Abstract
Men who have sex with men (MSM) are at disproportionate risk of acquisition of sexually transmitted infections (STIs). We used latent class analysis to examine patterns of sexual behavior among MSM and how those patterns are related to STIs. We examined patterns of sexual behavior using behavioral and clinical data from a cross-sectional study of 235 MSM who presented to an urban sexual health clinic for STI testing. Analyzed data were collected using a combination of interviewer- and self-administered surveys and electronic health records. We used latent class analysis to identify underlying subgroups of men based on their sexual behavior, described the demographics of the latent classes, and examined the association between the latent classes and STI status. We identified three latent classes of sexual behavior: Unprotected-Anal-Intercourse (UAI) only (67%), Partner-Seekers (14%), and Multiple-Behaviors (19%). Men in the Multiple-Behaviors class had a 67% probability of being STI-positive, followed by men in the UAI-only class (27%) and men in the Partner-Seekers class (22%). Examining the intersection of a variety of sexual practices indicates particular subgroups of MSM have the highest probability of being STI-positive.
INTRODUCTION
Sexually transmitted infections (STIs) are a growing public health problem in the United States (U.S.). Overall, rates of incident chlamydia, gonorrhea, and syphilis increased in 2014 for the first time since 2006, with respective rate increases among Americans of 2.8%, 15.1%, and 5.1% (CDC, 2015). In the U.S., men who have sex with men (MSM) are disproportionately impacted by STIs. MSM account for 83% of reported syphilis cases among men, and evidence from sentinel surveillance suggests that MSM are also burdened by increasing rates of gonorrhea and chlamydia (CDC, 2015), although national estimates of gonorrhea and chlamydia prevalence among MSM are largely unavailable because information on sex partners is not routinely collected in disease reports. These rising rates are particularly concerning because of the increased rates of HIV that are associated with STI infection (Galvin & Cohen, 2004). To develop effective disease control measures, researchers must better understand which sexual behaviors contribute to increased STI/HIV prevalence among MSM compared to other population groups (amfAR, 2008; Sullivan & Rosenberg, 2015). Current clinical guidelines and prevention strategies focus almost exclusively on unprotected anal intercourse (UAI) as a marker of risk (CDC, 2014; CDC, 2015b. However, MSM engage in a wide range of sexual behaviors, many of which have unknown correlations with STI/HIV (Rice et al, 2016). Choice of sexual behavior may be influenced by identification with a specific subgroup within the larger MSM community (Moskowitz, 2011). Research suggests that the MSM community, like all heterogeneous population groups, is made up of many different, and sometimes overlapping sub-communities, which differ with respect to perceptions of sex, sexuality, and risk; sociodemographics; sexual practices; and behavioral norms (amfAR, 2008; Moskowitz, 2011). Reported UAI does not fully capture STI/HIV risk, as more than one-third of gonorrhea and chlamydia infections among MSM occur in men who do not report UAI (Jin et al, 2007). Some other sexual behaviors are well described, but others have received little if any scientific attention. For example, group sex (sexual acts including more than two people at the same time) is reported by approximately one-quarter of MSM (Phillips et al, 2014; Rice et al, 2015) and has been significantly associated with STI (Rice et al, 2015). However, the potential STI/HIV risk associated with fisting (inserting a fist in to the rectum) is based largely on case reports (Cohen, Giles, & Nelson, 2004), not population-based research. Even among more widely described behaviors, the vast majority of published research focuses on characterizing a single behavior of interest (Klein, 2012; Noor & Rosser, 2014; Phillips et al, 2014; Rice et al, 2015). These reports provide valuable information about individual behaviors, but do not capture patterns of multiple behaviors occurring within a specific sexual experience or over a longer time period.
The CDC (CDC, 2015) and others (amfAR, 2008; Sullivan & Rosenberg, 2015) have highlighted the need to better understand the disproportionate burden of STIs and HIV among MSM, including a better understanding of specific behaviors and ways to provide more culturally-relevant care. Recent statistical advances allow for person-centered approaches to model patterns of behavior. One of these methods, latent class analysis (LCA) (Collins & Lanza, 2010), identifies underlying (latent) subgroups in a population based on individual responses to a set of variables, and characterizes the individual characteristics associated with subgroup membership. We use LCA to identify subgroups of individuals who engage in similar patterns of sexual behavior, in order to identify distinct profiles of sexual behavior among MSM and associations between those profiles and individual characteristics. We also document associations between behavior profiles and prevalent STI.
METHODS
We conducted this cross-sectional study between July 2012 and October 2013 in the sexual health clinic of a major Midwestern metropolitan health department. We screened all men presenting to the clinic for study eligibility. To be eligible, men were required to be able to speak and read English, be at least 18 years old, and report having had anal sex with a man in the last year. Written consent for study participation was obtained from all participants.
