Abstract
Background
Medical Emergency Teams (METs) are designed to respond to signs of clinical decline in order to prevent cardiopulmonary arrest and reduce mortality. The frequency of MET activation prior to pediatric cardiopulmonary resuscitation (CPR) is unknown.
Methods
Within the Get With The Guidelines-Resuscitation Registry (GWTG-R), we identified children with bradycardia or cardiac arrest requiring CPR on the general inpatient or telemetry floors from 2007–2013. We examined the frequency with which CPR outside the ICU was preceded by a MET evaluation. In cases where MET evaluation did not occur, we examined the frequency of severely abnormal vital signs at least 1 hour prior to CPR that could have prompted a MET evaluation but did not.
Results
Of 215 children from 23 hospitals requiring CPR, 48 (22.3%) had a preceding MET evaluation. Children with MET evaluation prior to CPR were older (6.8 ± 6.5 vs. 3.1 ± 4.7 years of age, p < 0.001) and were more likely to have metabolic/electrolyte abnormalities (18.8% vs. 5.4%, p=0.006), sepsis (16.7% vs. 4.8%, p=0.01), or malignancy (22.9% vs. 5.4%, p<0.001). Among patients who did not have a MET called and with information on vital signs, 55/141 (39.0%) had at least one abnormal vital sign that could have triggered a MET.
Conclusion
The majority of pediatric patients requiring CPR for bradycardia or cardiac arrest do not have a preceding MET evaluation despite a significant number meeting criteria that could have triggered the MET. This suggests opportunities to more efficiently use MET teams in routine care.
Keywords: pediatrics, medical emergency team, cardiopulmonary resuscitation
Medical emergency teams (METs), otherwise known as rapid response teams (RRTs) are interventions which have been advanced to reduce the incidence of and morbidity associated with in-hospital cardiac arrest (IHCA). Alerted by criteria suggestive of clinical decline (i.e. change in vital signs or neurologic status), a MET offers the opportunity to intervene early and direct management towards prevention of further clinical deterioration. Within the pediatric literature, MET teams have had variable results, with some studies demonstrating a decline in rates of cardiac arrest and hospital mortality following MET implementation and others failing to demonstrate such improvements.1–8 Importantly, there have been no studies, to date, that have specifically evaluated whether pediatric METs are being appropriately activated when patients exhibit clinical instability. Understanding whether MET teams are being appropriately utilized may provide important insights as to why pediatric MET studies have yielded conflicting results.
The Get With the Guidelines®-Resuscitation Registry (GWTG-Resuscitation), a large prospective registry of pediatric and adult patients requiring cardiopulmonary resuscitation (CPR), recently introduced a MET module specifically designed to collect data on patients for whom a MET was called. Together, the cardiopulmonary arrest (CPA) and MET modules allow for an examination of the frequency of MET evaluations and vital sign abnormalities among patients who progress to requirement for CPR. Accordingly, within this registry, we examined how often pediatric patients requiring CPR had a preceding MET evaluation, and if not, whether there were “missed” opportunities for activating the MET if such patients exhibited severe abnormalities in their vital signs prior to requiring CPR.
Methods
Data Source
A full description of GWTG-Resuscitation and its development has been previously published.9 In brief, GWTG-Resuscitation is a national prospective voluntary registry, sponsored by the American Heart Association, of pediatric and adult patients with IHCA or profound bradycardia requiring CPR. Trained hospital personnel at participating hospitals collect data on all consecutive patients experiencing pulselessness or pulse with poor perfusion requiring chest compressions and/or defibrillation with or without the need for bag-valve-mask ventilation. Patients are identified using a combination of the medical record, cardiac arrest forms, and telepage records. All cardiac arrests at hospitals participating in the registry are included in the database. Collected data include facility data, patient demographic data, pre-event data, event data (including vital signs), outcome data, and quality improvement data. Vital sign data is abstracted from the medical record. All vital signs in the four hours preceding cardiac arrest are recorded. Similarly, GWTG-Resuscitation collects information on all patients with a MET evaluation at hospitals choosing to submit data to both the MET and CPA modules. Standardized international Utstein definitions for defining clinical variables and outcomes are used to ensure uniformity in reporting.10,11 Data accuracy is further ensured by rigorous certification of hospital staff and use of standardized software with data checks for completeness and accuracy.
