Abstract
Background:
Medical students undergo significant stress during training which may lead to own suffering or problem in patient care. High level of burnouts and depression is also not uncommon. The transition from preclinical to clinical training has been regarded as crucial to student in relation to the stress.
Methodology:
An assessment of perceived stress and its relation to general psychopathology, the pattern of coping, and burnout in the final-year medical student was done to bring out clear nature, pattern, and extent of the problem.
Results:
Perceived stress had statistically significant association with general psychopathology and depressive-anxiety component of burnout. Acceptance, positive reframing, humor, planning, and active coping correlated with lower score on perceived stress.
Conclusion:
Higher score on perceived stress was associated with higher scores on general psychopathology and burnout. Age of joining MBBS course and doctor in the family did not affect the stress significantly. People who displayed positive coping strategies had lesser stress and general psychopathology.
Keywords: Burnout, coping, general psychopathology, medical students, perceived stress
There is ample support to the fact that the medical students go through a lot of stress during their medical study.[1,2] Sources of stress may be academic, social, financial, or personal problems. While academic stress involves dealing with death/suffering and relating with teachers, being a medical student itself comes with a lot of changes in personal life, leisure, and social commitments. Workload, overwhelming wealth of information, financial constraints, family dynamics, and examination pressure further increases the stress.[3,4,5] Burnout is group of symptoms which arises in professional in relation to the work. Pressure to perform in medical education can make an erstwhile, a hardworking and committed person increasingly dissatisfied or disillusioned with various aspects of work and life.[6] Evidence suggests that mental illness during medical training may predict later problems in terms of personal suffering or patient care.[7] Medical student does not seek professional help for themselves which they would otherwise render to their patients in similar situations.[8,9,10]
Little is known about the prevalence of mental distress in medical students; some have been extrapolation from medical fraternity of various hierarchies. Most of them have been from questionnaire data or qualitative group interviews. Psychiatric caseness was found in 22%–36%,[11] depression in 14%–21%,[12,13,14] and anxiety in 29%[15] in various studies in medical professionals. Indian studies have found the stress in up to 73.5% of the medical students.[16] Knowledge about the psychiatric conditions is important and would require attention if found. It also may suggest a vulnerability which a medical student need not be responsible for. Studies have found higher depression rates in medical student vis-a-vis general population even before their starting medical training.[17]
Whether it is the demand of medical education or the inherent disposition of the individual which leads to the manifestation of the problem has been questioned by many researchers in the past. Clear delineation has remained impossible.[18,19,20] Greater perception of stress leads to more mental distress. Burnout though a measure of induced distress has also been associated with neuroticism and Type A behavior.[21] Researchers have found the burnout to be as high as 45% in multicentric studies on medical students.[2]
Off late, there is trend toward developing curricula with integration of preclinical training and clinical training at an early phase of education. Although medical students have more negative attitude toward traditional curricula, there is no evidence that either model attracts more vulnerability.[22] However, the transition from preclinical training to clinical training in traditional curricula has been recognized as crucial to stress.[23] While internal disposition does affect the distress and burnout, it has been seen that the coping strategies of an individual also impact the manifestations significantly. Coping strategies, which are behavioral or psychological efforts employed to master or minimize stressful events, affect the medical students variably. Studies have revealed that the active coping strategies such as positive reframing, planning, and acceptance affect the mental health outcome favorably.[24]
With the above literature in review, we felt that there are less structured studies on medical students in particular (not medical professionals) in their transition phase from preclinical to clinical (final-year medical students) phase, data in Indian paradigm being further less. An assessment of perceived stress, coping pattern, burnout, and general psychopathology in final-year medical undergraduate students was done with objectives of determining the level of perceived stress and its relation with coping, burnout, and general psychopathology.
METHODOLOGY
The study was undertaken in a Government Medical College with an established MCI curriculum. One hundred students in their final year of medical training were taken up for the study. All the students were briefed about the study and informed consents were taken. They were then assessed using the following:
Structured pro forma for recording demographic profile and relevant medical and social history
Perceived Stress Scale:[25] A most widely used 10-item psychological instrument to measure the degree to which situations in an individual's life are appraised as stressful, which measures the perceived stress over the last 1-month duration
BRIEF COPE: The Brief COPE[26] is a self-report questionnaire used to assess a number of different coping behaviors and thoughts a person may have in response to a specific situation
General Health Questionnaire-12 (GHQ-12):[27] a self-administered standardized 12-item screening test sensitive for the presence of psychiatric disorders in individuals. Score of more than 2 was taken as abnormal
Maslach burnout inventory:[28] Valuable tool for assessing professional burnout in human service, education, business, and government professions. Burnout is assessed on following paradigms: depressive-anxiety syndrome, depersonalization, and reduction of person achievement. Scoring on each component yields mild, moderate, and high level of burnout
Appropriate tests of significance & correlation were done and statistically analyzed.