Data Collection
We collected data via interviewer-administered and self-administered surveys, using REDCap for electronic data capture (Harris et al, 2009). The self-administered survey included the most sensitive questions (e.g., specific sexual behaviors). Participants were compensated $10. We collected data on a variety of sexual behaviors in the last three months and over the lifetime, including insertive/receptive behaviors (UAI, oral sex, anal fingering, use of insertive sex toys, fisting, sounding, and enema use), behaviors that do not involve insertion of any fomite in to the mouth, urethra, or rectum (erotic asphyxiation, watersports, scatalogia, snowballing, use of sex sling, felching, and rimming), and behaviors that describe the context of the sex act (group sex and anonymous sex)(behavioral definitions are provided within methods section) (Rice et al, in press).
According to sexual health clinic protocols, all male patients are routinely tested for HIV, syphilis, urethral gonorrhea, and urethral chlamydia. Men who report receptive AI in the last year also undergo testing for rectal gonorrhea and rectal chlamydial infection; those who report oral sex are screened for oropharyngeal gonorrhea. Rectal and urethral chlamydia and gonorrhea are diagnosed by nucleic acid amplification testing (NAAT) via Tigris (Genprobe); culture is used to test for oropharyngeal gonorrhea. Syphilis is diagnosed through rapid plasma reagin (RPR) (Arlington Scientific) testing and confirmed by Treponema pallidum particle agglutination (TP-PA) or fluorescent treponemal antibody absorption (FTA-ABS). Test results are recorded in patients’ electronic health records (EHRs); these results were extracted and subsequently linked with survey.
Measures
Sexual Behaviors
Past three-month reports of eight behaviors were selected to include as binary items that together characterized the latent classes. These behaviors were chosen from among all behaviors (Rice et al, 2016) measured in the survey based on a priori hypotheses about STI risk associated with them, and based on the prevalence of these behaviors in our sample. We did not include behaviors with lower than 4% prevalence or higher than 90% prevalence, as these would not have permitted meaningful distinction between classes. The following behaviors were included in the LCA: UAI, fisting (insertion of fist in to rectum), enema use (injecting liquid or gas into the rectum, typically to expel its contents), felching (using mouth to suck semen from partner’s rectum), snowballing (oral exchange of semen between partners), use of a sex sling (sexual acts involving a harness that suspends one partner), use of insertive sex toys (toys that are inserted in to the body), anonymous sex (sex with a partner whose name you did not know), and group sex (sex with multiple individuals at the same time).
STI Status
Participants were coded STI-positive if they tested positive on the date of the interview for gonorrhea or chlamydia at any anatomical site or primary or secondary syphilis. If participants tested negative for all three infections, they were coded STI-negative.
Statistical Analyses
All statistical analyses were performed in SAS (Version 9.4, Cary, NC). We used descriptive statistics to examine characteristics of the sample, including age, race, ethnicity, education, employment, relationship status, sexual orientation, HIV status, sexual behaviors, and STI prevalence.
We conducted LCA to identify patterns of sexual behavior in our sample and identify subgroups of MSM most likely to have an STI. We performed LCA using PROC LCA [16]. Model identification was examined by comparing the solution obtained across 1000 sets of random starting values. The number of latent classes was selected based on information criteria, including the Akaike information criteria (AIC) and Bayesian information criteria (BIC), interpretability, and class separation. Optimal models are indicated by minimum values of AIC and BIC. Following model selection, we described each latent class of men by including each characteristic as a grouping variable in the latent class model and estimated the association between each characteristic and latent class membership by including each characteristic as a covariate in the model. Finally, we estimated the association between latent class membership and prevalent STI by including STI as a covariate and in the SAS macro LCA_Distal, which uses a flexible model-based approach to estimate the effect of latent class membership on a distal outcome (Lanza, Tan, & Bray, 2013), in order to fully characterize the association. To investigate the role of HIV status and number of recent sexual partners in our observed association between behavior class and STI, additional models were estimated adjusting for each of these factors individually.
Sensitivity Analysis
We treated UAI as a single behavior in our LCA model, without separating insertive and receptive roles, because we are not aware of evidence suggesting differential STI risk by sexual position. However, as a sensitivity analysis, we examined whether including insertive UAI and receptive UAI as two separate indicators in the latent class model would have impacted our findings.
RESULTS
We screened 1,866 men presenting to the sexual health clinic between July 2012 and October 2013 for study eligibility. Reasons for ineligibility included not reporting anal sex with men in the past year (99% of ineligible men, n=1568), age (n=13), and inability to speak English (n=10); 286 men were eligible. Of those, 51 (18%) opted out due to time constraints or lack of interest, and 235 enrolled.
