Abstract
Background
Advance directives and powers of attorney are increasingly common, yet data on their use in clinical situations remain sparse.
Methods
In this single center cross-sectional study, we collected data by questionnaire from 1004 intensive care patients in a university hospital. The frequencies of advance directives and powers of attorney were determined, and the factors affecting them were studied with multivariate logistic regression analysis.
Results
Usable data were obtained from 998 patients. 51.3% stated that they had prepared a document of at least one of these two kinds. Among them, 39.6% stated that they had given the relevant document(s) to the hospital, yet such documents were present in the patient’s hospital record for only 23%. 508 patients stated their reasons for preparing an advance directive or a power of attorney: the most common reason (48%) was the fear of being at other people’s mercy, of the lack of self-determination, or of medical overtreatment. The most important factors associated with a patient’s statement that he/she had prepared such a document were advanced age (advance directive: 1.022 [1.009; 1.036], p = 0.001; power of attorney: 1.027 [1.014; 1.040], p<0.001) and elective admission to the hospital (advance directive: 1.622 [1.138; 2.311], p<0.007; power of attorney: 1.459 [1.049; 2.030], p = 0.025). 39.8% of the advance directives and 44.1% of the powers of attorney that were present in the hospital records were poorly interpretable because of the incomplete filling-out of preprinted forms. Half of the patients who did not have such a document had already thought of preparing one, but had not yet done so.
Conclusion
For patients hospitalized in intensive care units, there should be early discussion about the presence or absence of documents of these kinds and early evaluation of the patient’s concrete wishes in critical situations. Future studies are needed to determine how best to assure that these documents will be correctly prepared and then given over to hospital staff so that they can take their place in the patient’s record.
In no area of medicine is progress so visible as in intensive care. Ever-improving machines, technology, new drugs, and invasive interventions are all features of any intensive care unit. The number of patients who are older, or have multiple comorbidities, is ever increasing. Intensive therapy must first and foremost align with the patient’s wishes; continuing to treat beyond reasonable limits, e.g., in a patient with an unfavorable long-term prognosis, should be avoided (1, 2).
Patients in intensive care are often so ill that it is impossible to explain invasive interventions to them and gain their consent. To maintain the individual’s right to self-determination beyond the acute setting, and, from the physician’s point of view, to avoid being open to a charge of legal assault, information must be provided to the patient about all further treatment measures (3). Normally, the patient is legally represented by a close relative or a professional health care proxy.
A medical power of attorney makes it unnecessary to employ a legally appointed proxy. A power of attorney that includes validity for medical decisions makes it possible to implement the patient’s wishes so far as they are known. Often, however, even the patient’s closest relatives are unable to say what the patient really wishes, or can do so only with some uncertainty. In one survey, for example, only 13% of relatives of 100 intensive care patients had ever discussed preferences regarding life-sustaining treatment with the patient (4). This dilemma can be avoided by setting up a patient advance directive describing the individual wishes of its creator.
According to a recent survey by a German opinion research institute (IfD Allensbach), 28% of German citizens now have an advance directive in place; the number has been rising steadily since 2009 (5). Among intensive care patients, too, powers of attorney and advance directives are becoming increasingly common. Up until now, only one German study (2009 to 2010) had investigated the prevalence of advance directives among intensive care patients. In this retrospective data analysis of deceased ICU-patients 12% had advance directives. However, the study did not assess any of the characteristics of the documents (6).
The aim of the present study was to collect data from the adult intensive care patient population about the frequency, characteristics, and factors influencing written statements of patients’ wishes before admission to hospital.
Methods
In this single-center cross-sectional study, between 1 November 2013 and 31 July 2014 a survey was carried out of adult patients treated in one of the 11 wards (132 beds) of the intensive care unit of the Hamburg-Eppendorf University Hospital, which had specialized wards for heart surgery, cardiology, internal medicine, neurosurgery, neurology, and surgery, in addition to five interdisciplinary wards. The study was approved by the ethics committee of the State Medical Association Hamburg (PV-4411).
All intensive care patients were screened every day. Inclusion criteria were: admission to any of the intensive care wards, age >18 years, and written consent to participate.
A condition of inclusion in the study was that the patients must be oriented in space, time, and their own person; i.e., they had to be capable of understanding a questionnaire that was administered immediately before they were moved to an ordinary ward. The patient’s suitability for participating had to be confirmed by the consultant physician on the ward and by the interviewer. The exclusion criteria are detailed in the eBox. The study was carried out by means of a questionnaire developed by ourselves, designed after extensive discussion with the director and senior consultants of the hospital and implemented after piloting on 70 patients. The items were evaluated by means of frequency analysis. The same person (C.R.) carried out all the interviews.
eBOX. Criteria for exclusion from the study.