RESULTS
The mean age of the study population was 22.45 years (standard deviation [SD] - 0.77) with the mean age of joining MBBS curriculum being 18.48 (SD - 0.80). Both median and mode for joining the MBBS course was 19 years. Nearly 18.3% of students have doctor as their relative, common being their father. Favorite pastime was listening to music in 14.1% of the cases. Favorite sport of the student was football (28.3%). Examination, viva voce, and studying were few common causes which made people anxious seen in 23.3%, 13.3%, and 12.4%, respectively. Others were case taking, missing class, getting up late, loud sounds, etc. Sleeping and listening to music were common modes of reducing anxiety in 18.4% and 9.2%, respectively. Others were jogging, going to gym, eating, watching comedy shows, etc.
Mean and SDs of important psychological variables are shown in Table 1. Nearly 53.5% of students were above cutoff on scores of general psychopathology. On depressive-anxiety score, 76.8% had low-level burnout, 18.1% had moderate level burnout, and others (5.1%) had high burnout. On depersonalization, component 29.3% had mild level burnout, 30.3% had moderate level burnout, and a significant portion of students (41.4%) had high-level burnout. On reduction of personal achievement component, 26.4% had mild level burnout and 27.2% had moderate level burnout whereas 46.4% students had high level of reduction of personal achievement.
Table 1.
Mean and standard deviation of important psychological variables

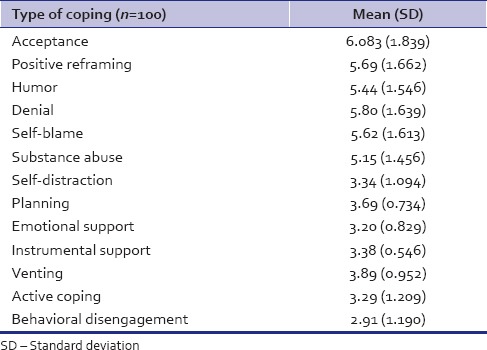
The mean and SD of various components of coping are shown in Table 2. Acceptance, positive reframing, humor, denial, self-blame, and substance abuse were found to be more commonly practiced coping.
Table 2.
Mean and standard deviation of components of coping skills
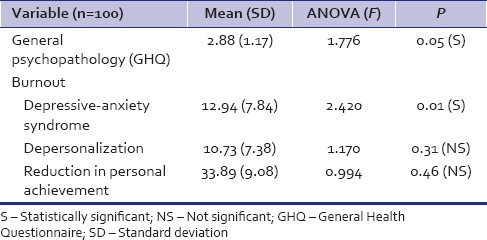
Analysis of association of various psychological variables with the perceived stress scale scores is shown in Table 3. The same was reconfirmed with various studies in Table 4. Perceived stress had statistically significant association with general psychopathology and depressive-anxiety component of burnout. Additional ANOVA of age at present (F = 1.260, P = 0.250) and while joining MBBS course (F = 0.989, P = 0.417) did not reveal any statistical association with the scores on perceived stress scale.
Table 3.
Association of various psychological variables with perceived stress
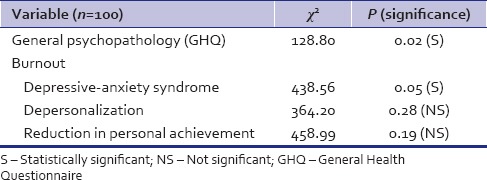
Table 4.
Association of variance of various psychological variables with perceived stress
Statistically significant correlation is shown in Table 5. Perceived stress was found to have significant positive correlation with burnout depressive-anxiety syndrome. Perceived stress though had significant association did not show any statistical correlation with general psychopathology. Perceived stress also did not correlate with age (ρ = 0.128, P = 0.20) or age of joining MBBS course (ρ = 0.062, P = 0.54). Age (ρ = 0.311, P = 0.00) and age of joining MBBS course (ρ = 0.222, P = 0.03), respectively, however had significant positive correlation with burnout depressive-anxiety syndrome.
Table 5.
Correlation analysis of perceived stress with various psychological parameters
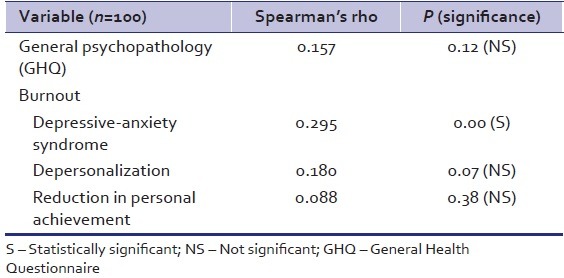
Correlation analysis of coping skill is shown in Table 6. Acceptance, positive reframing, humor, planning, and active coping correlated with lower score on perceived stress.
