Abstract
Background/Aims
Inflammatory bowel disease (IBD), including Crohn's disease (CD) and ulcerative colitis (UC), has been reported to have various ophthalmologic manifestations. The aim of this study was to evaluate the prevalence of ophthalmologic manifestations associated with IBD in Korea.
Methods
Sixty-one patients were examined between May 2013 and October 2014. We performed complete ophthalmologic examinations.
Results
Findings included 36 patients with CD and 25 with UC. The mean age of the patients was 34±16 years and disease duration was 45.3±23.9 months. Ophthalmologic manifestations were positive in 44 cases. Primary complication was diagnosed in 5 cases, as follows; iritis in 2 cases, episcleritis in one case, iritis with optic neuritis in 1 case, and serous retinal detachment in 1 case, without secondary complications. The most common coincidental complication was dry eye syndrome (DES), in 35 patients (57.4%). The prevalence of DES in the control group was 21.3%. The proportion of DES in patients with IBD was significantly higher than in the control group (P=0.002).
Conclusions
Ophthalmologic manifestations were high (72.1%) in IBD patients. Clinically significant primary ocular inflammation occurred in 8.2% of patients. The most common complication was DES. There was a higher rate of DES in patients with IBD compared to the control group. Evaluation of the eye should be a routine component in patients with IBD.
Keywords: Inflammatory bowel disease; Crohn disease; Colitis, ulcerative; Ophthalmology; Dry eye syndromes
INTRODUCTION
Inflammatory bowel disease (IBD) is a chronic disease of unknown cause.1 The prevalence of IBD is higher in North America and Northern Europe, but the incidence and prevalence of IBD has been increasing rapidly in Asia associated with urbanization.1,2,3,4 Extraintestinal manifestations can occur in the skin, joint, liver, and eye.1,2
Ophthalmologic complications have been reported with an incidence of 3.5% to 43%.2,5,6,7,8,9 The complications of CD occur frequently.5,6,7,8 Ophthalmologic complications can be divided into primary, secondary, and coincidental complications.2 Primary complication is related to disease activity, and the condition improved following steroid therapy or surgical treatment. Secondary complications occurred as a result of the primary complications, such as steroid-induced cataract or scleromalacia following scleritis. Coincidental complications include conjunctivitis or dry eye syndrome (DES) found during the regular eye examination, though patients have no prior history of ophthalmologic symptoms. Ophthalmologic complications that are currently recognized include episcleritis, scleritis, cataract, secondary glaucoma, uveitis, and optic neuritis.7,8
Taylor et al.9 reported that the most common complications are episcleritis, scleritis, and uveitis. Episcleritis occurs in 29% of cases and is the index of disease activity. Scleritis occurs in 18% of cases and uveitis in 17% of cases. Another study reported that episcleritis occurs in 7.7% of cases, uveitis in 11.5% of cases, retinal pigment epithelial detachment in 11.5% of cases and optic neuritis in 3.8% of cases.6 Coincidental DES was found in 50.0% of cases, steroid induced cataract in 30.7% of cases, and conjunctivitis in 3.8% of cases.6
However, the above reports are the result of research in Western countries and, to our knowledge, this study is the first study of its type with Korean patients. Therefore, the aims of the study were to investigate ophthalmologic manifestations in patients with CD and UC in Jeju Island, South Korea, and to determine the necessity of routine eye examination. This is a prospective cross-sectional study of a single institution.
METHODS
1. Patients Selection
Patients diagnosed with IBD in hospital or outpatient clinic in Division of Gastroenterology between May 2013 and October 2014 were examined in this prospective cross-sectional study. The subjects were included regardless of ocular symptom. Informed consent was obtained from all patients. We surveyed the patients' sex, age, past history, diagnosis of IBD, disease duration, medical treatments, ophthalmologic manifestations or complications and ophthalmologic treatments. All protocols were approved by the Institutional Review Board (IRB) at Jeju National University Hospital (IRB number: 2013-05-011), Jeju, South Korea.