Refusal to participate in the study
Age <18 years
Difficulties in communicating
-
Cognitive deficits, e.g., because of
Dementia
Delirium
Intellectual disability
Acute brain disorder, e.g., after trauma or insult with concomitant organic psychosyndrome
Psychiatric illness, e.g., acute psychosis
High-dose opioid therapy
Acute depressed mood, e.g., after receiving information about a tumor diagnosis on the day of transfer
Reduced general condition, e.g., before intended transfer to the palliative unit
Data analysis
Categorical variables were presented as absolute prevalences and percentages, while continuous variables were presented as means with standard deviations. The correlation between power of attorney or advance directive and age group was tested using the χ2, Fisher’s exact, and linear-by-linear association tests. Correlations between the influential factors ”admitting medical department,” “mode of admission (elective or emergency),” ”sex,” ”age,” “marital status,” “children,” ”history of disease (general),” ”history of specific disease (cardiac, pulmonary, neurologic, cancer),” ”medication consumption,” and “mode of life” (e.g., in a nursing home) and “presence of the documents” were tested using univariate and multivariate logistic regressional analysis. In multivariate regression analysis, all the influential factors listed above were included in the regression model in order to account for any confounding factors. Only datasets with values for all the variables were used (listwise deletion of missing cases). This corresponded to 958 cases; i.e., about 4% of cases were missing in the multivariate analysis. All analyses were carried out using SPSS Statistics version 23.0.
Results
Patient characteristics, admission mode, and admission diagnosis
Out of 5992 patients treated in intensive care in the hospital during the study period, 1049 were enrolled in the study, 45 of whom declined to take part. Of 1004 intensive care patients, 6 were unable to say whether they had set up a power of attorney or advance directive. Thus, data from 998 patients (16.7%) were analyzed (table 1).
Table 1. Patient characteristics.
| Patient characteristics | n (total 998) | % |
| Male | 569 | 57.0 |
| Age (years) (SD) | 62.7 ± 14.7 | |
| <30 years | 42 | 4.2 |
| >30–45 years | 86 | 8.6 |
| >45–65 years | 378 | 37.9 |
| >65–75 years | 306 | 30.7 |
| >75 years | 186 | 18.6 |
| History of disease | ||
| No previous disease | 83 | 8.3 |
| At least one relevant previous disease* | 915 | 91.7 |
| – Cancer as underlying disease | 412 | 41.3 |
| – Underlying cardiac disease | 392 | 39.3 |
| – Underlying pulmonary disease | 159 | 15.9 |
| – Underlying neurologic disease | 90 | 9.0 |
| Mode of life before hospital admission | ||
| Living independently at home | 933 | 93.5 |
| Cared for at home | 48 | 4.8 |
| Care home/nursing home | 12 | 1.2 |
| No data | 5 | 0.5 |
SD = standard deviation
* “At least one relevant previous disease” equates to a medical history of severe disease requiring long-term medical treatment
Of the 998 patients enrolled, 788 (79%) were admitted with a surgical main diagnosis, 211 (21.1%) were admitted with a nonsurgical diagnosis, and 5 patients (0.5%) could not be definitely assigned to either category. Admission was planned (elective) in the case of 618 patients (61.9%), while 361 patients (36.2%) were admitted as emergencies. Twenty-five patients (2.5%) could not be definitely assigned to either category.
Prevalence of powers of attorney and advance directives
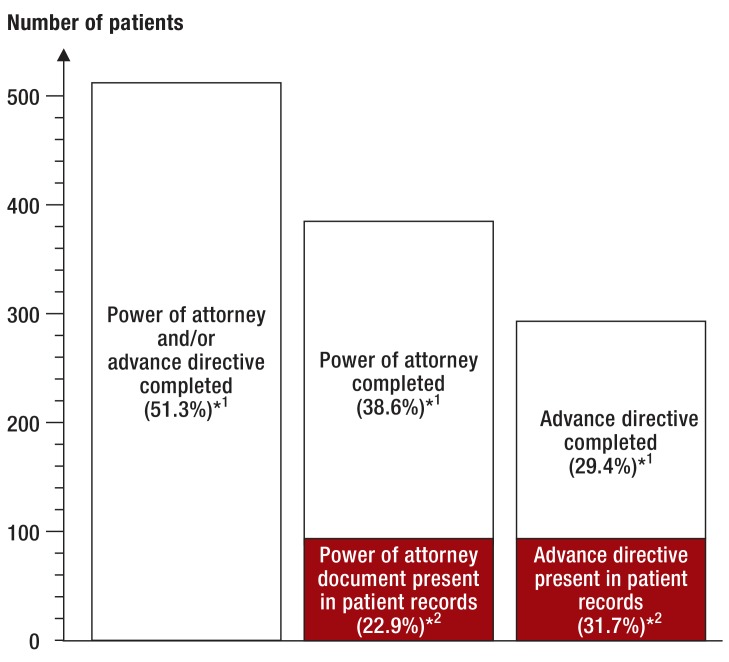
Of the 998 patients, 512 (51.3%) reported having set up either a power of attorney or an advance directive or both. A total of 385 powers of attorney (38.6% of patients) and 293 advance directives (29.4%) were reported as having been completed, while 486 patients (48.7%) had not completed either document.