Demographics & STI Prevalence
Participants (n=235) had a median age of 26 years (interquartile range=22–35). The majority was White non-Hispanic (57%) or Black non-Hispanic (23%); 7% and 13% identified as Hispanic or other racial/ethnic minority, respectively. Seventy-one percent had completed at least some college, and 73% were currently employed. Most self-identified as gay (76%) or bisexual (14%). Seventeen percent reported that they were HIV-positive (prior to any HIV testing performed that day). Across all anatomical sites (urethral, rectal, oral), 18% of men tested positive for gonorrhea, 19% for chlamydia, and 5% had primary or secondary syphilis. In total, 82 participants (35%) were classified as STI-positive for this analysis.
Sexual Behavior Prevalence
UAI was the most common recent behavior among participants, endorsed by 67% of men over the previous three months. Approximately one third of men reported use of enemas (30%), insertive sex toys (30%), or anonymous sex (31%) in the past three months. Recent group sex was reported by 25% of men and recent felching or snowballing was reported by 12%. Eight percent reported use of a sex sling, and 4% reported fisting (Table 1).
Table 1.
Overall Prevalence of Each Sexual Behavior and Item-Response Probabilities for Three-Class Model: Probability of Endorsing Item Given Latent Class
| Sexual Behavior | Overall Prevalencea | Class 1 (UAI-Only) | Class 2 (Partner-Seekers) | Class 3 (Multiple-behaviors) |
|---|---|---|---|---|
| Class Size | 67.40% | 13.90% | 18.70% | |
|
| ||||
| Unprotected Anal Intercourse (UAI) | 0.67 | 0.57 | 0.86 | 0.92 |
| Fisting | 0.04 | 0.01 | 0.03 | 0.18 |
| Enema Use | 0.30 | 0.21 | 0.14 | 0.74 |
| Felching/Snowballing | 0.12 | 0.04 | 0.18 | 0.37 |
| Use of Sex Sling | 0.08 | 0.01 | 0.08 | 0.30 |
| Use of Sex Toys | 0.34 | 0.19 | 0.19 | 1.00 |
| Anonymous Sex | 0.31 | 0.21 | 0.61 | 0.45 |
| Group Sex | 0.25 | 0.01 | 1.00 | 0.54 |
Note. Bold indicates an item-response probabilities of >0.30 to facilitate interpretation.
Overall prevalence reflects self-reported behavior within the past three months
Latent Class Analysis
We compared models with one through five latent classes to identify the optimal model based on fit criteria, interpretability, and class separation. According to information criteria, the two- or three-class model was optimal (Table 2). We selected the three-class model because of its clearer interpretability and high class separation. The bootstrap likelihood ratio test [18] also supported the three-class model as the optimal solution (Table 2).
Table 2.
Fit Statistics for Latent Class Models Reflecting Profiles of Sexual Behaviors Among MSM (N=235)
| Number of Classes | G2 | Degrees of Freedom (DF) | Akaike Information Criteria (AIC)a | Bayesian Information Criteria (BIC)a | Consistent Akaike Information Criteria (CAIC)a | Adjusted Bayesian Information Criteria (aBIC)a | % Seed | Bootstrap Likelihood Ratio Test |
|---|---|---|---|---|---|---|---|---|
| 1 | 248.4 | 247 | 264.4 | 292.0 | 300.0 | 266.7 | 100% | N/A |
| 2 | 133.5 | 238 | 167.5 | 226.2 | 243.2 | 172.3 | 99% | 0.01 |
| 3 | 105.9 | 229 | 157.9 | 247.7 | 273.7 | 165.3 | 60% | 0.03 |
| 4 | 90.6 | 220 | 160.6 | 281.5 | 316.5 | 170.6 | 2% | 0.38 |
| 5 | 75.9 | 211 | 163.9 | 315.9 | 359.9 | 176.4 | 2% | 0.34 |
Note. Bold indicates the selected model. % Seed indicates the percent of the 1000 randomly generated starting values sets that converged to the maximum likelihood solution.
Optimal models are indicated by minimum values of AIC, BIC, CAIC, & aBIC.
The item-response probabilities represent the conditional probability of reporting a recent behavior given membership in a latent class (Table 1). Probabilities close to 1 indicate that individuals in that class are likely to have engaged in the behavior. We relied on these probabilities to label the latent classes. Class 1, UAI-Only, contained men who likely engaged in UAI, but not in the other sexual behaviors, within the past three months. Men in Class 2, Partner-Seekers, differed from the UAI-Only class by their higher probability of endorsing recent anonymous sex and group sex along with UAI. In other words, these MSM sought out different types of sexual partners (in anonymous and group settings), but did not engage in a wide variety of behaviors. Class 3, Multiple-Behaviors, was clearly differentiated from both the other classes, with higher endorsement of every behavior. The most common latent class was UAI-Only (67%), followed by Multiple-Behaviors (19%), and Partner-Seekers (14%) (Table 1).