Table 6.
Significant correlation of perceived stress with various coping measures

DISCUSSION
The mean age of joining MBBS and current age of the study population is reflection of existing policy of applying for professional examination only after completing 12th standard by around 17 years of age. The observation was akin to those of Supe[16] in the Indian context. Demographic distribution can be reflection of choice versus population concentration of young generation in various states. Not much research exists in such direction. Around a fifth of the students had probable inspiration from their kith and kin to join the medical profession; however, evaluation did not reveal any higher stress in these students. This finding is not in consonance with those of Chandrasekhar et al.[25] This might be due to their prior sensitization and realistic orientation by relatives. Anxiety about examination, viva voce, and study have been vocalized in the past by other researchers as well.[3,4] They used established relaxation methods to overcome their stress.
Nearly 53.5% of students were above cut-off on scores of general psychopathology. This score was higher than few researchers,[11,16,25] it was lesser than that of Inam[29] who found it to the tune of 60% and above. High-level burnout was 5.1% on depressive-anxiety; 41.4% on depersonalization; and 46.4% on reduction of personal achievement. Dyrbye et al. also found the burnout to be around 45% in their study.[2]
Perceived stress had statistically significant association with general psychopathology and depressive-anxiety component of burnout. It was also seen that higher the perceived stress, higher was the scores on burnout. Findings are akin to those of similar researches in the past.[6,28] Not much research exists on medical students exists in this direction. GHQ failed to show any correlation despite significant association. Not much research exists in this direction. Although age at present and age of joining MBBS course had significant positive correlation with burnout depressive-anxiety syndrome, they fail to achieve any statistical association with perceived stress or other entity.
People who had fewer score on perceived stress were found to have more of acceptance, positive reframing, humor, planning, and active coping as coping methods. Active coping strategies such as positive reframing, planning, and acceptance have proven to be healthy in the past as well.[24]
CONCLUSION
Higher score on perceived stress was associated with higher scores on general psychopathology and burnout. Age of joining MBBS course and doctor in the family did not affect the stress significantly. People who displayed positive coping strategies had lesser stress and general psychopathology.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This paper is based on short-term student scholarship program under Indian Council of Medical Research.
REFERENCES
- 1.Wallin U, Runeson B. Attitudes towards suicide and suicidal patients among medical students. Eur Psychiatry. 2003;18:329–33. doi: 10.1016/j.eurpsy.2003.03.006. [DOI] [PubMed] [Google Scholar]
- 2.Dyrbye LN, Thomas MR, Huntington JL, Lawson KL, Novotny PJ, Sloan JA, et al. Personal life events and medical student burnout: A multicenter study. Acad Med. 2006;81:374–84. doi: 10.1097/00001888-200604000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Miller PM, Surtees PG. Psychological symptoms and their course in first-year medical students as assessed by the Interval General Health Questionnaire (I-GHQ) Br J Psychiatry. 1991;159:199–207. doi: 10.1192/bjp.159.2.199. [DOI] [PubMed] [Google Scholar]
- 4.Omokhodion FO. Psychosocial problems of pre-clinical students in the University of Ibadan medical school. Afr J Med Med Sci. 2003;32:135–8. [PubMed] [Google Scholar]
- 5.Thompson D, Goebert D, Takeshita J. A program for reducing depressive symptoms and suicidal ideation in medical students. Acad Med. 2010;85:1635–9. doi: 10.1097/ACM.0b013e3181f0b49c. [DOI] [PubMed] [Google Scholar]
- 6.Guthrie E, Black D. Psychiatric disorder, stress and burn-out. Adv Psychiatr Treat. 1997;3:275–81. [Google Scholar]
- 7.Firth-Cozens J, Greenhalgh J. Doctors' perceptions of the links between stress and lowered clinical care. Soc Sci Med. 1997;44:1017–22. doi: 10.1016/s0277-9536(96)00227-4. [DOI] [PubMed] [Google Scholar]
- 8.Rosvold EO, Bjertness E. Physicians who do not take sick leave: Hazardous heroes? Scand J Public Health. 2001;29:71–5. [PubMed] [Google Scholar]