Of the 512 patients who reported having completed a power of attorney or advance directive, 203 (39.6%) stated that the document had been handed over by themselves or their relatives during their hospital stay. The electronic patient data records contained documents from 118 patients (11.8% of the overall study group), made up of 88 of the 385 powers of attorney (22.9%) and 93 of the 293 advance directives (31.7%) (figure). The age distribution in relation to documents that had been completed and were actually available in the patients’ records is shown in Table 2.
Figure.
Prevalence of powers of attorney and advance directives: percentages reported as completed in the whole study group and percentages actually present in patient records
*1 Percentage relates to the numbers reported by patients
*2 Percentage relates to the total number of powers of attorney or advance directives reported as completed by patients
Table 2. Documents reported as completed in the study group and those actually available in patient records, in relation to age.
| Age (years) | Patients | Power of attorney | Advance directive | ||||||
| Completed | % *1 | Present in the records | % *2 | Completed | % *1 | Present in the records | %*2 | ||
| ≤ 65 | 506 | 155 | 30.6% | 40 | 25.8% | 120 | 23.7% | 38 | 31.7% |
| > 65 to ≤ 75 | 306 | 141 | 46.1% | 21 | 14.9% | 101 | 33.0% | 27 | 26.7% |
| >75 | 186 | 89 | 47.8% | 27 | 30.3% | 72 | 38.7% | 28 | 38.9% |
| n = | 998 | 385 | – | 88 | – | 293 | – | 93 | – |
*1 As a percentage of the number of patients in the age group
*2 As a percentage of the number of completed powers of attorney or advance directives in the age group
Completion of powers of attorney or advance directives
For 384 out of 512 patients (75%), the power of attorney and/or advance directive was completed independently of the disease that led to admission, while 50 (9.8%) completed a document at the onset of their disease, and 75 (14.6%) because of the planned hospital admission. Three patients (0.6%) gave no information on this point.
One hundred and five patients (20.5%) completed their documents without help, whereas 79 (15.4%) did so after consultation with a physician. The documents of 172 patients (33.6%) were completed with assistance from a legal professional, while 153 patients (29.9%) received help from friends or relatives.
Factors influencing completion of a power of attorney or advance directive
A variety of influential factors in the overall study group were investigated. Descriptive data of all patients—those who reported having a power of attorney or advance directive and those who reported having none—with relevant influential variables are shown in Table 3. Of all the factors investigated, univariate analysis showed “age” and “mode of admission,” and also “children,” ”marital status,” “history of disease,” and “medication consumption” to be relevant factors for reporting having completed a document (Table 3, Table 4). In the multivariate model this held only for the factors ”age” (advance directive: 1.022 [1.009; 1.036], p = 0.001; power of attorney: 1.027 [1.014; 1.040], p <0.001) and ”mode of admission” (advance directive: 1.622 [1.138; 2.311], p<0.007; power of attorney: 1.459 [1.049; 2.030], p = 0.025) (table 4). The probability that a power of attorney or advance directive had been completed was higher for patients admitted electively than for those admitted as emergencies, and rose with patient age.
Table 3. Descriptive data of all patients—those with and those without a power of attorney or advance directive—with relevant influential factors that were included in the multivariate analysis.
| Variable and category | Medical power of attorney | Advance directive | |||||||||||
| Not existing as reported by patient | Completed / existing as reported | Not existing as reported by patient | Completed / existing as reported | ||||||||||