2. Diagnosis of IBD
Four gastroenterologists in Jeju National University Hospital diagnosed IBD according to patients' clinical symptoms, endoscopy findings, imaging and histological examination. CD activity is classified according to CDAI by National Cooperative Crohn's Disease Study.10,11 UC is classified according to the Mayo score or the partial Mayo score.12,13
3. Ophthalmologic Examination Protocol
One ophthalmologist (H.J.L.) investigated patients' medical and ophthalmologic history and performed the ophthalmologic examinations with consistent testing methods and equipment. Cases including previous ocular trauma and eye surgery including refractive surgery were excluded from this study.
Every patient was measured for uncorrected visual acuity and corrected visual acuity with an early treatment of diabetic retinopathy study (ETDRS) 4-meter visual acuity chart (ETDRS chart R®; Precision Vision, La Salle, USA). They were also measured in each eye for intraocular pressure by non-contact tonometer (KT 800®; Kowa, Tokyo, Japan). Slit lamp biomicroscopic examination was performed on the eyelid, cornea, conjunctiva, sclera, episclera, anterior chamber, lens, and anterior vitreous state. Using non-mydriatic fundus camera (VX 10®; Kowa), the shape and color of the optic nerve and retina were examined. The presence of chorioretinitis, retinal detachment, and retinal pigment epithelium abnormalities were also assessed. When abnormalities of the retina or optic nerve were suspected because of atypical findings in the fundus, mydriatics were instilled in both eyes, and the retina was re-examined with indirect ophthalmoscopy. As needed, fluorescein angiography (Visucam NM/FA®; Carl Zeiss Meditec, Thüringen, Germany) or optical coherent tomography (CirrusHD-OCT4000®; Carl Zeiss Meditec, Dublin, CA, USA) was performed to diagnose ophthalmologic disease. Direct pupillary light reflex was inspected using a swing flashlight test for relative afferent pupillary defect, and if needed, Ishihara color vision test (Ishihara's test for color deficiency, 24 plates edition® 2005; Kanehara & Co., Ltd., Tokyo, Japan) was performed to determine optic nerve dysfunction.
DES was diagnosed according to the criteria of The Korean Corneal Disease Study Group, which included: (1) subjective symptoms: dryness, foreign body sensation, pain, burning sensation, blurring; (2) objective findings: tear breakup time (TBUT) test less than 5 seconds or less than 5 mm on Schirmer test I, or the presence of corneal staining using fluorescent paper and severity of corneal epithelial punctate erosion based on Oxford grading.14,15 DES was diagnosed when there was at least one kind of subjective symptom and more than one objective finding.15 Diagnosis of DES was excluded if only subjective symptoms and no objective findings were present.
In testing for TBUT, fluorescein (Fluorescein Paper Strip®; Haag-Streit AG, Koeniz, Switzerland) was smeared into the lower fornix. The patient was asked to blink 3 times and then stop. The time between the last blink and the first appearance of a black spot on the cornea was measured using slit lamp biomicroscopy with a cobalt blue filter setting. In this study, TBUT was measured twice and the average value was used.
Using the Schirmer test I, after asking the patient to look forward without topical anesthetic eye drops, 5 mm×35 mm-sized standard filter paper (Whatman filter paper no. 41) was folded 5 mm from one end and kept in the lower fornix at the junction of lateral third and medial two-thirds. The patient was asked to close their eyes. After 5 minutes, the paper was removed and the length of wetness was measured, using a pre-marked millimeter ruler.
If an ophthalmologic disease was present, treatment was applied and patients were re-examined to determine the improvement of the disease.