Characteristics of Sexual Behavior Classes
Class membership varied across several characteristics (Table 3). Education was significantly related to class membership (p=0.03), although membership in the UAI-only class was most common across all levels of education. Overall, age was not significantly associated with class membership (p=0.13). However, distribution of class membership differed significantly for the oldest men (>45 years) compared to the youngest (18–24 years). The oldest men were more likely than the youngest to be in the Multiple-Behaviors class (44% vs. 26%) and were also less likely to be in the UAI-only class (24% vs. 68%). Race/ethnicity overall was not significantly associated with class membership (p=0.12), although the pairwise comparison of White to Hispanic MSM approached statistical significance (p=0.08). Hispanics were very likely to be in the Partner-Seekers class (84%), while White MSM had a 42% probability of being in this class. Relationship status was not significantly associated with class membership (p=0.49), although notably 0% of men with a committed partner were in the Multiple-Behaviors class, while 43% of men with a committed partner were in the Partner-Seekers class. HIV status was significantly associated with class membership (p<0.01). Among the HIV-positive, 46% were in the Partner-Seekers class, 41% in the UAI-only class, and 13% in the Multiple-Behaviors class. Number of sexual partners in the last twelve months was also significantly associated with class membership (p<0.01). Among men who reported 1–3 partners in the last year, 88% were in the UAI-only class. Among men who reported 8 or more sexual partners, 22% were in the UAI-Only class, 28% were in the Partner-Seekers class, and 50% were in the Multiple-Behaviors class (Table 3).
Table 3.
Sexual Behavior Latent Class Membership as a Function of Key Characteristics
| Prevalence of Sexual Behavior Latent Class Membership Across Age, Race/Ethnicity, Education, Relationship Status, and HIV Status | Association between Characteristics of MSM and Latent Class Membership Relative to UAI-Only Class (Class 1) | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Characteristic | Class 1 (UAI-Only) | Class 2 (Partner-Seekers) | Class 3 (Multiple-Behaviors) | Class 2 (Partner-Seekers) | Class 3 (Multiple-Behaviors) | Overall Test of Significance p-value a | ||
|
| ||||||||
| (%) | (%) | (%) | Odds Ratio | 95% Confidence Interval | Odds Ratio | 95% Confidence Interval | ||
| Age | 0.13 | |||||||
| 18–24 | 68 | 6 | 26 | REF | – | REF | – | |
| 25–44 | 37 | 31 | 32 | 2.07 | (0.44, 9.75) | 2.00 | (0.75, 5.30) | |
| 45+ | 24 | 32 | 44 | 1.44 | (0.24,8.74) | 4.01 | (1.19, 13.44) | |
| Race/Ethnicity | 0.12 | |||||||
| White non-Hispanic | 24 | 42 | 34 | REF | – | REF | – | |
| Black non-Hispanic | 12 | 53 | 35 | 2.19 | (0.81, 5.96) | 0.53 | (0.17, 1.65) | |
| Hispanic | 8 | 84 | 7 | 0.65 | (0.06, 6.73) | 0.02 | (0.00, 47.24) | |
| Other | 14 | 39 | 47 | 2.48 | (0.73, 8.49) | 0.88 | (0.27, 2.87) | |
| Education | 0.03 | |||||||
| HS Diploma or less | 78 | 7 | 14 | REF | – | REF | – | |
| At least some college | 62 | 15 | 23 | 1.29 | (0.50, 3.32) | 3.92 | (1.05, 14.61) | |
| Relationship Status | 0.49 | |||||||
| Single | 32 | 60 | 8 | REF | – | REF | – | |
| Committed Partner | 57 | 43 | 0 | 1.56 | (0.64, 3.80) | 1.37 | (0.60,3.09) | |
| Known HIV Status | <0.01 | |||||||
| Not Positive | 73 | 13 | 14 | REF | – | REF | – | |
| Positive | 41 | 46 | 13 | 1.54 | (0.40, 5.94) | 6.56 | (2.30,18.68) | |
| Sexual Partners in Last Year | <0.01 | |||||||
| 1–3 | 88 | 2 | 10 | REF | – | REF | – | |
| 4–7 | 41 | 2 | 57 | 15.16 | (2.92, 78.61) | 2.21 | (0.12, 39.76) | |
| 8 or more | 22 | 28 | 50 | 24.38 | (3.88, 153.22) | 43.40 | (4.84, 389.12) | |
Based on test statistic for the overall association between characteristic and latent class membership (2*difference in log-likelihood of comparison models)
Association between Latent Class Membership and STI
Latent class membership was significantly associated with prevalent STI in this sample. The odds of being in the Multiple-Behaviors class (relative to the UAI-Only class) were 5.6 times higher for men with an STI compared to men without an STI (odds ratio (OR): 5.59, 95% confidence interval (CI): 2.32–13.51). The odds of being in the Multiple-Behaviors class (relative to the Partner-Seekers class) were 7.3 times higher among men with an STI (OR: 7.28, 95% CI: 1.57–33.85). The odds of being in the Partner-Seekers class relative to the UAI-Only class did not differ significantly between the STI-positive and STI-negative men (OR: 0.77, 95% CI: 0.21–2.82). Even after separately adjusting for known HIV status and number of partners in the last year (both as a continuous and binary variable), the associations between behavior latent class and STI remained significant. Further analysis using the LCA_distal macro revealed that MSM in the Multiple-Behaviors class had the highest probability of being STI-positive (67%), followed by men in the UAI-only class (27%) and men in the Partner-Seekers class (22%) (Figure 1).
