Summary
Objectives
Physical activity is important for weight management. However, it remains unclear what type of physical activity prescription/programme is optimal for increasing physical activity during a standard behavioural weight loss intervention. This study examined changes in physical activity after a 12‐week supervised programme prescribed in minutes per week (SUP‐PA), an unsupervised programme prescribed in minutes per week (UNSUP‐PA) and an unsupervised programme prescribed in steps per day (STEP).
Methods
Fifty‐two adults who were overweight or obese (age: 43.5 ± 10.1 years, BMI: 31.5 ± 3.5 kg·m−2) were randomized to STEP (n = 18), UNSUP‐PA (n = 17) and SUP‐PA (n = 17). Subjects attended weekly in‐person group intervention sessions and were prescribed a calorie‐restricted diet (1,200–1,800 kcals·day−1) combined with increased physical activity (150 min·week−1 or 10,000 steps·day−1 with 2,500 brisk steps·day−1).
Results
All three groups significantly increased moderate‐to‐vigorous physical activity (STEP: 80.6 ± 218.5 min·week−1, UNSUP‐PA: 112.9 ± 180.4 min·week−1 and SUP‐PA: 151.1 ± 174.0 min·week−1, p < 0.001) with no differences between groups (p = 0.94) or group by time interaction (p = 0.81). In addition, there were no significant differences in weight loss between the groups (p = 0.81).
Conclusions
In this short‐term study, all three physical activity programmes increased physical activity and elicited modest weight loss when combined with a standard behavioural weight loss intervention.
Keywords: Exercise, intervention, obesity
Introduction
Standard behavioural weight loss interventions typically recommend increasing physical activity and decreasing energy intake to promote weight loss 1, 2. Previous weight loss interventions have prescribed physical activity to be performed in either supervised or unsupervised conditions 3, 4, 5, 6. Supervised physical activity is typically completed in a health‐fitness facility under the direct supervision of trained staff, such that adherence to the prescription (e.g. duration, frequency, intensity and type) can be monitored. However, generalizing the results of supervised trials may not reflect physical activity participation that would be observed in non‐research settings where the majority of physical activity is unsupervised. In contrast, unsupervised research interventions may generalize and translate to non‐research settings. In addition, unsupervised interventions may be more convenient for participants, require less staff and be less expensive compared to supervised interventions 7, 8.
Previous comparisons of supervised vs. unsupervised physical activity programmes in adults who are overweight or obese have produced inconsistent findings for changes in physical activity, cardiorespiratory fitness and weight 9, 10, 11, 12. One limitation of these previous studies is that the unsupervised conditions relied on self‐report measures to confirm adherence to the prescribed dose of physical activity 9, 10, 11, 12. However, the availability of wearable technology facilitates objective measurement of prescribed aerobic moderate‐to‐vigorous physical activity (MVPA) regardless of whether the activity is supervised or unsupervised. This wearable technology may not accurately assess activities such as resistance training 13; however, ambulatory free‐living activities are detected by these monitors 14. Thus, it is possible to directly compare levels of aerobic physical activity participation in response to an unsupervised physical activity programme vs. a supervised programme (i.e. gold standard for research) using wearable technology. If both programmes invoke comparable results, this could have substantial impact on future physical activity interventions.
The primary aim of this study was to compare changes in objectively measured MVPA in adults who were overweight or obese and enrolled in a standard behavioural weight loss intervention with physical activity prescribed in either a supervised or unsupervised manner. Physical activity was prescribed as supervised with a targeted minute goal (SUP‐PA), unsupervised with a targeted minute goal (UNSUP‐PA) or unsupervised with a targeted step goal (STEP). Secondary outcomes included changes in weight, body composition, energy intake, cardiorespiratory fitness and other components of physical activity (e.g. sedentary behaviour [SED], light intensity physical activity [LPA] and steps).
Methods
Volunteers were recruited via mailings, research registries and through an email messaging system. Inclusion criteria were 18–55 years of age and BMI 25.0 to >40.0 kg·m−2. Exclusion criteria were (i) engaging in >60 min·week−1 (accumulated in bouts of ≥10 min) of MVPA over the past month via self‐report; (ii) previous participation in a weight management research project within the past 6 months; (iii) currently being treated for an eating disorder; (iv) currently pregnant or a pregnancy during the previous 6 months; (v) currently being treated for depression or anxiety; (vi) planned travel for ≥1 week during the intervention; (vii) currently using a physical activity device to monitor activity; (viii) history of metabolic, cardiac or pulmonary disease; (ix) weight loss ≥5% of current body weight or 15 pounds total in the previous 6 months; (x) previous bariatric surgery; or (xi) taking medications that affect heart rate, blood pressure, body weight or metabolism. Eligible participants provided written informed consent and physician's clearance prior to the baseline assessment. Procedures were approved by the University of Pittsburgh Institutional Review Board prior to the study beginning.
Intervention procedures
Eligible participants were randomized by computer software (IBM‐SPSS) after completion of baseline assessments. Participants were enrolled in a 12‐week standard behavioural weight loss intervention and randomized to either SUP‐PA, UNSUP‐PA or STEP. Participants attended weekly group intervention sessions for each of the 12 weeks of the study. The three groups had separate group meetings to avoid contamination. Group meetings lasted 30–45 min, were led by trained behavioural interventionists and focused on strategies to promote weight management including increasing physical activity and reducing caloric intake. These intervention sessions were modelled after prior standard behavioural weight loss interventions conducted in our research centre 3, 6.
Dietary component
SUP‐PA, UNSUP‐PA and STEP were provided the same dietary recommendations which included a reduced fat, calorie‐restricted diet (1,200–1,800 kcals·day−1). These dietary recommendations were similar to previous literature 3, 6, 9. To promote adoption and adherence, participants were provided meal plans and sample recipes. Participants were provided paper diaries to self‐monitor their eating behaviours; however, participants were allowed to self‐monitor using other methods (e.g. online dietary tracking tools) if preferred.
