Mental health is a major concern worldwide and India is not far behind in sharing this. If we evaluate developments in the field of mental health, the pace appears to be slow. Dr. Brock Chisholm, the first Director-General of the World Health Organization (WHO), in 1954, had presciently declared that “without mental health there can be no true physical health.”[1] More than 60 years later, the scenario has not altered substantially. About 14% of the global burden of disease is attributed to neuropsychiatric disorders. The burden of mental disorders is likely to have been underestimated because of inadequate appreciation of the inter-play between mental illness and other health disorders.[2] There remain considerable issues of priority-setting based on the burden of health problems and of addressing inequalities in relation to determinants and solutions for health problems.
Progress in mental health service delivery has been slow in most low- and middle-income countries. Barriers include the existing public-health priorities and its influence on funding; challenges to delivery of mental health care in primary-care settings; the low numbers of those trained in mental health care; and the lack of mental health perspective in public-health leadership.[3] There have been numerous calls for invoking political will, for enhancing advocacy and for galvanizing community participation; all with scant improvement in outcomes.
Thus, it becomes now opportune to explore the paradigm of mental health awareness as a means of combating stigma, enhancing prevention, ensuring early recognition, and also stimulating simple and practical interventions within the community. Today there are opportunities in terms of growing acknowledgement of mental disorders as key targets of global health action, as well as of leveraging new technologies particularly internet, big data and cell phones in amplifying simple field interventions found successful in primary care and other echelons.
MENTAL HEALTH AWARENESS
Mental health awareness campaigns have yielded positive outcomes. Some of the strategies undertaken to target awareness and address stigma around mental illness include participation by family members, sensitization to treatment and social inclusion.[4,5] Lack of knowledge about the mental illnesses poses a challenge to the mental health care delivery system.[6] Research has highlighted the role of community-based systems in low-income countries and has also yielded positive results in creating awareness, thereby impacting participation.[7]
Awareness and health literacy are two sides of the same coin. Stigma and discrimination are negative consequences of ignorance and misinformation.[8] There are a few studies which have measured mental health literacy in the Indian context. One study found mental health literacy among adolescents to be very low, i.e. depression was identified by 29.04% and schizophrenia/psychosis was recognized only by 1.31%. Stigma was noted to be present in help-seeking.[9]
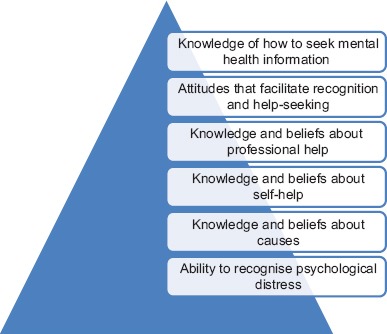
These findings reinforce the need to increase awareness of mental health. Mental health literacy is a related concept which is increasingly seen as an important measure of the awareness and knowledge of mental health disorders. Health literacy has been described as “ability to access, understand, and use the information to promote and maintain good health.”[10] Mental health literacy encompasses recognition, causes, self-help, facilitation of professional intervention, and navigating the information highway [Table 1]. Attitudes which hinder recognition and appropriate help-seeking can be counter-acted by information which is already readily available in the public domain. There are plenty of examples of awareness positively impacting mental health outcomes like the Norwegian campaign to reduce the duration of untreated psychosis.[11]
Table 1.
Components of mental health literacy: Jorm[12]
The impact of stigma has led to the institution of various programs worldwide to challenge the stereotypes and discrimination that generate social disability. Mental health awareness programs have had favorable impact and can produce positive change in people's views of mental illnesses. However, more robust evaluations are needed to assess the long-term impact of approaches to increasing mental health literacy worldwide.[13]
INDIAN SCENARIO
The WHO has defined sustainable development goals and elaborated the impact of mental illnesses and suicide on them. The suicide rate in India in 2015 at 15.7/100,000 is higher than the regional average of 12.9 and the global average of 10.6.[14] Suicide is the leading cause of death among those aged 15–29 in India.[15] There remains a massive unaddressed need within the population.
The treatment gap, as measured by the absolute difference between the prevalence of mental illnesses and the treated proportion, has been found to be 76%–85% in less-developed countries.[16] One of the major reasons attributed to such a wide treatment gap is the problem of inadequate resources. In India, inadequacy exists in infrastructure as well as in human resources.[17] Despite improvements in various health indicators, India contributes disproportionately to the global burden of disease. Our health indicators compare unfavorably with other middle-income countries and India's regional neighbors. A large proportion of the population ends up impoverished because of high out-of-pocket health-care expenditures and suffers the adverse consequences of the poor quality of care.[18] Task-shifting to nonspecialist community health workers has been recommended as an effective strategy for delivery of efficacious treatments in low-resource settings.[19] Given the dire shortage in numbers of psychiatrists, psychologists, psychiatric nurses, and social workers; piggy-backing on primary care systems and employing innovative force-multipliers are future courses of action.