Study Outcome
The primary outcome of interest was the proportion of pediatric patients requiring CPR who had a preceding MET evaluation. We defined a preceding MET evaluation as one which occurred within 24 hours prior to CPR in the case of CPR occurring on the general inpatient or telemetry floors. In cases where a patient had CPR in the ICU and had been transferred to the ICU by a MET, we defined a preceding MET evaluation as one which occurred within 48 hours of ICU transfer. Additionally, we were interested in the frequency of “missed” opportunities for a MET evaluation. A “missed” opportunity for a MET evaluation was defined as a patient with abnormal vital signs preceding their need for CPR for whom a MET was not called. Because we did not have information regarding the specific criteria used for activating the MET at each hospital, we used commonly accepted, age-specific criteria for determining the presence of abnormal vital signs that could have triggered a MET evaluation (Table 1).3
Table 1.
Age-Specific Criteria for Determining Physiological Decline to Activate a Medical Emergency Team
| Age | Systolic BP (mmHg) | Bradycardia (beats per minute) | Tachycardia (beats per minute) | Tachypnea (breaths per minute) |
|---|---|---|---|---|
| Term-3 months | <50 | <100 | >180 | >60 |
| 4–12 months | <60 | <100 | >180 | >50 |
| 1–4 years | <70 | <90 | >160 | >40 |
| 5–12 years | <80 | <80 | >140 | >30 |
| >12 years | <90 | <60 | >130 | >30 |
Adapted from Tibballs et al. Pediatric Critical Care Medicine.. May 2009;10(3):306–312
Selection of Participants
Because the purpose of our study was to examine whether a pediatric patient requiring CPR had a preceding MET evaluation, we linked the registry’s CPA and MET databases and then restricted our analyses to those hospitals that submitted data to both modules. The MET module was introduced into the registry in 2007. In order to ensure that our analysis was restricted to a time when the MET team was active at a given hospital, we only included CPR events that occurred after the date of the first MET submission from each hospital.
We included in our study population, cardiac arrest cases among pediatric patients (≤18 years of age) occurring between April 1, 2007 and December 21, 2013 (provided that they occurred after the date of the hospital’s first MET submission, as described above). We excluded patients with rhythms other than asystole, pulseless electrical activity (PEA), ventricular fibrillation (VF), pulseless ventricular tachycardia (VT), or bradycardia (i.e. supraventricular tachycardia, sinus tachycardia, unknown rhythm). We also excluded those patients without available survival information. Additionally, because a MET generally responds to patients on the general inpatient or telemetry units who are at risk for clinical deterioration, we excluded those patients whose cardiac arrest occurred in hospital locations where a MET would not generally be called (i.e. intensive care unit, ambulatory/outpatient areas, cardiac catheterization laboratory, delivery suite, diagnostic/interventional areas, emergency department, nursery, operating room, post-anesthesia care unit, same day surgical area). However, because one of the potential interventions of the MET is to transfer patients to the ICU, we included patients requiring CPR within an ICU but who were recently (within preceding 48 hours) transferred to the ICU by a MET team (to give credit for the MET team response prior to CPR).
Statistical Analysis
Our first objective was to determine the proportion of patients requiring CPR with a preceding MET evaluation. The proportion of pediatric patients requiring CPR with preceding MET evaluation was described using simple proportions. Characteristics of those patients with and without a MET evaluation preceding their need for CPR were compared using student’s t-test for continuous variables and chi-square or Fisher’s exact test for categorical variables. We then determined variability in utilization of the MET among hospitals by determining the frequency of cases requiring CPR with preceding MET evaluation among the seven hospitals (167 patients) with at least 10 CPR events. Hospital variation in use of the MET was described using simple descriptive statistics.