| N | Columns % | Rows % | N | Columns % | Rows % | N | Columns % | Rows % | N | Columns % | Rows % | ||
| Age (N, mean, standard deviation) | 613 | 60.3 | 15.6 | 385 | 66.5 | 12.2 | 705 | 61.0 | 15.3 | 293 | 66.6 | 12.4 | |
| Mode of admission | Emergency | 240 | 40.1 | 66.7 | 120 | 32.1 | 33.3 | 279 | 40.7 | 77.5 | 81 | 28.1 | 22.5 |
| Elective | 359 | 59.9 | 58.6 | 254 | 67.9 | 41.4 | 406 | 59.3 | 66.2 | 207 | 71.9 | 33.8 | |
| Marital status | Married | 331 | 54.1 | 59.9 | 222 | 57.8 | 40.1 | 367 | 52.2 | 66.4 | 186 | 63.5 | 33.6 |
| Divorced | 74 | 12.1 | 63.8 | 42 | 10.9 | 36.2 | 89 | 12.7 | 76.7 | 27 | 9.2 | 23.3 | |
| Widowed | 63 | 10.3 | 48.8 | 66 | 17.2 | 51.2 | 87 | 12.4 | 67.4 | 42 | 14.3 | 32.6 | |
| Cohabiting | 21 | 3.4 | 63.6 | 12 | 3.1 | 36.4 | 24 | 3.4 | 72.7 | 9 | 3.1 | 27.3 | |
| Single | 123 | 20.1 | 74.5 | 42 | 10.9 | 25.5 | 136 | 19.3 | 82.4 | 29 | 9.9 | 17.6 | |
| Children | No | 164 | 26.8 | 66.7 | 82 | 21.4 | 33.3 | 191 | 27.2 | 77.6 | 55 | 18.8 | 22.4 |
| Yes | 448 | 73.2 | 59.8 | 301 | 78.6 | 40.2 | 512 | 72.8 | 68.4 | 237 | 81.2 | 31.6 | |
| History of disease | No | 66 | 10.8 | 79.5 | 17 | 4.4 | 20.5 | 72 | 10.2 | 86.7 | 11 | 3.8 | 13.3 |
| Yes | 547 | 89.2 | 59.8 | 368 | 95.6 | 40.2 | 633 | 89.8 | 69.2 | 282 | 96.2 | 30.8 | |
| Cardiac | No | 389 | 63.5 | 64.2 | 217 | 56.4 | 35.8 | 447 | 63.4 | 73.8 | 159 | 54.3 | 26.2 |
| Yes | 224 | 36.5 | 57.1 | 168 | 43.6 | 42.9 | 258 | 36.6 | 65.8 | 134 | 45.7 | 34.2 | |
| Pulmonary | No | 525 | 85.6 | 62.6 | 314 | 81.6 | 37.4 | 592 | 84.0 | 70.6 | 247 | 84.3 | 29.4 |
| Yes | 88 | 14.4 | 55.3 | 71 | 18.4 | 44.7 | 113 | 16.0 | 71.1 | 46 | 15.7 | 28.9 | |
| Cancer | No | 380 | 62.0 | 64.8 | 206 | 53.5 | 35.2 | 436 | 61.8 | 74.4 | 150 | 51.2 | 25.6 |
| Yes | 233 | 38.0 | 56.6 | 179 | 46.5 | 43.4 | 269 | 38.2 | 65.3 | 143 | 48.8 | 34.7 | |
| Neurologic | No | 565 | 92.2 | 62.2 | 343 | 89.1 | 37.8 | 651 | 92.3 | 71.7 | 257 | 87.7 | 28.3 |
| Yes | 48 | 7.8 | 53.3 | 42 | 10.9 | 46.7 | 54 | 7.7 | 60.0 | 36 | 12.3 | 40.0 | |
| Medication consumption | No | 140 | 22.8 | 69.7 | 61 | 15.9 | 30.3 | 155 | 22.0 | 77.1 | 46 | 15.8 | 22.9 |
| Yes | 473 | 77.2 | 59.4 | 323 | 84.1 | 40.6 | 550 | 78.0 | 69.1 | 246 | 84.2 | 30.9 | |
Table 4. Factors potentially influencing completion of medical powers of attorney and patient advance directives.
| Variable and/or category | Medical power of attorney | Advance directive | ||||||||||
| Univariate | Multivariate | Univariate | Multivariate | |||||||||
| OR | [95% CI] | p | OR | [95% CI] | p | OR | [95% CI] | p | OR | [95% CI] | p | |
| Admitting department: surgical *1 | 1.11 | [0.81; 1.52] | 0.51 | 0.95 | [0.65; 1.40] | 0.80 | 1.40 | [0.99; 1.98] | 0.06 | 1.05 | 0.69; 1.59 | 0.83 |
| Mode of admission: elective | 1.42 | [1.08; 1.86] | 0.01 | 1.46 | [1.05; 2.03] | 0.02 | 1.76 | [1.30; 2.37] | <0.01 | 1.62 | [1.14; 2.31] | <0.01 |
| Sex: male | 1.01 | [0.78; 1.30] | 0.95 | 0.98 | [0.74; 1.30] | 0.89 | 1.08 | [0.82; 1.42] | 0.58 | 0.94 | [0.69; 1.28] | 0.70 |
| Age | 1.03 | [1.02; 1.04] | <0.01 | 1.03 | [1.01; 1.04] | <0.01 | 1.03 | [1.02; 1.04] | <0.01 | 1.02 | [1.01; 1.04] | <0.01 |
| Marital status*2 | <0.01 | 0.48 | <0.01 | 0.46 | ||||||||
| – Divorced | 0.85 | [0.56; 1.28] | 0.43 | 0.96 | [0.62; 1.51] | 0.87 | 0.60 | [0.38; 0.95] | 0.03 | 0.72 | [0.44; 1.18] | 0.19 |
| – Widowed | 1.56 | [1.06; 2.30] | 0.02 | 1.40 | [0.91; 2.15] | 0.12 | 0.95 | [0.63; 1.43] | 0.82 | 0.86 | [0.55; 1.36] | 0.53 |
| – Cohabiting | 0.85 | [0.41; 1.77] | 0.67 | 1.14 | [0.51; 2.55] | 0.76 | 0.74 | [0.34; 1.62] | 0.45 | 1.30 | [0.55; 3.03] | 0.55 |
| – Single | 0.51 | [0.34; 0.75] | <0.01 | 0.85 | [0.53; 1.36] | 0.49 | 0.42 | [0.27; 0.65] | <0.01 | 0.73 | [0.43; 1.24] | 0.25 |