Physical activity component
- SUP‐PA:
Participants reported to the research centre's fitness facility to engage in supervised physical activity sessions. The use of the fitness facility was free for participants, included free parking and exercise equipment included built‐in entertainment (e.g. televisions and music) in an attempt to decrease the burden of this condition. Endurance aerobic training was performed using treadmills, elliptical trainers, adaptive motion trainers and stationary cycles. Participants chose their preferred mode of exercise and could vary this from session to session. MVPA was prescribed at 100 min week−1 for weeks 1–2, 125 min·week−1 for weeks 3–4 and 150 min·week−1 for weeks 5–12. Physical activity was to be spread across three to five supervised sessions per week, with each session being 10–60 min. Physical activity was completed at 60–75% of age‐predicted maximal heart rate, which was quantified using a heart rate monitor. An exercise physiologist recorded attendance, duration and monitored heart rate. SUP‐PA was not given any advice on modifying physical activity behaviour outside of these supervised sessions.
- UNSUP‐PA:
Participants were recommended to engage in MVPA in bouts of ≥10 min at an intensity of 12–14 using the Borg 15‐category rating of perceived exertion (RPE) scale 15. This intensity recommendation closely aligns with the physical activity intensity recommended for SUP‐PA. UNSUP‐PA had a brief physical activity education session during week 1. At this first session, an interventionist led a 10‐min exercise walk so participants were anchored to the proper intensity of physical activity. After the completion of this session, physical activity was to be completed at a time and place that was convenient for the individual (i.e. not at the research centre). Similar to SUP‐PA, MVPA was prescribed at 100 min·week−1 for weeks 1–2, 125 min·week−1 for weeks 3–4 and 150 min·week−1 for weeks 5–12, and activity was to be spread across ≥3 days week−1.
- STEP:
Participants were prescribed a step goal that progressed from 6,000 steps·day−1 for weeks 1–2, to 8,000 steps·day−1 for weeks 3–4, to 10,000 steps·day−1 for weeks 5–12. A digital hip‐worn pedometer was provided to each participant in this intervention condition to facilitate the monitoring of steps. Participants were instructed that 25% of these daily steps should be completed at a perceived ‘brisk’ pace, which was anchored using the Borg 15‐category RPE scale similar to UNSUP‐PA. Each participant was instructed to engage in 1,500 brisk steps·day−1 during weeks 1–2, 2,000 brisk steps·day−1 during weeks 3–4 and 2,500 brisk steps·day−1 during weeks 5–12.
Assessment procedures
Assessments conducted at baseline (week 0) and post‐intervention (week 12) included measurements of height, weight, BMI, body composition, cardiorespiratory fitness and dietary intake. Participants were asked to complete the physical assessment after fasting for >4 h and refraining from exercise for 24 h prior. Objectively measured physical activity was assessed at weeks 0, 4, 8 and 12. All assessments were completed by trained staff.
- Height, weight, body composition:
Height was measured in duplicate to the nearest 0.1 cm using a wall‐mounted stadiometer. Body weight was measured in duplicate using a calibrated digital scale to the nearest 0.1 kg. Participants were weighed while wearing a lightweight hospital gown. Body composition was assessed via dual‐energy x‐ray absorptiometry (DXA) using a total body scan (GE Lunar iDXA; Madison, WI). Dual‐energy x‐ray absorptiometry provided data for fat mass, fat‐free mass and percent body fat. Waist and hip circumferences were assessed in duplicate using a Gulick tape measure to the nearest 0.1 cm.
- Cardiorespiratory fitness:
Cardiorespiratory fitness was measured using a submaximal graded exercise with the speed held constant at 80.4 m·s−1 and grade starting at 0% and increasing 1.0% each minute until the participant reached 85% of their age‐predicted maximal heart rate. Fitness was defined as the oxygen consumption, measured via indirect calorimetry at the point of test termination.
- Dietary intake:
Energy intake (kilocalories per day; kcal day−1) and macronutrient composition were measured using the Block Food Frequency Questionnaire (FFQ) (Dietary Data Systems; Berkeley, CA) 16.
- Physical activity:
Physical activity was assessed using the SenseWear device (BodyMedia Inc.; Pittsburgh, PA). SenseWear is a multi‐sensor monitor that collects minute‐by‐minute physical activity data and has been previously validated 17. Participants were instructed to wear the device during all waking hours for seven consecutive days for each assessment. Physical activity data were considered valid if the device was worn ≥4 days and ≥10 h·day−1 18. Analyses were also conducted using all participants with ≥1 day and ≥10 h·day−1. Mean measures of physical activity were similar, and, therefore, the data for ≥ 1 day and ≥10 h·day−1 are presented. Data were used to identify changes in steps, SED (<1.5 metabolic equivalents; METs), LPA (1.5 to >3.0 METs) and MVPA (≥3.0 METs). Total SED, LPA and MVPA were computed as the sum of all 1‐min epocs that met the specific MET criteria. Moderate‐to‐vigorous physical activity was also computed as the sum of periods that met the ≥3.0 MET criteria performed for >10 continuous minutes.
Statistical analyses
Statistical analyses were performed using SPSS software (IBM‐SPSS, version 24). Statistical significance was set at p ≤ 0.05. Analyses were performed to examine if data were normally distributed. Normally distributed data are presented as mean ± standard deviation (SD). When data were not normally distributed, non‐parametric tests were performed or data were transformed. Descriptive statistics summarized the study sample at baseline, and primary outcomes were analysed using repeated measures ANOVA. Significance for the effects of treatment group, time and group by time interaction were examined. Differences between SUP‐PA, UNSUP‐PA and STEP were examined over time with the p‐value adjusted for multiple comparisons using the Bonferroni procedure. Difference in the number of study participants achieving >5% weight loss between the intervention groups was determined using a chi‐square test.
