Abstract
Calgary Laboratory Services provides global hospital and community laboratory services for Calgary and surrounding areas (population 1.4 million) and global academic support for the University of Calgary Cumming School of Medicine. It developed rapidly after the Alberta Provincial Government implemented an austerity program to address rising health care costs and to address Alberta’s debt and deficit in 1994. Over roughly the next year, all hospital and community laboratory test funding within the province was put into a single budget, fee codes for fee-for-service test billing were closed, roughly 40% of the provincial laboratory budget was cut, and roughly 40% of the pathologists left the province of Alberta. In Calgary, in the face of these abrupt changes in the laboratory environment, private laboratories, publicly funded hospital laboratories and the medical school department precipitously and reluctantly merged in 1996. The origin of Calgary Laboratory Services was likened to an “unhappy shotgun marriage” by all parties. Although such a structure could save money by eliminating duplicated services and excess capacity and could provide excellent city-wide clinical service by increasing standardization, it was less clear whether it could provide strong academic support for a medical school. Over the past decade, iterations of the Calgary Laboratory Services model have been implemented or are being considered in other Canadian jurisdictions. This case study analyzes the evolution of Calgary Laboratory Services, provides a metric-based review of academic performance over time, and demonstrates that this model, essentially arising as an unplanned experiment, has merit within a Canadian health care context.
Keywords: academic laboratory services, Alberta, Calgary, Canada, pathology and laboratory medicine
This is a case study of an academic department of pathology and laboratory medicine (DPLM) developing from an abrupt merger of public, private, and academic pathology laboratories in Calgary, Alberta, Canada. In order to situate the case, it is important to understand the Canadian Health Care System, the province of Alberta, the University of Calgary Faculty of Medicine, and the dynamics of the provincial health system.
Canadian Health Care System
In Canada, provinces have jurisdiction over health care for their citizens. The federal government is a major source of funding for the provincial health systems. This funding is provided under the auspices of the Canada Health Act that stipulates 5 principles for the receipt of these funds. These principles are public administration, comprehensiveness, universality, portability, and accessibility (http://www.canadian-healthcare.org/page2.html). Although provinces must meet the requirements of the Canada Health Act to receive federal funding, provincial governments are free to design and run health services as they see fit. Therefore, this first principle, public administration, allows day-to-day partisan provincial politics to interject into decision making and sometimes to even abruptly alter the long-term course of the provincial health care system. In Canadian health care systems, the payer for laboratory services, both hospital based and community based, is generally the provincial government.
Province of Alberta
Alberta, geographically the fourth largest province in Canada, is located in Western Canada at the interface of the prairies and the rocky mountains; it is a wilderness destination with many nearby national parks. Alberta has a population of roughly 4 million people, with approximately 81% living in urban areas (https://en.wikipedia.org/wiki/Alberta). There are 2 large cities with populations exceeding 1 million: Edmonton, which is the capital, and Calgary, the most populous city; they are approximately 180 miles apart, and the province’s third largest city is roughly halfway in between. Traditionally, the population of Alberta tends to be conservative, and until May 2015, the same political party (Progressive Conservatives) had been in power for 44 years in succession. Alberta has an energy-based economy, and the province’s fortunes are cyclical based on commodity prices. During one of the “boom” periods, the province took energy revenue surpluses and created the Alberta Heritage Foundation for Medical Research (AHFMR), established in 1980, to support health research within the province. Alberta has 2 medical schools, the University of Alberta (UofA) and the University of Calgary (UofC). For several decades, the research enterprises of both medical schools grew rapidly with AHFMR soft funding for salary support for research-intensive faculty members. However, in 2010, the provincial government abruptly decided to restructure AHFMR and discontinue these award competitions (http://eae.alberta.ca/research/system/alberta-innovates/history/questions.aspx), and it was announced that current AHFMR salary awards were to be phased out over a 7-year period, thus creating budget crises at both medical schools.
University of Calgary Medical School and the Department of Pathology and Laboratory Medicine at Its Inception
The UofC Faculty of Medicine opened in 1970. It was designed to produce family doctors and was expected to be less academic than the longer standing medical school at UofA. The medical school campus was built adjacent to the new Foothills Hospital, which opened in 1966, on the outskirts of the city and became its primary teaching hospital.
As might be predicted when creating a new medical school from scratch, the new DPLM lacked an academic orientation, and the local pathologists did not buy into the new expectation of “academic culture.” In the early years of the medical school, pathology services were repeatedly identified in medical school accreditation reports as problematic. For instance, the 1985 Committee on the Accreditation of Canadian Medical Schools (CACMS) and the Liaison Committee on Medical Education (LCME) Accreditation Survey identified Pathology as 1 of the 5 major weaknesses in the medical school: “Although improvement has occurred since 1980, the centrality of Pathology in any medical school is such that this department’s progress toward academic strength can only be described as disappointing. The lack of significant progress, as compared to other disciplines, may be due to a combination of factors such as inadequate university support, inflexible hospital budget restrictions, previous faculty recruitment, practices, or departmental attitudes. This department should do better than heretofore, and the survey team suggests that consideration be given to a university hospital reevaluation of its academic future.” Having been identified as 1 of the 5 major weaknesses and a problem that had to be resolved for the next accreditation, considerable effort was directed at addressing this problem by the new incoming department head, and the next CACMS/LCME accreditation team was, in fact, complimentary of recent changes. The 1993 CACMS/LCME Accreditation Survey Report indicated that “there had been seven new pathologists recruited, three of whom won support as Heritage Scholars, with the result that the academic strength of the department had improved dramatically …” and that “the current survey team did not detect continuing problems …”. However, the nascent achievement of an “academic culture” in pathology at Foothills Hospital in the early 1990s was to be short lived, as it immediately predated the austerity programs associated with regionalization and the formation of Calgary Laboratory Services (CLS; see subsequently).
