ABSTRACT
Background:
Cirrhosis is a chronic and progressive disease that causes various complications for patients due to disturbance of the liver’s usual function. Self-efficacy refers to an individual’s belief in one’s ability to perform the necessary behaviors to achieve one’s goals. Self-management is also an important criterion for long-term change in behavior. The present study aimed to investigate the effect of self-management training on self-efficacy of patients suffering from liver cirrhosis.
Methods:
This randomized controlled clinical trial was conducted on 74 patients with liver cirrhosis randomly assigned to an intervention (receiving self-management training) and a control group (routine care) from 2012 to 2013. The data were collected in the transplantation center affiliated to Shiraz University of Medical Sciences. Self-management training was performed in six 90-minute sessions twice a week. Besides, the intervention group was followed up for a month via telephone. Levo self-efficacy questionnaire was filled out by the patients before, immediately after, and one month after the intervention. Then, the data were entered into the SPSS statistical software (v. 16) and analyzed using independent t-test, Chi-square test, and repeated measures ANOVA.
Result:
At the beginning of the study, no statistically significant difference was found between the two groups regarding self-efficacy (P=0.18). However, the total score of the questionnaire and those of all its dimensions significantly improved in the intervention group immediately and one month after training self-management skills (P<0.001). The mean score of self-efficacy was 102.24±7.79 and 76.78±9.49 in the intervention and control groups, respectively. On the other hand, no statistically significant difference was observed in the control group’s self-efficacy immediately and one month after the intervention (P=0.6).
Conclusion:
The results showed that the self-management program resulted in improvement of self-efficacy in the patients with liver cirrhosis. Therefore, this supportive strategy could be useful in patients with chronic illnesses for improvement of care and prevention of complications.
KEYWORDS: Self-management, Self-efficacy, Liver cirrhosis
INTRODUCTION
Cirrhosis is a chronic and progressive disease distributed by fibrosis and distinguished by nodules in the liver.1 As the seventh reason for death among 25-64-year-old American individuals, it is the final step of liver disease that affects the patients’ most important years of life.2 Alcohol overuse has been considered to be the most common cause of cirrhosis in the western world, but hepatitis B is the main reason for cirrhosis in developing countries, such as Iran.3 Approximately, 1.5 million individuals in Iran suffer from this type of hepatitis about 15-40% of whom are at risk of being affected with cirrhosis or hepatocellular carcinoma.4 Up to now, no studies have been done on the prevalence of cirrhosis in Iran.5 Cirrhosis is the third leading cause of digestive disease-related mortality in Iran.6 In addition, ascites is the most common complication of liver cirrhosis. Variceal hemorrhage and portal hypertension are common, as well.7
According to Baundura’s theory, self-efficacy refers to the confidence in one’s abilities to do self-care desirably. Promoting self-efficacy may lead to better outcomes of self-management, increase life expectancy, and modify health behaviors. Self-efficacy is also considered to be an important concept in managing chronic diseases.8
Self-management training causes the patients to actively participate in caring for themselves and increases their responsibility for controlling the symptoms and complications.9 Xi et al. conducted a study on the impact of application of self-management education on the rehabilitation process of liver transplant patients after discharge. The results showed that self-management, as a low-cost and effective method, could have a positive impact on these patients’ rehabilitation.10
Furthermore, Beg et al. revealed the positive effect of education on self-management of liver cirrhosis patients. They also stated that cirrhotic patients lacked the required knowledge to manage their disease.11
Similarly, Xing et al. carried out a research in China and reported the need for improvement of liver transplant patients’ self-management behaviors. Thus, the related experts were recommended to consider the targeted health education in order to promote these patients’ healthy lifestyles and improve their self-efficacy.12 The results of the study by Delsasso et al. also indicated low perceived self-efficacy in patients who were in the list of liver transplantation.13
Overall, review of the literature showed that self-management training was effective in patients with chronic conditions, such as asthma,14 diabetes,15 and chronic heart failure.16 The results of a previous study entitled “The effect of training self-management program on self-efficacy of patients suffering from multiple sclerosis” showed a significant difference in self-efficacy and its subscales, except for receiving help from others and contact with physician, immediately and two months after the intervention.17 However, studies on self-efficacy in patients with liver cirrhosis are scanty, and interventions to evaluate the effectiveness of a comprehensive self-management program in these patients have rarely been taken into consideration. Therefore, using a self-management program to achieve better outcomes and reduce the costs of patient care is useful and effective and can help control the symptoms and complications of the disease. Hence, the present study aimed to determine the effect of self-management on promoting self-efficacy in these patients.