An a priori power analysis was conducted to determine the sample size estimate for this study. This was based on the primary outcome of MVPA differences between the groups, with 80% statistical power and a type one error rate of 0.05, which was adjusted for two comparisons (SUP‐PA vs. UNSUP‐PA and SUP‐PA vs. STEP) using the Bonferroni procedure. From a previous study comparing a supervised and unsupervised physical activity programme, we assumed the standard deviation for MVPA to be 26 min·week−1 10. Based on this assumption and to be able to detect a 20 min·week−1 difference in MVPA between the planned comparisons, we required a sample size of 17 participants per group.
Results
Fifty‐two adults between the ages of 18 and 55 years with a BMI of 25.0 to <40.0 kg·m−2 were randomized. Mean age was 43.5 ± 10.1 years, and mean BMI was 31.5 ± 3.5 kg·m−2, with 26.9% males and 32.7% non‐white participants. Baseline characteristics are shown in Table 1. Figure 1 illustrates recruitment, randomization and retention. Fifty‐two individuals completed the baseline assessment and were randomized to STEP, SUP‐PA or UNSUP‐PA. Forty‐nine participants (94.2%) completed the baseline and 12‐week physical assessment. Data reported are based on those with complete data only. This was a pragmatic trial aimed at evaluating the effectiveness of supervised physical activity programmes vs. unsupervised programmes; thus, participants were not excluded from analyses based on non‐compliance to the programme. Previous, supervised exercise trials have excluded participants who did not comply to exercise recommendations (~40% of participants enrolled); 19 however, this approach limits generalizability.
Table 1.
Baseline characteristics
| Characteristics |
TOTAL n = 52 Mean ± SD |
STEP n = 18 Mean ± SD |
UNSUP‐PA n = 17 Mean ± SD |
SUP‐PA n = 17 Mean ± SD |
|---|---|---|---|---|
| Age (years) | 43.5 ± 10.1 | 39.3 ± 10.7 | 46.2 ± 10.1 | 45.2 ± 8.5 |
| Height (cm) | 165.5 ± 9.0 | 168.2 ± 8.9 | 165.9 ± 6.8 | 162.3 ± 10.4 |
| Weight (kg) | 86.4 ± 13.5 | 88.2 ± 14.5 | 86.5 ± 12.8 | 84.5 ± 13.6 |
| BMI (kg·m−2) | 31.5 ± 3.5 | 31.1 ± 3.8 | 31.3 ± 3.3 | 32.0 ± 3.5 |
| Sex | ||||
| Male n,% | 14, 26.9% | 5, 27.8% | 5, 29.4% | 4, 23.5% |
| Female n,% | 38, 73.1% | 13, 72.2% | 12, 70.6% | 13, 76.5% |
| Race | ||||
| White n, % | 35, 67.3% | 12, 66.7% | 11, 64.7% | 12, 70.6% |
| Non‐white n,% | 17, 32.7% | 6, 33.3% | 6, 35.3% | 5, 29.4% |
| Black or African American n, % | 12, 23.1% | 3, 16.7% | 5, 29.4% | 4, 23.5% |
| Asian n, % | 5, 9.6% | 3, 16.7% | 1, 5.9% | 1, 5.9% |
Figure 1.
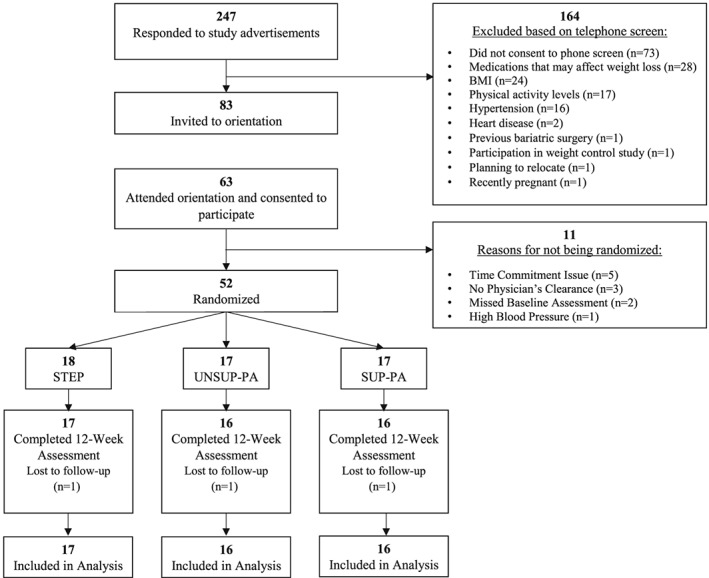
Consort diagram.
Change in physical activity
At baseline, there were no significant differences between groups for any measures of physical activity. Treatment groups reported similar amounts of activity monitor wear time (days/week and h/day) across the 12‐week intervention. All three groups significantly increased MVPA (≥3.0 METs in bouts of ≥10 min) over the 12‐week intervention (p < 0.001), with no differences between groups (p = 0.94) or group by time interaction (p = 0.81) (Table 2, Figure 2). Similar results were observed if all MVPA bouts >1 min were included. All groups increased total steps/day (p < 0.001) and MVPA steps/day completed in bouts ≥10 min (p < 0.001), with no significant group or group by time effects.
Table 2.