Finally, in order to determine the frequency of “missed” MET opportunities, we identified those patients requiring CPR without a preceding MET evaluation and determined the frequency of abnormal vital signs present <1 hour, ≥1- <2 hours, ≥2- <3 hours, ≥3- <4 hours, and ≥4 hours prior to CPR. We identified abnormal vital signs among all patients without a preceding MET and also subdivided patients based upon rhythm at the time of the resuscitation event (bradycardia vs. pulseless cardiac arrest rhythms). The frequency of abnormal vital signs in the hours preceding need for CPR was described using simple proportions.
All study analyses were performed with SAS 9.4 (SAS Institute, Cary, NC) and R version 2.15.0.12 All analyses were evaluated using a 2-sided significance level of 0.05. All authors have read and agree to the manuscript as written. The study was conducted on de-identified quality improvement registry data and did not meet criteria for requirement of informed consent. The American Heart Association’s GWTG-Resuscitation Committee approved the final manuscript draft.
Results
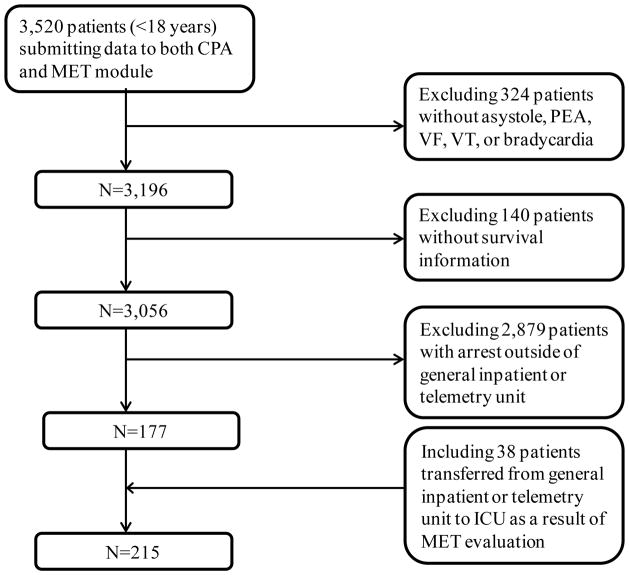
Between April 1, 2007 and December 31, 2013, a total of 3,520 children with an IHCA or a bradycardia event requiring chest compressions were identified (Figure 1). We excluded the 324 patients with rhythms other than asystole, PEA, VF, pulseless VT, or bradycardia and 140 patients without survival information. We excluded 2,879 patients whose cardiac arrest occurred in hospital locations other than the general inpatient or telemetry units. We included 38 patients requiring CPR within an ICU but who were transferred in the preceding 48 hours to the ICU as a result of MET activation. Our final study cohort included 215 patients from 23 different hospitals.
Figure 1.
Definition of the study cohort.
Of 215 patients requiring CPR, 48 (22.3%) had a preceding MET evaluation. The mean age of the study population was 3.9 ± 5.3 years. The majority of patients (58.6%) were male and 27.0% were of black race. The most common co-morbid condition was respiratory insufficiency, which occurred in 50.7% of patients. Over half (52.1%) of patients had a first-documented rhythm of bradycardia, 20.0% had asystole, 22.3% PEA, and 5.6% had VF or VT.
Table 2 summarizes the baseline characteristics of those with and without MET evaluation prior to their need for CPR. Children with a MET evaluation prior to CPR were older (6.8 ± 6.5 vs. 3.1 ± 4.7 years, p < 0.001). They were also more likely to have coexisting metabolic/electrolyte abnormalities (9/48 [18.8%] vs. 9/167 [5.4%], p=0.006), sepsis (8/48 [16.7%] vs. 8/167 [4.8%], p=0.01), or malignancy (11/48 [22.9%] vs. 9/167 [5.4%], p<0.001) at the time of CPR.
Table 2.