4. Setting the Control Group of DES
As previous reports revealed that patients with IBD had significantly high proportion of DES,6,16 in this study, the control group was set to compare the prevalence of DES between IBD patients and with a control group. The control group included patients with decreased visual acuity due to refractive errors, and patients for counseling of refractive surgery. No patients had a history of systemic disease accompanying DES, were taking medications that could cause DES, or had previously undergone ocular surgery. Medical and ophthalmologic history was assessed, and ophthalmologic examinations were performed on 61 patients in the control group using the same test method with the same diagnostic criteria as described.
5. Statistical Analysis
The data were analyzed using PASW Statistics 18.0 (IBM Corp., Armonk, NY, USA). Patients' age, sex, and the presence or absence of complications was expressed as average and percentage. Continuous variables were described as mean and SD, and paired Student t-test was used for comparison. The chi-square test (Fisher exact test was used for 5 or fewer patients) was used to compare for nominal variables. A P-value of less than 0.05 was considered statistically significant.
RESULTS
1. Patients
Among the 61 patients (37 males, 24 females) with IBD, CD was measured in 36 patients (59.0%), and UC was measured in 25 patients (41.0%). The mean age was 34 years (range, 13–77 years), and the average duration of the disease was 45.3 months (range, 2–264 months). The mean age of UC patients (44 years) was higher than that of CD patients (27 years), which was statistically significant (P=0.003). In this study, 36 patients (59.0%) were in remission, while 14 patients (23.0%) were mild and 11 patients (18.0%) were moderate to severe. There was no difference between CD and UC in the proportion of severity.
The proportion of azathioprine for treatment in patients with CD (77.8%) was higher than that in patients with UC (36.0%) (P=0.004). With the exception of age and usage of azathioprine, there was no statistically significant difference between the 2 groups (Table 1).
Table 1. Demographic Characteristics of 61 IBD Patients Who Underwent Ophthalmologic Examination.
| Characteristic | Total (n=61) | CD (n=36) | UC (n=25) | P-value |
|---|---|---|---|---|
| Age (yr) | 34±16 | 27±13 | 44±15 | 0.003 |
| Male sex | 37 (60.7) | 25 (69.4) | 12 (48.0) | 0.092 |
| Disease duration (mo) | 45.3±23.9 | 37.1±20.3 | 57.2±32.7 | 0.102 |
| Disease activitya | ||||
| Remission | 36 (59.0) | 23 (63.9) | 13 (52.0) | 0.353 |
| Mild | 14 (23.0) | 10 (27.8) | 4 (16.0) | 0.362 |
| Moderate | 10 (16.4) | 3 (8.3) | 7 (28.0) | 0.075 |
| Severe | 1 (1.7) | 0 | 1 (4.0) | 0.410 |
| Treatment | ||||
| 5-ASA | 56 (91.8) | 34 (94.4) | 22 (88.0) | 0.374 |
| Corticosteroid | 29 (47.5) | 16 (44.4) | 13 (52.0) | 0.557 |
| Azathioprine | 37 (60.7) | 28 (77.8) | 9 (36.0) | 0.004 |
| Infliximab | 10 (16.4) | 6 (16.7) | 4 (16.0) | 0.935 |
| No. of patients with ocular manifestations | 44 (72.1) | 25 (69.4) | 19 (76.0) | 0.571 |
| Ocular treatmentb | 24 (39.3) | 13 (36.1) | 11 (44.0) | 0.398 |
Values are presented as mean±SD or number (%).
aCD, CDAI; UC, Mayo or partial Mayo score.
bNeed for ocular treatment at the initial presentation.
5-ASA, 5-aminosalicylic acid.