| Children: yes | 1.34 | [0.99; 1.82] | 0.06 | 0.94 | [0.65; 1.36] | 0.75 | 1.61 | [1.15; 2.25] | <0.01 | 1.15 | [0.77; 1.73] | 0.48 |
| Previous disease: yes | 2.61 | [1.51; 4.52] | <0.01 | 1.31 | [0.69; 2.50] | 0.41 | 2.92 | [1.52; 5.58] | <0.01 | 1.38 | [0.66; 2.86] | 0.39 |
| Cardiac: yes | 1.34 | [1.04; 1.74] | 0.03 | 0.95 | [0.69; 1.30] | 0.74 | 1.46 | [1.11; 1.92] | <0.01 | 1.18 | [0.84; 1.65] | 0.34 |
| Pulmonary: yes | 1.35 | [0.96; 1.90] | 0.09 | 1.39 | [0.95; 2.03] | 0.09 | 0.98 | [0.67; 1.42] | 0.90 | 0.98 | [0.65; 1.47] | 0.91 |
| Cancer: yes | 1.42 | [1.09; 1.83] | <0.01 | 1.27 | [0.95; 1.72] | 0.11 | 1.55 | [1.17; 2.03] | <0.01 | 1.28 | [0.93; 1.75] | 0.13 |
| Neurologic: yes | 1.44 | [0.93; 2.23] | 0.10 | 1.39 | [0.87; 2.24] | 0.17 | 1.69 | [1.08; 2.64] | 0.02 | 1.55 | [0.96; 2.52] | 0.07 |
| Medication consumption: yes | 1.57 | [1.12; 2.19] | <0.01 | 1.12 | [0.76; 1.65] | 0.57 | 1.51 | [1.05; 2.16] | 0.03 | 1.06 | [0.70; 1.60] | 0.79 |
| Mode of life*2 | 0.84 | 0.16 | 0.95 | 0.69 | ||||||||
| Mode of life: at home with help | 0.86 | [0.47; 1.59] | 0.64 | 0.60 | [0.31; 1.16] | 0.13 | 0.99 | [0.52; 1.87] | 0.98 | 0.78 | [0.39; 1.56] | 0.49 |
| Mode of life: care/nursing home | 0.79 | [0.24; 2.64] | 0.70 | 0.44 | [0.13; 1.56] | 0.20 | 0.80 | [0.22; 2.98] | 0.74 | 0.69 | [0.18; 2.69] | 0.59 |
*1 Reference categories: Admitting department: internal medicine; Mode of admission: emergency; Sex: female; Marital status: married; Children: no; History of disease: none; Cardiac: no; Pulmonary: no; Cancer: no; Neurologic: no; Medication consumption: no; Mode of life: independent
*2 “Global” Wald test
Rows in bold type indicate influential factors shown to be statistically significant in both univariate and multivariate analysis.
OR, odds ratio; 95% CI, 95% confidence interval
Reasons for completing a power of attorney or advance directive
Regarding the reasons for having completed one of these documents, evaluable data were available for 508 patients. Of these, 244 (48%) said the reason was fear of being at the mercy of others, of the lack of self-determination, or of overtreatment. One hundred thirty-four patients (26.4%) had been encouraged by the advice of relatives or their primary care physician. Seventy-eight patients (15.4%) had been prompted by the media or by information leaflets, etc. Fifty-two (10.2%) stated that they had been influenced by past experience, while 9 (1.8%) gave no information.
Reasons for not completing a power of attorney or advance directive
The 486 patients who had completed neither document were also asked about their reasons. Of these, 245 (50.4%) had previously thought about completing one, but had not done so at the time of the survey; 191 (39.3%) had never thought about it; 40 (8.2%) refused on principle to think about it; and 10 patients (2.1%) reported a fear of undertreatment. Thus, 50 (5%) of the overall study group actively refused to complete one of these documents. Seven patients (1.4%) gave no information.
Analysis of powers of attorney and advance directives
The electronic patient records contained documents from 118 patients who had completed 88 powers of attorney and 93 advance directives. A completely prewritten document had been used for 32 powers of attorney (36.4%) and 15 advance directives (16.1%). A similarly prewritten form containing additional alternative options regarding conditions of validity or treatment measures had been used for 16 powers of attorney (18.2%) and 24 advance directives (25.8%). Documents of this nature had also been used for a further 35 powers of attorney (39.8%) and 41 advance directives (44.1%), but the alternative options had not been filled in, or not in a way that could be interpreted. Five powers of attorney (5.7%) and 13 advance directives (14%) had been written entirely by the individuals concerned.