Figure 1.
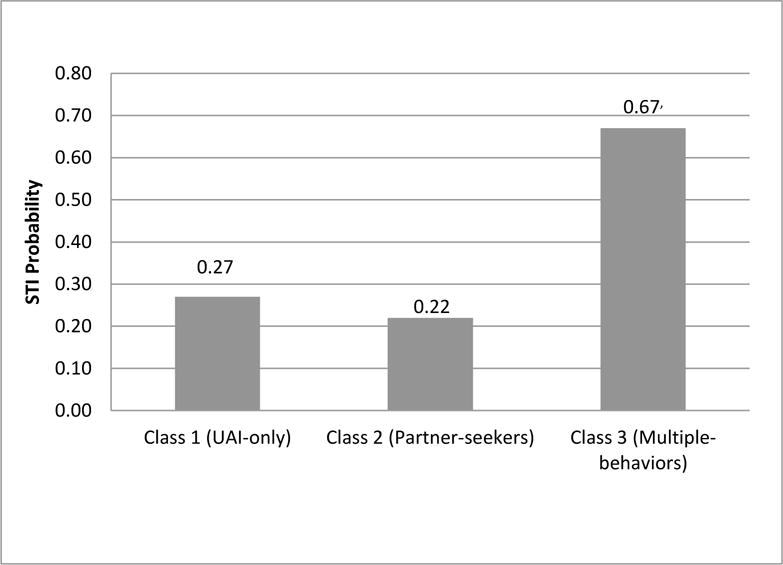
Estimated probability of STI prevalence, conditional on class membership.
Sensitivity Analysis
Including two indicators for UAI, insertive UAI and receptive UAI, did not meaningfully change our results. The Multiple-Behaviors class, which in the new analysis included men who were likely to endorse both insertive and receptive UAI, continued to be the class with highest prevalence of STI compared to the other classes.
DISCUSSION
This analysis identified three latent classes of sexual behavior among MSM presenting to an urban sexual health clinic. The UAI-Only class was characterized by endorsement of recent UAI, but little to no endorsement of other sexual behaviors. The Partner-Seekers class was characterized by high endorsement of UAI, group sex, and anonymous sex, but lower endorsement of other sexual behaviors. Alternatively, the Multiple-Behaviors class was characterized by higher probabilities of every behavior except group sex and anonymous sex, compared to the other two latent classes. MSM with an STI were significantly more likely to be in the Multiple-Behaviors class than the Partner-seekers class or the UAI-Only class. The Multiple-Behaviors class had the highest probability of STI infection.
Unexpectedly, the UAI-Only class and Partner-Seekers class did not significantly differ with respect to STI prevalence. Group sex and anonymous sex have been associated with STI (Rice et al, 2015; Kim, Kent, & Klausner, 2003), yet the Partner-Seekers class, which was identified by extremely high endorsement of these behaviors, was not associated with increased odds of STI in this analysis. It is possible that this was because men may practice safe sex with outside partners, but not with primary partners (Jacobs & Ownby, 2012), thus limiting the additional risk that could be attributed to group and anonymous sex.
We identified several sub-populations of interest in our analysis of demographic patterns within latent classes. MSM older than 44 years of age were significantly more likely to be in the Multiple-Behaviors class, the class with the highest odds of STI. Meanwhile, men aged 18–24 were most likely to be in the UAI-only class. Sex practices other than anal intercourse may appeal to older MSM if they have challenges finding sexual partners or erection difficulties (Jacobs, Kane, & Ownby, 2013). While the CDC has identified young MSM as the population at highest risk for HIV acquisition (CDC, 2012), our findings demonstrate that older MSM are have substantial STI prevalence, which supports previous findings Jacobs et al, 2013; Heath, Lanoye, & Maisto, 2012). While class membership did not differ significantly by race/ethnicity, we observed some suggestive trends. For example, eighty-four percent of Hispanic MSM were in the Partner-Seekers class, with probabilities under 10% of being in either other class. Given the small number of Hispanic men in this sample (n=16), the p-value of 0.08 is notable. Further research is needed to understand how sexual behavior choices may be influenced by race/ethnicity. Given the current reliance on UAI as a marker of risk (Frye et al, 2015) and as a single indicator for determining whether intervention occurs (CDC, 2014; CDC, 2015b), it is important to note that UAI is highly prevalent. A surveillance study concluded that 54% of MSM report UAI in the past year (Finlayson et al, 2011). In our analysis, MSM in all classes were characterized by high probabilities of recent UAI, ranging from 57% in the UAI-only class to 92% in the Multiple-Behaviors class. Yet, the Multiple-Behaviors class had nearly 6 times the odds of STI, compared to the UAI-Only class. These findings contribute to the CDC’s recent call for research that contributes to improved, culturally relevant care for MSM (CDC, 2015).