MATERIALS AND METHODS
This randomized controlled trial was conducted on patients with liver cirrhosis who had referred to the transplantation center of Nemazee teaching hospital affiliated to Shiraz University of Medical Sciences, one of the major referral centers for liver disease and the only center for liver transplantation in the south of Iran. Data collection was performed from July until September 2013. Following the eligibility assessment, the patients were familiarized with the study and those who agreed to participate received a consent form to sign.
At first, 80 patients with liver cirrhosis were randomly assigned to an intervention (receiving self- management training) and a control group (routine care) through simple random sampling using the table of random numbers. The inclusion criteria of the study were being 18-60 years old, not suffering from other chronic diseases, and being able to write and read. On the other hand, the exclusion criteria were suffering from severe cirrhosis, death, and not being willing to cooperate during the research. For blinding the study, a researcher’s assistant was required to complete the questionnaires.
According to the study objectives, based on the results of the study performed by DalSasso-Mendes et al. in 2011(13), considering power=80%,d=2, α=0.05, S=3, β=0.20, and d=µ1-µ2=8.1-6.05=2.05, and using the following formula, a70-subject sample size was determined for the study (35 participants in each group):
The sample size was raised to 80 patients to compensate for the dropout. Overall, 86 subjects were assessed for eligibility. However, 6 subjects were excluded from the study because of unwillingness to participate (n=4) and other reasons (n=2). In the intervention group, three subjects were excluded due to liver transplantation (n=2) and unwillingness to continue participation in the study (n=1). Also, three participants in the control group were dropped out of the study because of liver transplantation (n=1), no reason (n=1), and death (n=1). Therefore, a total of 74 patients were enrolled into the study (37 in the intervention group and 37 in the control group). Diagram of the participants in this study are presented in figure 1.
Figure1.
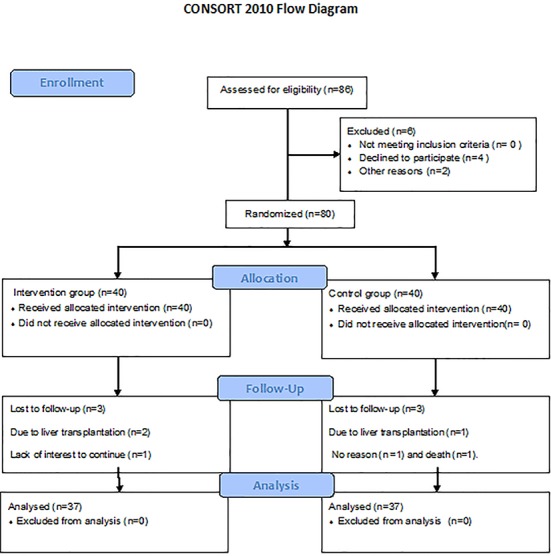
Study selection process
After the study protocol was approved by the research Ethics Committee of the University (No. 92-6567), the researcher referred to Nemazee transplantation center. After getting permission from the hospital’s authority, 86 participants were selected through purposive sampling. The patients were familiarized with the study and those who agreed to participate received a consent form to sign. The subjects were also ascertained about the confidentiality and anonymity of their information as well as their right to withdraw during the study. Numeric codes and publication data were used for anonymity of the participants.
The patients’ demographic and self-efficacy data were collected by questionnaires. The demographic and clinical characteristics form, which was collected at baseline, included information about the patients’ age, gender, marital status, education level, length of suffering from the disease, Child-Pugh score, frequency of hospitalization, and etiology of the disease.