Although the UofC medical school was not begun with the intent that it would be research intensive, it quickly evolved in that direction, in large part because of the availability of AHFMR salary support. However, it should be noted that other than the 3 AHFMR scholars recruited to the DPLM at Foothills Hospital in the mid-late 1980s, the Faculty’s AHFMR salary awards for the next 2 decades went to other UofC departments, and the DPLM did not directly benefit from this program again until its last 2 competitions in 2009 and 2010, where 2 new DPLM recruits were awarded 7-year long salary awards. In retrospect, AHFMR salary awards primarily made the strong academic departments stronger as these departments generally have larger numbers of geographic full-time (GFT) faculty positions, which are fully or partially funded by UofC and often have 50% to 75% academic protected time, while most of the weaker departments were comprised primarily of clinical faculty members funded by the health care system and lacking academic protected time. Ironically, as the AHFMR salary award programs were being phased out, there was a need to use the University’s contributions to the salaries of retiring GFT faculty members in DPLM and other weaker departments to cover the GFT salaries of >60 research-intensive faculty members who would be losing their AHFMR funding. Faculty records show that DPLM lost university funding for more GFT faculty member positions over the last 6 years than any other clinical department, as these dollars were clawed back to support retention of basic or clinical scientists in departments that had been historically more research intensive than DPLM.
Currently, among Canadian medical schools, UofC is roughly now between the 65th and 70th percentile in research output and improving. In 2014, the UofC Faculty of Medicine was renamed the Cumming School of Medicine (CSM) after a local businessman Geoffrey Cumming donated C$100 million to support neuroscience and inflammation research, and this was matched dollar-for-dollar by the province.
Case Scenario—Health Care Institutional Restructuring in Alberta and the Formation of Calgary Laboratory Services
In 1993, a new premier (roughly equivalent to a state governor in the United States) was elected in the province of Alberta on a platform of balancing the budget and paying off all debt (C$23 billion; https://en.wikipedia.org/wiki/Ralph_Klein). Since health care was the province’s largest expense, it was targeted along with other portfolios. In 1994, the provincial health care budget was cut by 18% (to be spread out over 4 years), and the Alberta Medical Association, essentially the physician’s union, accepted an overall 6% cut in physicians billings which included a “47% reduction in laboratory physician fees compared to a 4% reduction for the other physicians.”1(p74) A process of health care institutional “regionalization” modeled after the system in New Zealand was implemented. Almost immediately, 250 hospital/public health boards were disbanded and 17 regional health authorities were created; one of these was the Calgary Regional Health Authority (CRHA; see subsequently). These changes were implemented to decrease the cost of administrative oversight (nb: a few years later, the number of authorities was decreased from 17 to 9 in an attempt to cut additional administrative costs). These extreme austerity measures, although unpopular within the health care system, resonated sufficiently with taxpayers that the premier was reelected 3 more times in 1997, 2001, and 2004. Health care cuts, cuts in other portfolios, and increased revenues from a boom in the oil and gas industries resulted in surpluses, and eventually, the goal of zero provincial debt was reached in 2005; however, this was short-lived as revenues from the oil and gas industries soon plummeted, and the province, which prides itself for having the lowest taxes in Canada, chose not to raise taxes. In 2008, a new Premier merged the remaining 9 health authorities into a single province-wide entity with almost 100 000 employees called Alberta Health Services (AHS). The AHS immediately became the largest health authority in Canada, the largest single employer in Alberta, and the fifth largest single employer in Canada (https://en.wikipedia.org/wiki/Alberta_Health_Services). The AHS was divided into 5 zones; one of these was the AHS Calgary Zone. The geographic footprints of the CRHA and the AHS Calgary Zone were the same, and so this latter change, while disruptive on the clinical service side, is not an important variable in the analysis of the academic model described subsequently.
As part of the original regionalization process in 1994, the city of Calgary’s 7 hospital boards and executives were disbanded, and 1 board and a single executive leadership group for the CRHA were created. As a cost-containment measure, 3 of the 7 of the city’s hospitals (ie, the older ones) were closed. Initially, laboratory services in Calgary were comprised of 7 hospital laboratories providing in-house services, and 4 private commercial laboratories focused primarily on community testing; these private laboratories provided 110 collection sites across the city. In 1994, laboratory services came squarely into the province-wide, budget-cutting crosshairs. Over roughly the next year, all hospital and community laboratory test funding within the province was put into a single budget, fee codes for fee-for-service test billing were closed, roughly 40% of the provincial laboratory budget was cut, and roughly 40% of the pathologists left the province of Alberta. In Calgary, 4 private commercial laboratory entities merged, creating 2 distinct private laboratories, which fiercely competed for survival. The provincial government indicated that this was the new reality and asked laboratory physicians to suggest possible solutions. This case study will focus on what transpired next in Calgary and how this affected the academic mandate for the associated medical school; it should be noted that the scenario in Edmonton was very different.1
Formation of Calgary Laboratory Services
Calgary Laboratory Services began as an “unhappy shotgun marriage” of private commercial laboratories and the pathology departments of community hospitals, the Foothills Hospital, and the medical school (minus the basic scientists) in 1996. Immediately prior to the formation of CLS, the laboratory environment had sustained significant changes including the closure of hospitals (and their associated clinical laboratories), 40% laboratory-specific budget cuts, exodus of many of the city’s pathologists, and extensive private laboratory restructuring. Specifically, in roughly 1 year, Calgary Diagnostic Laboratories and Associated Clinical Laboratories merged to become Kasper Medical Laboratories which then merged with Calgary Medical Laboratories to become MDS-Kasper Laboratories which then merged with the 4 remaining hospital laboratories that had just been merged together into CRHA. The new CLS laboratory was overseen by a management committee with membership from major stakeholders. The CLS began as a public–private partnership with the private laboratory (MDS-Kasper) owning 50.1%. Ironically, the minor partner (CRHR), owning 49.9%, was the primary customer of the new laboratory (nb: 10 years later, the CRHA bought out the private holdings and CLS became a wholly owned subsidiary of the CRHA). It is worthy of noting that the restructuring was driven by the health care system, and academics was not necessarily considered in decision making. Furthermore, there was no specific transition funding for a common information technology system or transition to a standardized testing platform.