HIV status was significantly associated with latent class membership, as odds of being in the Multiple-Behaviors class, relative to either of the other classes, was significantly higher among HIV-positive men. If HIV status is a significant predictor of specific sexual behaviors, serosorting could be occurring. Unfortunately, more direct examination of the role of HIV status in this analysis, perhaps as an effect modifier between latent classes and STI status, was not possible in our sample due to sample size restrictions. Further, because we did not assess information about partners for each behavior, we were unable to definitively examine whether serosorting, strategic positioning, or other biobehavioral factors may play a role in the observed association.
Our study was cross-sectional; therefore we cannot make temporal statements about the association between these behavior profiles and STI. In addition, our analysis relies on self-reported behaviors, which are prone to social desirability and recall biases (Gallo et al, 2013). However, we collected the most sensitive behavioral data through self-administered surveys, which minimize those biases (Macalino, Celentano, Latkin, Strathdee, & Vlahov, 2002; Kim, Dubowitz, Hudson-Martin, & Lane, 2008; NIMH, 2008). Finally, our sample comprised men who reported anal sex with a man in the last year and presented to a sexual health clinic for STD testing. These two factors likely limit the generalizability of this analysis. Specifically, our sample may have higher STI prevalence than the larger MSM community. Further, our eligibility criteria may have led to the exclusion of some men who engage in other sexual behaviors with men or who are attracted to men. Despite these limitations, this sample represents an understudied population, as much of the current research on sexual behaviors among MSM has been conducted in venues associated with high risk, including sex resorts (Crosby & Mettey, 2004) and internet chat rooms (Klein, 2012).
This work provides a valuable contribution to literature about sexual health among MSM as patterns of behavior likely represent a more realistic and comprehensive assessment than in depth assessments of any single behavior. However, our resulting profiles lack information about the frequency and timing of the behaviors, the context of the behaviors, or how they might be combined within a single sexual experience. We hypothesize that the higher STI prevalence in the Multiple-Behaviors class was a result of compounded risk associated with engagement in multiple behaviors. For example, both UAI (Powers, Poole, Pettifor, & Cohen, 2008) and enema use (Noor & Rosser, 2014) have been linked with risk of STI/HIV acquisition; participating in both likely results in higher STI risk than in either on its own. While the latent class model categorizes men based on recent sexual behaviors, other differences exist between classes. We were able to assess some of these differences, including HIV-status, number of sexual partners in the last year, and relationship status. However, it is likely that other unmeasured differences that may provide important context for understanding the differential rate of STI observed across classes. In addition, many of the behaviors included in this analysis may have variable risk associated with them, depending on whether the man is the active or passive partner (e.g. fisting), or whether the behavior was done before or after AI (e.g. enema use). Further, some research suggests that partner status (e.g. primary or outside partner) may be an important predictor of behavior, including UAI (Jin et al, 2009; Hoff et al, 2012). To explore these hypotheses fully, capturing specific event-level sexual behavior data is needed.
Our findings might be used to inform new prevention messages and initiatives for the most at-risk MSM. Historically, STI/HIV prevention programs have relied heavily on the promotion of “safe sex” (e.g., avoid UAI), but evidence of “prevention fatigue” among MSM (Flowers, Knussen, & Duncan, 2001; Halkitis, Parsons, & Wilton, 2003; Wolitski, 2005) reveals the limitations of this approach. New prevention messages that target previously underdocumented behaviors and behavior combinations may not face the same fatigue among MSM. In addition, given the strong association between the Multiple-behaviors class and STI, ensuring that condoms are available in venues where diverse sexual behaviors occur may also lead to meaningful public health benefit.
This analysis provides further evidence of the utility of LCA to describe patterns of sexual behavior. Our final model was identified, in part, because of excellent class separation, and was effective at identifying patterns of behavior associated with prevalent STI. This analysis should be replicated in other samples to look for similar patterns. Including additional factors in future analyses may also be informative.