ROADMAP FOR MENTAL HEALTH AWARENESS
For the large Indian population to be involved in its own mental health, the only way forward is through enhancing mental health awareness which will generate its own demand. With rising awareness, it can be expected that early recognition and access to treatment will follow, as will the adoption of preventive measures. It can also be expected that with enlarging awareness in a democratic society, advocacy, leveraging of political will, funding, and cross-synergies shall follow. It is envisaged that bulk of the awareness contributions shall flow from the following six platforms [Figure 1].
Figure 1.
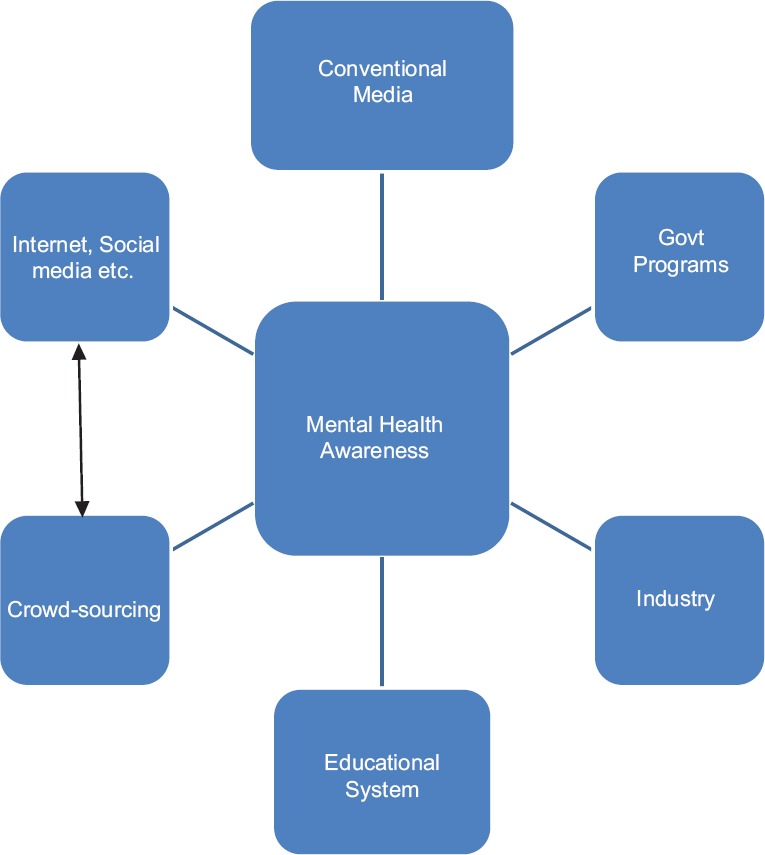
Model for mental health awareness
Conventional media
Media has been the cornerstone of the previous action in the field of mental health awareness. Celebrity endorsements, like the recent one by actress Deepika Padukone who shared her experience of depression, together with succinct tag-lines of advertisements and content-rich narrations and documentaries; have been the mainstay of media drives so far.
Making evidence-based mental health information easily available to journalists and other content providers like internet portals from trusted and reliable sources like Indian Psychiatry Society, research organizations, medical colleges, etc., through their websites is a relatively simple step. Accessibility of simply translated jargon-free content in various regional languages in written and spoken forms will go a long way. It also behoves professionals in the mental health domain to take the lead in engaging and partnering with the media. Encouraging recovered patients to make their success stories accessible to all shall make good the paucity of authentic narratives.
Government programs
Despite some caviling about the quantum, the government remains the biggest single spender in the mental health sector. While most new interventions remain isolated and confined to urban areas, it is only the public health system through large programs which can reach the rural masses. Apart from the National and District Mental Health Programs, the National Rural Health Mission is on its way to becoming the vehicle for delivering mental health as a part of integrated primary care at the cutting edge of the public healthcare system. Seeing that it partners with existing private and alternative care providers in a nonthreatening manner, shall help such large interventions synergize and succeed.
Educational system
Most chronic and debilitating mental illnesses have their onset before 24 years of age when most are a part of the educational system. From including mental health narratives in curricula toward, de-stigmatization, removing discrimination and early detection, to empowering stakeholders for early detection and simple interventions; the educational system yields myriad opportunities for enhancing mental health awareness.
Industry
The organized sector suffers significant loss of effective workforce through mental ill-health. Not only as a part of corporate social responsibility but also to maintain productivity, it becomes important to engage with mental health awareness in a concerted fashion.
Internet, social media and cellphones
Hand-held devices and the social media can truly be game-changers in the propagation of effective mental health interventions through focussed amplification, and not just in increasing information. With the greater utilization of big data, the understanding of subtle and distributed patterns over large volumes shall inform decision making.