In this stressful environment in which there had historically been a weak academic culture, community hospital pathologists, without much consultation, were now expected to participate in a more academic form of practice. Predictably, this escalated existing “town and gown”-based antagonism between academic and community pathologists that persists today among a few of the less than a dozen remaining pathologists who transferred to CLS at the time of its formation.
When merging independent health care providers into a single provider, savings are expected through economies of scale. The primary reason for the creation of CLS was to save money for the health care system. Laboratory services are both “low profile” and expensive. Concerns regarding replication of services and over/inappropriate test utilization have resulted in laboratories being attractive venues to seek savings. On the other hand, >70% of important medical decision making depends upon laboratory data,2 and there is little public tolerance of “laboratory error” precipitated by government underresourcing. Clearly, the expectation was that CLS would save money for the health care system by eliminating duplicated services and excess capacity (eg, 110 community collection sites quickly became 25 and later 18 collection sites) while providing excellent city-wide clinical service by increasing standardization. Importantly, a single patient-centric longitudinal record of laboratory results was expected to offer further savings, as there would be less tendency to duplicate testing as patients traversed the health care system. However, it is not clear how a system rapidly designed around cost savings could provide strong and robust academic support for a medical school. It is a tribute to those involved in the merger that the outcome is a happy one. However, as will be clear from the data presented subsequently, it took some time to recover from the disruption caused by the creation of CLS.
Methods
This case study is produced using multiple sources of data available to the author. Before considering writing it, I analyzed my qualifications and my biases. What are my “qualifications” to do this analysis? First of all, I am a detail-oriented and analytical academic pathologist with a Masters of Arts in Medical History who has been publishing on the history of North American pathology for 30 years.3-6 Second, I am 1 of 4 coauthors of the official history of the UofC’s CSM book to be released for its 50th anniversary and thus have easy access to local archival materials. Third, having just completed two 5-year terms (2005-2015) as joint Clinical (CRHA/AHS) and Academic (UofC) Department Head in Calgary (ie, half of the existence of CLS), I know the DPLM/CLS well. Fourth, I have a good relationship with key people involved in the initial formation of CLS and have been probing them for information over the past decade. Finally, as a senior Canadian medical school department head regularly asked to review other Canadian pathology departments when their department heads are being considered after 5 years for reappointment, I have had ample opportunity to hone my assessment skills and gain insights into other academic pathology departments across Canada. In all of these contexts, I have thought about CLS from a number of different perspectives, and it is clear to me that the CLS model has, through serendipity, been a unique experiment in the history of North American academic pathology. And, although I liken CLS to an “experiment,” I must admit it was not always a carefully designed experiment as many of the variables were not (or, perhaps more correctly for political reasons, could not be) carefully controlled. On the other hand, as former UofC and CRHA/AHS Calgary Zone Head of the DPLM and as a former member of the CLS Executive, I recognize that I have inherent biases; however, these biases are lessened by the fact that CLS was created before I began my term and its structure was mostly determined by others. Regardless, to minimize any effect of bias, after providing the necessary historical context, my analysis of the academic model will be metric based. In weighing whether or not to write this article, I eventually decided in favor as I believe that the model works very well in a Canadian context, and it has now become a prototype that is being partially replicated at several other Canadian medical schools. Therefore, such an analysis would be a useful addition to the academic pathology literature.
Academic Performance at University of Calgary Department of Pathology and Laboratory Medicine and Calgary Laboratory Services
This case study will now focus on the academic performance of CLS and the DPLM at UofC. My hope is to demonstrate that the CLS model is capable of providing strong support for the academic mandates of teaching and research. It is given that CLS provides high-quality laboratory services for the people of Calgary and its surrounding zone. Although the quality of service was generally good from its inception, CLS has continuously improved through hiring exceptional laboratory physicians and scientists. The only services that required major restructuring were neuropathology and autopsy7; laboratory informatics, however, needed to be created from scratch.
Teaching at Calgary Laboratory Services
Calgary Laboratory Services is a clinical service powerhouse providing more than 25 million laboratory tests per year, including signing out more than 130 000 surgical, 220 000 cytology, 200 adult autopsy, and 300 pediatric/fetal autopsy cases. With these volumes and a current medical scientific staff of roughly 100 covering almost every subspecialty focus, CLS is well endowed to teach pathology and laboratory medicine, and hence that is our major academic focus. As documented subsequently, the educational mandate has fared exceedingly well under CLS.
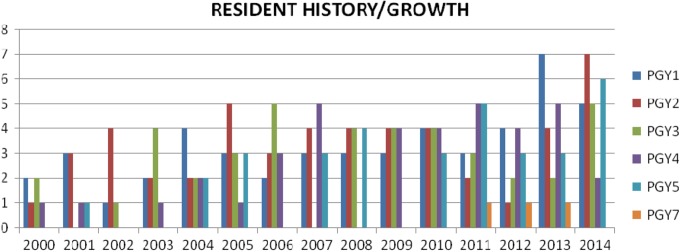
When CLS formed, there were 2 Royal College of Physicians & Surgeons of Canada (RCPSC) accredited residency training programs (anatomic pathology and neuropathology) but few residents. Now, CLS offers accredited residency training programs in anatomic pathology, neuropathology, general (anatomic/clinical) pathology, and as of July 2016, medical microbiology; most positions are filled. Figure 1 shows the upward trend in total numbers of DPLM residents over the past 15 years. Although not demonstrated by a quantitative metric, the quality of residents accepted into the program has improved considerably over time—as documented by, in most years, the ability to fill most or all DPLM postgraduate year 1 positions with highly ranked applicants in the first round of the match. Furthermore, the quality of resident teaching improved. In the past 5 years, 2 different DPLM clinical faculty members have been selected as the faculty of medicine’s postgraduate medical education teacher of the year and 2 of our GFT faculty members have been selected as the recipient of the Faculty’s Smith (only open to full professors) or Watanabe (only open to assistant/associate professors) awards. These latter awards, both named after the former deans, are for all-around (both teaching and research) achievement and are among the most prestigious awards in the CSM. These teaching accomplishments are notable as no DPLM faculty member had ever previously received a faculty-wide award of any kind (ie, a single faculty member is selected from one of 20 departments in the faculty). Finally, DPLM graduates are well trained; no graduate of any of the residency programs has failed to pass their Royal College specialty board examinations in at least a decade, and the first attempt pass rate exceeds 95%.