Change in objectively measured physical activity
| Outcome | Groups | Assessment periods | P‐values | |||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 4 weeks | 8 weeks | 12 weeks | Group | Time | Group × time | ||
| Total steps (steps·day−1) | STEP (n = 17) | 7,728 ± 1,456 | 9,883 ± 2,142 | 10,267 ± 2,251 | 10,323 ± 2,538 | 0.40 | <0.001 | 0.79 |
| UNSUP‐PA (n = 16) | 6,975 ± 2,716 | 8,931 ± 4,063 | 8,701 ± 3,622 | 9,108 ± 3,589 | ||||
| SUP‐PA (n = 16) | 7,265 ± 1,875 | 9,458 ± 2,388 | 9,980 ± 3,114 | 9,229 ± 2,187 | ||||
| SED (min·day−1) | STEP (n = 17) | 585.6 ± 113.6 | 579.2 ± 105.4 | 521.8 ± 126.3 | 524.7 ± 110.0 | 0.20 | <0.001 | 0.99 |
| UNSUP‐PA (n = 16) | 638.3 ± 106.4 | 621.3 ± 88.2 | 586.5 ± 103.0 | 582.1 ± 112.7 | ||||
| SUP‐PA (n = 16) | 583.7 ± 109.1 | 571.8 ± 114.8 | 517.9 ± 110.6 | 520.9 ± 129.1 | ||||
| LPA (min·day−1) | STEP (n = 17) | 189.3 ± 57.9 | 210.2 ± 62.2 | 252.7 ± 82.0 | 259.0 ± 65.3 | 0.27 | <0.001 | 0.30 |
| UNSUP‐PA (n = 16) | 174.0 ± 67.7 | 180.2 ± 66.7 | 199.8 ± 62.8 | 231.1 ± 81.2 | ||||
| SUP‐PA (n = 16) | 209.1 ± 82.8 | 216.7 ± 73.9 | 249.4 ± 90.5 | 237.4 ± 76.6 | ||||
| MVPA (min·day−1) | STEP (n = 17) | 60.9 ± 45.2 | 71.5 ± 33.3 | 76.9 ± 41.0 | 75.3 ± 40.2 | 0.74 | <0.001 | 0.98 |
| UNSUP‐PA (n = 16) | 49.2 ± 44.3 | 63.3 ± 49.8 | 67.6 ± 53.4 | 64.8 ± 50.2 | ||||
| SUP‐PA (n = 16) | 55.3 ± 46.9 | 75.4 ± 43.4 | 80.3 ± 53.8 | 75.3 ± 55.4 | ||||
| Bouted MVPA (min·day−1) | STEP (n = 17) | 35.4 ± 33.5 | 42.8 ± 23.6 | 51.2 ± 33.5 | 47.0 ± 28.2 | 0.94 | <0.001 | 0.81 |
| UNSUP‐PA (n = 16) | 25.6 ± 36.0 | 38.3 ± 42.6 | 46.1 ± 45.5 | 41.7 ± 44.5 | ||||
| SUP‐PA (n = 16) | 28.0 ± 23.5 | 44.4 ± 24.0 | 54.3 ± 37.2 | 49.6 ± 38.7 | ||||
| Bouted MVPA steps (steps·day−1) | STEP (n = 17) | 2,178 ± 1,391 | 3,579 ± 1,615 | 4,067 ± 2,149 | 3,762 ± 1,762 | 0.79 | <0.001 | 0.94 |
| UNSUP‐PA (n = 16) | 1,943 ± 2,724 | 3,415 ± 4,066 | 3,480 ± 3,738 | 3,363 ± 3,534 | ||||
| SUP‐PA (n = 16) | 1,385 ± 826 | 3,148 ± 1,601 | 3,859 ± 2,506 | 3,096 ± 1,451 | ||||
| Intensity of MVPA (METs) | STEP (n = 16) | 4.4 ± 0.8 | 4.8 ± 0.9 | 4.9 ± 0.9 | 5.0 ± 1.1 | 0.43 | 0.01 | 0.68 |
| UNSUP‐PA (n = 11) | 4.2 ± 0.6 | 4.7 ± 0.6 | 4.5 ± 0.8 | 4.5 ± 0.6 | ||||
| SUP‐PA (n = 13) | 4.3 ± 0.4 | 4.5 ± 0.6 | 4.6 ± 0.7 | 4.7 ± 0.8 | ||||
SED: sedentary time (<1.5 METs per minute).
LPA: light‐intensity physical activity (≥1.5 METs per minute to <3.0 METs per minute).
MVPA: moderate‐to‐vigorous physical activity (≥3.0 METs per minute in bouts of ≥1 min).
Bouted MVPA: (≥3.0 METs per minute in bouts ≥10 min).
Bouted MVPA steps: (steps/day at ≥3.0 METs per minute in bouts ≥10 min).
Intensity of MVPA: (average METs per minute of moderate‐to‐vigorous physical activity in bouts ≥10 min).
Figure 2.
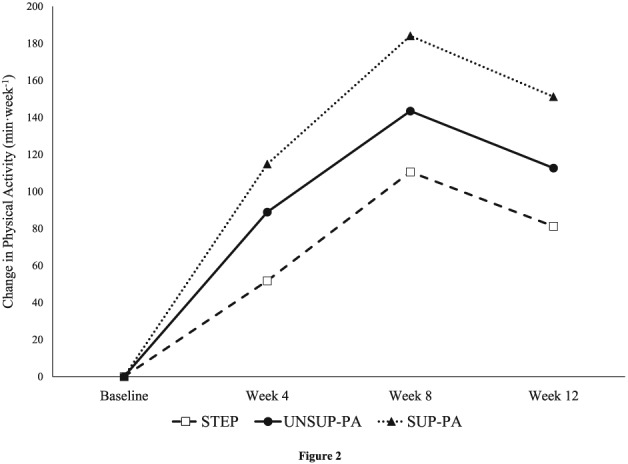
Change in objectively measured moderate‐to‐vigorous physical activity completed in bouts of ≥10 min.