Baseline Characteristics of Patients With and Without MET Evaluation Preceding CPR
| Total (N =215) | Preceding MET Activation (n=48) | No Preceding MET Activation (n= 167) | P value | |
|---|---|---|---|---|
| Demographics | ||||
| Age | <0.001 | |||
| Mean ± SD | 3.9 ± 5.3 | 6.8 ± 6.5 | 3.1 ± 4.7 | |
| Median (IQR) | 1.0 (0.2, 7.0) | 3.5 (0.7, 14.0) | 0.7 (0.1, 3.0) | |
| Male Sex | 126 (58.6%) | 31 (64.6%) | 95 (56.9%) | 0.34 |
| Race | 0.88 | |||
| White | 114 (53.0%) | 25 (52.1%) | 89 (53.3%) | |
| Black | 58 (27.0%) | 15 (31.3%) | 43 (25.7%) | |
| Other | 16 (7.4%) | 3 (6.3%) | 13 (7.8%) | |
| Unknown | 27 (12.6%) | 5 (10.4%) | 22 (13.2%) | |
| Pre-Existing Conditions | ||||
| Heart failure this admission | 13 (6.0%) | 3 (6.3%) | 10 (6.0%) | 1.00 |
| Heart failure prior to admission | 6 (2.8%) | 1 (2.1%) | 5 (3.0%) | 1.00 |
| Hypotension | 25 (11.6%) | 19 (39.6%) | 6 (3.6%) | < 0.001 |
| Respiratory insufficiency | 109 (50.7%) | 24 (50.0%) | 85 (50.9%) | 0.91 |
| Renal insufficiency | 15 (7.0%) | 3 (6.3%) | 12 (7.2%) | 1.00 |
| Metabolic/Electrolyte | 18 (8.4%) | 9 (18.8%) | 9 (5.4%) | 0.006 |
| Abnormalities | ||||
| Sepsis | 16 (7.4%) | 8 (16.7%) | 8 (4.8%) | 0.01 |
| Pneumonia | 12 (5.6%) | 3 (6.3%) | 9 (5.4%) | 0.73 |
| Metastatic or hematologic malignancy | 20 (9.3%) | 11 (22.9%) | 9 (5.4%) | < 0.001 |
| Major trauma | 2 (0.9%) | 2 (4.2%) | 0 (0.0%) | 0.05 |
| Hepatic insufficiency | 5 (2.3%) | 3 (6.3%) | 2 (1.2%) | 0.07 |
| Baseline depression in CNS function | 32 (14.9%) | 5 (10.4%) | 27 (16.2%) | 0.32 |
| Acute CNS non-stroke event | 10 (4.7%) | 5 (10.4%) | 5 (3.0%) | 0.05 |
| Event Characteristics | ||||
| Initial Rhythm | 0.19 | |||
| Asystole | 43 (20.0%) | 5 (10.4%) | 38 (22.8%) | |
| PEA | 48 (22.3%) | 13 (27.1%) | 35 (21.0%) | |
| VF | 2 (0.9%) | 0 (0.0%) | 2 (1.2%) | |
| Pulseless VT | 10 (4.7%) | 4 (8.3%) | 6 (3.6%) | |
| Bradycardia | 112 (52.1%) | 26 (54.2%) | 86 (51.5%) | |
| Time of Arrest | 0.42 | |||
| Week day | 116 (54.0%) | 22 (45.8%) | 94 (56.3%) | |
| Weeknight | 36 (16.7%) | 10 (20.8%) | 26 (15.6%) | |
| Weekend | 63 (29.3%) | 16 (33.3%) | 47 (28.1%) | |
| Arrest Location | < 0.001 | |||
| General Inpatient Area | 109 (50.7%) | 8 (16.7%) | 101 (60.5%) | |
| Telemetry/Step-down | 68 (31.6%) | 2 (4.2%) | 66 (39.5%) | |
| Adult ICU | 1 (0.5%) | 1 (2.1%) | 0 (0.0%) | |
| Pediatric ICU | 37 (17.2%) | 37 (77.1%) | 0 (0.0%) | |
| Hospital Teaching Status | 0.006 | |||
| Major teaching* | 190 (88.4%) | 37 (77.1%) | 153 (91.6%) | |
| Minor teaching† | 24 (11.2%) | 10 (20.8%) | 14 (8.4%) | |
| Non-teaching | 1 (0.5%) | 1 (2.1%) | 0 (0.0%) | |
| Hospital Bed size | 0.178 | |||
| <250 beds | 1 (0.5%) | 1 (2.1%) | 0 (0.0%) | |