For 52 of the 118 patients (44.1%), the answer to the question about whether their power of attorney or advance directive contained a statement about organ donation contradicted what was later found when the document concerned was analyzed. Of 14 patients (11.9%) who said their document made no statement about this matter, 10 had refused organ donation and 4 had expressly agreed to it.
Discussion
In this cross-sectional study, a large group of intensive care patients were asked about their possession or otherwise of a power of attorney or advance directive. The prevalence of these documents as reported by the patients is higher than some figures published elsewhere in the literature, but the number of documents actually available for inspection—powers of attorney for 8.8% and advance directives for 9.3% of the whole group—is rather lower. For example, a study carried out in the USA, in which 112 cardiac intensive care patients were interviewed, found a prevalence of advance directives of 26% (7). While a German retrospective study of patient records showed that, out of 658 intensive care patients who died, 12% had an advance directive (6), a US retrospective data analysis from 2010 showed as many as 19% powers of attorney and 22% advance directives in a group of 512 cardiac intensive care patients (8).
Up to 2009, the year in which the German Advance Directives Act was passed, the prevalence of the documents of interest in various patient groups, both in surveys and in data analyses, was lower than it has become since that date (9). A data analysis carried out in 2007 in 11 German nursing homes showed only 11% of residents to have an advance directive (10), whereas a similar data analysis of 181 geriatric traumatology patients performed by a German university hospital in 2013–2014 showed that 33% had completed a power of attorney and 27% an advance directive (11). In a questionnaire survey carried out in the hematology-oncology outpatient department of a German university hospital in 2011–2012, as many as 31% of the 503 patients said they had completed an advance directive; 54% of them had done so since 2009 (12).
In the present study, “more advanced age” was independently associated with the existence of one of the documents under study. This has already been confirmed in a variety of studies (13, 14). In old age the need is greater for patients to be involved in decisions about the nature and extent of medical interventions (15, 16). However, it is not possible to infer wishes about life-sustaining interventions on the basis of age alone—doctors frequently draw false conclusions in this regard (15– 19).
Of those patients who reported having a power of attorney and/or advance directive, 39.6% reported having also handed them over to the hospital. However, the documents were actually available in the patient records for only 23% of this patient group.
This discrepancy cannot be explained with absolute certainty. Misfiling of documents on such a scale is not likely. A more probable explanation is that not all patients knew exactly what had happened to their documents; it may be that more of the documents should have been presented by relatives. Other studies have also found a relatively low rate of powers of attorney or advance directives either deposited with the hospital or brought into it by the patient or a relative (11, 14, 20).
Irrespective of the availability of powers of attorney or advance directives, a judgment needs to be made about how helpful these documents are for decision making in intensive care. In a questionnaire survey of physicians and relatives, Leder et al. found that agreement about the practical meaning of advance directives containing widely used, prewritten wording was assessed as low, and that this form of advance directive therefore appeared unsuited to the intensive care setting (21). Similar findings have been reported by other groups (22, 23). A retrospective cohort study of 477 patients who had died in intensive care showed that resuscitation was carried out less often in patients who had an advance directive (24). In regard to other life-sustaining measures and the duration of stay in the intensive care unit or hospital, no significant difference was found.
An Anglo-American retrospective data analysis of 1121 intensive care patients found that the availability of a medical power of attorney (“health care proxy”) or advance directive (“living will”) did not influence treatment, treatment decisions, or patient outcome (25).
Recently, the German Federal Supreme Court decided that phrases such as “I decline life sustaining treatment” are not specific enough for the individual case, and that a written patient advance directive under Section 1901a, Paragraph 1 of the German Civil Code (Bürgerliches Gesetzbuch, BGB) is binding only when it contains specific decisions about patient consent or withholding of consent for particular medical interventions that are not immediately imminent (26). For a non-medically trained person, creating a patient advance directive alone and without medical advice is difficult because of the unpredictable and medically complex developments that can occur in intensive care. A structured consultation is helpful for patients writing an advance directive, and is welcomed by patients (27, 28).
Few patient advance directives accurately reflect the complex situations that arise in an intensive care unit. However, if patients and/or relatives have already gone through the process involved in writing an advance directive, this makes it easier to approach the subject in physician-patient conversations.
Limitations
The patient selection could be regarded as a limitation of this study. Our sample consisted of 16.7% of the patients treated in intensive care during the study period. Since we surveyed only patients who were transferred to ordinary wards after a stay in intensive care, we have no data from patients who
were unable to take part, or consent to taking part, in the survey at the time of transfer, e.g., because of persistent delirium or dementia
were being ventilated on transfer to a rehabilitation or weaning unit
died as a result of their disease.