STEP, UNSUP‐PA and SUP‐PA significantly decreased objectively measured SED (p < 0.001) and increased LPA (p < 0.001) over the 12‐week intervention. Analyses were repeated with SED represented as a percentage of wear time and had the same pattern with all groups significantly reducing SED over the 12‐week intervention (STEP: −8.6±10.7%, UNSUP‐PA: −6.4±8.2%, SUP‐PA: −6.9±7.0%). There were no group or group by time effects for SED or LPA.
Change in weight and body composition
Change in weight and body composition is shown in Table 3. STEP, UNSUP‐PA and SUP‐PA had significant reductions weight (p < 0.001) with no differences between the groups. Percent weight loss was also not significantly different between the groups (STEP: −6.0 ± 4.0%, UNSUP‐PA: −5.8 ± 3.6%, SUP‐PA: −4.5 ± 3.5%; p < 0.43). Weight loss of 5% has been suggested as a minimal goal of standard behavioural weight loss interventions; 1 thus, STEP, UNSUP‐PA and SUP‐PA were further examined based upon achievement of 5% weight loss. Adjusted for multiple comparisons, Chi square analyses demonstrated that STEP (n = 12) and UNSUP‐PA (n = 11) had more individuals attain 5% weight loss compared to SUP‐PA (n = 5) (p < 0.05).
Table 3.
Change in weight, body composition, anthropometrics and fitness
| P‐values | |||||||
|---|---|---|---|---|---|---|---|
| Outcome | Group | Baseline | 12 weeks | Change | Group | Time | Group × Time |
| Weight (kg) | STEP (n = 17) | 87.7 ± 14.7 | 82.3 ± 14.1 | −5.3 ± 3.6 | 0.81 | <0.001 | 0.36 |
| UNSUP‐PA (n = 16) | 86.8 ± 13.1 | 81.6 ± 11.8 | −5.1 ± 3.3 | ||||
| SUP‐PA (n = 16) | 84.0 ± 13.7 | 80.1 ± 13.2 | −3.8 ± 3.0 | ||||
| Percent weight change (%) | STEP (n = 17) | −6.0 ± 4.0 | 0.43 | ||||
| UNSUP‐PA (n = 16) | −5.8 ± 3.6 | ||||||
| SUP‐PA (n = 16) | −4.5 ± 3.5 | ||||||
| Fat mass (kg) | STEP (n = 17) | 33.7 ± 6.3 | 29.6 ± 6.2 | −4.1 ± 2.4 | |||
| UNSUP‐PA (n = 16) | 35.4 ± 7.6 | 31.3 ± 8.2 | −4.0 ± 2.8 | 0.77 | <0.001 | 0.95 | |
| SUP‐PA (n = 15) | 34.6 ± 6.7 | 30.8 ± 6.4 | −3.8 ± 2.8 | ||||
| Fat free mass (kg) | STEP (n = 17) | 50.9 ± 10.5 | 49.7 ± 10.5 | −1.2 ± 1.7 | 0.69 | <0.001 | 0.06 |
| UNSUP‐PA (n = 16) | 48.2 ± 9.9 | 47.2 ± 9.3 | −1.0 ± 1.1 | ||||
| SUP‐PA (n = 15) | 47.3 ± 11.1 | 47.3 ± 11.2 | −0.1 ± 1.4 | ||||
| Total body fat (%) | STEP (n = 17) | 38.7 ± 4.6 | 36.2 ± 5.6 | −2.5 ± 2.1 | 0.49 | <0.001 | 0.96 |
| UNSUP‐PA (n = 16) | 41.1 ± 6.9 | 38.5 ± 8.4 | −2.6 ± 2.3 | ||||
| SUP‐PA (n = 15) | 41.2 ± 6.8 | 38.5 ± 7.2 | −2.7 ± 2.2 | ||||
| Waist circumference (cm) | STEP (n = 17) | 100.1 ± 9.6 | 94.6 ± 8.4 | −5.5 ± 5.8 | 0.68 | <0.001 | 0.32 |
| UNSUP‐PA (n = 16) | 101.8 ± 6.8 | 97.9 ± 8.3 | −3.9 ± 5.6 | ||||
| SUP‐PA (n = 15) | 101.8 ± 9.2 | 94.7 ± 9.3 | −7.0 ± 5.9 | ||||
| Hip circumference (cm) | STEP (n = 17) | 109.5 ± 8.8 | 105.3 ± 7.1 | −4.2 ± 3.9 | 0.67 | <0.001 | 0.65 |
| UNSUP‐PA (n = 16) | 109.8 ± 6.5 | 105.7 ± 7.3 | −4.0 ± 2.7 | ||||
| SUP‐PA (n = 15) | 111.3 ± 9.2 | 108.1 ± 8.1 | −3.2 ± 3.2 | ||||
| Peak VO2 (mL kg·min−1) | STEP (n = 17) | 27.9 ± 5.5 | 29.2 ± 6.0 | 1.3 ± 2.4 | 0.26 | <0.001 | 0.01 |
| UNSUP‐PA (n = 16) | 23.9 ± 4.5 | 27.7 ± 5.7 | 3.8 ± 3.2 | ||||
| SUP‐PA (n = 16) | 24.4 ± 4.2 | 28.2 ± 4.9 | 3.8 ± 1.6 | ||||
| Peak VO2 (L·min−1) | STEP (n = 17) | 2.43 ± 0.56 | 2.39 ± 0.60 | −0.04 ± 0.19 | 0.44 | <0.001 | <0.01 |
| UNSUP‐PA (n = 16) | 2.08 ± 0.52 | 2.25 ± 0.54 | 0.17 ± 0.24 | ||||
| SUP‐PA (n = 16) | 2.09 ± 0.59 | 2.31 ± 0.71 | 0.22 ± 0.23 | ||||
Change in body composition and circumferences measures were also similar between treatment groups. Significant reductions in fat mass (p < 0.001), % fat (p < 0.001), lean mass (p < 0.001), waist circumference (p < 0.0001) and hip circumference (p < 0.0001) were observed in all groups, with no significant group or group × time effects.