| 250–499 beds | 124 (57.7%) | 32 (66.7%) | 92 (55.1%) | |
| >499 beds | 90 (41.9%) | 15 (31.3%) | 75 (44.9%) | |
Abbreviations: MET, medical emergency team; SD, standard deviation; IQR, inter-quartile range; CNS, central nervous system; PEA, pulsesless electrical activity; VF, ventricular fibrillation; VT, ventricular tachycardia; ICU, intensive care unit
Includes institutions with residents and fellows
Includes institutions with residents
Among the 23 hospitals in the study cohort, 7 hospitals had at least 10 patients requiring CPR. Among the 7 hospitals with this case volume, the proportion of patients who had a MET evaluation prior to CPR varied substantially (median of 20%; inter-quartile range: 3.4%–29.8%; total range: 0%–36.4%).
To determine whether MET team activation could have occurred more frequently, we examined the vital signs of those patients without MET evaluation preceding their need for CPR. Of 167 patients without a MET evaluation, vital sign data was available for 141 (84.4%). Among these 141 patients, over one-third (36.9%) had one or more abnormal vital signs at least 1 hour preceding CPR. Table 3 shows the frequency and timeline of abnormal vital signs prior to CPR. Patients with any abnormal vital sign preceding their need for CPR had ample warning of physiological decline, with many exhibiting abnormal vital signs three or more hours before their cardiac arrest. Most patients with abnormal vital signs preceding CPR had only one abnormal vital sign, with tachypnea being the most common vital sign abnormality (Table 4). Patients with severe bradycardia had a similar frequency of abnormal vital signs compared to those with a pulseless cardiac arrest, with 29.6% experiencing one or more abnormal vital signs at least one hour preceding CPR.
Table 3.
Timing of Abnormal Vital Signs in Patients Requiring CPR without Preceding MET
| Timing of Abnormal Vital Signs | All Patients (PEA, VF, VT, asystole, bradycardia) N = 141 |
PEA, VF, VT asystole patients n = 70 |
Bradycardia only patients n=71 |
|---|---|---|---|
| No Abnormal Vital Signs | 86 (61.0%) | 38 (54.3%) | 48 (67.6%) |
| 0.5- <1 hour prior to CPR | 3 (2.1%) | 1 (1.4%) | 2 (2.8%) |
|
| |||
| ≥ 1 hour prior to CPR | 52 (36.8%) | 31 (44.3%) | 21 (29.6%) |
|
|
|
|
|
| 1- <2 hour prior to CPR | 7 (5.0%) | 4 (5.7%) | 3 (4.2%) |
| 2- <3 hour prior to CPR | 7 (5.0%) | 6 (8.6%) | 1 (1.4%) |
| 3- <4 hour prior to CPR | 16 (11.4%) | 6 (8.6%) | 10 (14.1%) |
| 4- <5 hour prior to CPR | 22 (15.6%) | 15 (21.4%) | 7 (9.9%) |
Abbreviations: MET, medical emergency team; IHCA, in-hospital cardiac arrest; PEA, pulseless electrical activity; VF, ventricular fibrillation; VT, ventricular tachycardia
Table 4.