In this study, self-management training was the independent variable, while self-efficacy was the dependent variable. Self-efficacy was assessed using Strategies Used by People to Promote Health(SUPPH) questionnaire.18 In a previous study conducted by Moattari et al. in Shiraz, this questionnaire was translated into Persian and back-translated into English to ensure its validity, which was further confirmed by a panel of experts. Then, they distributed the instrument among 30 representative patients for measurement of its reliability. The reliability of stress reduction, decision-making, and positive attitude dimensions in the original form was approved by Cronbach’s alpha coefficients of 0.89, 0.83, and 0.92, respectively.19
Self-management training was performed for the intervention group (two groups each containing twenty subjects) at the conference room of Nemazee hospital through six 90-minute sessions held twice a week. In the first three sessions, the patients received the necessary information about their disease (nature of cirrhosis, diet, and medication). In the second three sessions, they got familiar with problem-solving, decision-making, cognitive-behavioral techniques, and empowerment of positive attitude. During these sessions, cognitive errors were raised and some examples were presented. Then, the patients were encouraged to express their disease-related experiences and emotions. Meanwhile, their cognitive errors were determined and discussed. It is necessary to mention that 15 minutes of each session were allocated to training and performing relaxation methods. Muscle relaxation audio CDs were also prepared and given to the patients. The educational classes were held considering the patients’ cultural beliefs, previous interests, and knowledge levels. Indeed, the educational content was expressed through simple language, and one of the patients’ main family members was employed for facilitation of training. The educational intervention was carried out through lecture, group discussion, and question and answer methods. Additionally, the learning process was facilitated by teaching aids, such as PowerPoint, photos, and booklets. The control group, on the other hand, received the routine care without any interventions, but was provided with the educational booklet after the intervention. All the participants filled out the questionnaires in the conference room of Nemazee hospital one month after the intervention under supervision of the researcher and co-researcher.
All data analyses were performed using SPSS statistical software (version 16). Independent t-test and Chi-square test were used to assess the differences between the study groups regarding socio-demographic characteristics. Besides, comparison of the two groups was performed by repeated measures ANOVA at the end of the 4-week intervention period. P<0.05 were considered to be statistically significant. It should be noted that the data were analyzed by an individual who was blind to the study groups.
RESULTS
The results of Chi-square and independent t-test revealed no statistically significant difference between the two groups regarding qualitative and quantitative demographic variables (P>0.05) before the intervention. Therefore, the two groups were homogeneous in this regard (Table 1).
Table 1.
Socio-demographic characteristics of the participants in the intervention and control groups
| Socio-demographic characteristics | Intervention N (%) | Control N (%) | P value | |
|---|---|---|---|---|
| Sex | Female | 14 (35) | 12 (30) | 0.81* |
| Male | 26 (65) | 28 (70) | ||
| Marital status | Single | 10 (25) | 8 (20) | 0.70* |
| Married | 28 (70) | 31 (77.5) | ||
| Widowed | 2(5) | 1(2.5) | ||
| Education level | Primary school | 4 (10) | 2 (5) | 0.70* |
| Middle school | 10 (25) | 11 (27.5) | ||
| High school and above | 26 (65) | 27 (67.5) | ||
| Age | Mean age (years) | 41.6±13.8 | 41.37±12.02 | 0.99** |
Chi-Square test
independent t-test
Prior to the study, the mean score of self-efficacy was 74.62±6.10 in the intervention group and 76.78±5.38 in the control group, but the difference was not statistically significant (P=0.18). However, the results of ANOVA showed a significant difference between the intervention and control groups regarding the total score and the scores of all the dimensions of self-efficacy immediately and one month after the intervention (P<0.001). According to Table 2, after self-management training, the total score and the scores of all the subscales of self-efficacy significantly increased in the intervention group compared to the control group (P<0.05).
Table 2.