However, the questionnaire was administered on 11 different intensive care units, to patients in all age groups, irrespective of their admission diagnosis or whether they had been admitted as an emergency or electively, and for this reason we believe the results of the study may be taken as valid. Furthermore, this study did not analyze the disease leading to admission in any detail, distinguishing only between surgical and nonsurgical patients. In the course of the document analysis, discrepancies became apparent between the survey results and those of the analysis. Whether these discrepancies arose because, when documents were created a long time ago, some of the details may be remembered incorrectly, or because patients felt uncomfortable about some answers—e.g., about stating their attitude to organ donation—cannot be determined.
In conclusion, we found that older, electively admitted patients more often report having a power of attorney and/or advance directive in place. However, the documents often fail to be handed over to the hospital. Also, although they have often been created due to a fear of being at the mercy of others or of overtreatment, and are intended to be used as a basis for significant medical decisions, few patients ask for a physician’s help in writing them.
Documents regarding a patient’s wishes are too often unavailable on the intensive care unit, or cannot be applied because they are inappropriately worded. With all its limitations, the face-to-face interview between the physician and the patient or relative continues to be the most frequent route to assessing the patient’s wishes.
Key Messages.
Half of all patients in intensive care reported having prepared documents (medical powers of attorney or advance directives) indicating their wishes in advance.
More patients who are older and have been admitted electively have prepared such documents.
In many cases, some specific contents of the documents, e.g., those relating to a patient’s willingness to donate organs, may not be reliably reported.
Few patients receive/seek medical support when preparing powers of attorney or advance directives, although the present results suggest that this would be desirable.
Acknowledgments
Translated from the original German by Kersti Wagstaff, MA.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.May AT, Brokmann JC. Medizinische und medizinethische Grundlagen der Vorsorgemöglichkeiten. Anaesthesist. 2010;59:118–125. doi: 10.1007/s00101-010-1687-9. [DOI] [PubMed] [Google Scholar]
- 2.Janssens U, Burchardi H, Duttge G, et al. Therapiezieländerung und Therapiebegrenzung in der Intensivmedizin. Med Klin Intensivmed Notfmed. 2013;108:47–52. doi: 10.1007/s00063-012-0190-2. [DOI] [PubMed] [Google Scholar]
- 3.Ulsenheimer K. Neue Regelung der Patientenverfügung. Welche Konsequenzen ergeben sich für die Praxis? Anaesthesist. 2010;59:111–117. doi: 10.1007/s00101-010-1682-1. [DOI] [PubMed] [Google Scholar]
- 4.Booth MG, Doherty P, Fairgrieve R, Kinsella J. Relatives’ knowledge of decision making in intensive care. J Med Ethics. 2004;30:459–461. doi: 10.1136/jme.2002.000802. discussion 61-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Allensbach IfD. Deutlicher Anstieg bei Patientenverfügungen Allensbach Kurzbericht. www.ifd-allensbach.de/studien-und-bericht (last accessed on 24 April 2017) [Google Scholar]
- 6.Riessen R, Bantlin C, Wiesing U, Haap M. Therapiezieländerungen auf einer internistischen Intensivstation. Med Klin Intensivmed Notfmed. 2013;108:412–418. doi: 10.1007/s00063-013-0233-3. [DOI] [PubMed] [Google Scholar]
- 7.Kirkpatrick JN, Guger CJ, Arnsdorf MF, Fedson SE. Advance directives in the cardiac care unit. Am Heart J. 2007;154:477–481. doi: 10.1016/j.ahj.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 8.Kumar A, Aronow WS, Alexa M, et al. Prevalence of use of advance directives, health care proxy, legal guardian, and living will in 512 patients hospitalized in a cardiac care unit/intensive care unit in 2 community hospitals. Arch Med Sci. 2010;6:188–191. doi: 10.5114/aoms.2010.13892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Justinger C, Richter S, Moussavian MR, Serrano Contreras T, Schilling MK. Patientenverfügung aus der Sicht des chirurgischen Patienten. Chirurg. 2009;80:455–456. doi: 10.1007/s00104-008-1662-z. 8-61. [DOI] [PubMed] [Google Scholar]