Figure 1.
Numbers of Department of Pathology and Laboratory Medicine residents from 2000 to 2014 and their postgraduate year levels.
Related to undergraduate medical teaching, there have been no obvious changes in quantity of teaching, as the DPLM has always provided all of the medical student teaching it was asked to provide. However, in the past year, 1 clinical faculty member was selected by the medical students as its teacher of the year (2015 Student Union Teaching Excellence Award). This is the first university-wide award ever received by a pathologist.
At the founding of CLS, there were no hard-funded postgraduate fellowship training program positions. The CLS now internally funds 8 postgraduate fellowship training program positions per year, and the DPLM/CLS offers subspecialty training in 13 different disciplines—nine 1-year anatomic pathology fellowships (breast, cytopathological, dermatological, gastrointestinal, gynecological, pediatric–perinatal, pulmonary, renal, and genitourinary pathology), a 1-year hematopathology fellowship, and 3 accredited 2-year CP fellowships, which are open to MDs or PhDs (clinical biochemistry, cytogenetics, and histocompatibility). The CLS Clinical Biochemistry Fellowship, which started in 2013, was the first new accredited chemistry training program in Canada in the past 30 years. Graduates are currently able to write the Canadian Academy of Clinical Biochemistry board examination. The program is in the process of applying for Commission on Accreditation in Clinical Chemistry accreditation so that graduates can write both the Canadian and the American board examinations and become board certified in both countries. The CLS histocompatibility training program, which started in 2008, is accredited by American Society of Histocompatibility and Immunogenetics to train HLA laboratory directors and is one of only 7 programs worldwide and the only program in Canada. Graduates are eligible to write the American Board of Histocompatibility and Immunogenetics certification examination. Finally, CLS offers a cytogenetics fellowship in collaboration with the Alberta Children’s Hospital; graduates are able to write the Canadian College of Medical Genetics board examination. Unlike the United States, where fellowships in some AP subspecialty disciplines can be accredited allowing graduates to take subspecialty examinations from the American Board of Pathology, subspecialty fellowships for physicians in Canada traditionally have not been recognized by the Royal College, and so Canadians have often chosen to pursue their subspecialty fellowships in the United States. To both standardize and improve the quality of fellowship training and to help retain Canadian trainees, the Royal College has very recently developed Areas of Focused Competence (Diploma) Programs in a small number of medical and surgical subspecialties (http://www.royalcollege.ca/portal/page/portal/rc/credentials/discipline_recognition/afc_program). Obtaining a diploma program is a 2-step process that takes several years of paperwork; first, a subspecialty must be approved nationally by the Royal College, and then individual programs wanting to offer training in that subspecialty must be approved. At the time this case study was written, the only Royal College Diploma program in the medical school was the DPLM program in cytopathology; the application fees and maintenance fees were supported by CLS. Having outstanding training programs, residents, and fellows benefits the health care system, as CLS and other Alberta laboratories often hire these well-trained graduates.
Recognizing a shortage of ASCP board-certified pathologists’ assistants in Canada, the DPLM and CLS opened the second NAACLS-accredited 2-year MSc training program for Pathologists’ Assistants in Canada in July 2012. To bypass considerable bureaucracy, the program began as a specialization in an already existing thesis-based medical sciences master’s degree with CLS paying the C$20 000/year graduate student stipends. This approach allowed the enrollment of 2 to 3 first-year students per year with return-of-service agreements to CLS. The ultimate goal was a course-based MSc program that would train larger numbers of students who would pay their own tuition and be free agents after graduation. CLS began the application process in September 2012 and obtained approval in January 2015 from the Alberta Ministry of Enterprise and Higher Education to offer this new degree and train up to 10 MSc students/year. The process of phasing out the thesis-based program and implementing the course-based program with the first entry class in 2016 is now underway. This year, the program director, a clinical faculty member received the Graduate Student Teacher of the Year Award within the medical school. Clearly, increasing the number of MSc trained, ASCP board-certified pathologists’ assistants in the province improves the quality of pathology services and, as physician extenders, decreases health care costs.
The DPLM and CLS play important roles in providing continuing medical education (CME) experiences required for the maintenance of competency. In addition to participating in several dozen weekly and monthly RCPSC-accredited departmental and extradepartmental specialty and subspecialty rounds, the DPLM’s penultimate CME contribution is the annual 3-day Banff pathology course, which is held at an elegant hotel in Banff National Park and is cosponsored by the DPLM and Department of Laboratory Medicine and Pathology at UofA. The Banff course, one of the premier annual pathology CME events in Canada, usually attracts 100 to 150 registrants from across North America and elsewhere. The Banff course typically provides in-depth coverage of a broad topic (eg, in 2014, gastrointestinal/liver pathology) and utilizes a combination of internationally renowned external and local faculty (http://banffpathology.ucalgary.ca/).
Clearly, the expansion in training programs, the increased number and quality of trainees enrolled, and the substantial increase in faculty-wide teaching awards demonstrate that CLS effectively supports the teaching mandate.