References
- The Foundation for AIDS Research (amfAR) Global Consultation on MSM and HIV/AIDS Research: The MSM Initiative. Washington D.C.: Sep 28–29, 2008. 2008. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Prevalence and awareness of HIV infection among men who have sex with men: 21 cities, United States, 2008. Morbidity and Mortality Weekly Report (MMWR) 2010;59(37):1202–1209. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) HIV surveillance in men who have sex with men (MSM) U.S. Department of Health and Human Services; 2012. Retrieved from www.cdc.gov/hiv/library/slideSets/index.html. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Preexposure prophylaxis for the prevention of HIV infection in the United States – 2014: A Clinical Practice Guideline. U.S. Department of Health and Human Services; 2014. Retrieved from http://www.cdc.gov/hiv/pdf/prepguidelines2014.pdf. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Atlanta: U.S. Department of Health and Human Services; 2015. Sexually Transmitted Disease Surveillance 2014. Retrieved from http://www.cdc.gov/std/stats14/surv-2014-print.pdf. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) 2015 Sexually Transmitted Diseases Treatment Guidelines. U.S. Department of Health and Human Services; 2015b. Retrieved from http://www.cdc.gov/std/tg2015/specialpops.htm. [Google Scholar]
- Cohen CE, Giles A, Nelson M. Sexual trauma associated with fisting and recreational drugs. Sexually Transmitted Infections. 2004;80:469–470. doi: 10.1136/sti.2004.011171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins LM, Lanza ST. Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. New York: Wiley; 2010. [Google Scholar]
- Crosby R, Mettey A. A descriptive analysis of HIV risk behavior among men having sex with men attending a large sex resort. Journal of Acquired Immune Deficiency Syndrome. 2004;37(4):1496–1499. doi: 10.1097/01.qai.0000127065.61454.b4. [DOI] [PubMed] [Google Scholar]
- Dziak JJ, Lanza ST, Xu S. LCABootstrap SAS macro users’ guide (version 1.1.0) University Park: The Methodology Center, Penn State; 2011. Retrieved from http://methodology.psu.edu. [Google Scholar]
- Finlayson TJ, Le B, Smith A, Bowles K, et al. HIV risk, prevention, and testing behaviors among men who have sex with men –National HIV Behavioral Surveillance System, 21 US Cities, United States, 2008. MMWR Surveillance Summaries. 2011;60(14):1–34. [PubMed] [Google Scholar]
- Flowers P, Knussen C, Duncan B. Re-appraising HIV testing among Scottish gay men: The impact of new HIV treatments. Journal of Health Psychology. 2001;6(6):665–678. doi: 10.1177/135910530100600605. [DOI] [PubMed] [Google Scholar]
- Frye V, Nandi V, Egan J, Cerda M, Greene E, Tieu HV, Ompad DC, Hoover DR, Lucy D, Baez E, Koblin BA. Sexual orientation- and race-based discrimination and sexual HIV risk behavior among urban MSM. AIDS and Behavior. 2015;19:257–269. doi: 10.1007/s10461-014-0937-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo MF, Steiner MF, Hobbs MM, Warner L, Jamieson DJ, Macaluso M. Biological markers of sexual activity: tools for improving measurement in HIV/STI prevention research. Sexually Transmitted Diseases. 2013;40:447–452. doi: 10.1097/OLQ.0b013e31828b2f77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galvin SR, Cohen MS. The role of sexually transmitted diseases in HIV transmission. Nature Reviews Microbiology. 2004;2:33–42. doi: 10.1038/nrmicro794. [DOI] [PubMed] [Google Scholar]
- Halkitis PN, Parsons JT, Wilton L. Barebacking among gay and bisexual men in New York City: Explanations for the emergence of intentional unsafe behavior. Archives of Sexual Behavior. 2003;32(4):351–357. doi: 10.1023/a:1024095016181. [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap) – A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath J, Lanoye A, Maisto SA. The role of alcohol and substance use in risky sexual behavior among older men who have sex with men: A review and critique of the current literature. AIDS and Behavior. 2012;16(3):578–589. doi: 10.1007/s10461-011-9921-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoff CC, Chakravarty MA, Beogher SC, Neilands TB, Darbes LA. Relationship characteristics associated with sexual risk behavior among MSM in committed relationships. AIDS Patient Care STDS. 2012;26(12):738–745. doi: 10.1089/apc.2012.0198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobs RJ, Ownby RL. Sexual communication and seroadaptation practices among HIV-negative MSM aged 40 and older in South Florida, United States. Journal of Sexual Medicine. 2012;8:133. [Google Scholar]