2. Ophthalmologic Manifestations
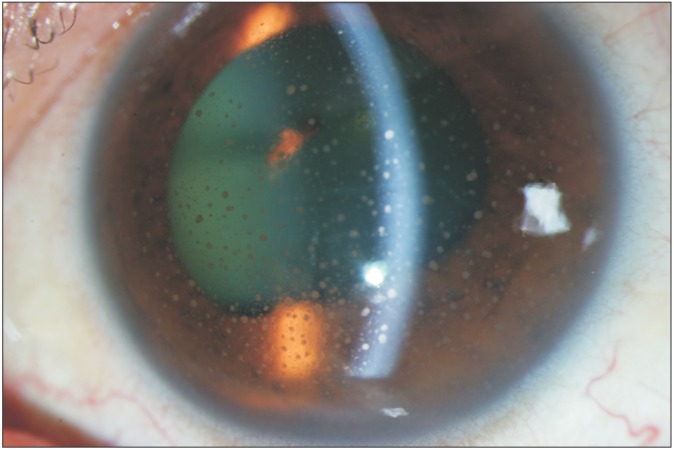
Ophthalmologic manifestations in patients with IBD were found in 44 patients (72.1%, 25 CD and 19 UC). Sixteen patients had more than 1 ocular manifestation. Twenty-five patients were male and, 19 patients were female. There were no differences in the frequency of accompanying ocular manifestations between CD and UC. The most common primary complication that could cause ocular pain or loss of vision was iritis which appeared in 3 cases, followed by episcleritis in 1 patient, optic neuritis in 1 patient, and serous retinal detachment in 1 case (Table 2). All 3 patients with iritis had monocular iritis; one, a 76-year-old woman with UC, had monocular iritis. However, we suspected that the iris pigments were observed from the anterior surface of the lens in both eyes were the cause of chronic alternating iris inflammation (Fig. 1). One patient had both iritis and optic neuritis, therefore, 5 patients (8.2%) were diagnosed with primary complication. There was no patient with secondary complication in this study. The most common coincidental complication was DES appearing in 35 patients, followed by blepharitis in 15 patients, incidentally found cataract in 4 patients, and chorioretinal scar, which was the suspected cause of prior chorioretinitis in 3 patients.
Table 2. Ophthalmologic Manifestations of IBD Patients.
| Total (n=61) | CD (n=36) | UC (n=25) | P-value | |
|---|---|---|---|---|
| Primary complication | ||||
| Iritis | 3 (4.9) | 2 (5.6) | 1 (4.0) | 1 |
| Episcleritis | 1 (1.6) | 1 (2.8) | 0 | 1 |
| Optic neuritis | 1 (1.6) | 1 (2.8) | 0 | 1 |
| Serous RD | 1 (1.6) | 0 | 1 (4.0) | 0.407 |
| Coincidental complication | ||||
| Dry eye syndrome | 35 (57.4) | 20 (55.6) | 15 (60.0) | 0.731 |
| Blepharitis | 15 (24.6) | 7 (19.4) | 8 (32.0) | 0.258 |
| Cataract | 4 (6.6) | 2 (5.6) | 2 (8.0) | 1 |
| Chorioretinal scar | 3 (4.9) | 1 (2.8) | 2 (8.0) | 0.556 |
Values are presented as number (%).
RD, retinal detachment.
Fig. 1. Anterior segment photograph of a 76-year-old female patient with UC. This picture shows severe iritis in the left eye.
3. Dry Eye Syndrome
Thirty-five patients with IBD (57.4%) were diagnosed with DES. Twenty patients had CD and, 15 patients had UC. In the control group, 13 patients (21.3%) were diagnosed with DES. There was no statistically significant difference between the patients with IBD and the control group in terms of age and sex ratio (Table 3). However, the proportion of DES in case of IBD was statistically significant higher than in the control group (57.4% vs. 21.3%, P=0.002).
Table 3. Comparison of Dry Eye Syndrome between IBD Patients and Healthy Control Groups.
| IBD (n=61) | Control (n=61) | P-value | |
|---|---|---|---|
| Age (yr) | 35±15 | 33±10 | 0.506 |
| Male sex | 37 (60.7) | 30 (49.2) | 0.275 |
| Prevalence | 35 (57.4) | 13 (21.3) | 0.002 |
Values are presented as mean±SD or number (%).