Research at Calgary Laboratory Services
For several reasons, some related to the structure of CLS and others related to the structure of CSM, the CLS system supports the teaching mandate better than the research mandate. First of all, the vast majority of CLS’s pathologists are clinical faculty members and do not have research as part of their job description, whereas all are expected to teach. In fact, over the past 10 years, about 85% of DPLM/CLS recruiting has been for clinical faculty members with essentially no protected time for research. Second, the DPLM is a clinical department; every member of the CLS medical or scientific staff has a clinical role. At about the time CLS was formed, the few pure basic scientists in the DPLM were transferred to basic science departments. Third, essentially, all research resources within the medical school are allocated through 7 research institutes (http://cumming.ucalgary.ca/research/institutes); departments provide position vacancies and salaries for hiring new faculty members but generally have no ability to allocate either research space or research funds. Furthermore, CLS, which is almost entirely funded by AHS, cannot normally provide startup packages or research space. CLS primarily provides salaries for clinical faculty. Fourth, the institute model works seamlessly for departments with a natural institute partner (eg, Department of Cardiac Sciences with the Libin Cardiovascular Institute or the Department of Clinical Neurosciences with the Hotchkiss Brain Institute); unfortunately, DPLM research spans all 7 institutes and does not naturally align with a single “partner” institute, making it more difficult (and requiring greater creativity) to jointly recruit clinician–scientists requiring wet laboratory space and startup funding. Finally, graduate programs within the medical school are not aligned with departments; therefore, there is no PhD program in pathology. All of these features work against DPLM, becoming highly research intensive. But, as described subsequently, the DPLM hits well above its weight in research, but this is primarily because DPLM has generally targeted recruitment to laboratory physicians focused on clinical research and/or informatics, where assignment of wet laboratory space and startup funds are less critical. Some of the research metrics presented subsequently show changes in productivity over time within DPLM, and others compare DPLM with other departments across the medical school.
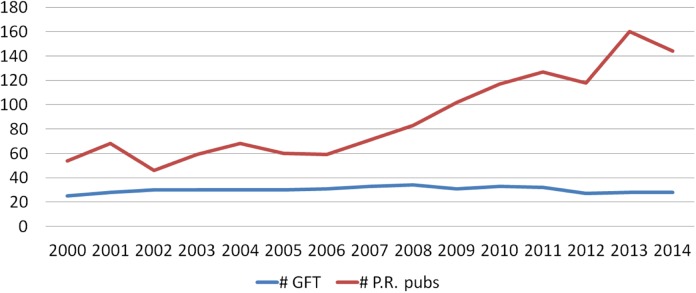
Figure 2 shows the number of articles in peer-reviewed journals published by faculty members with primary appointments in the DPLM as well as the number of GFT faculty members with primary appointments in the DPLM from 2000 to 2014. As can be seen, the upward slope in numbers of publications cannot be explained by an increase in the number of GFT faculty members. More detailed publication metrics over a 10-year period including breakdown by academic division, hospital site, GFT versus clinical faculty, and so on, are available in the annual report posted on the DPLM Web site (http://www.pathology.ucalgary.ca/). The mean impact factor of the journals DPLM faculty members have published in over the past 5 years is 4.00.
Figure 2.
Number of articles in peer-reviewed journals published by faculty members with primary appointments in the Department of Pathology and Laboratory Medicine and the number of geographic full-time (GFT) faculty members (2000-2015).
In 2015, for the first time, the CSM research office provided all 20 of its departments a “Research Report Card.” The data provided relate only to GFT faculty members and covers the year 2013. According to the report, the DPLM’s 28 GFT faculty members’ overall average job profile was 48% clinical, 28% research, 14% education, and 10% administration. When the Research Office adjusted publication output into “research equivalents” (ie, RE = the sum obtained by adding the amount of protected time for research for each DPLM GFT position), DPLM’s average publication productivity in 2013 (14.55 publications/RE with 702 citations/RE) was at least several-fold higher than average for the CSM (3.19 publications/RE with 287 citations/RE). Some DPLM publications are highly cited. The CSM defines highly cited as articles with 50 or more citations over 5 years. Over the reported time frame from 2004 through 2009, the DPLM placed fourth overall of the 20 departments and was trending upward; in the last year (2009), DPLM tied for the second place within the CSM with 14 articles cited 50 or more times. This documents the importance of work published by GFT faculty members in the DPLM.
The DPLM has matured as an academic department. Prior to 2015, no DPLM faculty member had held a named/endowed research chair. Three DPLM GFT faculty members were appointed to competitive named/endowed research chairs at CSM in 2015. From the late 1980s until 2009, there were no new AHFMR salary awards within the DPLM; a DPLM faculty member was successful in each of the last 2 competitions (2009 and 2010). When CLS began, there were no faculty members in the DPLM with over 100 career publications. In 2015, DPLM had 9 faculty members with >100, 3 with >150, and 1 with >250 publications. Although peer-reviewed publications, in general, represent the generation of new knowledge, the publication of book chapters, which is usually by invitation, is a measure of stature of faculty members. Department members with a primary appointment in the DPLM published 19 chapters and 1 book in 2013 and 15 chapters and 3 books in 2014.
Where DPLM has not excelled is in the grant funding arena (Table 1). Although the metric shows a modest upward trend in funding per GFT faculty member, the CSM Research Report Card showed that DPLM had relatively few federal Tri-Council research grants. This is not surprising as the number of RE is low, few faculty members have wet laboratory space, and all faculty members provide clinical service. That being said the Report Card also showed that because of low funding levels and high publication output, DPLM’s “cost per publication” was among the lowest in CSM (data not shown). Although the vast majority of research output is from DPLM’s GFT faculty, in 2013, 1 clinical faculty member received the DPLM’s first ever faculty-wide research award.
Table 1.
