JN, Keir PJ. Continuous assessment of low back loads in long-term care nurses. Ergonomics 2010; 53 (9): 1108-1116. [DOI] [PubMed] [Google Scholar]
- 39). Wong WY, Wong MS. Trunk posture monitoring with inertial sensors. Eur Spine J 2008; 17 (5): 743-753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40). Ribeiro DC, Sole G, Abbott JH, Milosavljevic S. The effectiveness of a lumbopelvic monitor and feedback device to change postural behavior: a feasibility randomized controlled trial. J Orthop Sports Phys Ther 2014; 44 (9): 702-711. [DOI] [PubMed] [Google Scholar]