4. Ophthalmologic Treatments
Ocular treatments at the time of initial presentation were needed for 24 patients (13 CD and 11 UC, 15 male and 9 female). The mean age of these patients was 35 years. Three of these patients used steroid eyedrops for the treatment of primary complication such as iritis or episcleritis. Six of 8 patients with blepharitis had DES and they were treated with both antibiotic eyedrops and artificial tears (Table 4).
Table 4. Treatments of Ophthalmologic Complications.
| No. of patients (%) | Treatment | |
|---|---|---|
| Primary complication | ||
| Iritis | 2 (4.5) | Steroid eyedrops |
| Episcleritis | 1 (2.3) | Steroid eyedrops |
| Coincidental complication | ||
| Dry eye syndrome | 19 (43.2) | Artificial tears |
| Blepharitis | 8 (18.2) | Antibiotic eyedrops |
DISCUSSION
Prevalence of IBD is higher in Western countries, but in recent years, the incidence of IBD has been increasing in South Korea.4 Because of the unknown cause and pathophysiology of the disease, it is fairly difficult to determine the correlation between IBD and ophthalmologic complications associated with specific ophthalmologic disease.16,17 Several studies in countries outside of Asia have reported ophthalmologic complications with an incidence of 3.5% to 43%.5,6,7,8,9 Only a few studies were performed in a single center (Table 5).6,16,18 The results of those single center studies, including the present study, were divided into primary, secondary, and coincidental complications , as in the case of Knox et al.2
Table 5. Comparison of Ophthalmologic Complications among Single Center Studies.
| Author (year) | Country | No. of patients (CD/UC) | Male sex (%) | Average age (yr) | Ocular complication (%) | Most common complication | DES in IBD (%) | No. of controls | DES in control (%) |
|---|---|---|---|---|---|---|---|---|---|
| Felekis et al. (2009)6 | Greece | 60 (23/37) | 53 | 50 | 43 | DES | 22 | 276 | 11 |
| Cury and Moss (2010)16 | Brazil | 88 (48/40) | 38 | 41 | 59 | DES | 43 | 24 | 12 |
| Yilmaz et al. (2007)18 | Turkey | 116 (20/96) | 60 | 41 | 29 | Conjunctivitis | NA | NA | NA |
| Current study | South Korea | 61 (36/25) | 61 | 34 | 72 | DES | 57 | 61 | 21 |
DES, dry eye syndrome; NA, not applicable.
Felekis et al.6 conducted a study in Greece with 60 patients who had IBD and 26 patients (43%) had eye complications (14 CD and 12 UC, 12 male and 14 female). The most common primary complications, as in the case of Knox et al.,2 were iritis and retinal pigment epithelium detachment in 5.0% of cases, which was followed by episcleritis in 3.3% of cases, serous retinal detachment in 3.3% of cases and optic neuritis in 1.7% of cases. Secondary complications of steroid-induced cataract were observed in 8 cases (13.3%). Compared to this, the Greek study showed a higher incidence of primary and secondary complications than the in the present study. DES was the most common coincidental complication, as found in 13 of 26 patients (50%). In 276 persons of the control group (90 male, 186 female; average age, 51.9 years), the prevalence of DES was 11%. The prevalence of DES in patients with IBD was higher than that of the control group.
In a Brazilian study, 112 patients including 24 patients in the control group were enrolled in a community-based cohort study by Cury and Moss.16 Primary complications, including uveitis in 1.8% of cases and episcleritis in 0.9% of cases, were found. Forty-three percent of the patients with IBD were diagnosed with DES compared to the control group, where it occurred in 12% of cases. The research hypothesized that the use of 5-aminosalicylic acid (ASA) exceeding 3 g per day might be associated with the high prevalence of DES. In this study, 5-ASA was used in 91.8% of cases, but it was difficult to prove an association with DES because of its cross-sectional nature. In another prospective study undertaken in Turkey, 116 patients with IBD were given ophthalmological examinations every month for 12 months.18 Thirty-four patients (29.3%) had ophthalmologic complications, which appeared often in CD (CD 60.0%, UC 22.9%) patients. The most common primary complication was uveitis in 5.2% of patients followed by episcleritis in 3.5% of patients. Cataracts were observed as a secondary complication in 5.2% of patients. The coincidental complication was conjunctivitis in 8.6% of patients, followed by blepharitis in 6.9% of patients. A survey for DES was not conducted.