- 10.Sommer S, Marckmann G, Pentzek M, Wegscheider K, Abholz HH, Schmitten J. Advance directives in nursing homes: prevalence, validity, significance, and nursing staff adherence. Dtsch Arztebl Int. 2012;109:577–583. doi: 10.3238/arztebl.2012.0577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hack J, Buecking B, Lopez CL, Ruchholtz S, Kuhne CA. Patientenverfügung, Vorsorgevollmacht und gesetzliche Betreuung im unfallchirurgischen Alltag: Zahlen aus einem alterstraumatologischen Zentrum. Z Gerontol Geriatr. 2016;49:721–726. doi: 10.1007/s00391-015-0981-1. [DOI] [PubMed] [Google Scholar]
- 12.Hubert E, Schulte N, Belle S, et al. Cancer patients and advance directives: a survey of patients in a hematology and oncology outpatient clinic. Onkologie. 2013;36:398–402. doi: 10.1159/000353604. [DOI] [PubMed] [Google Scholar]
- 13.Lang FR, Wagner GG. Patientenverfügungen in Deutschland: Bedingungen für ihre Verbreitung und Gründe der Ablehnung. Dtsch Med Wochenschr. 2007;132:2558–2562. doi: 10.1055/s-2007-993097. [DOI] [PubMed] [Google Scholar]
- 14.Driehorst F, Keller F. Patientenverfügung bei Patienten mit Nierenerkrankungen im Vergleich zu allgemein-internistischen Patienten. Dtsch Med Wochenschr. 2014;139:633–637. doi: 10.1055/s-0034-1369881. [DOI] [PubMed] [Google Scholar]
- 15.Hamel MB, Teno JM, Goldman L, et al. Patient age and decisions to withhold life-sustaining treatments from seriously ill, hospitalized adults SUPPORT Investigators. Ann Intern Med. 1999;130:116–125. doi: 10.7326/0003-4819-130-2-199901190-00005. [DOI] [PubMed] [Google Scholar]
- 16.Messer M, Huber W, Allmann J, et al. Treatment preferences of hospitalized medical patients for life-sustaining interventions and intensive care unit admission. Br J Anaesth. 2015;115:317–318. doi: 10.1093/bja/aev237. [DOI] [PubMed] [Google Scholar]
- 17.Jecker NS, Pearlman RA. Ethical constraints on rationing medical care by age. J Am Geriatr Soc. 1989;37:1067–1075. doi: 10.1111/j.1532-5415.1989.tb06923.x. [DOI] [PubMed] [Google Scholar]
- 18.Avorn J. Benefit and cost analysis in geriatric care Turning age discrimination into health policy. N Engl J Med. 1984;310:1294–1301. doi: 10.1056/NEJM198405173102005. [DOI] [PubMed] [Google Scholar]
- 19.Uhlmann RF, Pearlman RA. Perceived quality of life and preferences for life-sustaining treatment in older adults. Arch Intern Med. 1991;151:495–497. [PubMed] [Google Scholar]
- 20.Christ M, Liebeton J, Breker IM, Grett M, von Auenmuller KI, Trappe HJ. Verfügbarkeit von Patientenverfügungen in einer interdisziplinären Notaufnahme. Dtsch Med Wochenschr. 2015;140:e231–e236. doi: 10.1055/s-0041-106869. [DOI] [PubMed] [Google Scholar]
- 21.Leder N, Schwarzkopf D, Reinhart K, Witte OW, Pfeifer R, Hartog CS. The validity of advance directives in acute situations—a survey of doctors’ and relatives’ perceptions from an intensive care unit. Dtsch Arztebl Int. 2015;112:723–729. doi: 10.3238/arztebl.2015.0723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Langer S, Stengel I, Fleischer S, Stuttmann R, Berg A. Umgang mit Patientenverfügungen in Deutschland. Dtsch Med Wochenschr. 2016;141:e73–e79. doi: 10.1055/s-0042-104038. [DOI] [PubMed] [Google Scholar]
- 23.Peters M, Kern BR, Buschmann C. Medizinrechtliche Aspekte bei der notärztlichen Versorgung. Med Klin Intensivmed Notfmed. 2015;112:136–144. doi: 10.1007/s00063-015-0120-1. [DOI] [PubMed] [Google Scholar]
- 24.Hartog CS, Peschel I, Schwarzkopf D, et al. Are written advance directives helpful to guide end-of-life therapy in the intensive care unit? A retrospective matched-cohort study. J Crit Care. 2014;29:128–133. doi: 10.1016/j.jcrc.2013.08.024. [DOI] [PubMed] [Google Scholar]
- 25.Halpern NA, Pastores SM, Chou JF, Chawla S, Thaler HT. Advance directives in an oncologic intensive care unit: a contemporary analysis of their frequency, type, and impact. J Palliat Med. 2011;14:483–489. doi: 10.1089/jpm.2010.0397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bundesgerichtshof. Anforderungen an Vorsorgevollmacht und Patientenverfügung im Zusammenhang mit dem Abbruch lebenserhaltender Maßnahmen XII ZB 61/16. Pressestelle des Bundesgerichtshofes 2016. http://juris.bundesgerichtshof.de/cgi-bin/rechtsprechung/document.py?Gericht=bgh&Art=pm&Datum=2016&Sort=3&nr=75566&pos=0&anz=136 (last accessed on 1st July 2016) [Google Scholar]
- 27.Schoffner M, Schmidt KW, Benzenhofer U, Sahm S. Patientenverfügung auf dem Prüfstand: Ärztliche Beratung ist unerlässlich. Dtsch Med Wochenschr. 2012;137:487–490. doi: 10.1055/s-0031-1298998. [DOI] [PubMed] [Google Scholar]
- 28.Pfirstinger J, Kattner D, Edinger M, Andreesen R, Vogelhuber M. The impact of a tumor diagnosis on patients’ attitudes toward advance directives. Oncology. 2014;87:246–256. doi: 10.1159/000363508. [DOI] [PubMed] [Google Scholar]