Change in cardiorespiratory fitness
Cardiorespiratory fitness data are presented in Table 3. Cardiorespiratory fitness improved over the 12‐week intervention (p < 0.001), and there was a significant group × time interaction effect (p = 0.01). Post‐hoc analysis revealed a greater improvement in fitness in both SUP‐PA (3.8 ± 1.6 mL kg·min−1) and UNSUP‐PA (3.8 ± 3.2 mL kg·min−1) compared to STEP (1.3 ± 2.4 mL kg·min−1) (p < 0.05). There was no statistical difference between SUP‐PA and UNSUP‐PA for change in cardiorespiratory fitness. Because weight change could be a potential confounder in interpreting changes in relative VO2 (mL kg·min−1), analyses were also performed using absolute VO2 (L·min−1). There was a significant group × time interaction with UNSUP‐PA (0.17 ± 0.24 L·min−1) and SUP‐PA (0.22 ± 0.23 L·min−1) improving more than STEP (−0.04 ± 0.19 L·min−1) (p < 0.01). There was no significant difference between UNSUP‐PA and SUP‐PA.
Change in energy intake
There was a significant reduction in caloric intake (p < 0.01), fat intake (p < 0.01), carbohydrate intake (p < 0.001) and protein intake (p < 0.01) for STEP, UNSUP‐PA and SUP‐PA over the 12‐week intervention. There were no significant differences between groups, and there were no group × time interactions. There were no changes in percent of intake from fat (p = 0.34) or percent of intake from carbohydrates (p = 0.75); however, there was a significant increase in percent intake from protein (p < 0.01) for all treatment groups. Data are presented in Table 4.
Table 4.
Change in dietary intake
| P‐values | |||||||
|---|---|---|---|---|---|---|---|
| Outcome | Group | Baseline | 12 weeks | Change | Group | Time | Group × Time |
| Energy Intake (kcal·day−1) | STEP (n = 17) | 1,885 ± 905 | 1,497 ± 522 | −388 ± 1,056 | 0.51 | <0.01 | 0.88 |
| UNSUP‐PA (n = 16) | 1,773 ± 922 | 1,342 ± 438 | −431 ± 953 | ||||
| SUP‐PA (n = 14) | 1,774 ± 679 | 1,214 ± 370 | −561 ± 862 | ||||
| Dietary fat (g) | STEP | 76.0 ± 39.4 | 54.4 ± 20.8 | −21.5 ± 32.3 | 0.89 | <0.01 | 0.79 |
| UNSUP‐PA | 74.3 ± 51.5 | 48.6 ± 17.8 | −25.7 ± 54.7 | ||||
| SUP‐PA | 69.5 ± 30.7 | 53.5 ± 18.8 | −15.9 ± 22.4 | ||||
| Dietary carbohydrates (g) | STEP | 216.6 ± 107.3 | 151.2 ± 66.8 | −65.4 ± 80.6 | 0.79 | <0.001 | 0.66 |
| UNSUP‐PA | 194.3 ± 84.6 | 153.7 ± 64.0 | −40.7 ± 85.2 | ||||
| SUP‐PA | 215.8 ± 95.6 | 167.8 ± 47.0 | −48.0 ± 72.9 | ||||
| Dietary protein (g) | STEP | 75.5 ± 36.6 | 60.3 ± 24.7 | −15.2 ± 23.9 | 0.73 | <0.01 | 0.85 |
| UNSUP‐PA | 69.5 ± 40.3 | 53.0 ± 19.2 | −16.4 ± 40.5 | ||||
| SUP‐PA | 71.7± 28.2 | 61.3 ± 19.8 | −10.4 ± 20.5 | ||||
| % intake from fat | STEP | 36.6 ± 5.0 | 36.9 ± 7.0 | 0.3 ± 5.8 | 0.48 | 0.34 | 0.64 |
| UNSUP‐PA | 37.1 ± 8.1 | 35.1 ± 5.7 | −2.0 ± 8.4 | ||||
| SUP‐PA | 35.0 ± 6.6 | 33.9 ± 5.1 | −1.1 ± 6.1 | ||||
| % intake from carb | STEP | 46.8 ± 7.4 | 44.7 ± 7.4 | −2.1 ± 6.7 | 0.51 | 0.75 | 0.47 |
| UNSUP‐PA | 47.0 ± 9.6 | 48.2 ± 6.3 | 1.2 ± 8.5 | ||||
| SUP‐PA | 48.6 ± 8.8 | 48.5 ± 7.2 | −0.1 ± 7.5 | ||||
| % intake from protein | STEP | 16.6 ± 3.7 | 18.3 ± 4.6 | 1.7 ± 3.8 | 0.58 | <0.01 | 0.74 |
| UNSUP‐PA | 15.9 ± 2.3 | 16.9 ± 2.1 | 1.0 ± 2.2 | ||||
| SUP‐PA | 16.4 ± 2.9 | 17.6 ± 3.1 | 1.2 ± 2.9 | ||||
Discussion
The results of this study demonstrate that, when combined with a 12‐week standard behavioural weight loss intervention, supervised and unsupervised physical activity result in increases in objective measures of physical activity. Moreover, STEP, UNSUP‐PA and SUP‐PA resulted in similar reductions in body weight and changes in body composition. These findings suggest that the three physical activity programmes examined in this study are feasible options for increasing physical activity and promoting weight loss within a standard behavioural weight loss intervention.