In this study, 61 patients were targeted, and 61 were recruited as a control group for DES. Forty-four patients (72.1%) had ophthalmologic manifestations, a higher incidence compared to other studies.6,7,18 Primary complications were diagnosed in 5 cases (8.2%), iritis in 2 cases (3.3%), episcleritis in 1 case (1.6%), both iritis and optic neuritis in 1 case (1.6%) and serous retinal detachment in 1 case (1.6%). In addition to this, 3 patients had chorioretinal scarring, which caused us to suspect this as the cause of the history of chorioretinitis, while another 3 patients (4.9%) showed iris pigments on the anterior lens surface without active inflammation in the anterior chamber, with suspected history of iritis. If this was a large cohort study, the prevalence of primary complications might be higher.
However, secondary ophthalmologic complications, such as steroid-induced cataract, glaucoma, or scleromalacia, were not found. It can be speculated that the small number of patients with a short follow-up period result from the prospective cross-sectional study. This may also have been due to the small number of patients using corticosteroids (29, 47.5%) with short-term use and mild disease activity.
The most common coincidental complication was DES in 35 patients (57.4%), followed by blepharitis in 24.6% of cases. There was no difference between CD and UC with regard to the incidence of ophthalmologic complications (Table 2). Four patients, coincidentally-diagnosed with cataracts, did not include steroid-induced posterior subcapsular cataract: 3 patients with senile nucleosclerosis and 1 patient with anterior cortical cataract. Jobling and Augusteyn19 emphasized that care should be taken when using steroids because steroid-induced cataracts tend to occur in proportion to the total amount of corticosteroid. In children, in particular, at lower amounts of steroid, steroid-induced cataracts occurred faster. Therefore, when using corticosteroids in patients with IBD, the possibility of cataracts should be explained and regular eye examinations should be recommended.
The incidence of DES in this study was similar to other studies (43%–50%).6,16 It is important to note the interpretation of the results concerning the incidence of DES, as the diagnostic criteria for each study were slightly different from one other. In the Greek study, 3 ophthalmologic examinations were performed: (1) 10 seconds or less in TBUT, (2) more than 3 points after staining with Rose Bengal dye, and (3) less than 5.5 mm after 5 minutes in the Schirmer test I. In that study, DES was defined as abnormal if any of the 3 above were found.6 In Brazil, abnormality was defined as 10 seconds or less in TBUT, more than 3 points after staining with Rose Bengal dye, less than 10 mm after 5 minutes in the Schirmer test I. DES was diagnosed when 2 or more of the above were found. However, the Brazilian study had a problem in the small number (only 24 participants) of the control group.16 Although the diagnostic criteria in this study were more stringent than in the previous 2 reports,6,16 the prevalence of DES in control group appeared as 11% in Greece,6 12% in Brazil,16 and 21% in this study. Comparatively, the Korean study appeared to have a relatively high proportion of DES. However, the control group included persons who were examined for refractive surgery and typically had used contact lenses previously. DES can be induced by contact lenses, so there might be a selection bias, which caused the error to be exaggerated.