Comparison of the mean changes in self-efficacy at baseline and immediately and one month after the intervention in the intervention and control groups
| Variables | Time | Baseline (mean±SD) | Immediately after the intervention (mean±SD) | One month after the intervention (mean±SD) | P value | |
|---|---|---|---|---|---|---|
| Group | Within group* | Between group* | ||||
| Total self-efficacy | Intervention | 74.62±6.10 | 84.59±5.16 | 102.24±7.79 | <0.001 | <0.001 |
| Control | 76.78±5.38 | 77.76±6.33 | 76.78±9.49 | 0.60 | ||
| Stress reduction | Intervention | 25.05±4.23 | 29.62±2.88 | 35.59±3.20 | <0.001 | <0.001 |
| Control | 26.68±3.23 | 27.02±3.39 | 26.15±4.25 | 0.50 | ||
| Decision-making | Intervention | 8.81±2.81 | 9.75±2.25 | 12.32±2.04 | <0.001 | <0.001 |
| Control | 7.60±2.81 | 7.63±2.85 | 7.36±2.81 | 0.77 | ||
| Positive attitude | Intervention | 40.75±4.17 | 45.21±3.50 | 54.32±4.79 | <0.001 | <0.001 |
| Control | 42.50±4.30 | 43.10±4.22 | 43.26±5.39 | 0.57 | ||
Repeated measures ANOVA
DISCUSSION
The results of the present study showed that self-management training had positive effects on the total score and the scores of all the dimensions of self-efficacy immediately and one month after the intervention. This finding is consistent with that of the study conducted on patients with liver cirrhosis in New York in which nursing intervention led to promotion of these patients’ self-efficacy and knowledge.20 These results are also in line with those of most studies focusing on providing education to increase self-efficacy in other chronic diseases. For instance, a previous study on hypertensive patients showed a significant difference between the control and intervention groups concerning self-efficacy after self-management training.21 Similar results were also obtained in other studies.22,23
McGillion et al. (2007) conducted a clinical trial on 117 patients suffering from stable angina in Canada to investigate the effect of chronic angina self-management program on life quality, self-efficiency, and ability of self-management of angina pain control. The results showed that self-management training improved the total score of self-efficiency in the intervention group compared to the control group.24 Unsal et al. (2010) also performed a research entitled “Effect of Education on Perceived Self-Efficacy for Individuals with Arthritis” and indicated a positive relationship between training and self-efficiency promotion.25 However, no studies have been conducted on the effectiveness of self-management training in promotion of self-efficacy in patients with liver cirrhosis. Improvements in decision-making, stress reduction, and positive attitude in the current study could be attributed to the features of our self-management training program, including engagement of family members and healthcare providers in the problem-solving process. Additionally, the patients practiced Jacobson relaxation techniques, which might have caused a decrease in their stress. Relaxation techniques improved self-efficacy26 and relieved psychosocial distress in patients with chronic diseases.27 In contrast, Hamnes et al. carried out a study to determine the impact of self-management programs on self-efficacy of patients with fibromyalgia syndrome for 4 weeks (one week of intervention and three weeks of follow-up). The results showed that educational programs had no impact on the patients. Some limitations of that study included the intensive intervention and lack of attention to patients’ motivation.28 Studies have shown that sharing experiences influenced successful self-management factors, while factors such as poor communications with healthcare providers and lack of knowledge were obstacles against the success of a self-management program.29-30 Hence, in the present study, efforts were made to support the patients and provide them with adequate information by creating group discussions and strengthening their positive abilities. On the other hand, the patients’ self-efficacy was improved by lengthening the duration of the intervention and follow-up period compared to the study by Hamnes.
Training intervention is one of the effective methods in modifying lifestyle, which is worthwhile in healthcare because it allows individuals to perform great changes and control their health. Nurses, as a part of the healthcare team who work in different centers in the society, play a key role as an important source of information for different society members. Therefore, using the results of the current research, we can design self-management training by nurses as a part of treatment in these patients and reduce their physical, mental, and social problems. Additionally, due to the weakness of the traditional education in terms of considering the active role of patients, nurses can apply the self-management program that is a non-invasive and low-cost method. Also, by encouraging the patients to participate more actively and feel more responsibility, they might take major steps towards improving the quality of their care.
One of the limitations of the present study was its short follow-up period after the intervention. Therefore, further longitudinal studies are recommended to be performed in this regard. Another study limitation was the small sample size, which limited the power of the research.
CONCLUSION
The findings of the present study indicated that self-management training improved the self-efficacy of the patients with liver cirrhosis. Accordingly, self-management training had a positive impact on reduction of the patients’ physical, mental, and social problems. Yet, further studies are recommended to assess the effect of self-management training on the patients with liver cirrhosis in longer time periods.