- Jacobs RJ, Kane MN, Ownby RL. Condom use, disclosure, and Risk for unprotected sex in HIV-negative midlife and older men who have sex with men. American Journal of Men’s Health. 2013;7(3):186–97. doi: 10.1177/1557988312463417. [DOI] [PubMed] [Google Scholar]
- Jin F, Prestage GP, Mao L, Kippax SC, Pell CM, Donovan B, Cunningham PH, Templeton DJ, Kaldor JM, Grulich AE. Incidence and risk factors for urethral and anal gonorrhea and chlamydia in a cohort of HIV-negative homosexual men: the Health in Men Study. Sexually Transmitted Infections. 2007;83:113–119. doi: 10.1136/sti.2006.021915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin F, Crawford J, Prestage GP, Zablotska I, Imrie J, Kippax SC, Kaldor JM, Grulich AE. Unprotected anal intercourse, risk reduction behaviours, and subsequent HIV infection in a cohort of homosexual men. AIDS. 2009;23(2):243–52. doi: 10.1097/QAD.0b013e32831fb51a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim AA, Kent CK, Klausner JD. Risk factors for rectal gonococcal infection amidst resurgence in HIV transmission. Sexually Transmitted Diseases. 2003;30:813–7. doi: 10.1097/01.OLQ.0000086603.55760.54. [DOI] [PubMed] [Google Scholar]
- Kim J, Dubowitz H, Hudson-Martin E, Lane W. Comparison of 3 data collection methods for gathering sensitive and less sensitive information. Ambulatory Pediatrics. 2008;8:255–260. doi: 10.1016/j.ambp.2008.03.033. [DOI] [PubMed] [Google Scholar]
- Klein H. Felching among men who engage in barebacking (unprotected anal sex) Archives of Sexual Behavior. 2012;41:377–384. doi: 10.1007/s10508-011-9770-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, Collins LM, Lemmon DR, Schafer JL. PROC LCA: A SAS procedure for latent class analysis. Structural Equation Modeling. 2007;14:671–694. doi: 10.1080/10705510701575602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, Tan X, Bray BC. Latent class analysis with distal outcomes: A flexible model-based approach. Structural Equation Modeling: A Multidisciplinary Journal. 2013;20:1–26. doi: 10.1080/10705511.2013.742377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macalino GE, Celentano DD, Latkin C, Strathdee SA, Vlahov D. Risk behaviors by audio computer-assisted self-interviews among HIV-seropositive and HIV-seronegative injection drug users. AIDS Education and Prevention. 2002;14:367–378. doi: 10.1521/aeap.14.6.367.24075. [DOI] [PubMed] [Google Scholar]
- Moskowitz DA, Seal DW, Rintamaki L, Reiger G. HIV in the leather community: rates and risk-related behaviors. AIDS Behavior. 2011;15:557–564. doi: 10.1007/s10461-009-9636-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIMH Multisite HIV/STD Prevention Trial for African American Couples Group. Designing an audio computer-assisted self-interview (ACASI) system in a multi-site trial: A brief report. Journal of Acquired Immune Deficiency Syndromes. 2008;49:S52–S58. doi: 10.1097/QAI.0b013e318184481a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noor SW, Rosser S. Enema use among men who have sex with men: A behavioral epidemiologic study with implications for HIV/STI prevention. Archives of Sexual Behavior. 2014;43(4):755–769. doi: 10.1007/s10508-013-0203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips G, Magnus M, Kuo I, Rawls A, Peterson J, West-Ojo T, Jia Y, Opoku J, Greenberg AE. Correlates of group sex among a community-based sample of men who have sex with men (MSM) in Washington, DC. AIDS and Behavior. 2014;18:1413–1419. doi: 10.1007/s10461-013-0527-8. [DOI] [PubMed] [Google Scholar]
- Powers KA, Poole C, Pettifor AE, Cohen MS. Rethinking the heterosexual infectivity of HIV-1: a systematic review and meta-analysis. Lancet Infect Dis. 2008;8:553–563. doi: 10.1016/S1473-3099(08)70156-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice CE, Lynch CD, Norris AH, Davis JA, Fields KS, Ervin M, Turner AN. Group sex and prevalent sexually transmitted infections among men who have sex with men. Arch Sex Behav. 2015 doi: 10.1007/s10508-015-0554-9. [DOI] [PubMed] [Google Scholar]
- Rice CE, Maierhofer C, Fields KS, Ervin M, Lanza ST, Turner AN. Beyond anal sex: Sexual practices among MSM and associations with HIV and other sexually transmitted infections. Journal of Sexual Medicine. 2016;13(3):374–382. doi: 10.1016/j.jsxm.2016.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan PS, Rosenberg ES. Breaking bias: Improved methods for analyzing HIV/AIDS data. Epidemiology. 2015;26:625–627. doi: 10.1097/EDE.0000000000000356. [DOI] [PubMed] [Google Scholar]
- Wolitski RJ. The emergence of barebacking among gay and bisexual men in the United States: A public health perspective. Journal Of Gay & Lesbian Psychotherapy. 2005;9:9–34. [Google Scholar]