To date, episcleritis, scleritis and iritis have been known to occur in association with disease activity of IBD according to previous studies.3,4,6,9 Among 5 patients with primary complication in this study, 1 patient with episcleritis and, 2 of 3 patients with iritis had mild disease activity, while another patient with both iritis and optic neuritis was in a state of remission. Only 1 patient with serous chorioretinal detachment in UC had severe disease activity (Table 6). Cury and Moss's research16 demonstrated a rate of 1.8% of uveitis and 0.9% of episcleritis, though the patients who ranked over 250 on the CDAI with CD and moderate or severe in Truelove and Witt's activity with UC totaled 59% of all patients. In this study, most primary complication occurred in patients in remission or with mild disease activity.
Table 6. Primary Ocular Complications According to IBD Activity.
| CD according to CDAI (n=36) | No. of CD patients | UC according to Mayo or partial Mayo score (n=25) | No. of UC patients | |
|---|---|---|---|---|
| Remission | 1 With iritis and optic neuritis | 23 | 0 | 13 |
| Mild | 1 With episcleritis, 1 with iritis | 10 | 1 With iritis | 4 |
| Moderate | 0 | 3 | 0 | 7 |
| Severe | 0 | 0 | 1 With serous retinal detachment | 1 |
This study has some limitations. The number of patients with IBD was insufficient. Patient disease activity was stabilized following long-term medication after being previously diagnosed in the division of gastroenterology. As UC patients tend toward a low percentage of admission, because symptoms of UC are mild, many patients without ocular symptoms often refused ophthalmologic tests. The annual incidence of Korean patients with IBD is 0.34 per 100,000 people in CD, and 3.08 persons in UC.4 The incidence of UC is greater than CD. However, in this study, the percentage of patients with CD was higher than that with UC. The results could be influenced by the high proportion of young patients, short average disease duration, short term follow-up duration, mild clinical aspects and good response to medication for IBD in Korean patients.17 A greater number of patients will be needed for long-term follow-up research with regular (defined as, every 1 or 2 months) eye examinations. Moreover, future research of the correlation between ophthalmologic complications and disease activity, prevalence of secondary complications, such as steroid-induced cataract or glaucoma, and the relevance of medication and ophthalmologic complication is necessary. In addition, further investigations of patients with ocular symptoms in the active phase should be conducted. Despite the limitations in this study, this is the first prospective cross-sectional study in a single center in South Korea.
In conclusion, ophthalmologic complications occurred in 72.1% of patients with IBD. Patients with IBD had primary complications that could cause ocular pain or visual loss in 8.2% of cases. There was no secondary complication. The most common coincidental complication was DES, the prevalence of which was higher than in the control group. Although DES rarely causes severe visual loss, it can cause ocular discomfort and a lower quality of life. By ocular examination and treatment, it is possible to reduce the symptoms of DES in IBD patients. Therefore, a thorough ophthalmologic examination at the time of diagnosis of IBD should be a routine component. In addition, regular ophthalmologic examination of patients without ocular symptoms can help prevent irreversible visual loss through early detection and treatment.
Footnotes
Financial support: This work was supported by the research grant of Jeju National University Hospital in 2013.
Conflict of interest: None.