Type of Vital Sign Abnormality Among Patients with Abnormal Vital Signs ≥1 hour prior to CPR
| N=52 | |
|---|---|
| Tachypnea* | 35 (67.3%) |
| Tachycardia* | 12 (23.1%) |
| Bradycardia* | 10 (19.2%) |
| Hypotension* | 6 (11.5%) |
|
| |
| 1 abnormal vital sign | 43 (82.7%) |
| 2 abnormal vital signs | 7 (13.5%) |
| >2 abnormal vital signs | 2 (3.8%) |
Abbreviations: CPR, cardiopulmonary resuscitation
Sum of individual vital sign abnormalities is greater than 50 as one patient could have ≥1 vital sign abnormality
Discussion
Within a large national registry, we evaluated the proportion of pediatric patients evaluated by a MET prior to an event requiring CPR. We then determined whether patients not evaluated by a MET had evidence of clinical deterioration, based upon the presence of one or more abnormal vital signs, representing a “missed” opportunity for MET evaluation. We found that the vast majority (77.7%) was not evaluated by a MET prior to emergent CPR, and a significant number of these had abnormal vital signs at least 1 hour prior to their CPR event that may have suggested impending deterioration. The findings of our study suggest an opportunity for hospitals to better utilize their MET team in patients meeting certain clinical criteria, in order to more rapidly recognize and treat children at risk for cardiopulmonary arrest.
There have been several prior studies evaluating the effectiveness of MET teams in the pediatric population. In a large, single center study evaluating the effectiveness of a MET at an academic center, the authors found a decrease in mean monthly mortality of 18% following implementation of the MET and a decrease in the monthly code rate per 1000 admissions of 71.2%.6 In another study of MET implementation at a pediatric hospital in Australia, the authors found a decrease in total hospital and unexpected ward deaths but did not find a decrease in rates of unexpected cardiac arrests following implementation of a MET.4 Still another study found no difference in the rates of all-cause hospital mortality in the pre vs. post MET period.5 Other studies have offered equivocal results with regards to the MET, with non-significant decreases in the rates of cardiac and respiratory arrests1 and no changes in mortality8 or a reduction in codes only when both cardiac and respiratory2 or respiratory arrests alone were considered.13
There have been several proposed explanations for the variability in success of the MET between different studies. Prior studies have postulated that the higher acuity at some centers translates into more patients at risk for cardiac arrest and thus a greater likelihood of detecting significant declines in rates of IHCA following MET implementation.6 Others have proposed that some hospitals adopted MET teams before others, which could explain differences in outcomes. Centers who recently adopted the MET may not yet have experienced significant improvement in outcomes compared to centers whose MET is well established and experienced.6 Still others have proposed that, unlike adults who may have a period of clinical instability prior to their cardiac arrest, children are better able to compensate and more likely to experience IHCA without preceding warning signs. While each of these theories could conceivably explain different outcomes between studies, the results of our study offer another very plausible explanation for the inconsistent success of the MET among hospitals. In our study, over three quarters of pediatric patients requiring CPR did not have an antecedent MET activation. Moreover, in many cases, patients demonstrated abnormal vital signs several hours prior to their event, suggesting that a significant number of pediatric patients do experience evidence of clinical instability prior to their requirement for CPR. Therefore, it seems possible that the lack of improved benefit after MET implementation in some studies could be due to MET underutilization and that centers adhering to MET calling criteria may achieve lower rates of IHCA and mortality following MET implementation.
The findings of our study suggest future opportunities for the study of pediatric METs. Though in our study, we were able to identify “missed” opportunities for activation of the MET, we were unable to identify the precise circumstances surrounding these “missed” opportunities. Future studies should focus on evaluating these specific circumstances in order to identify why a MET is not being activated despite abnormal vital signs. The concept of “failure-to-rescue” is one that is being increasingly described in the pediatric surgical literature but which has applications to other aspects of clinical care as well.14 Failure to rescue refers to the concept that hospitals with lower mortality rates may not necessarily be experiencing fewer complications, but rather may be better at recognizing and managing complications that do occur and consequently experiencing lower mortality rates. The presence of abnormal vital signs prior to CPR in our patient population suggests that the concept of failure to rescue may apply to pediatric IHCA and bradycardia events necessitating emergent CPR. Abnormal vital signs in sick patients invariably occur, but some hospitals may be using their MET teams more appropriately and be more effective in managing their patients with physiological decline. It is possible that improved utilization of the MET for patients meeting clinical criteria for physiological decline would lead to more rapid recognition and intervention for at-risk patients, ultimately leading to fewer cardiopulmonary arrests and lower mortality. Nonetheless, nearly two-thirds of patients did not meet criteria for MET activation suggesting that either clinical decline occurred rapidly or that more sensitive MET calling criteria may be needed, recognizing that more sensitive criteria needs to be balanced with the potential for false identification of patients at risk of cardiac arrest.