It is likely that weight loss outcomes were predominantly influenced by changes in energy intake. By design, STEP, UNSUP‐PA and SUP‐PA were given the same dietary recommendations and delivered via the same weekly behavioural lessons in an attempt to minimize variations in energy intake changes between groups. All three groups significantly reduced caloric intake by ~400 to 500 kcals·day−1 across the intervention with no differences between groups. In addition, changes in macronutrient intake were also similar across treatment groups. Because there were no differences in energy intake, it is not surprising that there were no differences in weight change and body composition change between the groups.
STEP, UNSUP‐PA and SUP‐PA were successful at increasing levels of MVPA completed in bouts of ≥10 min with no differences between groups. Results of this study suggest that prescribing unsupervised physical activity can be just as effective as supervised physical activity for increasing MVPA completed in bouts of ≥10 min. This is important because MVPA, and more specifically MVPA completed in bouts of ≥ 10 min, are associated with improved long‐term weight loss and weight maintenance 20, 21, 22. STEP, UNSUP‐PA and SUP‐PA demonstrated similar decreases in MVPA from weeks 8 to 12 despite physical activity recommendations remaining constant. It is unclear why all of the intervention conditions demonstrated this response, and further investigation of this pattern is warranted. However, while speculative, this may reflect the need for more effective behavioural strategies to sustain physical activity beyond the initial 8 weeks or for the final weeks leading up to study completion. In addition, all groups showed an increase in LPA and a decrease in SED across the 12‐week intervention. Thus, all three physical activity programmes elicited similar physical activity responses including changes in SED, LPA and MVPA.
The observed weight losses are comparable to previous standard behavioural weight loss intervention that were 3–6 months in duration 10, 11, 12. Results of the current study closely parallel the findings of Craighead and Blum, which found that combining a standard behavioural weight loss intervention with supervised exercise induced a weight loss of 5.0 ± 1.2 kg, while contracted (unsupervised) exercise induced a weight loss of 3.8 ± 1.4 kg 12. However, physical activity participation data were not reported by Craighead and Blum 12, whereas these data are reported in the current study. Moreover, the current study reported that both STEP and UNSUP‐PA had significantly more individuals achieving 5% weight loss compared to SUP‐PA. It is unclear why STEP and UNSUP‐PA had higher rates of individuals achieving 5% weight loss because physical activity and energy intake were not different between groups. Nonetheless, this is an intriguing finding that warrants further investigation.
Both UNSUP‐PA and SUP‐PA improved relative and absolute fitness more than STEP in response to this intervention. When comparing SUP‐PA and UNSUP‐PA, the results of the current study closely parallel those of Perri et al., which found that supervised exercise and home‐based exercise improved relative VO2 peak and absolute oxygen consumption after 6 months of training 10. While it is unclear why STEP did not improve absolute fitness, it is possible that there were differences in intensity or volume of physical activity compared to SUP‐PA and UNSUP‐PA that were not detectable with the measures used in this study.
A unique contribution of this study was to compare a steps/day physical activity prescription (STEP) to both SUP‐PA and UNSUP‐PA. Objective physical activity data confirmed that STEP closely matched the step recommendations throughout the intervention and had similar changes in physical activity behaviours (i.e. SED, LPA and MVPA) compared to SUP‐PA and UNSUP‐PA. Because walking is an easy, safe and highly accessible form of physical activity, this finding has multiple public health implications. Physical activity in the form of walking and brisk walking may facilitate engagement in physical activity within the context of a standard behavioural weight loss intervention, and this may contribute to weight loss. Physical activity prescriptions in the form of steps/day recommendations may be well received in the general population, especially with the influx of consumer physical activity devices available. Moreover, for individuals who prefer walking vs. other forms of physical activity, this study provides evidence that this form of physical activity is sufficient to elicit significant weight loss when combined with dietary change.
The limitations of this study should be considered when interpreting the observed results. This study was 12 weeks in duration, which may not represent the effectiveness of these different intervention strategies if observed for a longer period of time. Moreover, this study focused on initial weight loss rather than maintenance, so it will be necessary to determine if these strategies to increase physical activity have similar effects on weight loss maintenance. Despite the participants self‐reporting <60 min·week−1 of structured physical activity upon entry into this study, these participants were relatively more active than population averages based on objective assessment at study entry, which may have influenced the findings. Furthermore, this study may have been underpowered to detect meaningful clinical difference between the intervention conditions. This may be a result of the sample size being based on the ability to detect a 20 min per week difference between groups, which may have been too small of a difference, or due to the higher than anticipated variance observed in objectively measured physical activity in this study. However, these data may be valuable to inform future samples sizes in similar studies of physical activity.
Conclusion
This study demonstrates that unsupervised physical activity programmes can be as effective as a supervised programme for increasing MVPA during a standard behavioural weight loss intervention for adults who are overweight or obese. Within the context of a standard behavioural weight loss intervention, increased MVPA was also accompanied by significant reductions in body weight and favourable reductions in body fatness. Future studies that do not have the facilities or resources to conduct supervised physical activity sessions may benefit from prescribing physical activity in a similar unsupervised manner. Whether the results of this study will apply to interventions of longer duration or for other study populations warrants further investigation. However, this study provides compelling evidence that unsupervised physical activity, prescribed in minutes or steps, can elicit engagement in physical activity that is similar to supervised physical activity within the context of a comprehensive standard behavioural weight loss intervention in adults who are overweight or obese.
Funding
University of Pittsburgh School of Education
Disclosures
Seth Creasy, PhD has nothing to disclose.
Renee J. Rogers, PhD reports grants from Weight Watchers International, outside the submitted work.
Kelliann K. Davis, PhD has nothing to disclose.
Bethany Barone Gibbs, PhD reports grants from Humanscale, outside the submitted work.
Erin E. Kershaw, MD: No conflicts to disclose
John M. Jakicic, PhD reports grants from Weight Watchers International, grants from HumanScale, personal fees from Weight Watchers International, grants from National Institutes of Health, outside the submitted work.