- 9.Rosvold EO, Bjertness E. Illness behaviour among Norwegian physicians. Scand J Public Health. 2002;30:125–32. doi: 10.1080/14034940210133744. [DOI] [PubMed] [Google Scholar]
- 10.Hooper C, Meakin R, Jones M. Where students go when they are ill: How medical students access health care. Med Educ. 2005;39:588–93. doi: 10.1111/j.1365-2929.2005.02175.x. [DOI] [PubMed] [Google Scholar]
- 11.Guthrie E, Black D, Bagalkote H, Shaw C, Campbell M, Creed F. Psychological stress and burnout in medical students: A five-year prospective longitudinal study. J R Soc Med. 1998;91:237–43. doi: 10.1177/014107689809100502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tjia J, Givens JL, Shea JA. Factors associated with undertreatment of medical student depression. J Am Coll Health. 2005;53:219–24. doi: 10.3200/JACH.53.5.219-224. [DOI] [PubMed] [Google Scholar]
- 13.Givens JL, Tjia J. Depressed medical students' use of mental health services and barriers to use. Acad Med. 2002;77:918–21. doi: 10.1097/00001888-200209000-00024. [DOI] [PubMed] [Google Scholar]
- 14.Clark DC, Zeldow PB. Vicissitudes of depressed mood during four years of medical school. JAMA. 1988;260:2521–8. [PubMed] [Google Scholar]
- 15.Caplan RP. Stress, anxiety, and depression in hospital consultants, general practitioners, and senior health service managers. BMJ. 1994;309:1261–3. doi: 10.1136/bmj.309.6964.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Supe AN. A study of stress in medical students at Seth G.S. Medical College. J Postgrad Med. 1998;44:1–6. [PubMed] [Google Scholar]
- 17.Zoccolillo M, Murphy GE, Wetzel RD. Depression among medical students. J Affect Disord. 1986;11:91–6. doi: 10.1016/0165-0327(86)90065-0. [DOI] [PubMed] [Google Scholar]
- 18.Rosal MC, Ockene IS, Ockene JK, Barrett SV, Ma Y, Hebert JR. A longitudinal study of students' depression at one medical school. Acad Med. 1997;72:542–6. doi: 10.1097/00001888-199706000-00022. [DOI] [PubMed] [Google Scholar]
- 19.Enns MW, Cox BJ, Sareen J, Freeman P. Adaptive and maladaptive perfectionism in medical students: A longitudinal investigation. Med Educ. 2001;35:1034–42. doi: 10.1046/j.1365-2923.2001.01044.x. [DOI] [PubMed] [Google Scholar]
- 20.McManus IC, Keeling A, Paice E. Stress, burnout and doctors' attitudes to work are determined by personality and learning style: A twelve year longitudinal study of UK medical graduates. BMC Med. 2004;2:29. doi: 10.1186/1741-7015-2-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shaufeli W, Enzmann D. The Burnout Companion to Study and Practice – A Critical Analysis. London: Taylor and Francis; 1998. [Google Scholar]
- 22.Gude T, Hjortdahl P, Anvik T, Baerheim A, Fasmer OB, Grimstad H, et al. Does change from a traditional to a new medical curriculum reduce negative attitudes among students. A quasi-experimental study? Med Teach. 2005;27:737–9. doi: 10.1080/01421590500271498. [DOI] [PubMed] [Google Scholar]
- 23.Helmers KF, Danoff D, Steinert Y, Leyton M, Young SN. Stress and depressed mood in medical students, law students, and graduate students at McGill University. Acad Med. 1997;72:708–14. doi: 10.1097/00001888-199708000-00018. [DOI] [PubMed] [Google Scholar]
- 24.Sreeramareddy CT, Shankar PR, Binu VS, Mukhopadhyay C, Ray B, Menezes RG. Psychological morbidity, sources of stress and coping strategies among undergraduate medical students of Nepal. BMC Med Educ. 2007;7:26. doi: 10.1186/1472-6920-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chandrashekhar TS, Pathiyil RS, Binu VS, Mukhopadhyay C, Biswabina R, Menezes RG. Psychological morbidity, sources of stress and coping strategies among undergraduate medical students of Nepal. BMC Medical Education. 2007;7:26. doi: 10.1186/1472-6920-7-26. doi:101186/1472-6920-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carver CS. You want to measure coping but your protocol's too long: Consider the brief COPE. Int J Behav Med. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 27.Goldberg D. The Detection of Psychiatric Illness by Questionnaire: A Technique for the Identification and Assessment of Non-Psychotic Psychiatric Illness. London, New York: Oxford University Press; 1972. [Google Scholar]
- 28.Maslach C, Leiter MP. The Truth About Burnout: How Organizations Cause Personal Stress and What to Do About It. San Francisco, CA: Jossey-Bass; 1997. [Google Scholar]
- 29.Inam SB. Anxiety and depression among students of a medical college in Saudi Arabia. Int J Health Sci (Qassim) 2007;1:295–300. [PMC free article] [PubMed] [Google Scholar]