Our study should be interpreted in the context of the following limitations. First, we acknowledge that in defining a “missed” opportunity for activation of the MET, we based this solely on vital signs in the four hours preceding cardiac arrest. Given that hospitals likely utilize other data (i.e. clinical appearance, change in neurologic status, parental or provider concern, Pediatric Early Warning System [PEWS]) in deciding when to activate the MET, our ability to assess utilization of the MET may have been limited.15 Nonetheless, since this additional information typically represents other criteria for MET team activation, it is likely that our rates of CPR events with physiological decline in patients without a MET team evaluation preceding their CPR would have been even higher (i.e., worse). We also acknowledge that not all hospitals utilize the same specific vital sign criteria for activating their MET and that some hospitals may not adhere to strict vital sign cutoffs when deciding upon MET activation. However, the vital sign criteria we used for determining missed opportunities for MET activation included vital signs that would be accepted by most as being abnormal and which has been previously cited in the pediatric MET literature. Additionally, while we were able to identify the frequency of “missed” opportunities for utilization of the MET as well as the variability in utilization of the MET between hospitals, studies examining whether improved MET utilization would translate into improved outcomes are needed. Ideally, such a study would compare each hospital’s MET utilization rate with its risk-standardized mortality rate. However, with only seven hospitals containing at least ten cardiac arrest cases, we were underpowered for this type of analysis. In our study, though we were able to describe the proportion of cardiac arrest cases preceded by MET activation and to identify instances of “missed” opportunities for MET utilization, we were unable to identify the precise reason why a MET was not called. Though we presume that some of the “missed” opportunities for MET activation are because clinical instability was unrecognized or under-appreciated by the medical team, there are other instances where the medical team may have actively decided not to activate the MET for other reasons (i.e. high census in the intensive care unit precluding patient transfer; clinical instability addressed by the ward team so MET activation deemed unnecessary). Furthermore, there may have been instances of abnormal vital signs, for which there was appropriate clinical explanation and for which a MET may not have been necessary (i.e. tachycardia associated with fever). Future efforts should be directed towards investigating cases where a MET was not called in order to explore the specific circumstances and identify instances where a MET may have been clinically beneficial. Lastly, our study only represents data from those centers participating in the GWTG-Resuscitation Registry and may not be reflective of all centers. Participation in the GWTG-Resuscitation Registry reflects a commitment to quality improvement, and practice patterns may be different at non-registry hospitals.
Conclusion
Using a large national registry, we found that the majority of pediatric patients requiring CPR for bradycardia or cardiac arrest do not have a preceding MET evaluation, despite the fact that many patients had one or more abnormal vital signs in the hours preceding their event. The findings of our study suggest an opportunity for hospitals to better utilize their MET in order to lower the incidence of and improve outcomes for pediatric patients requiring CPR.
Acknowledgments
Funding/Support:
Dr. Chan is supported by a R01 Award (1R01HL123980) from the National Heart Lung and Blood Institute.
Abbreviations
- BP
blood pressure
Footnotes
- The authors have no conflicts of interest to disclose.
- Dr. Chan has worked as a consultant with the American Heart Association.