ACKNOWLEDGEMENT
This manuscript was extracted from Maryam Ghadami’s M.Sc. thesis in nursing, which was financially supported by the Research Vice-chancellor of Shiraz University of Medical Sciences (grant No. 92-6567). Hereby, the authors would like to thank Shiraz University of Medical Sciences and the healthcare providers in the transplantation center for their assistance. They also wish to acknowledge all the 74 study participants for contributing their time and effort to this study. Thanks also go to Ms. A. Keivanshekouh at the Research Improvement Center of Shiraz University of Medical Sciences for improving the use of English in the manuscript.
Conflict of Interest:None declared.
REFRENCES
- 1.Black JM, Hawks JH. Medical-Surgical Nursing: Clinical Management for Positive Outcomes. 8th ed. USA: Saunders; 2008. [Google Scholar]
- 2.Hansen L, Sasaki A, Zucker B. End-stage liver disease: challenges and practice implications. The Nursing Clinics of North America. 2010;45:411–26. doi: 10.1016/j.cnur.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 3.Forootan H, Hosseini A, Esteghamati AR, et al. Hypothalamic-pituitary-gonadal axis in cirrhotic patients in Imam Khomeini Hospital, Tehran. Iranian Journal of Endocrinology and Metabolism. 2001;3:23–30. [In persian] [Google Scholar]
- 4.Alavian SM, Hajarizadeh B, Ahmadzad-ASL M, et al. Hepatitis B virus infection in Iran: A systematic review. Hepatitis Montly. 2008;8:281–94. [Google Scholar]
- 5.Ganji A, Malekzadeh F, Safavi M, et al. Digestive and liver disease statistics in Iran. Middle East Journal of Digestive Diseases. 2009;1:56–62. [Google Scholar]
- 6.Khademolhosseini F, Malekhosseini S, Salahi H, et al. Outcome and characteristics of patients on the liver transplant waiting list: Shiraz experience. Middle East Journal of Digestive Diseases. 2009;1:63–7. [Google Scholar]
- 7.Elfaki A. Aetiology, complications, and preventive measures of Liver cirrhosis; Elobeid hospital; West Sudan. Sudan Journal of Medical Sciences. 2008;3:25–8. [Google Scholar]
- 8.Frei A, Svarin A, Steurer-Stey C, Puhan MA. Self-efficacy instruments for patients with chronic diseases suffer from methodological limitations-a systematic review. Health and Quality of Life Outcomes. 2009;7:86. doi: 10.1186/1477-7525-7-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nolte S, Elsworth GR, Sinclair AJ, Osborne RH. The extent and breadth of benefits from participating in chronic disease self-management courses: a national patient-reported outcomes survey. Patient Education and Counseling. 2007;65:351–60. doi: 10.1016/j.pec.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 10.Shu-hua X, Pei-fang Z, Rong H. The application of self-management education in the rehabilitation process of liver transplant patients after discharge. Chinese Journal of Nursing. 2010;3:010. [Google Scholar]
- 11.Beg S, Curtis S, Shariff M. Patient education and its effect on self-management in cirrhosis: a pilot study. European Journal of Gastroenterology & Hepatology. 2016;28:582–7. doi: 10.1097/MEG.0000000000000579. [DOI] [PubMed] [Google Scholar]
- 12.Xing L, Chen QY, Li JN, et al. Self-management and self-efficacy status in liver recipients. Hepatobiliary & Pancreatic Diseases International. 2015;14:253–62. doi: 10.1016/s1499-3872(15)60333-2. [DOI] [PubMed] [Google Scholar]
- 13.Sasso-Mendes K, da Costa Ziviani L, Rossin FM, et al. Perceived self-efficacy among liver transplant candidates and recipients. Gastroenterology Nursing. 2011;34:236–41. doi: 10.1097/SGA.0b013e31821b47c3. [DOI] [PubMed] [Google Scholar]
- 14.Jones MA. Asthma self-management patient education. Respiratory Care. 2008;53:778–86. [PubMed] [Google Scholar]