References
- 1.Ernst BB, Lowder CY, Meisler DM, Gutman FA. Posterior segment manifestations of inflammatory bowel disease. Ophthalmology. 1991;98:1272–1280. doi: 10.1016/s0161-6420(91)32143-2. [DOI] [PubMed] [Google Scholar]
- 2.Knox DL, Schachat AP, Mustonen E. Primary, secondary and coincidental ocular complications of Crohn's disease. Ophthalmology. 1984;91:163–173. doi: 10.1016/s0161-6420(84)34322-6. [DOI] [PubMed] [Google Scholar]
- 3.Hu PJ. Inflammatory bowel disease in Asia: the challenges and opportunities. Intest Res. 2015;13:188–190. doi: 10.5217/ir.2015.13.3.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lee JW, Im JP, Cheon JH, Kim YS, Kim JS, Han DS. Inflammatory bowel disease cohort studies in Korea: present and future. Intest Res. 2015;13:213–218. doi: 10.5217/ir.2015.13.3.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghanchi FD, Rembacken BJ. Inflammatory bowel disease and the eye. Surv Ophthalmol. 2003;48:663–676. doi: 10.1016/j.survophthal.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 6.Felekis T, Katsanos K, Kitsanou M, et al. Spectrum and frequency of ophthalmologic manifestations in patients with inflammatory bowel disease: a prospective single-center study. Inflamm Bowel Dis. 2009;15:29–34. doi: 10.1002/ibd.20584. [DOI] [PubMed] [Google Scholar]
- 7.Vavricka SR, Schoepfer A, Scharl M, Lakatos PL, Navarini A, Rogler G. Extraintestinal manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2015;21:1982–1992. doi: 10.1097/MIB.0000000000000392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomas AS, Lin P. Ocular manifestations of inflammatory bowel disease. Curr Opin Ophthalmol. 2016;27:552–560. doi: 10.1097/ICU.0000000000000310. [DOI] [PubMed] [Google Scholar]
- 9.Taylor SR, McCluskey P, Lightman S. The ocular manifestations of inflammatory bowel disease. Curr Opin Ophthalmol. 2006;17:538–544. doi: 10.1097/ICU.0b013e3280109461. [DOI] [PubMed] [Google Scholar]
- 10.Winship DH, Summers RW, Singleton JW, et al. National Cooperative Crohn's Disease Study: study design and conduct of the study. Gastroenterology. 1979;77(4 Pt 2):829–842. [PubMed] [Google Scholar]
- 11.Sostegni R, Daperno M, Scaglione N, Lavagna A, Rocca R, Pera A. Review article: Crohn's disease: monitoring disease activity. Aliment Pharmacol Ther. 2003;17(Suppl 2):11–17. doi: 10.1046/j.1365-2036.17.s2.17.x. [DOI] [PubMed] [Google Scholar]
- 12.D'Haens G, Sandborn WJ, Feagan BG, et al. A review of activity indices and efficacy end points for clinical trials of medical therapy in adults with ulcerative colitis. Gastroenterology. 2007;132:763–786. doi: 10.1053/j.gastro.2006.12.038. [DOI] [PubMed] [Google Scholar]
- 13.Lewis JD, Chuai S, Nessel L, Lichtenstein GR, Aberra FN, Ellenberg JH. Use of the noninvasive components of the Mayo score to assess clinical response in ulcerative colitis. Inflamm Bowel Dis. 2008;14:1660–1666. doi: 10.1002/ibd.20520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea. 2003;22:640–650. doi: 10.1097/00003226-200310000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Hyon JY, Kim HM, Lee D, et al. Korean guidelines for the diagnosis and management of dry eye: development and validation of clinical efficacy. Korean J Ophthalmol. 2014;28:197–206. doi: 10.3341/kjo.2014.28.3.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cury DB, Moss AC. Ocular manifestations in a community-based cohort of patients with inflammatory bowel disease. Inflamm Bowel Dis. 2010;16:1393–1396. doi: 10.1002/ibd.21180. [DOI] [PubMed] [Google Scholar]
- 17.Kim ES, Kim WH. Inflammatory bowel disease in Korea: epidemiological, genomic, clinical, and therapeutic characteristics. Gut Liver. 2010;4:1–14. doi: 10.5009/gnl.2010.4.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yilmaz S, Aydemir E, Maden A, Unsal B. The prevalence of ocular involvement in patients with inflammatory bowel disease. Int J Colorectal Dis. 2007;22:1027–1030. doi: 10.1007/s00384-007-0275-1. [DOI] [PubMed] [Google Scholar]
- 19.Jobling AI, Augusteyn RC. What causes steroid cataracts? A review of steroid-induced posterior subcapsular cataracts. Clin Exp Optom. 2002;85:61–75. doi: 10.1111/j.1444-0938.2002.tb03011.x. [DOI] [PubMed] [Google Scholar]