Acknowledgements
We would like to thank Sara Kovacs, Meghan McGuire, Robert Kowalsky, Matthew O'Dell, Katherine Collins, Shawn Raybuck, Marissa Marcin, Pat Donahue and Melissa Vendetti for their help with recruitment, data collection, intervention sessions and exercise supervision. In addition, we would like to thank all of the employees of the University of Pittsburgh Physical Activity and Weight Management Research Center for their help with this study. This research was supported by the University of Pittsburgh School of Education.
Creasy, S. A. , Rogers, R. J. , Davis, K. K. , Gibbs, B. B. , Kershaw, E. E. , and Jakicic, J. M. (2017) Effects of supervised and unsupervised physical activity programmes for weight loss. Obesity Science & Practice, 3: 143–152. doi: 10.1002/osp4.107.
References
- 1. Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol 2014; 63: 2985–3023. [DOI] [PubMed] [Google Scholar]
- 2. Wadden TA, Webb VL, Moran CH, Bailer BA. Lifestyle modification for obesity: new developments in diet, physical activity, and behavior therapy. Circulation 2012; 125: 1157–1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Jakicic JM, Tate DF, Lang W, et al. Effect of a stepped‐care intervention approach on weight loss in adults: a randomized clinical trial. JAMA 2012; 307: 2617–2626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ross R, Dagnone D, Jones PJ, et al. Reduction in obesity and related comorbid conditions after diet‐induced weight loss or exercise‐induced weight loss in men: a randomized, controlled trial. Ann Intern Med 2000; 133: 92–103. [DOI] [PubMed] [Google Scholar]
- 5. Ross R, Janssen I, Dawson J, et al. Exercise‐induced reduction in obesity and insulin resistance in women: a randomized controlled trial. Obes Res 2004; 12: 789–798. [DOI] [PubMed] [Google Scholar]
- 6. Jakicic JM, King WC, Marcus MD, et al. Short‐term weight loss with diet and physical activity in young adults: The IDEA study. Obesity 2015; 23: 2385–2397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dunn AL, Marcus BH, Kampert JB, Garcia ME, Kohl HW III, Blair SN. Comparison of lifestyle and structured interventions to increase physical activity and cardiorespiratory fitness: a randomized trial. JAMA 1999; 281: 327–334. [DOI] [PubMed] [Google Scholar]
- 8. Sevick MA, Dunn AL, Morrow MS, Marcus BH, Chen GJ, Blair SN. Cost‐effectiveness of lifestyle and structured exercise interventions in sedentary adults: results of project ACTIVE. Am J Prev Med 2000; 19: 1–8. [DOI] [PubMed] [Google Scholar]
- 9. Andersen RE, Wadden TA, Bartlett SJ, Zemel B, Verde TJ, Franckowiak SC. Effects of lifestyle activity vs structured aerobic exercise in obese women: a randomized trial. JAMA 1999; 281: 335–340. [DOI] [PubMed] [Google Scholar]
- 10. Perri MG, Martin AD, Leermakers EA, Sears SF, Notelovitz M. Effects of group‐versus home‐based exercise in the treatment of obesity. J Consult Clin Psychol 1997; 65: 278. [DOI] [PubMed] [Google Scholar]
- 11. Leermakers EA, Jakicic JM, Viteri J, Wing RR. Clinic‐based vs. home‐based interventions for preventing weight gain in men. Obes Res 1998; 6: 346–352. [DOI] [PubMed] [Google Scholar]
- 12. Craighead LW, Blum MD. Supervised exercise in behavioral treatment for moderate obesity. Behav Ther 1989; 20: 49–59. [Google Scholar]
- 13. Benito PJ, Neiva C, Gonzalez‐Quijano PS, Cupeiro R, Morencos E, Peinado AB. Validation of the SenseWear armband in circuit resistance training with different loads. Eur J Appl Physiol 2012; 112: 3155–3159. [DOI] [PubMed] [Google Scholar]
- 14. Berntsen S, Hageberg R, Aandstad A, et al. Validity of physical activity monitors in adults participating in free‐living activities. Br J Sports Med 2010; 44: 657–664. [DOI] [PubMed] [Google Scholar]
- 15. Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982; 14: 377–381. [PubMed] [Google Scholar]
- 16. Block G, Woods M, Potosky A, Clifford C. Validation of a self‐administered diet history questionnaire using multiple diet records. J Clin Epidemiol 1990; 43: 1327–1335. [DOI] [PubMed] [Google Scholar]
- 17. Jakicic JM, Marcus M, Gallagher KI, et al. Evaluation of the SenseWear Pro Armband to assess energy expenditure during exercise. Med Sci Sports Exerc 2004; 36: 897–904. [DOI] [PubMed] [Google Scholar]
- 18. Miller GD, Jakicic JM, Rejeski WJ, et al. Effect of varying accelerometry criteria on physical activity: the look ahead study. Obesity 2013; 21: 32–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Donnelly JE, Hill JO, Jacobsen DJ, et al. Effects of a 16‐month randomized controlled exercise trial on body weight and composition in young, overweight men and women: the Midwest Exercise Trial. Arch Intern Med 2003; 163: 1343–1350. [DOI] [PubMed] [Google Scholar]
- 20. Jakicic JM, Clark K, Coleman E, et al. American College of Sports Medicine position stand. Appropriate intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc 2001; 33: 2145–2156. [DOI] [PubMed] [Google Scholar]
- 21. Jakicic JM, Tate DF, Lang W, et al. Objective physical activity and weight loss in adults: the step‐up randomized clinical trial. Obesity 2014; 22: 2284–2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc 2009; 41: 459–471. [DOI] [PubMed] [Google Scholar]