Crowd-sourcing
The ultimate convergence of information and technology in a free society results in crowd-sourcing which breaks down barriers of geography, historical inequities, and economies of scale. It is the true involvement of communities real and virtual, harnessed to make a change. Thus, dynamic ideas of individuals can synergize with the success stories of nongovernmental organizations to amplify them across geographies and time. Crowd-funding is a successful model in testing radical ideas which flounder outside the mainstream.
CONCLUSION
Considering that most of the earlier strategies to enhance mental health have not succeeded over the past six decades or more in less-developed countries, the time has come to take on a new approach with renewed vigor. Mental health awareness can become both the means and the way of ending this apathy. Progressive government policies based on evidence-based approaches, an engaged media, a vibrant educational system, a responsive industry, aggressive utilization of newer technologies and creative crowd-sourcing might together help dispel the blight of mental illnesses.
REFERENCES
- 1.Kolappa K, Henderson DC, Kishore SP. No physical health without mental health: Lessons unlearned? Bull World Health Organ. 2013;91:3–3A. doi: 10.2471/BLT.12.115063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet. 2007;370:859–77. doi: 10.1016/S0140-6736(07)61238-0. [DOI] [PubMed] [Google Scholar]
- 3.Saraceno B, van Ommeren M, Batniji R, Cohen A, Gureje O, Mahoney J, et al. Barriers to improvement of mental health services in low-income and middle-income countries. Lancet. 2007;370:1164–74. doi: 10.1016/S0140-6736(07)61263-X. [DOI] [PubMed] [Google Scholar]
- 4.Patel V, Saxena S. Transforming lives, enhancing communities – Innovations in global mental health. N Engl J Med. 2014;370:498–501. doi: 10.1056/NEJMp1315214. [DOI] [PubMed] [Google Scholar]
- 5.Rebello TJ, Marques A, Gureje O, Pike KM. Innovative strategies for closing the mental health treatment gap globally. Curr Opin Psychiatry. 2014;27:308–14. doi: 10.1097/YCO.0000000000000068. [DOI] [PubMed] [Google Scholar]
- 6.Brown VA, Harris JA, Russell JY. Tackling Wicked Problems through the Transdisciplinary Imagination. London: Earthscan; 2010. [Google Scholar]
- 7.Trani JF, Ballard E, Bakhshi P, Hovmand P. Community based system dynamic as an approach for understanding and acting on messy problems: A case study for global mental health intervention in Afghanistan. Confl Health. 2016;10:25. doi: 10.1186/s13031-016-0089-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pinfold V. London: Rethink Publications; 2003. How can We Make Mental Health Education Work? Example of Successful Local Mental Health Awareness Programme Challenging Stigma and Discrimination. [Google Scholar]
- 9.Ogorchukwu JM, Sekaran VC, Nair S, Ashok L. Mental health literacy among late adolescents in South India: What they know and what attitudes drive them. Indian J Psychol Med. 2016;38:234–41. doi: 10.4103/0253-7176.183092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nutbeam D, Wise M, Bauman A, Harris E, Leeder S. Canberra: Australia Government Publishing Service; 1993. Goals and Targets for Australia's Health in the Year 2000 and Beyond. [Google Scholar]
- 11.Joa I, Johannessen JO, Auestad B, Friis S, McGlashan T, Melle I, et al. The Key to Reducing Duration of Untreated First Psychosis: Information Campaigns Schizophr Bull. 2008;34:466–72. doi: 10.1093/schbul/sbm095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jorm AF. Mental health literacy. Public knowledge and beliefs about mental disorders. Br J Psychiatry. 2000;177:396–401. doi: 10.1192/bjp.177.5.396. [DOI] [PubMed] [Google Scholar]
- 13.Pinfold V, Stuart H, Thornicroft G, et al. Working with young people: The impact of mental health awareness programs in schools in the UK and Canada. World Psychiatry. 2005;4(Suppl 1):48–52. [Google Scholar]
- 14.World Health Organization. World Health Statistics 2016. Geneva 27, Switzerland: World Health Organization; 2016. [Google Scholar]
- 15.Patel V, Ramasundarahettige C, Vijayakumar L, Thakur JS, Gajalakshmi V, Gururaj G, et al. Suicide mortality in India: A nationally representative survey. Lancet. 2012;379:2343–51. doi: 10.1016/S0140-6736(12)60606-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581–90. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 17.Thirunavukarasu M. Closing the treatment gap. Indian J Psychiatry. 2011;53:199–201. doi: 10.4103/0019-5545.86803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel V, Parikh R, Nandraj S, Balasubramaniam P, Narayan K, Paul VK, et al. Assuring health coverage for all in India. Lancet. 2015;386:2422–35. doi: 10.1016/S0140-6736(15)00955-1. [DOI] [PubMed] [Google Scholar]
- 19.Patel V, Goel DS, Desai R. Scaling up services for mental and neurological disorders in low-resource settings. Int Health. 2009;1:37–44. doi: 10.1016/j.inhe.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]