- 15.Powers MA, Bardsley J, Cypress M, et al. Diabetes Self-management Education and Support in Type 2 Diabetes A Joint Position Statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. J Acad Nutr Diet. 2015;115:1323–34. doi: 10.1016/j.jand.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 16.Meng K, Musekamp G, Seekatz B, et al. Evaluation of a self-management patient education program for patients with chronic heart failure undergoing inpatient cardiac rehabilitation: study protocol of a cluster randomized controlled trial. BMC Cardiovascular Disorders. 2013;13:60. doi: 10.1186/1471-2261-13-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kafami F. The effective of selfmanagment program on self efficacy and health position in MS patients [Thesis] Tehran (Iran): Iran univ of Welfare and Rehabilitation Sci; 2009. [Google Scholar]
- 18.Rambod M, Rafei F, Hossini F. Quality of life in patients with chronic renal failure. Hayat. 2008;14:51–61. [In persian] [Google Scholar]
- 19.Moattari M, Ebrahimi M, Sharifi N, Rouzbeh J. The effect of empowerment on the self-efficacy, quality of life and clinical and laboratory indicators of patients treated with hemodialysis: a randomized controlled trial. Health and Quality of Life Outcomes. 2012;10:115. doi: 10.1186/1477-7525-10-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Delair S, Feeley TH, Kim H, et al. A peer-based intervention to educate liver transplant candidates about living donor liver transplantation. Liver Transplantation. 2010;16:42–8. doi: 10.1002/lt.21937. [DOI] [PubMed] [Google Scholar]
- 21.Savadkooh OK, Zakerimoghadam M, Gheyasvandian S, Kazemnejad A. Effect of Self-Management Program onSelf-Efficacy in Hypertensive Patients. Journal of Mazandaran Univercity of Medical Sciences. 2012;22:19–28. [In persian] [Google Scholar]
- 22.Baljani E, Rahimi J, Amanpour E, et al. Effect of a nursing intervention on improving self-efficacy and redusing cardiovascular risk factor in patients with cardiovascular diseases. Hayat. 2011;17:45–54. [In persian] [Google Scholar]
- 23.Kim M, Song M. Effects of Self-management Program applying Dongsasub Training on Self-efficacy, Self-esteem, Self-management Behavior and Blood Pressure in Older Adults with Hypertension. Journal of Korean Acad Nurs. 2015;45:576–86. doi: 10.4040/jkan.2015.45.4.576. [DOI] [PubMed] [Google Scholar]
- 24.McGillion MH, Watt-Watson J, Stevens B, et al. Randomized controlled trial of a psychoeducation program for the self-management of chronic cardiac pain. Journal of Pain and Symptom Management. 2008;36:126–40. doi: 10.1016/j.jpainsymman.2007.09.015. [DOI] [PubMed] [Google Scholar]
- 25.Unsal A, Kasikci MK. Effect of education on perceived self-efficacy for individuals with arthritis. International Journal of Caring Science. 2010;3:3–11. [Google Scholar]
- 26.Diezemann A. Relaxation techniques for chronic pain. Schmerz (Berlin, Germany) 2011;25:445–53. doi: 10.1007/s00482-011-1019-2. [DOI] [PubMed] [Google Scholar]
- 27.Yu DS, Lee DT, Woo J. Effects of relaxation therapy on psychologic distress and symptom status in older Chinese patients with heart failure. Journal of Psychosomatic Research. 2007;62:427–37. doi: 10.1016/j.jpsychores.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 28.Hamnes B, Mowinckel P, Kjeken I, Hagen KB. Effects of a one week multidisciplinary inpatient self-management programme for patients with fibromyalgia: a randomised controlled trial. BMC Musculoskeletal Disorders. 2012;13:189. doi: 10.1186/1471-2474-13-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hamnes B, Hauge MI, Kjeken I, Hagen KB. I have come here to learn how to cope with my illness, not to be cured’: A Qualitative Study of Patient Expectations Prior to a One-Week Self-Management Programme. Musculoskeletal Care. 2011;9:200–10. doi: 10.1002/msc.212. [DOI] [PubMed] [Google Scholar]
- 30.Jerant AF, von Friederichs-Fitzwater MM, Moore M. Patients’ perceived barriers to active self-management of chronic conditions. Patient Education and Counseling. 2005;57:300–7. doi: 10.1016/j.pec.2004.08.004. [DOI] [PubMed] [Google Scholar]