Total “Calendar Year-Adjusted” Principal Investigator Grant Funding for Faculty Members With Primary Appointments in the Department of Pathology and Laboratory Medicine (2005-2014).
| Year | Total Annual PI Funding | GFT | C$/GFT |
|---|---|---|---|
| 2005 | $1.30 million | 30 | $43 333 |
| 2006 | $1.56 million | 31 | $50 323 |
| 2007 | $1.94 million | 33 | $58 788 |
| 2008 | $2.54 million | 34 | $74 706 |
| 2009 | $2.44 million | 31 | $78 710 |
| 2010 | $1.64 million | 33 | $49 697 |
| 2011 | $2.59 million | 32 | $80 938 |
| 2012 | $1.83 million | 27 | $67 778 |
| 2013 | $2.12 million | 28 | $75 813 |
| 2014 | $2.96 million | 28 | $105 876 |
Abbreviations: GFT, geographic full-time; PI, principal investigator.
Overall, based upon the DPLM’s contributions in both teaching and research, CLS gets excellent value for its support of academics (ie, primarily its provision of salaries) and is living up to its commitments to the UofC. Furthermore, having strong clinician–scientists scattered throughout CLS and providing outstanding subspecialty expertise supports CLS clinical service mandate and its mission statement: “Improving health and well-being through laboratory diagnostic excellence, education, and research.” This expertise also allows CLS to provide expert consult services to southern and central Alberta.
Analysis
Why Is the Calgary Laboratory Services Model Unique and Why Is the Model Worthy of Study?
There are several obvious reasons that a practice model like CLS could never have happened within the United States or, at the time, even elsewhere in Canada. First of all, in American cities large enough to have one or more medical school(s), there tend to be multiple providers of health care services, multiple clinical information systems, multiple providers of laboratory services, and multiple laboratory information systems. It is implausible that a state government could mandate bringing all of this together into a single package in the United States. In contrast, AHS Calgary Zone is essentially the only health care provider and CLS essentially has a government-mandated monopoly for the provision of virtually all laboratory services for the 1.4 million population of the Calgary Zone (ie, 1.1 million within the city and 0.3 million in the rest of the zone). This combination has created a massive laboratory providing a wealth of data for laboratory informatics and clinical research.
Second, CLS, by virtue of the fact that it was to be the only laboratory service provider for an entire geographic region that included a medical school, obviously had, by default, to become the pathology department for the medical school. The UofC, although not in the “driver’s seat” related to health care system mergers resulting from regionalization, did have a vested interest in trying to make certain that pathology and laboratory services remained sufficiently strong so as not to adversely affect medical school accreditation. Therefore, early in the process of formation of CLS, interested parties negotiated a University-CLS Affiliation Agreement asserting that the medical and scientific staff at CLS would be the DPLM for the medical school, thus thrusting nonacademic pathologists into teaching roles to which some objected. More than a decade later, this Affiliation Agreement was further strengthened to make it a requirement that any pathologist working at CLS must have an academic appointment (either GFT or clinical) in the medical school; this was a critical positive change as it precluded pathologists from trying to opt out of teaching and meant that teaching became part of every pathologist’s job description. This allowed enthusiasm for teaching to be a factor in recruitment.
Although the inability of government to intervene and create a clinical service monopoly may explain why no American laboratory could have stumbled into a CLS-like model, this does not necessarily explain why this had not happened elsewhere in Canada. Unique to Alberta was the acute crisis created by cutting the laboratory budget by ∼40% in 1 year, thus precipitating the mass exodus of pathologists. The provincial government of the time does not deserve all of the “credit” for this decision, as how the new austerity was to have been apportioned within various physician groups was not a unilateral decision by government (ie, it ended up that physician negotiators representing the vast majority of Alberta physicians were willing to sacrifice their laboratory medicine colleagues to lessen their own economic pain).1 However, regardless of how the blame for this decision is apportioned, there were simply not enough pathologists remaining to provide health care services. This situation created an opportunity, and a task force was established to determine how to entice pathologists to relocate to Alberta. Whatever was to be done, it needed to be highly attractive as the pathologists who had left the province had little good to say about working in Alberta. Figuring importantly into these discussions was that few Canadian medical graduates had gone into pathology in the 1990s, resulting in a shortage across Canada.8 After a couple of stressful years, the solution unveiled in 1998 was Alberta’s “pathologist GRID,” a remuneration system that paid pathologists at one of 4 very attractive levels, depending upon years of experience (nb: the GRID accelerated to the top level at 4 years of experience). Although the GRID was negotiated primarily by nonacademic pathologists, a small cohort of influential academic pathology leaders worked skillfully behind the scene to achieve 2 critical concessions—first, that the GRID be also applied to academic pathologists and, second, that an hour of academic time be compensated at the same rate as an hour of clinical work. Critical to the widespread acceptance of this by rank-and-file pathologists was that almost everyone got a substantial raise. The GRID has been essential to the academic success of the CLS model, as it has facilitated the recruitment of outstanding research-oriented pathologists with strong diagnostic and teaching skills.
Clearly, both the UofA and the UofC benefited from the GRID. Why did a CLS-like structure not develop in Edmonton during the late 1990s? Likely, the primary reason was that, unlike in Calgary, Edmonton had 2 major Catholic hospitals which had separate administrative structures; for political reasons, these could not be merged into the Capital Health Regional Authority, and so true “regionalization” did not occur at that time. Furthermore, the Department of Laboratory Medicine and Pathology at the UofA, being the stronger medical school based in the provincial capital, was in a better position to insist on maintaining its autonomy. Although there was some restructuring of private laboratories in Edmonton, the resulting private laboratory,1 which has undergone name and ownership changes, has maintained its position providing predominately community testing for the duration of a 15-year contract. Interestingly, at the end of 15 years, a request-for-proposals process was put in place to merge all laboratory services in Edmonton, including those at the University, into a single private laboratory entity expected to replicate many features of CLS (see subsequently).
Keys to Academic Success at Calgary Laboratory Services
Upon reflection, there appear to have been 5 keys to successful promotion of the academic mandate within CLS. These are the GRID, the University-CLS Affiliation Agreement (both previously discussed), gaining buy-in for the academic mandate by understanding and trying to manage town–gown dynamics, turnover, and successful recruitment/retention.