- Dr. Parshuram holds shares in a clinical decision support company.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Zenker P, Schlesinger A, Hauck M, et al. Implementation and impact of a rapid response team in a children’s hospital. Joint Commission Journal on Quality and Patient Safety/Joint Commission Resources. 2007;33(7):418–25. doi: 10.1016/s1553-7250(07)33048-1. [DOI] [PubMed] [Google Scholar]
- 2.Brilli RJ, Gibson R, Luria JW, et al. Implementation of a medical emergency team in a large pediatric teaching hospital prevents respiratory and cardiopulmonary arrests outside the intensive care unit. Pediatric Critical Care Medicine: A Journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2007;8(3):236–46. doi: 10.1097/01.PCC.0000262947.72442.EA. quiz 47. [DOI] [PubMed] [Google Scholar]
- 3.Tibballs J, Kinney S, Duke T, Oakley E, Hennessy M. Reduction of paediatric in-patient cardiac arrest and death with a medical emergency team: preliminary results. Archives of Disease in Childhood. 2005;90(11):1148–52. doi: 10.1136/adc.2004.069401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tibballs J, Kinney S. Reduction of hospital mortality and of preventable cardiac arrest and death on introduction of a pediatric medical emergency team. Pediatric Critical Care Medicine: A Journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2009;10(3):306–12. doi: 10.1097/PCC.0b013e318198b02c. [DOI] [PubMed] [Google Scholar]
- 5.Kotsakis A, Lobos AT, Parshuram C, et al. Implementation of a multicenter rapid response system in pediatric academic hospitals is effective. Pediatrics. 2011;128(1):72–8. doi: 10.1542/peds.2010-0756. [DOI] [PubMed] [Google Scholar]
- 6.Sharek PJ, Parast LM, Leong K, et al. Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU in a Children’s Hospital. JAMA. 2007;298(19):2267–74. doi: 10.1001/jama.298.19.2267. [DOI] [PubMed] [Google Scholar]
- 7.Bonafide CP, Localio AR, Roberts KE, Nadkarni VM, Weirich CM, Keren R. Impact of rapid response system implementation on critical deterioration events in children. JAMA Pediatrics. 2014;168(1):25–33. doi: 10.1001/jamapediatrics.2013.3266. [DOI] [PubMed] [Google Scholar]
- 8.Hanson CC, Randolph GD, Erickson JA, et al. A reduction in cardiac arrests and duration of clinical instability after implementation of a paediatric rapid response system. Quality & Safety in Health Care. 2009;18(6):500–4. doi: 10.1136/qshc.2007.026054. [DOI] [PubMed] [Google Scholar]
- 9.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58(3):297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 10.Cummins RO, Chamberlain D, Hazinski MF, et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital ‘Utstein style’. American Heart Association Circulation. 1997;95(8):2213–39. doi: 10.1161/01.cir.95.8.2213. [DOI] [PubMed] [Google Scholar]
- 11.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa) Circulation. 2004;110(21):3385–97. doi: 10.1161/01.CIR.0000147236.85306.15. [DOI] [PubMed] [Google Scholar]
- 12.R Development Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2008. http://www.R-project.org. [Google Scholar]
- 13.Hunt EA, Zimmer KP, Rinke ML, et al. Transition from a traditional code team to a medical emergency team and categorization of cardiopulmonary arrests in a children’s center. Archives of Pediatrics & Adolescent Medicine. 2008;162(2):117–22. doi: 10.1001/archpediatrics.2007.33. [DOI] [PubMed] [Google Scholar]
- 14.Pasquali SK, Li JS, Burstein DS, et al. Association of center volume with mortality and complications in pediatric heart surgery. Pediatrics. 2012;129(2):e370–6. doi: 10.1542/peds.2011-1188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raymond TT, Bonafide CP, Praestgaard A, et al. Pediatric Medical Emergency Team Events and Outcomes: A Report of 3647 Events From the American Heart Association’s Get With the Guidelines-Resuscitation Registry. Hospital Pediatrics. 2016;6(2):57–64. doi: 10.1542/hpeds.2015-0132. [DOI] [PMC free article] [PubMed] [Google Scholar]