The UofC has very little ability to provide financial support to DPLM, and so the vast majority of funding for laboratory physician salaries comes from the health care system. In fact, most faculty members are clinical, without protected time, rather than GFT. Therefore, it is important to get “buy-in” for the academic mandate from clinical faculty. In the ideal world, clinical and GFT faculty should work together in harmony and respect. The GFT faculty should value the clinical faculty who, by doing 100% clinical work, subsidize their protected time for research. Likewise, clinical faculty should value and take pride in being a member of an academically strong department having GFT colleagues who publish important papers and who are international authorities in their fields. Repeated attempts to educate both groups, although not always successful, are necessary. In a system like CLS where some physicians have protected time and most do not, allowing any GFT to slack-off or “coast” is fatal to maintaining cohesion. Because laboratory physicians doing research are paid at the same level as those doing 100% clinical work, research-intensive faculty must be held accountable for every bit of their protected time. The UofC has mechanisms for dealing with chronic low productivity, and these were applied judiciously.
The ability to recruit effectively has been fundamental to the success of CLS. During its early years, there was a shortage of pathologists in Canada,8 and recruitment had to be focused on finding pathologists to provide clinical service, and it was not feasible to hire only those with strong academic credentials or even only those generally supportive of the academic mandate. Furthermore, because of the way it was formed, CLS was not initially a happy place. Many of the hard-earned gains that led to a successful academic culture in the DPLM at the Foothills Hospital in the early 1990s and that supported the medical school’s accreditation were threatened when the pathologists at the private laboratories and community hospitals arrived as many did not see any value in their new GFT colleagues having protected time for academics. Although many of the new nonacademic pathologists joining CLS were genuinely enthusiastic about opportunities to teach their profession as clinical faculty members to residents, many did not appreciate being “second-class” faculty who were expected to teach while performing full-time clinical service when their GFT colleagues had protected time for teaching. However, once the smoke had cleared and CLS was almost fully staffed, later rounds of recruitment allowed greater and greater selectivity and the ability to raise the bar with each subsequent recruitment. When the occasional opportunity to hire a new GFT faculty member arose, searches were failed, if necessary, in order to hire only excellent candidates. Many new clinical faculty brought strong publication track records and sufficient energy to find their own time for clinical research. Although not all newly recruited pathologists were expected to publish, everybody had to express enthusiasm for teaching residents and fellows during the interview process and be able to document a strong teaching track record. Undoubtedly, recruitment to CLS was aided by Calgary being an attractive place to live with 8 national parks within a 4-hour driving radius.
Part of the CLS transformation was turnover. In the past 10 years, 77 new medical and scientific staff who openly supported DPLM’s and CLS’s academic mandate were carefully recruited. In the same time frame, 36 departed for a variety of reasons including retirements, opportunities elsewhere, or simply not agreeing with the current more academic direction in which DPLM and CLS were moving. This resulted in a net gain of 41 medical and scientific staff over 10 years. Remuneration ceased to be an important reason for staying at CLS, as pathologist remuneration in much of the rest of Canada eventually caught up with the Alberta GRID that had been implemented to attract pathologists back to Alberta.
In recent years, CLS has provided a good work environment. In 2009, CLS achieved the status of being named one of the top 40 companies in Alberta based upon its human resource practices, and it has continued to hold top company status in most years since that date. An AHS Calgary Zone Medical Affairs physician engagement survey in late 2014 showed that the DPLM medical staff are generally happy. Department of Pathology and Laboratory Medicine tied with one other clinical department for having the most favorably + neutrally engaged (83%) and least negatively (17%) engaged physicians in its workforce.
Academic promotion is perhaps the best metric for measuring growth of academic culture in the CLS system. The DPLM GFT faculty members have always been anxious to be promoted, but DPLM clinical faculty members historically were never motivated by promotion. Because both GFT and clinical faculty members who are physicians are paid according to the GRID, increasing academic rank does not increase remuneration, and so there is no financial incentive. In the early years of CLS, there were no clinical faculty members promoted. In the past 9 years, there have been 16 successful clinical faculty promotions. Increased interest in promotion supports the tenet that many clinical faculty members have bought into the academic culture and are now much more enthusiastic about having clinical faculty appointments. Part of promoting academic culture is acknowledging and rewarding academic excellence by nominating faculty for awards and mentoring for promotion.
Although CLS is clearly a Canadian model, most of these elements of success, with the notable exception of a provincial payment GRID, are applicable to an American environment. Although a formal academic affiliation agreement may not be necessary for university-based academic departments, having absolute clarity as to expectations, limitations, and deliverables is highly advantageous; this clarity should exist at both the university–department level and the department–faculty member level, as this is critical for accountability. In departments with clinical faculty, efforts directed at faculty engagement and minimizing town–gown issues clearly promote departmental unity and academic success. Finally, no 2 academic departments play on a level playing field, as academic assets, opportunities, and liabilities differ from department to department. Therefore, it is critical to scan local, national, and, in some instances, international environments to establish a “departmental niche” that optimizes areas of potential competitive academic advantage. Establishing a niche facilitates optimal and targeted recruitment as well as promotes retention of high-quality faculty members.
Calgary Laboratory Services as a Template for Academic Pathology in Canada
During its almost 20-year history, CLS has become a prototype that is now being partially replicated at several other Canadian medical schools. Similar to the formation of CLS, these changes are being driven by expected savings for the respective provincial health care systems. In Ottawa, the nation’s capital, 16 hospital laboratories in the city, and surrounding area were merged into a single publicly owned laboratory entity, in partnership with the University of Ottawa, called the Eastern Ontario Regional Laboratory Association (EORLA; http://www.eorla.ca/). In this model, EORLA is the pathology department for the Faculty of Medicine, and the Chair of the DPLM at the University is the medical and scientific director at EORLA. EORLA bears striking similarity to CLS, except that EORLA is responsible for laboratory services only in the partner hospitals; community testing, which is part of the CLS service mandate, is specifically excluded and is provided by a private medical laboratory company which was not merged into EORLA. EORLA was registered as a nonprofit organization in 2003 but took the better part of 10 years for the plan to be fully implemented in a controlled manner and with transition funding from the provincial government. Also in 2003, pathology and laboratory services throughout the province of Manitoba began a province-wide merger process to form Diagnostic Services of Manitoba (DSM; http://dsmanitoba.ca/wp-content/uploads/2015/02/History-and-Evolution-of-DSM-Board.pdf). The department at the University of Manitoba is a core component in provision of general and advanced diagnostic services for DSM, whereas DSM provides considerable funding for the academic department. Although DSM has a similar mandate to that of CLS, this model has weaker similarities.
As briefly mentioned earlier, with the 15-year contract for Edmonton Zone’s current corporate provider of community laboratory services about to end, AHS has been in the process of creating a CLS-like laboratory in Edmonton with a large multinational laboratory firm functioning as the Department of Laboratory Medicine and Pathology for the UofA and supporting all aspects of the academic mandate (http://www.cbc.ca/news/canada/edmonton/alberta-health-services-privatizing-edmonton-labs-1.2460544; http://www.cbc.ca/news/canada/edmonton/australia-s-sonic-healthcare-nets-3b-contract-for-edmonton-labs-1.2802270; http://www.albertahealthservices.ca/assets/wf/lab/ahs-lab-ed-lab-faq.pdf). The new entity was also expected to provide clinical services for the entire northern part of the province (geographically about 75% of the province). However, there were legal challenges to the bidding process by the current corporate provider of community laboratory services when their application was not chosen by AHS, and this appeal delayed further negotiations and implementation for over 6 months. Unexpectedly, during this delay, in May 2015, the party that had been in power for 44 years lost a provincial election and was replaced by a left-leaning centrist party ideologically opposed to health care privatization. On August 14, 2015, as this article was being finalized for submission, the new government of Alberta cancelled the request for proposals stating that additional privatization was not in the public interest (http://www.cbc.ca/news/canada/edmonton/health-minister-cancels-3b-contract-will-not-expand-private-services-in-alberta-1.3190004; http://globalnews.ca/news/2163916/watch-live-albertas-health-minister-discusses-lab-services-in-edmonton/; http://alberta.ca/release.cfm?xID=3840692B96D62-E6DD-4217-8185C0474417A051). The project is now on hold for further study and deliberations.
Conclusion
Hopefully, this case study has demonstrated that the unique Canadian CLS model, a success story originating from an unplanned “experiment” in academic pathology, can provide robust academic support for a medical school while providing efficient, economical, and excellent clinical service. Calgary Laboratory Services came into existence rapidly, out of dire necessity, and in reaction to abrupt and drastic changes in laboratory service funding and started essentially as an “unhappy shotgun marriage” of public, private, and academic laboratory physicians. The early years were unsettling, but by 2009, CLS had achieved the status of being one of Alberta’s top 40 companies. It took CLS the better part of 2 decades to develop an academic culture and achieve the current level of success; perhaps, the length of time can be shortened at other Canadian medical schools through advanced planning and studying what happened in Calgary.
Finally, it is hoped that this case study will allow American colleagues to understand some of the differences in practicing academic pathology in Canada, where provincial politics can induce abrupt changes in direction. Clearly, of the previously mentioned 5 principles of the Canada Health Act, “public administration,” which facilitates government micromanagement instead of an arm’s length approach, can be the most trying for medical administrators.
Acknowledgments
The author would like to thank Drs Fred Swaine and Lynn McIntyre for reading late drafts of this manuscript and for helpful comments.
Authors’ Note: Previously presented by JR Wright Jr. State of the DPLM. Calgary Laboratory Services weekly CME series; May 21, 2015; Foothills Medical Centre, Calgary, Alberta, Canada.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. The author declared no potential conflicts of interest with respect to financial or commercial interests, but as a former department head and member of the CLS Executive may have personal biases. This is addressed within the text under a discussion of qualifications to write a paper on this topic and potential biases.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Fagg KL, Gordon P, Reib B, et al. Laboratory restructuring in metropolitan Edmonton: a model for laboratory reorganization in Canada. Clin Chim Acta. 1999;290:73–91. [DOI] [PubMed] [Google Scholar]
- 2. Forsman RW. Why is the laboratory an afterthought for managed care organizations? Clin Chem. 1996;42:813–816. [PubMed] [Google Scholar]
- 3. Wright JR., Jr The development of the frozen section technique, the evolution of surgical biopsy, and the origins of surgical pathology (William Osler Medal Essay). Bull Hist Med. 1985;59:295–326. [PubMed] [Google Scholar]
- 4. Wright JR., Jr Cytopathology: why did it take so long to thrive? Diagn Cytopathol. 2015;43:275–263. [DOI] [PubMed] [Google Scholar]
- 5. Wright JR, Jr, Wold LE, Carney JA, Young RH. History of gynecological pathology: XXVI. Dr. Malcolm Dockerty. Int J Gynecol Pathol. 2015;34:101–110. [DOI] [PubMed] [Google Scholar]
- 6. Wright JR, Jr, Baskin LB. Pathology and laboratory medical support for the American Expeditionary Forces by the US Army Medical Corps during World War i. Arch Pathol Lab Med. 2015;139:1161–1172. [DOI] [PubMed] [Google Scholar]
- 7. Wright JR, Jr, Shokeir MO, Joseph JJ, Gao ZH. Late autopsy reports: the Calgary solution. Can J Pathol. 2011;3:26–30. [Google Scholar]
- 8. Colgan TJ, Geldenhuys L. The practice of pathology in Canada: decreasing pathologist supply and uncertain outcomes. Arch Pathol Lab Med. 2012;136:90–94. [DOI] [PubMed] [Google Scholar]